Abstract
There is a rapidly growing body of animal and clinical evidence suggesting that the exposure to anesthetics and sedatives during critical stages of brain development results in long-lasting (perhaps permanent) impairment in cognitive development in a variety of mammalian species. With improved understanding of the mechanisms responsible for behavioral outcomes of anesthesia-induced developmental neurotoxicity there is hope for development of protective strategies that will enable safe use of anesthesia in the youngest members of our society. Here I review presently available evidence regarding anesthesia-induced neurocognitive and social behavioral impairments and possible strategies for preventing them. I also review limited and somewhat controversial evidence that examines the effects of nociception and surgical stimulation on anesthesia-induced developmental neurotoxicity.
Keywords: learning and memory, social behavior, anesthetics, neurotoxicity, neurodevelopment, immature brain
I. Introduction
Over the last decade mounting animal data and rapidly emerging clinical evidence suggest that the exposure to anesthetics and sedatives during critical stages of brain development (often referred to as synaptogenesis) results in long-lasting (perhaps permanent) impairment in cognitive development. These new findings are likely to have lasting impact on anesthesia and sedation practices in pediatrics. Although it is indisputable that a child's comfort during painful interventions is critically important, we now are focusing more on how to achieve a fine balance between providing anesthetic conditions that permit critical surgeries and procedures while avoiding serious, previously unknown neurotoxicities.
There is no controversy about the animal evidence showing that early exposure to clinically used general anesthetics leads to substantial neuronal injury and impairment in synaptogenesis in the neonatal brain, or about the fact that such injury is associated with long-term behavioral impairments [1–11]. However, the mechanisms for these effects and potential causality between morphological and functional outcomes remain to be established. The quest to understand the mechanisms responsible for neuronal damage has led to a flurry of studies and implication of a variety of cellular processes, such as extensive apoptotic activation [1–7], disturbances in organelle homeostasis (mitochondrial and endoplasmic reticuli in particular) [12–14], and alterations in cytoskeletal formation and function [15]. The hope is that better understanding of key factors that trigger widespread injury to the immature neurons and synapses will aid in devising protective strategies that can enable safe use of anesthesia in the youngest members of our society, with special emphasis on ameliorating anesthesia-induced impairments of behavioral development. Here I review presently available evidence regarding anesthesia-induced functional impairments and possible strategies for preventing them.
II. Early exposure to anesthesia and behavioral development in rodents
Initial work with rats exposed to general anesthesia (a cocktail containing a sedative dose of midazolam with nitrous oxide and isoflurane) at the peak of their brain development showed that their cognitive abilities in young adulthood lagged behind those of controls; the gap in learning abilities widened later in adulthood, as demonstrated by an inability to master more complicated learning paradigms [1]. Although isoflurane seems to be most detrimental [16] other volatile anesthetics such as desflurane [10] and sevoflurane [11] also have been shown to compromise cognitive development in rodents. In addition, there is mounting evidence that early exposure to the most commonly used intravenous anesthetics, propofol [17] and ketamine [6], leads to persistent learning deficits when animals are examined in young adulthood. For example, ketamine was shown to cause significant deficits in habituation, marked deficits in acquisition and retention of memory in the radial arm maze-learning task, as well as decreased shift learning in a circular swim maze-learning task [6]. Propofol was shown to impair explorative learning, as tested in the hole board test, more than spatial navigation, as estimated using the Morris water maze test [17].
In addition to the evidence of significant impairment in cognitive development, there is concern that early exposure to anesthesia may harm the development of social behavior. For example, studies of mice have shown that early exposure to intravenously administered general anesthetics in combination, but not singly, significantly alters the social behavior of the mice during young adulthood (postnatal days 55 to 70). Frederiksson et al. [6] have shown that mice exposed at postnatal day 10 to propofol or thiopental in combination with ketamine exhibited hypoactivity followed by distinct hyperactivity behavior and complete lack of habituation to the activity test chambers during a 60 min test period. More recent study by Satomoto et al., [11] has shown that exposure of neonatal mice (at post-natal day 6) to inhaled sevoflurane causes abnormal social behavior suggestive of autism spectrum disorder. For instance, they report that exposure of neonatal mice to clinically relevant concentration of sevoflurane caused impaired social memory and decreased interaction with a social target despite normal general interest in novelty or in olfactory sensation.
