Abstract
Background
Immigrants have disproportionate lack of access to healthcare and insurance. Emergency departments could serve as a healthcare substitute and increased demand can negatively affect the U.S. emergency services system.
Methods
Medical Expenditures Panel Survey (2000–2008) data was modeled to compare ED use between non-citizens, foreign-born (naturalized), and US-born citizens. Group differences were assessed using non-linear decomposition techniques.
Results
Non-citizens were less likely to use ED services (8.7%) compared to naturalized immigrants (10.6%) and US-born Americans (14.7%). Differences in ED use persisted after adjusting for the Behavioral Model covariates. Healthcare need and insurance partially explained the differences in ED use between the groups.
Conclusion
Between 2000–2008 non-citizen immigrants used markedly less ED services compared to U.S. citizens, regardless of their nation of origin. We also found that demographic and healthcare need profiles contributed to the divergence in use patterns between groups. A less restrictive healthcare policy environment can potentially contribute to lower population disease burden and greater efficiencies in the U.S. health care system.
INTRODUCTION
The proportion of U.S. immigrants will nearly double between 2010 and 2050.1 Evidence about how different healthcare policy environments affect immigrant access to care is currently underdeveloped.2,3 A significant concern is the potential over-reliance among immigrants on emergency department services.
Healthcare disparities among immigrants have been documented 3,4 with considerable variation reported within and between immigrant groups. Contributors to these disparities include socio-economic factors that enable healthcare access, legal residency issues that are compounded by length of residence, acculturation, and difficulty integrating into a new culture.4–6 Predisposing characteristics (e.g., racial/ethnicity), may reinforce such disparities. Differential healthcare access among immigrants, especially insurance coverage, has widened recently; notably following the 1996 welfare reform and subsequent economic downturns.7,8 A substantial proportion of immigrants will continue to face access restrictions under the Affordable Care Act (ACA).9
Disproportionate access to insurance10 and primary and preventive care3,11 services can negatively affect immigrants’ healthcare behavior. Lower use of these services has been documented among both privately and publicly insured immigrants,12 affecting citizens and non-citizens alike.13 Neither group fully converges with the higher access of US-born citizens.13 Reduced access to healthcare services, especially due to lack of insurance, could shift help-seeking to less appropriate and efficient modes of healthcare, such as emergency departments (ED).14 Lower access also leads to delays in treatment until more severe symptoms and disease complications occur, therefore requiring more intensive interventions.15,16
The continuing shift in population toward more immigrant-centered households, if associated with an increase in use of ED services for routine non-acute services, could herald future pressures on the emergency services system. The ED care system is not structured to accommodate the resulting increase in demand, which could exacerbate ED overcrowding, delay access for patients with critical needs, reduce patient satisfaction, further drive up costs, and reduce providers’ profitability.17–20
The three main purposes of this study were to: (1) provide a detailed accounting of ED use with policy-relevant immigrant classifications;21 (2) examine associations between ED use and citizenship status using a Behavioral Model of healthcare access and utilization;22,23 and (3) determine the most important factors associated with differences in immigrants’ ED services use. We conclude with a set of recommendations that could enhance efficiencies in US healthcare access and use.
METHODS
Data
We used data from the Medical Expenditures Panel Survey (MEPS) full-year consolidated files. The yearly files can be used to generate calendar year estimates for the US non-institutionalized population. Since the MEPS does not collect respondents’ citizenship status, we linked the MEPS files to data from the National Health Interview Survey which include this information.24 To increase sample size and permit time trends analyses, we aggregated 9-years of MEPS data (2000–2008). The combined files were linked to a common variance structure file that allows investigators to combine multiple years and generate valid population statistical inferences.25 Detailed analysis guidelines and technical treatments of MEPS/NHIS data linkage and MEPS yearly files aggregation are available elsewhere.24,25 Between 2000 and 2008, the MEPS response rates varied between 66.3% and 56.9%.26
Main Outcome
Self-reported past-year ED use was used to generate a dichotomous indicator with a “no ED visit” and a “one or more visits” group. The total number of visits reported was also examined to ensure the robustness of our findings to rival outcome operationalization.
Main predictor
Self-reported immigration status and nativity were used to create a three-category indicator of US-born citizens (USB); naturalized foreign-born (FB) citizens (immigrants who have obtained US citizenship) and FB non-citizens. We used “citizenship groups” and “citizenship status” interchangeably to refer to these groupings. Neither the MEPS nor the NHIS include information on immigrants’ documentation status. The non-citizens category combines legal permanent residents (slightly less than half of non-citizens), as well as undocumented and “other” immigrants.27,28
Multivariate model covariates
We used a Behavioral Model of healthcare services access approach 22,23 to test for main predictor modifications and explain possible difference in ED use between groups. Our healthcare access enabling factors included: (1) insurance status (i.e., private insurance, public insurance; and uninsured), (2) household income-to-poverty threshold ratio accounted for using a MEPS staff generated indicator (<100%; 100%–124%; 125%–199%; 200%–399%; and ≥ 400%),29 and 3) usual source of care (USC) availability (No; Yes). Our predisposing factors included: (1) self-reported ethnicity/race grouped into four categories (Non-Latino Whites, Non-Latino Blacks, Latinos/Hispanics, or Non-Latino “Other”), (2) age (18–34; 35–44; 45–54; 55–64; and 65-years and older), (3) gender (Female; Male), and (4) education level (< high school; high school; some college; and college or more). We assessed healthcare need factors using four dichotomous indicators including: (1) A general self-rated health indicator30 based on the question: “In general, would you say your health is Excellent, Very Good, Good, Fair, or Poor?” (recoded as: Poor/Fair; Good/Very Good/Excellent), (2) medical conditions including angina, asthma, coronary heart disease, diabetes, hypertension, reporting having a heart attack or other heart conditions, stroke, emphysema, and joint pain (none; at least one), (3) past-year healthcare provider visit (No; Yes), and 4) one or more past-year hospital discharge (No; Yes). Finally, we controlled for possible regional effects (Northeast; Midwest; South; and West) and urbanicity using Metropolitan Statistical Area residence as a proxy (MSA; non-MSA), and accounted for time using a categorical survey year indicator setting 2000 as the reference.
Analytic approach
We used the survey procedures available in the Stata 12.1 software, adjusting for the sample survey design, including stratification, clustering and probability weighting when applicable and allowing correct population inferences. Our population of interest was adults 18-years and older residing in the US, chosen because of the bimodal concentration of ED use among both young and older adults.31,32 Observations with missing data on the model covariates (5.25% of the sample) were excluded. Compared to our analytical sample, the excluded subsample did not present statistically significant differences in ED services use or expenditures. The analytical sample included n=167,889 respondents representing yearly weighted population counts of 198,156,235 US residents.