When anesthetic agents with γ-amino-butyric acid (GABA)ergic and N-methyl-D-aspartate (NMDA) antagonist properties are combined, which is done frequently in the clinical setting (for example, nitrous oxide and volatile anesthetics or propofol and ketamine), behavioral deficits, including cognitive ones, appear to be even more profound [1,6,7]. Coincidentally, the severity of behavioral deficits seems to correlate with the severity of neuronal damage since combined anesthetics have been shown to induce more profound neurotoxicity than the individual agents [1,6,7].
It is noteworthy that the initial study [1] and numerous others that followed over the ensuing decade [2,6,7,9–11,13] were focused mainly on the effects of anesthesia in the absence of painful and/or surgical stimulation on subsequent development of behavioral responses. Although there are many instances in clinical practice when anesthesia is administered in the absence of a painful stimulus (e.g. imaging studies such as MRI and CT scanning), substantially more anesthesia exposures during early stages of human brain development are performed to permit painful interventions. Thus, anesthesia-induced impairment of subsequent behavioral responses also must be examined under surgical conditions. Based on a recent report by Shu et al. [18], it appears that surgical incision and nociception induced by formalin injection worsen cognitive impairment caused by combined nitrous oxide/isoflurane anesthesia when examined in 7-day old rat pups and compared to anesthesia without painful stimuli. When pathomorphological outcomes were assessed, it was discovered that nociceptive stimulation with formalin or surgical incision increased the injury in the brain cortex. In contrast, Liu et al. [19] reported that noxious peripheral stimulation with complete Freund's adjuvant resulted in an attenuated neurotoxic response to ketamine in postnatal day 7 rat pups. However, the functional implications of this finding were not investigated.
A third study which assessed the role of nociception in anesthesia-induced cognitive development reported that sevoflurane anesthesia produced comparable impairment in neurocognitive functioning whether administered with or without a painful stimulus and tissue injury (tail pinch) [30]. These conflicting studies indicate a need for additional investigation into the conditions under which painful stimuli may or may not exacerbate impairments caused by application of anesthesia during synaptogenesis.
Considering that general anesthetics are often a necessity when a child's well being is in jeopardy, protection from anesthesia-induced developmental neurotoxicity is an important issue. Several protocols have been described in which concomitant administration of protective agents such as melatonin [20], L-carnitine [21], β estradiol [22], and dexmedetomidine [23] was noted to offer protection against neuronal injury. Although the reports regarding the beneficial effects of these protective agents on cognitive behavior are scarce, some promising clues are beginning to emerge. Recently published evidence indicates that anesthesia impairs morphogenesis and function of mitochondria in developing neurons, suggesting that strategies aimed at protecting mitochondria and curtailing oxygen free radical production may offer beneficial effects [13]. For example, oxygen free radical up-regulation was curtailed and outcomes of acute oxidative stress such as lipid peroxidation and neuronal deletion were abated when anesthesia administration was accompanied by administration of EUK-134, a synthetic oxygen free radical scavenger having both Mn-superoxide dismutase (SOD) and catalase activity [24,25], or R(+) pramipexole [R(+) PPX], a synthetic aminobenzothiazol derivative that blocks permeability transition pores, restores the integrity of mitochondrial membranes [26] and limits production of reactive oxygen species (ROS) [27–29]. Most importantly, these preventive strategies led to complete abolishment of anesthesia-induced cognitive impairments [13]. These results suggest that protection of mitochondria may be a strategy for prevention of developmental neurotoxicity when anesthesia is used during critical stages of brain development.
Another interesting possibility for treatment rather than prevention of anesthesia-induced cognitive decline involves the behavioral strategies referred to as `delayed environmental enrichment'. Stratmann and colleagues [30] examined the value of nonspecific but powerful environmental enrichment in young adolescent animals (4 weeks of age) that previously were exposed to general anesthesia during a critical period of their brain development (7 days of age). They discovered that the anesthesia-treated rats that were exposed to a home environment that provided voluntary exercise, environmental complexity and social interaction with a group of rats showed clear signs of rescued memory function when compared to anesthesia-treated rats that were exposed to a standard home cage environment. They suggest that “environmental enrichment, including voluntary exercise, might be a potential therapeutic strategy, in case long-term cognitive impairment caused by anesthesia in infancy occurs in humans.”
III. Early exposure to anesthesia and behavioral consequences in non-human primates
Behavioral studies in rodents have provided important support for the effects of anesthesia on cognitive development; however the relevance of rodent behavioral findings to human clinical settings remains to be determined. Due to the numerous ethical and medical considerations that limit randomized prospective trials in very young children, the importance of well designed behavioral studies with non-human primates cannot be overemphasized. Recently, Paule and colleagues [31] have addressed long-standing questions regarding the effects of anesthesia during the early period of brain development on the cognitive development of nonhuman primates. They demonstrated that the use of continuous low dose ketamine infusion to maintain a light surgical plane of general anesthesia during a critical period of brain development in rhesus monkeys (120 to 123 days in-utero), resulted in significant and long-lasting cognitive impairment compared with unexposed monkeys. They used the Operant Test Battery designed to assess learning, motivation, color discrimination, and short-term memory, and found that ketamine-treated monkeys demonstrate lower training scores starting at about 10 months of postnatal age and lasting beyond 3 years of age. The impairments were noted not only in accuracy of task performance, but in response speed as well. The authors report lower motivation in the ketamine-treated group, which could account for some aspects of their impaired cognitive performance. However, this qualification does not lessen apprehension regarding the long-term and possibly permanent effects of anesthesia on cognitive development and normal functioning after only a single exposure during the critical period of synaptogenesis. Of particular concern is the fact that concept formation, one of the most important cognitive functions, was most vulnerable. In view of the fact that monkey performance on the Operant Test Battery is quite similar to that of humans [32], it is reasonable to propose that early exposure to general anesthesia also may cause long-lasting impairment in children's cognitive development. Careful randomized prospective clinical trials are warranted.
IV. Early exposure to anesthesia and behavioral consequences in humans
Although some earlier studies suggested the possibility that early exposure to anesthesia may have lasting effects on psychological and emotional development of children, the major impetus for methodical investigations into the possibility of anesthesia-induced neurotoxicity in newborns and infants came from several early preclinical studies [1,6,7] that clearly implicated anesthetic agents in a variety of behavioral disturbances indicative of impaired neurocognitive development. Previous assumptions had held that the main factors in children's regressive behavioral changes after surgery were the emotional shocks of hospitalization and separation from family, and the physical traumas of surgical intervention, such as pain, fluid imbalance, nutritional changes, and blood loss. These assumptions now are being challenged.
Although investigations are still at an early stage, the clinical evidence that has emerged over the last few years has begun to point to potentially detrimental effects of anesthetic agents on cognitive development. In a population-based retrospective birth-cohort study of 5,357 children, Wilder et al. [33] found that although a single exposure to general anesthesia was not associated with a greater risk of learning disabilities, children who were exposed to general anesthesia two or more times before the age of 4 years were at significantly increased risk of learning disabilities compared with unexposed children. Moreover, that risk increased with longer cumulative duration (more than 2 hours) of anesthesia exposure. Of particular concern is their finding that the cohort exposed to anesthesia before the age of 4 years had cognitive scores over their years of schooling that were, on average, two standard deviations below the predicted ones based on the individual assessment of their cognitive ability, i.e. IQ scores. This result suggests that early exposure to general anesthesia prevented these individuals from reaching their full cognitive potential.
In an even larger population study, Sun et al. [34] focused on assessing learning disabilities in 228,961 patients. They reported that children who had received anesthesia before the age of 3 years required higher use of Medicaid services to deal with learning deficits than did children who had not been exposed to anesthesia.
Several studies of premature infants have suggested that behavioral disabilities later in life are more prevalent among those who were exposed to surgery and general anesthesia during the neonatal period than they are among premature infants who were treated medically. For example, surgically treated premature infants with patent ductus arteriosus [35] or necrotizing enterocolitis [36] had worse neurological outcomes than did premature infants who were treated medically. Although a possible causal link between early exposure to general anesthesia and neurocognitive deficits could be suggested on the basis of these studies, a measure of caution is advisable since the effects of surgery cannot be separated clearly from the effects of anesthesia.
Some newer retrospective evidence points toward a clear negative correlation between the duration of anesthesia exposure and scores on academic achievement tests, i.e. the longer the duration of anesthesia, the lower the scores [37]. Although the authors caution that there may be other explanations, it is of concern that they report a significantly higher percentage of otherwise healthy Iowa children performing below the 5th percentile on academic achievement tests in the groups exposed to anesthesia at a very young age (about 12–14%) when compared to the Iowa population as a whole (about 5%).