Our analyses were done in five steps. First, we provided descriptive statistics for study variables by citizenship status. Second, we calculated average prevalence of ED use over the study period. Next, we generated a profile of healthcare services expenditures and use for ED users and non-users by citizenship status. To examine expenditures we looked at overall spending as well as ED and hospitalization expenditures. To examine use we looked at frequency of ED use, primary care visits, and hospitalization discharges. We used chi-squared and Wald adjusted independence and means tests to establish statistical differences. Third, we looked at time trends in ED use by citizenship status to examine stability of use overtime. Graphs of these trends were subsequently generated. Given the lack of difference in ED expenditures by citizenship status among those who reported ED services use (see results), we focused our attention on the propensity to use ED services. Fourth, we modeled the relationship between ED use and our covariates of interest. Logistic regression models were fit incrementally to test the relationship between our dichotomous indicator distinguishing between spenders and non-spenders and the main predictor and covariates of interest. Given the high differences in rates of uninsurance between citizenship groups we tested for the ED as a “safety net” immigrant care provider hypothesis by accounting for the interactive effects of citizenship status and insurance. Finally, we used Fairlie’s nonlinear decomposition method33–35 to investigate the factors contributing to the differences in propensity of use between the three considered groups. The method uses iterative sampling (500 in this study) and group matching techniques to partition the predicted gap in the probability of an outcome into differences explained by the distribution of model covariates in two groups of interest, and differences due to unobserved factors. Subsequently, it estimates the contribution of each model covariate to the explained difference between the groups.34
RESULTS
Sample characteristics
Descriptive statistics (Table 1) indicated that non-citizens were younger, and economically and educationally disadvantaged compared to citizens (both foreign and US-born). Non-citizens, also, had lower “potential” (health insurance) and “realized” (USC) levels of access to healthcare compared to the other groups. Non-citizens had favorable health profiles with less than a third reporting one or more chronic conditions (29.5%) compared to a majority of both the FB (51%) and USB (56.6%) citizens.
Table 1.
Descriptive statistics of U.S. adults 18-years and older by citizenship status. Results are from the Medical Expenditures Panel Survey (2000–2008).
| Non-Citizens n=20,449 |
FB-Citizensa n=14,338 |
USBa n=133,102 |
Total n=167,889 |
|
|---|---|---|---|---|
| %(se) | %(se) | %(se) | %(se) | |
| Ageb | ||||
| 18–34 | 43.6(0.8) | 19.9(0.6) | 29.1(0.3) | 29.5(0.3) |
| 35–44 | 27.9(0.6) | 21.6(0.6) | 19.2(0.2) | 20.0(0.2) |
| 45–54 | 15.3(0.5) | 22.5(0.6) | 19.6(0.2) | 19.5(0.2) |
| 55–64 | 7.5(0.4) | 17.1(0.5) | 14.6(0.2) | 14.3(0.2) |
| 65+ | 5.6(0.3) | 18.8(0.7) | 17.5(0.3) | 16.7(0.3) |
| Race/Ethnicityb | ||||
| Non-Latino Whites | 15.9(0.9) | 29.6(0.9) | 79.8(0.5) | 71.5(0.6) |
| Non-Latino Blacks | 5.7(0.5) | 6.4(0.5) | 11.6(0.4) | 10.8(0.4) |
| Latinos | 58.9(1.3) | 36.3(1.2) | 6.0(0.4) | 12.0(0.5) |
| All Other (Non-Latino) | 19.4(0.9) | 27.7(1.1) | 2.6(0.2) | 5.6(0.2) |
| Sexb | ||||
| Female | 48.8(0.5) | 52.6(0.6) | 52.3(0.1) | 52.0(0.1) |
| Male | 51.2(0.5) | 47.4(0.6) | 47.7(0.1) | 48.0(0.1) |
| Educationb | ||||
| Less than high school | 45.4(1.0) | 24.6(0.7) | 17.2(0.3) | 19.8(0.3) |
| High school | 19.6(0.6) | 22.5(0.6) | 32.8(0.4) | 31.1(0.3) |
| Some college | 8.4(0.4) | 13.4(0.5) | 16.1(0.2) | 15.3(0.2) |
| College or more | 26.6(0.9) | 39.6(0.9) | 33.9(0.5) | 33.8(0.5) |
| Poverty Statusb | ||||
| Poor | 17.7(0.6) | 10.0(0.4) | 9.6(0.2) | 10.2(0.2) |
| Near poor | 7.3(0.3) | 4.5(0.3) | 3.6(0.1) | 3.9(0.1) |
| Low income | 21.2(0.5) | 13.3(0.4) | 11.9(0.2) | 12.7(0.2) |
| Middle income | 31.1(0.7) | 30.8(0.7) | 31.2(0.3) | 31.2(0.2) |
| High income | 22.6(0.8) | 41.4(0.9) | 43.7(0.5) | 41.9(0.5) |
| Insurance Statusb | ||||
| Private | 47.3(1.0) | 68.1(0.8) | 75.5(0.4) | 72.9(0.4) |
| Public | 14.3(0.6) | 17.9(0.6) | 13.6(0.3) | 13.9(0.3) |
| No Insurance | 38.5(1.0) | 13.9(0.6) | 10.9(0.2) | 13.2(0.2) |
| Self-reported Health Statusb | ||||
| Good/Very good/Excellent | 86.0(0.4) | 83.2(0.5) | 86.3(0.2) | 86.1(0.2) |
| Poor/Fair | 14.0(0.4) | 16.8(0.5) | 13.7(0.2) | 13.9(0.2) |
| Medical conditionsb | ||||
| None | 70.5(0.6) | 49.1(0.8) | 43.4(0.3) | 45.9(0.3) |
| One or more | 29.5(0.6) | 50.9(0.8) | 56.6(0.3) | 54.1(0.3) |
| Usual Source of Careb | ||||
| No | 45.3(0.9) | 22.9(0.7) | 19.4(0.3) | 21.6(0.3) |
| Yes | 54.7(0.9) | 77.1(0.7) | 80.6(0.3) | 78.4(0.3) |
| MSA Statusb | ||||
| Non-MSA | 5.3(0.8) | 5.2(0.6) | 20.0(0.9) | 17.9(0.8) |
| MSA | 94.7(0.8) | 94.8(0.6) | 80.0(0.9) | 82.1(0.8) |
| Regionb | ||||
| Northeast | 18.9(1.2) | 27.3(1.6) | 18.1(0.9) | 18.8(0.8) |
| Midwest | 9.8(1.0) | 11.9(0.9) | 24.8(1.0) | 22.7(0.9) |
| South | 31.3(1.8) | 26.8(1.4) | 37.2(1.2) | 36.0(1.2) |
| West | 40(1.8) | 34.0(1.7) | 19.9(1.2) | 22.4(1.2) |
| Survey yearb | ||||
| 2000 | 8.3(0.7) | 7.9(0.6) | 10.7(0.8) | 10.3(0.7) |
| 2001 | 9.8(0.4) | 9.2(0.4) | 10.8(0.2) | 10.6(0.2) |
| 2002 | 11.0(0.4) | 11.0(0.3) | 10.9(0.2) | 10.9(0.2) |
| 2003 | 11.4(0.4) | 11.7(0.4) | 11.0(0.2) | 11.1(0.2) |
| 2004 | 11.5(0.4) | 11.8(0.5) | 11.1(0.2) | 11.2(0.2) |
| 2005 | 11.5(0.4) | 11.4(0.4) | 11.3(0.2) | 11.3(0.2) |
| 2006 | 11.9(0.4) | 12.0(0.4) | 11.4(0.2) | 11.5(0.2) |
| 2007 | 12.3(0.4) | 12.5(0.4) | 11.3(0.2) | 11.5(0.2) |
| 2008 | 12.3(0.7) | 12.5(0.6) | 11.6(0.4) | 11.7(0.4) |
“FB-Citizens” indicates foreign-born citizens (i.e., naturalized), and USB stands for United States born citizens
Design adjusted χ2 test indicated statistically significant differences between groups; P<0.01
Profiles of healthcare use and expenditures
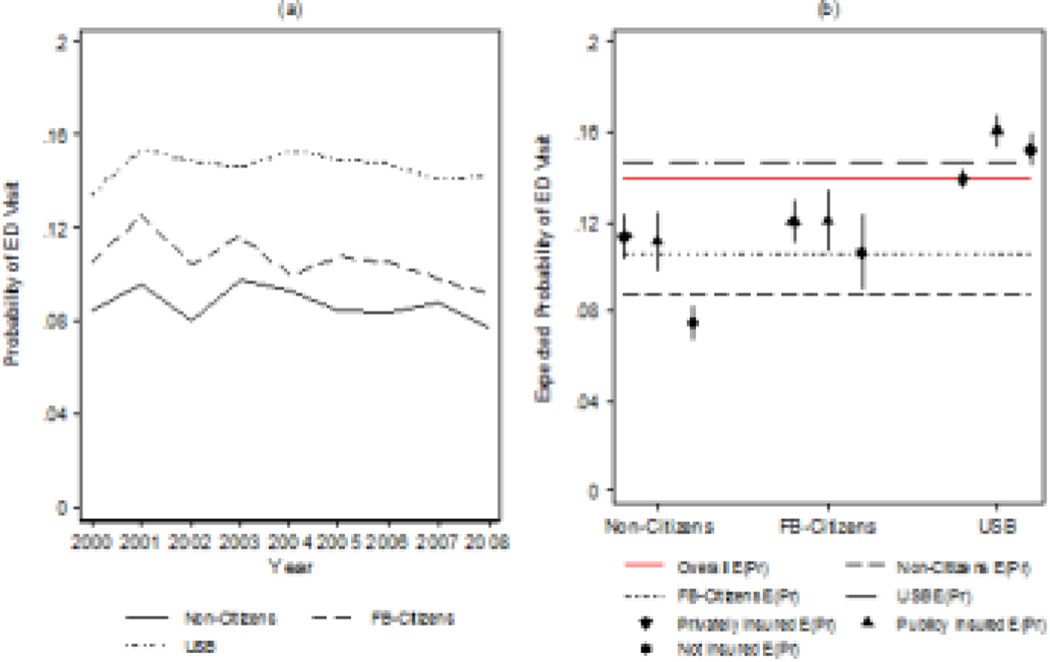
Results in Table 2 showed that immigrants, and particularly non-citizens, were less likely to use ED services compared to the USB. Rates of ED use increased between 2000 and 2006, but trended back to 2000 levels by 2008. The time trends were statistically comparable across the three groups [Figure 1; (a)].Lower use among non-citizens was also evident with the other considered services; group members reported lower rates of physician visits, hospitalizations, and repeat use of healthcare services compared to the other groups. These findings were present among both users and non-users of ED services (Table 2).
Table 2.
Healthcare use and expenditures among adults 18-years and older in the U.S by emergency department use and citizenship status. Results are from the Medical Expenditures Panel Survey (2000–2008).
| Non-Citizens n=20,449 |
FB-Citizensa n=14,338 |
USBa n=133,102 |
Total n=167,889 |
|
|---|---|---|---|---|
| Adults 18-years and older | ||||
| ED Use 12-month [%(SE)]b | 8.7(0.3) | 10.6(0.3) | 14.7(0.2) | 13.9(0.2) |
|
Non-Citizens n=18,600 |
FB-Citizens n=12,718 |
USB n=111,952 |
Total n=143,270 |
|
|
Adults 18-years and older with NO ED Use Utilization |
||||
| Doctor visit [%(SE)]b | 47.5(0.8) | 67.1(0.7) | 72.4(0.2) | 70.1(0.2) |
| Repeat Doctor visits (i.e. >=2 visits) [%(SE)]b | 34.3(0.7) | 52.7(0.6) | 56.1(0.3) | 54.1(0.3) |
| Hospitalization [%(SE)]b | 3.9(0.2) | 4.2(0.2) | 5.2(0.1) | 5.0(0.1) |
| Repeat hospitalization (i.e. >=2 discharges) [%(SE)]b | 0.3(0.0) | 0.5(0.1) | 0.8(0.0) | 0.7(0.0) |
| Expenditures per-capita | ||||
| Overall Expenditures (U.S. $) [Mean(SE)] | 1368(64) | 2777†(82) | 3309†‡(39) | |
| Hospitalization Expenditures (U.S. $) [Mean(SE)] | 393(45) | 557*(51) | 678†¥(16) | |
|
Non-Citizens n=1,849 |
FB-Citizens n=1,620 |
USB n=21,150 |
Total n=24,619 |
|
|
Adults 18-years and older with ED use Utilization |
||||
| Doctor visit [%(SE)]b | 74.8(1.4) | 83.7(1.3) | 83.3(0.3) | 82.9(0.3) |
| Repeat Doctor visits (i.e. >=2 visits) [%(SE)]b | 58.3(1.6) | 72.7(1.6) | 71.3(0.4) | 70.8(0.4) |
| Repeat ED use (i.e. >=2 visits) [%(SE)]b | 20.0(1.3) | 24.9(1.4) | 24.4(0.4) | 24.2(0.3) |
| Hospitalization [%(SE)]b | 26.4(1.2) | 29.3(1.5) | 32.6(0.4) | 32.1(0.4) |
| Repeat hospitalization (i.e. >=2 discharges) [%(SE)]b | 3.7(0.6) | 9.4(0.9) | 9.4(0.3) | 9.1(0.2) |
| Expenditures per-capita | ||||
| Overall Expenditures (U.S. $) [Mean(SE)] | 7021(443) | 11856†(1246) | 11105†(236) | |
| ED Expenditures (U.S. $) [Mean(SE)] | 937(54) | 1065(78) | 976(18) | |
| Hospitalization Expenditures (U.S. $) [Mean(SE)] | 3407(348) | 5969*(1165) | 5107†(186) | |
| Out of pocket proportion of ED expenditures | ||||
| ED [Proportion(SE)] | 0.23(0.01) | 0.14†(0.01) | 0.15†(0.00) | |
“FB-Citizens” indicates foreign-born citizens (i.e., naturalized), and USB stands for United States born citizens
Design adjusted χ2 test indicated statistically significant differences between groups; P<0.01
Significantly different than non-citizens P<0.01
Significantly different than non-citizens P<0.05
Significantly different than FB-citizens P<0.01
Significantly different than FB-citizens P<0.05
Figure 1.
Emergency department use by citizenship status among U.S. adults 18-years and older. Data from the medical Expenditure Panel Survey (2000–2008).
Note 1: “FB-Citizens” indicates foreign-born citizens (i.e., naturalized), and USB stands for US-born citizens
Note 2: Panel (a) Presents unadjusted trends in emergency department use by citizenship status among U.S. adults 18-years and older.