Another recent report from the Mayo clinic suggests that early exposure to anesthesia may result in higher incidence of attention deficit/hyperactivity disorder. Sprung and colleagues [38] report that, after adjustment for co-morbidities, children who underwent multiple (two or more), but not a single exposure to anesthesia, had a significantly higher risk of developing hyperactivity problems when anesthesia exposure occurred before the age of 2 years.
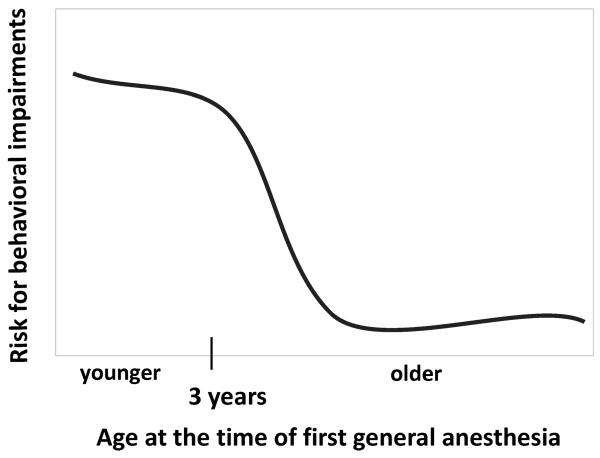
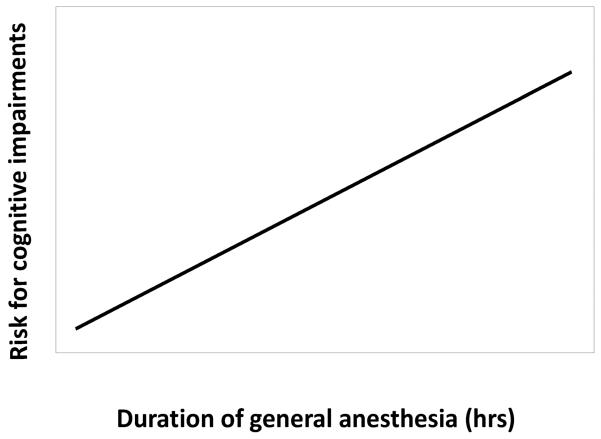
Taken together presently available clinical evidence suggests that children younger than 3 years of age are particularly vulnerable to general anesthesia since there seems to be higher risk for them to develop a variety of behavioral impairments compared to children older than 3 years at the time of first exposure (Figure 1). Furthermore, there appears to be a direct correlation between the duration of exposure to general anesthesia and the risk for developing cognitive impairments, i.e. longer the exposure, more likely it is that the child will exhibit some form of learning disability later in life (Figure 2).
Figure 1. Schematic representation of the relative risk for the development of behavioral impairments and the age of children at the time of first exposure to general anesthesia.
It suggests that children younger than 3 years of age are particularly vulnerable to general anesthesia since they are at higher risk to develop a variety of behavioral impairments compared to children older than 3 years of age.
Figure 2. Schematic representation of the relative risk for cognitive impairments in children and the duration of exposure to general anesthesia.
It suggests direct correlation, i.e. longer the exposure, higher the risk for learning disabilities.
Presently available information that stratifies children based on a mode of delivery (Cesarean section vs. vaginally) suggests that the risk for learning disabilities were higher among children born vaginally compared to the ones born by Cesarean section under regional anesthesia. Interestingly, there was no significant difference in the risk for cognitive impairments between children born by Cesarean section under general or regional (neuroaxial) anesthesia suggesting that brief perinatal exposure to general anesthetics may not have adverse effect on cognitive development [39].
Although, to date, these few clinical studies suggest that the exposure of infants and neonates to surgery and general anesthetics may cause significant neurocognitive deficits and a variety of behavioral sequellae, all of these studies were done retrospectively and therefore could not control for the many variables that come into play during the perioperative period. The complex issues associated with the design of randomized, double-blinded prospective clinical studies of very young patients cannot be underestimated. These issues include, but are not limited to, ethical considerations; the lack of biomarkers of apoptosis that can be used safely in a living organism; the complexity and meaningfulness of various clinical outcomes, especially neurocognitive ones; and the lack of appropriate controls.
V. Conclusion
Based on presently available evidence, it is becoming clear that regressive behavioral changes in children exposed to general anesthesia are most common in those exposed before the age of 4 years, which coincides with the time period of rapid brain development in humans. A causal relationship between a specific anesthesia protocol and specific cognitive disturbances has not been reported, suggesting that the majority of commonly used general anesthetics could be detrimental.