Note 3: Panel (b) presents the predicted probabilities of emergency department use among U.S. adults 18-years and older by citizenship and insurance status. Predicted values are based on logistic regression model using data from the Medical Expenditure Panel Survey (2000–2008). E(pr) indicates the expected 12-month probability of emergency department use. The straight lines present the average unadjusted probability of use for the overall sample, as well as by citizenship grouping. The point estimates represent fully adjusted expected probabilities and their 95% confidence interval by citizenship and insurance status.
Non-citizens presented the lowest overall and hospitalization specific per-capita expenditures. These expenditures were highest among FB-citizens reporting an ED visit. Variations in per-capita ED expenditures for the three citizenship groups were not statistically distinguishable (Table 2). As expected, however, given the lower insurance prevalence in the group, the out of pocket proportion of ED spending was highest among non-citizens compared to both citizens and the US-born.
Citizenship status, insurance and ED use
Results in Table 3 showed that citizens, especially the USB, had higher odds of ED use compared to non-citizens. Differences were maintained after fully adjusting for our enabling, predisposing and need factors. Accounting for the covariates slightly attenuated the odds of ED use among the USB (Model 2). Insurance status presented different effects within citizenship groups (Model 3). Lack of insurance decreased the probability of use among the two FB groups, but the effects of un-insurance on the drop in the probability of use were significantly pronounced among non-citizens. Public insurance increased the probability of use among the USB. Predicted ED use profiles by citizenship grouping and insurance status are presented in Figure 1, (b).
Table 3.
Correlates of emergency department use among U.S. adults 18-years and older. Results are from logistic regression models using the Medical Expenditures Panel Survey (2000–2008).
| Model 1 OR(95%CI) |
Model 2 OR(95%CI) |
Model 3 OR(95%CI) |
|
|---|---|---|---|
| Primary Predictor | |||
| Immigrant Status (ref: USB) | |||
| Non-Citizens | 0.55***(0.52–0.60) | 0.61***(0.56–0.66) | 0.77***(0.68–0.86) |
| FB-Citizens | 0.69***(0.64–0.74) | 0.76***(0.70–0.84) | 0.82***(0.74–0.92) |
| Enabling factors | |||
| Insurance Status (ref: Private insurance) | |||
| Public | 1.20***(1.13–1.27) | 1.22***(1.15–1.29) | |
| No Insurance | 1.05(0.98–1.12) | 1.13***(1.05–1.21) | |
| Immigration*Insurance Status | |||
| Non-Citizen*Private insurance | 0.80**(0.66–0.96) | ||
| Non-Citizen*Public insurance | 0.53***(0.44–0.63) | ||
| FB-Citizen*Private insurance | 0.83**(0.70–0.98) | ||
| FB-Citizen*Public insurance | 0.76**(0.61–0.94) | ||
| Poverty Status (ref: High income) | |||
| Poor | 1.50***(1.41–1.60) | 1.50***(1.41–1.60) | |
| Near poor | 1.40***(1.28–1.53) | 1.40***(1.27–1.53) | |
| Low income | 1.33***(1.25–1.41) | 1.32***(1.25–1.40) | |
| Middle income | 1.12***(1.06–1.18) | 1.12***(1.06–1.17) | |
| Usual Source of Care (ref: No) | |||
| Yes | 0.99(0.94–1.05) | 0.99(0.94–1.05) | |
| Predisposing factors | |||
| Age (ref: 18–34) | |||
| 35–44 | 0.79***(0.75–0.83) | 0.79***(0.75–0.83) | |
| 45–54 | 0.71***(0.67–0.75) | 0.71***(0.67–0.75) | |
| 55–64 | 0.59***(0.56–0.63) | 0.59***(0.56–0.63) | |
| 65+ | 0.61***(0.58–0.65) | 0.62***(0.58–0.66) | |
| Race/Ethnicity (ref: Non-Latino Whites) | |||
| Non-Latino Blacks | 1.20***(1.13–1.27) | 1.19***(1.12–1.26) | |
| Latinos | 0.98(0.91–1.06) | 1.00(0.93–1.08) | |
| All Other (Non-Latino) | 0.93(0.83–1.03) | 0.90*(0.81–1.00) | |
| Sex (ref: Female) | |||
| Male | 0.98(0.94–1.02) | 0.98(0.94–1.02) | |
| Education (ref: Less than high school) | |||
| High school | 0.89***(0.84–0.93) | 0.88***(0.84–0.93) | |
| Some college | 0.83***(0.78–0.89) | 0.83***(0.78–0.89) | |
| College or more | 0.70***(0.67–0.75) | 0.70***(0.66–0.74) | |
| Need factors | |||
| Health Status (ref: Good/Very good/Excellent) | |||
| Poor/Fair | 1.62***(1.55–1.70) | 1.62***(1.54–1.70) | |
| Medical conditions (ref: None) | |||
| One or more | 1.57***(1.50–1.64) | 1.57***(1.50–1.64) | |
| 12-month Doctor Visit (ref: No) | |||
| Yes | 1.53***(1.45–1.61) | 1.53***(1.46–1.61) | |
| 12-month Hospitalization (ref: No) | |||
| Yes | 7.00***(6.68–7.33) | 6.99***(6.68–7.33) | |
| Controls | |||
| Region (ref: Northeast) | |||
| Midwest | 1.01(0.94–1.10) | 1.02(0.94–1.10) | |
| South | 0.87***(0.81–0.93) | 0.87***(0.81–0.93) | |
| West | 0.86***(0.79–0.93) | 0.86***(0.79–0.93) | |
| Metropolitan Statistical Area (ref: No) | |||
| Yes | 1.00(0.94–1.06) | 1.00(0.94–1.06) | |
| Survey year (ref: Year 2000) | |||
| 2001 | 1.19***(1.11–1.29) | 1.20***(1.11–1.29) | |
| 2002 | 1.13***(1.03–1.23) | 1.13***(1.03–1.23) | |
| 2003 | 1.15***(1.06–1.25) | 1.15***(1.06–1.25) | |
| 2004 | 1.17***(1.06–1.29) | 1.17***(1.07–1.29) | |
| 2005 | 1.15***(1.06–1.25) | 1.15***(1.06–1.25) | |
| 2006 | 1.17***(1.07–1.27) | 1.17***(1.07–1.27) | |
| 2007 | 1.08*(0.99–1.18) | 1.08*(0.99–1.18) | |
| 2008 | 1.09*(1.00–1.20) | 1.10**(1.00–1.20) | |
Note 1: “FB-Citizens” indicates foreign-born citizens (i.e., naturalized), and USB stands for United States born citizens
Model 1: Unadjusted
Model 2: Adjusted for enabling, predisposing, and need factors
Model 3: Adjusted with citizenship by insurance status interaction
P<0.01
P<0.05
Covariates effects
The statistical effects of the Behavioral Model factors were largely in the expected directions. The enabling effects of higher income on healthcare access were reflected in lower ED use. Among the predisposing factors, being African American increased the odds of use relative to Whites, while older age (compared to young adults; 18–34 years) and higher education decreased the odds of use. It is worth noting that the bivariate positive association between age (especially older age) and ED use was reversed in the fully adjusted model particularly after accounting for need factors. All need factors were associated with higher use, but, not surprisingly, distinctly high odds ratios were registered among those reporting at least one hospital discharge in the 12-month preceding the interview.
Sensitivity Analysis
To ensure the validity of our findings and guard against the possibility that our results were sensitive to our operationalization of ED use, we modeled the outcome as a count indicator (i.e., reported number of ED visits). A series of Poisson regressions were fit to estimate the effects of the main predictor and covariates on ED use. Similar results (not shown) were found. Complementing bivariate results presented in Table 2, this extended the finding that non-citizens are less likely to use ED services and showed that they are also less likely to be repeat users relative to the USB.
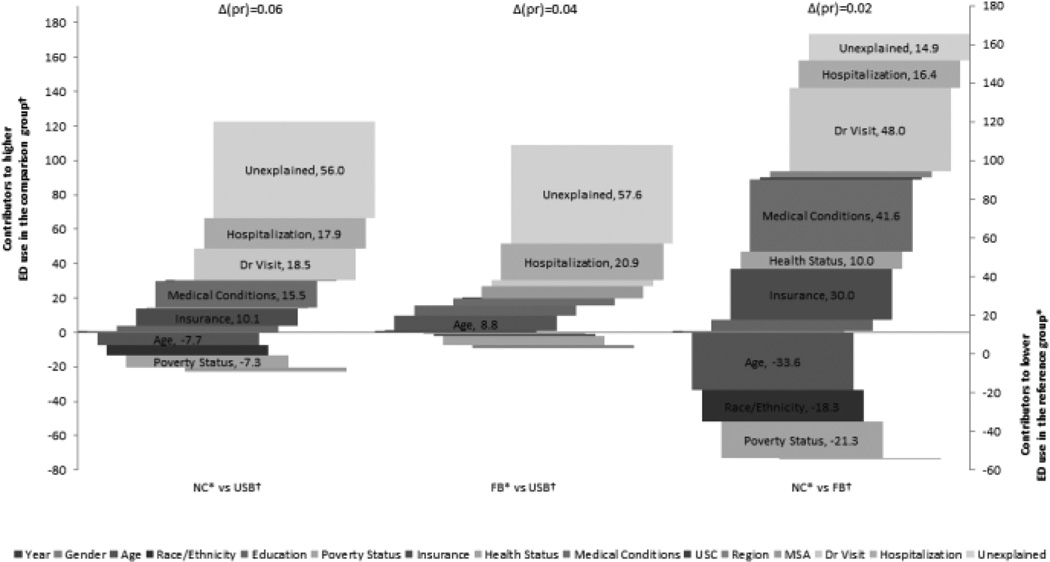
Explaining differences in probability of use
We found that less than half (44.0%) of the ED use probability differential (Δ(pr)=0.06) between the USB and non-citizen groups was explained by our model covariates (Figure 2). The highest contributors to the inflated use levels among the USB included reporting a doctor’s visit (18.5%), hospitalization (17.9%), medical conditions (15.5%), and insurance status (10.1%). Conversely, the younger age (7.7%) and higher poverty levels (7.3%) of the non-citizens group increased their probability of use relative to the USB by about 15%.
Figure 2.
Non-linear (Fairlie) decompositon of differences in expected probability of emergency department use between adult (18-years and older) citizenship groups in the United States. Results are from the Medical Expenditures Panel Survey (2000–2008).
Δ(pr) is the difference in the expectedprobability of use between the reference and comparison groups
† Comparison group
* Reference group
Note 1: “Non” indicates non-citizens, “FB” indicates foreign-born citizens and “USB” indicates US-born citizens.
Note 2: Only statistically significant factors are emphasized.
Note 3: Bars included in the negative quadrant of the graph represent factors that contribute to higher probability of use in the reference groups. Bars included in the positive quadrant of the graph represent factors that increase the probability of use among the comparison groups. The width of each included bar represents the percentage of between group difference in the probability (i.e. Δ(pr)) of reporting ED use explained by the factor or, more specifically, the expected change in difference if both groups had similar factor characteristics. The sum of the positive (including unexplained) and negative contributors add up to 100% of the difference between the compared groups.
The capacity of the model covariates in explaining the USB/FB-citizen use differential (Δ(pr)=0.04) was slightly higher than two-fifths (42.4%) of the evidenced difference (Figure 2). Hospitalization (21%), and age (8.8%) were the most salient contributors to the increase in use among the USB.
Lastly, our model covariates explained more than four-fifths (84.6%) of the difference in probability of use (Δ(pr)=0.02) between the FB groups (Figure 2). Our decomposition indicated that reporting a doctor’s visit (48%), medical conditions (41.6%), insurance status (30.0%), hospitalization (16.4%), and reported health status (10.0%) inflated the estimated levels of use among FB-citizens. Inversely, age (33.6%), poverty (21.3%), and the ethnic/racial (18.3%) structure of the non-citizen population inflated their probability of use relative to FB-citizens.
DISCUSSION
Two major findings emerged from this work. First, immigrants, particularly non-citizens, were less likely to use ED services compared to the US-born respondents, consistent over 9 years of study. Within the FB groups, naturalized immigrants were more likely to report ED use compared to non-citizens. Second, ED use differentials between groups were partially explained by Behavioral Model factors. Higher healthcare need and insurance coverage were the most salient determinants of higher ED use among citizens, both foreign and US-born, compared to non-citizens.
Given concerns about the capacity of the ED system for dealing with an enlarged number of both patients and responsibilities,20 this work provides evidence to presently dissociate higher ED use from the combined effects of immigration status and un-insurance.17 Non-citizen immigrants, especially the uninsured, have low level of ED use despite federal laws mandating service provision irrespective of insurance status and extending emergency Medicaid services when individuals are ineligible for full public coverage.36
Our results show that both naturalization and nativity are associated with gradually higher rates of ED use, and that healthcare needs partially explain ED use differences between groups. These findings provide support for both the “healthy migrant” and negative acculturation hypotheses.37 The foreign-born population is currently younger38 and healthier than the US-born.39 However, in coming decades immigrants, especially non-citizens, will age and form a larger share of the elderly population.1 As their age, acculturation, and healthcare need profiles change and their health advantages decline they will require more healthcare services.37 Immigrant neutral public health policies are needed to offset these trends. Therefore, federal restrictions aimed at undocumented and some legal immigrants in the early years following immigration as stipulated in the American Affordable Care Act (ACA),9,21,40 and scaled back federal and state initiatives, although politically necessary, could prove shortsighted. They can potentially increase patient burden and add unnecessary costs as a result of substandard preventive care, and inefficient healthcare services use, including at EDs.41,42
The interactive effects of citizenship status and insurance present more challenging findings. In particular, the notably lower probability of ED use among uninsured non-citizens, and the relatively equal probability clustering of the insured foreign-born irrespective of citizenship. We put forward two considerations to explain this. First, uninsured noncitizens possibly withhold use until care access enabling channels (e.g. insurance) or favorable immigration status change is secured. Legal status is a likely influence on immigrants’ decision of where, when, and for what to seek care.6,43–46 Despite the lack of longitudinal studies designed to specifically test for care delay and its association with immigration status change, regional studies47,48 and immigrant ethnic specific research consistently document higher healthcare services use in general, and ED use in particular, among citizens compared to non-citizens and undocumented individuals.6,44,49 Second, uninsured non-citizens delay use until they reach more acute, and likely resource intensive, levels of healthcare needs.43 Fear and misinformation can affect access to healthcare among uninsured non-citizens.50–53 Indeed, in a recent report the American College of Physicians calls for a national immigration policy on healthcare to prevent the consequences of these apprehensions,54 and acknowledges that they “can result in increased pain and suffering due to delay in treatment until patients are acutely ill, and ultimately places a greater burden on the health system.“p.13
We explained less than half of the differences in use between immigrants (both citizens and non-citizens) and the USB. Several possible contributors including patient preference, perception of need and case seriousness, convenience and timeliness of care, previous experience and trust in ED care providers, among other factors were not accounted for in our models.55–57 Future work should address the possible contribution of these factors, as well as the explicit role of fear and misinformation, in explaining differences among citizenship groups.
Policy solutions to increase healthcare efficiencies and reduce costs should facilitate rather than restrict more effective and prompt use of healthcare among immigrants. First, increase efforts, especially through workplace, churches, and schools, to target immigrants immediately following their arrival to the U.S. Use community resources and culturally appropriate channels to increase and instill awareness about correct healthcare habits. Second, reduce current barriers to healthcare access, including employer provided insurance and ability to participate in health insurance exchanges as stipulated by the ACA, enabling preventive and timely care and stemming the development of more complicated and expensive medical conditions. Third, focus on appropriate financing of health programs and investments that increase geographic availability and access to lower cost healthcare providers – especially, health centers, urgent care centers, and community clinics.58,59 These providers are equipped for providing good quality and timely preventive and non-acute medical care at lower costs,60 yet are less likely to service healthcare vulnerable populations.61
Concurrent policy solutions need to be devised to target all ED users, irrespective of citizenship status. However, results on intervention measures aimed at shifting ED use such as higher deductibles and copays, managed care, patient level care planning and case management, user follow-up and communication with primary care providers are inconclusive.32,62 Other methods such as more aggressive triage processes present ethical challenges.63 More research and better data is needed to understand the complexities and variations in patient ED use decision-making and the best mix of incentives that could alter it.
Several limitations to this work should be noted. First, we do not distinguish between urgent and non-urgent care. To our knowledge, no generalizable definitions of “urgency” (other than pain) exist,56 with previous work suggesting a low prevalence in cases were emergent care is not preventable or avoidable.64 Second, we were unable to control for the effects of some factors (e.g. users preferences and perceptions, convenience, trust) that have been shown to impact ED use.14,56 Third, neither the MEPS nor the NHIS include information on immigrants’ documentation status so we could not isolate the effects of legal residency on use patterns. Grouping non-citizens into a broad category can mask structural heterogeneity in legal, demographic, socioeconomic, and cultural status. It is especially important to indicate that undocumented immigrants face higher barriers to health insurance and healthcare access in the U.S. 6,9,40,45,46,65 Fourth, due to design adjustments by AHRQ, not all MEPS observations could be linked to NHIS immigration records. However, we found no statistically significant differences in ED use among the matched and unmatched groups, which is consistent with previous work.66 Finally, self-reported measures could be subject to recall and other exogenous individual biases, however, validation studies suggest favorable characteristics.67–70
CONCLUSION
Between 2000 and 2008, we found that immigrants, especially non-citizens, used ED at a lower level than the US-born. Immigrants, particularly uninsured non-citizens, do not currently present a disproportionate burden on the U.S. healthcare system. However, changes in immigrant group members’ demographic and healthcare need profiles and stringent limitations on access to healthcare might exert untoward pressures on the healthcare system capacity through increased dependence on EDs as a first choice and last resort for medical care.
Acknowledgments
Funding/Support: Drs. Tarraf and González are supported by the National Institutes of Health, NIMH (R01) MH 84994 and NHLBI HC 65233.
Role of Funding Source: This work was supported by the National Institutes of Health, National Institute of Mental Health, and the National Heart Lung Blood Institute. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Financial Disclosures: The authors report no conflicts of interest that could inappropriately influence this work.
REFERENCES
- 1.Passel JS, Cohn DV. U.S. Population Projections: 2005–2050. Washington, DC: Pew Research Center; 2008. Accessed from http://pewhispanic.org/files/reports/85.pdf on February, 17th 2011. [Google Scholar]
- 2.Kandula NR, Kersey M, Lurie N. Assuring the Health of Immigrants: What the Leading Health Indicators Tell Us. Annual Review of Public Health. 2004;25(1):357–376. doi: 10.1146/annurev.publhealth.25.101802.123107. [DOI] [PubMed] [Google Scholar]
- 3.Derose KP, Bahney BW, Lurie N, Escarce JJ. Immigrants and Health Care Access, Quality, and Cost. Medical Care Research and Review. 2009 doi: 10.1177/1077558708330425. [DOI] [PubMed] [Google Scholar]
- 4.Derose KP, Escarce JJ, Lurie N. Immigrants And Health Care: Sources Of Vulnerability. Health Affairs. 2007 Sep 1;26(5):1258–1268. doi: 10.1377/hlthaff.26.5.1258. 2007. [DOI] [PubMed] [Google Scholar]
- 5.Lee S, Choi S. Disparities in access to health care among non-citizens in the United States. Health Sociology Review. 2009;18(3):307–314. [Google Scholar]
- 6.Ortega AN, Fang H, Perez VH, et al. Health Care Access, Use of Services, and Experiences Among Undocumented Mexicans and Other Latinos. Arch Intern Med. 2007 Nov 26;167(21):2354–2360. doi: 10.1001/archinte.167.21.2354. 2007. [DOI] [PubMed] [Google Scholar]
- 7.Shah NS, Carrasquillo O. Twelve-Year Trends In Health Insurance Coverage Among Latinos, By Subgroup And Immigration Status. Health Affairs. 2006 Nov 1;25(6):1612–1619. doi: 10.1377/hlthaff.25.6.1612. 2006. [DOI] [PubMed] [Google Scholar]
- 8.Kullgren JT. Restrictions on Undocumented Immigrants' Access to Health Services: The Public Health Implications of Welfare Reform. Am J Public Health. 2003 Oct 1;93(10):1630–1633. doi: 10.2105/ajph.93.10.1630. 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaiser. Key Facts on Health Coverage for Low-Income Immigrants Today and Under Health Reform: Kaiser Family Foundation. Washington, DC: 2012. Accessed from: http://www.kff.org/uninsured/upload/8279.pdf on July, 2nd 2012. [Google Scholar]
- 10.Ku L. Health Insurance Coverage and Medical Expenditures of Immigrants and Native-Born Citizens in the United States. Am J Public Health. 2009 Jul 1;99(7):1322–1328. doi: 10.2105/AJPH.2008.144733. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vargas Bustamante A, Fang H, Garza J, et al. Variations in Healthcare Access and Utilization Among Mexican Immigrants: The Role of Documentation Status. Journal of Immigrant and Minority Health. 2010:1–10. doi: 10.1007/s10903-010-9406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldman DP, Smith JP, Sood N. Immigrants And The Cost Of Medical Care. Health Affairs. 2006 Nov 1;25(6):1700–1711. doi: 10.1377/hlthaff.25.6.1700. 2006. [DOI] [PubMed] [Google Scholar]
- 13.Pylypchuk Y, Hudson J. Immigrants and the use of preventive care in the United States. Health Economics. 2009;18(7):783–806. doi: 10.1002/hec.1401. [DOI] [PubMed] [Google Scholar]
- 14.Newton MF, Keirns CC, Cunningham R, Hayward RA, Stanley R. Uninsured Adults Presenting to US Emergency Departments. JAMA: The Journal of the American Medical Association. 2008 Oct 22/29;300(16):1914–1924. doi: 10.1001/jama.300.16.1914. 2008. [DOI] [PubMed] [Google Scholar]
- 15.Weissman JS. Delayed access to health care: risk factors, reasons, and consequences. Annals of internal medicine. 1991;114(4):325. doi: 10.7326/0003-4819-114-4-325. [DOI] [PubMed] [Google Scholar]
- 16.Chen J, Rizzo JA, Rodriguez HP. The Health Effects of Cost-Related Treatment Delays. American Journal of Medical Quality. 2011 Jul-Aug;26(4):261–271. doi: 10.1177/1062860610390352. 2011. [DOI] [PubMed] [Google Scholar]
- 17.Delia D. Emergency department utilization and capacity. The Synthesis project. Research synthesis report. 2009;(17) [PubMed] [Google Scholar]
- 18.GAO-09-347. Hospital emergency departments crowding continues to occur, and some patients wait longer than recommended time frames : report to the Chairman, Committee on Finance, U.S. Senate. 2009 http://purl.access.gpo.gov/GPO/LPS114578.
- 19.Kellermann AL. Crisis in the Emergency Department. New England Journal of Medicine. 2006;355(13):1300–1303. doi: 10.1056/NEJMp068194. [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine. Hospital-based emergency care at the breaking point. Washington, D.C.: National Academies Press; 2007. Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. [Google Scholar]
- 21.Fortuny K, Chaudry A. A comprehensive review of immigrant access to health and human services. Washington, DC: The Urban Insitute; 2011. [Google Scholar]
- 22.Andersen R, Newman JF. Societal and Individual Determinants of Medical Care Utilization in the United States. Milbank Quarterly. 2005;83(4):1–28. [PubMed] [Google Scholar]
- 23.Andersen RM. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? Journal of Health and Social behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 24.Agency for Healthcare Research and Quality. [Accessed May 31st, 2012];MEPS Link Files to NHIS. http://meps.ahrq.gov/mepsweb/data_stats/more_info_download_data_files.jsp#hc-nhis.
- 25.Agency for Healthcare Research and Quality. [Accessed May 31st, 2012];MEPS HC-036:1996–2009 Pooled Linkage Variance Estimation File. 2011 http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h36/h36u09doc.pdf.
- 26.Agency for Healthcare Research and Quality. [Accessed May 31st, 2012];MEPS-HC Response Rates by Panel. http://meps.ahrq.gov/mepsweb/survey_comp/hc_response_rate.jsp.
- 27.Rytina N. Estimates of the Legal Permanent Resident Population in 2009: Office of Immigration Statistics, Policy Directorate, U.S. Department of Homeland Security. 2010 Accessed from: http://www.dhs.gov/xlibrary/assets/statistics/publications/lpr_pe_2009.pdf on February, 17th 2011.
- 28.Baker BC. Estimates of the Resident Nonimmigrant Population in the United States: 2008: Office of Immigration Statistics, Policy Directorate, U.S. Department of Homeland Security. 2010 Accessed from: http://www.dhs.gov/xlibrary/assets/statistics/publications/ois_ni_pe_2008.pdf on January, 27th 2011.
- 29.Banthin J, Selden T. Income Measurement in the Medical Expenditure Panel Survey: Agency for Healthcare Research and Quality, Working Paper No. 06005. 2006 http://gold.ahrq.gov.
- 30.DeSalvo KB. Health Care Expenditure Prediction With a Single Item, Self-Rated Health Measure. Medical Care. 2009;47(4):440–447. doi: 10.1097/MLR.0b013e318190b716. [DOI] [PubMed] [Google Scholar]
- 31.Nawar EW, Niska RW, J X. Advance data from vital and health statistics; no. 386. Hyattsville, MD: National Center for Health Statistics; 2007. National Hospital Ambulatory Medical Care Survey: 2005 Emergency Department Summary. 2007. [PubMed] [Google Scholar]
- 32.LaCalle E, Rabin E. Frequent Users of Emergency Departments: The Myths, the Data, and the Policy Implications. Annals of Emergency Medicine. 2010;56(1):42–48. doi: 10.1016/j.annemergmed.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 33.Jann B. fairlie: Stata module to generate nonlinear decomposition of binary outcome differentials. 2006 Available from http://ideas.repec.org/c/boc/bocode/s456727.html.
- 34.Fairlie RW. An extension of the Blinder-Oaxaca decomposition technique to logit and probit models. Journal of Economic and Social Measurement. 2005;30(4):305–316. [Google Scholar]
- 35.Jann B. The Blinder-Oaxaca decomposition for linear regression models. Stata. 2008 May;8(4):453–479. 2008. [Google Scholar]
- 36.Ku L, Matani S. Left Out: Immigrants’ Access To Health Care And Insurance. Health Affairs. 2001 Jan 1;20(1):247–256. doi: 10.1377/hlthaff.20.1.247. 2001. [DOI] [PubMed] [Google Scholar]
- 37.Antecol H. Unhealthy Assimilation: Why Do Immigrants Converge to American Health Status Levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 38.US Census Bureau. Table 40 Native and Foreign-Born Populations by Selected Characteristics: 2010. U.S. Census Bureau, Statistical Abstract of the United States. 2012 Accessed from http://www.census.gov/compendia/statab/2012/tables/12s0040.pdf on Friday December 14th 2012.
- 39.Tarraf W, Miranda PY, González HM. Medical Expenditures Among Immigrant and Nonimmigrant Groups in the United States: Findings From the Medical Expenditures Panel Survey (2000–2008) Medical Care. 2012;50(3):233. doi: 10.1097/MLR.0b013e318241e5c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zuckerman S, Waidmann TA, Lawton E. Undocumented Immigrants, Left Out Of Health Reform, Likely To Continue To Grow As Share Of The Uninsured. Health Affairs. 2011 Oct 1;30(10):1997–2004. doi: 10.1377/hlthaff.2011.0604. 2011. [DOI] [PubMed] [Google Scholar]
- 41.Andrulis DP, Siddiqui NJ. Health Reform Holds Both Risks And Rewards For Safety-Net Providers And Racially And Ethnically Diverse Patients. Health Affairs. 2011 Oct 1;30(10):1830–1836. doi: 10.1377/hlthaff.2011.0661. 2011. [DOI] [PubMed] [Google Scholar]
- 42.Ortega A. And health care for all: immigrants in the shadow of the promise of universal health care. American journal of law & medicine. 2009;35(1):185–204. doi: 10.1177/009885880903500105. [DOI] [PubMed] [Google Scholar]
- 43.DuBard CA, Massing MW. Trends in Emergency Medicaid Expenditures for Recent and Undocumented Immigrants. JAMA: The Journal of the American Medical Association. 2007 Mar 14;297(10):1085–1092. doi: 10.1001/jama.297.10.1085. 2007. [DOI] [PubMed] [Google Scholar]
- 44.Vargas Bustamante A. Variations in Healthcare Access and Utilization Among Mexican Immigrants: The Role of Documentation Status. Journal of Immigrant and Minority Health. 2010 doi: 10.1007/s10903-010-9406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodríguez M, Vargas Bustamante A, Ang A. Perceived Quality of Care, Receipt of Preventive Care, and Usual Source of Health Care Among Undocumented and Other Latinos. Journal of General Internal Medicine. 2009;24(0):508–513. doi: 10.1007/s11606-009-1098-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nandi A, Galea S, Lopez G, Nandi V, Strongarone S, Ompad DC. Access to and Use of Health Services Among Undocumented Mexican Immigrants in a US Urban Area. Am J Public Health. 2008 Jan 2; doi: 10.2105/AJPH.2006.096222. 2008:AJPH.2006.096222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McConville S, Lee H. Emergency Department Care in California. Public Policy Institute of California. 2008 [Google Scholar]
- 48.Cunningham PJ. What Accounts For Differences In The Use Of Hospital Emergency Departments Across U.S Communities? Health Affairs. 2006 Sep 1;25(5):w324–w336. doi: 10.1377/hlthaff.25.w324. 2006. [DOI] [PubMed] [Google Scholar]
- 49.Chen J, Vargas-Bustamante A. Estimating the Effects of Immigration Status on Mental Health Care Utilizations in the United States. Journal of Immigrant and Minority Health. 2011;13(4):671–680. doi: 10.1007/s10903-011-9445-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Feld P, Power B. Immigrants' Access to Health Care After Welfare Reform: Findings from Focus Groups in Four Cities: Kaiser Family Foundation. Washington, DC: 2000. Accessed from: http://www.kff.org/uninsured/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=13375 on July, 2nd 2012. [Google Scholar]
- 51.Berk M, Schur C. The Effect of Fear on Access to Care Among Undocumented Latino Immigrants. Journal of Immigrant Health. 2001 Jul 01;3(3):151–156. doi: 10.1023/A:1011389105821. 2001. [DOI] [PubMed] [Google Scholar]
- 52.Berk ML, Schur CL, Chavez LR, Frankel M. Health care use among undocumented Latino immigrants. Health Affairs. 2000 Jul 1;19(4):51–64. doi: 10.1377/hlthaff.19.4.51. 2000. [DOI] [PubMed] [Google Scholar]
- 53.Kaushal N, Kaestner R. Welfare Reform and Health Insurance of Immigrants. Health Services Research. 2005;40(3):697–722. doi: 10.1111/j.1475-6773.2005.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.American College of Physicians. National Immigration Policy and Access to Health Care. Philadelphia: American College of Physicians; 2011. Policy Paper. Accessed from: http://www.acponline.org/advocacy/where_we_stand/policy/natl_immigration.pdf.2011. [Google Scholar]
- 55.Guttman N, Zimmerman DR, Nelson MS. The Many Faces of Access: Reasons for Medically Nonurgent Emergency Department Visits. Journal of Health Politics, Policy and Law. 2003 Dec;28(6):1089–1120. doi: 10.1215/03616878-28-6-1089. 2003. [DOI] [PubMed] [Google Scholar]
- 56.Afilalo J, Marinovich A, Afilalo M, et al. Nonurgent Emergency Department Patient Characteristics and Barriers to Primary Care. Academic Emergency Medicine. 2004;11(12):1302–1310. doi: 10.1197/j.aem.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 57.Penson R, Coleman P, Mason S, Nicholl J. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department? Emergency Medicine Journal. 2011 May 11; doi: 10.1136/emj.2010.107276. 2011. [DOI] [PubMed] [Google Scholar]
- 58.GAO-11-414R. Hospital Emergency Departments: Health Center Strategies That May Help Reduce Their Use. 2011 Accessed from http://www.gao.gov/assets/100/97416.pdf on March 13th, 2012.
- 59.Weinick RM, Burns RM, Mehrotra A. Many Emergency Department Visits Could Be Managed At Urgent Care Centers And Retail Clinics. Health Affairs. 2010 Sep 1;29(9):1630–1636. doi: 10.1377/hlthaff.2009.0748. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mehrotra A, Liu H, Adams JL, et al. Comparing Costs and Quality of Care at Retail Clinics With That of Other Medical Settings for 3 Common Illnesses. Annals of internal medicine. 2009 Sep 1;151(5):321–328. doi: 10.7326/0003-4819-151-5-200909010-00006. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pollack CE, Armstrong K. The Geographic Accessibility of Retail Clinics for Underserved Populations. Arch Intern Med. 2009 May 25;169(10):945–949. doi: 10.1001/archinternmed.2009.69. 2009. [DOI] [PubMed] [Google Scholar]
- 62.Wharam JF, Landon BE, Galbraith AA, Kleinman KP, Soumerai SB, Ross-Degnan D. Emergency Department Use and Subsequent Hospitalizations Among Members of a High-Deductible Health Plan. JAMA: The Journal of the American Medical Association. 2007 Mar 14;297(10):1093–1102. doi: 10.1001/jama.297.10.1093. 2007. [DOI] [PubMed] [Google Scholar]
- 63.Weinick RM, Zuvekas SH, Cohen JW. Racial and Ethnic Differences in Access to and Use of Health Care Services, 1977 to 1996. Medical Care Research and Review. 2000 Nov 1;57(suppl 1):36–54. doi: 10.1177/1077558700057001S03. 2000. [DOI] [PubMed] [Google Scholar]
- 64.Billings J. Emergency department use in New York City: a substitute for primary care? Issue brief (Commonwealth Fund) 2000;(433):1–5. [PubMed] [Google Scholar]
- 65.Goldman DP, Smith JP, Sood N. Legal Status And Health Insurance Among Immigrants. Health Affairs. 2005 Nov 1;24(6):1640–1653. doi: 10.1377/hlthaff.24.6.1640. 2005. [DOI] [PubMed] [Google Scholar]
- 66.Stimpson JP, Wilson FA, Eschbach K. Trends In Health Care Spending For Immigrants In The United States. Health Affairs. 2010;29(3):544–550. doi: 10.1377/hlthaff.2009.0400. [DOI] [PubMed] [Google Scholar]
- 67.Zuvekas SH, Olin GL. Validating Household Reports of Health Care Use in the Medical Expenditure Panel Survey. Health Services Research. 2009;44(5p1):1679–1700. doi: 10.1111/j.1475-6773.2009.00995.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zuvekas SH. The effects of recall length and reporting aids on household reporting of health care events in the medical expenditure panel survey. Journal of Economic and Social Measurement. 2011;36(4):321. [Google Scholar]
- 69.Zuvekas SH. Accuracy of Medicare Expenditures in the Medical Expenditure Panel Survey. Inquiry (Chicago) 2009;46(1):92–108. doi: 10.5034/inquiryjrnl_46.01.92. [DOI] [PubMed] [Google Scholar]
- 70.Hill SC. Implications of the Accuracy of MEPS Prescription Drug Data for Health Services Research. Inquiry (Chicago) 2011;48(3):242–259. doi: 10.5034/inquiryjrnl_48.03.04. [DOI] [PubMed] [Google Scholar]