In view of this rapidly emerging information, it is of paramount importance to better understand the etiology of poor neurocognitive outcomes that may be anesthesia-induced so that prevention strategies can be developed. Only then can we feel confident that existing anesthetics can be used to their full advantage for therapeutic benefits without the risk of neurotoxic side effects, especially in cases when life-threatening conditions make frequent surgical interventions and prolonged stays in intensive units necessary for a child's survival.
Acknowledgments
This work was supported by NIH/NICHD HD 44517 (to V.J-T.), John E. Fogarty Award TW007423-128322 (to P.I. V.J-T.), ARRA supplement NIH/NICHD HD 44517 (to V. J-T.), March of Dimes National Award (to V.J-T.) and Harold Carron endowment (to V.J-T). V.J-T. was an Established Investigator of the American Heart Association.
References
- 1.Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876–882. doi: 10.1523/JNEUROSCI.23-03-00876.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loepke AW, Istaphanous GK, McAuliffe JJ, 3rd, et al. The effects of neonatal isoflurane exposure in mice on brain cell viability, adult behavior, learning, and memory. Anesth Analg. 2009;108:90–104. doi: 10.1213/ane.0b013e31818cdb29. [DOI] [PubMed] [Google Scholar]
- 3.Young C, Jevtovic-Todorovic V, Qin YQ, et al. Potential of ketamine and midazolam, individually or in combination, to induce apoptotic neurodegeneration in the infant mouse brain. Br J Pharmacol. 2005;146:189–97. doi: 10.1038/sj.bjp.0706301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rizzi S, Carter LB, Ori C, Jevtovic-Todorovic V. Clinical anesthesia causes permanent damage to the fetal guinea pig brain. Brain Pathol. 2008;18:198–210. doi: 10.1111/j.1750-3639.2007.00116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slikker W, Jr, Zou X, Hotchkiss CE, et al. Ketamine-induced neuronal cell death in the perinatal rhesus monkey. Toxicol Sci. 2007;98:145–58. doi: 10.1093/toxsci/kfm084. [DOI] [PubMed] [Google Scholar]
- 6.Fredriksson A, Pontén E, Gordh T, Eriksson P. Neonatal exposure to a combination of N-methyl-D-aspartate and gamma-aminobutyric acid type A receptor anesthetic agents potentiates apoptotic neurodegeneration and persistent behavioral deficits. Anesthesiology. 2007;107:427–36. doi: 10.1097/01.anes.0000278892.62305.9c. [DOI] [PubMed] [Google Scholar]
- 7.Fredriksson A, Archer T, Alm H, et al. Neurofunctional deficits and potentiated apoptosis by neonatal NMDA antagonist administration. Behav Brain Res. 2004;153:367–76. doi: 10.1016/j.bbr.2003.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Pesic V, Milanovic D, Tanic N, et al. Potential mechanism of cell death in the developing rat brain induced by propofol anesthesia. Int J Dev Neurosci. 2009;27:279–87. doi: 10.1016/j.ijdevneu.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Viberg H, Pontén E, Eriksson P, et al. Neonatal ketamine exposure results in changes in biochemical substrates of neuronal growth and synaptogenesis, and alters adult behavior irreversibly. Toxicology. 2008;49:153–9. doi: 10.1016/j.tox.2008.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Kodama M, Satoh Y, Otsubo Y, Araki Y, Yonamine R, Masui K, Kazama T. Neonatal desflurane exposure induces more robust neuroapoptosis than do isoflurane and sevoflurane and impairs working memory. Anesthesiology. 2011;115:979–91. doi: 10.1097/ALN.0b013e318234228b. [DOI] [PubMed] [Google Scholar]
- 11.Satomoto M, Satoh Y, Terui K, Miyao H, Takishima K, Ito M, Imaki J. Neonatal exposure to sevoflurane induces abnormal social behaviors and deficits in fear conditioning in mice. Anesthesiology. 2009;110:628–37. doi: 10.1097/ALN.0b013e3181974fa2. [DOI] [PubMed] [Google Scholar]
- 12.Sanchez V, Feinstein SD, Lunardi N, Joksovic PM, Boscolo A, Todorovic SM, Jevtovic-Todorovic V. General Anesthesia Causes Long-term Impairment of Mitochondrial Morphogenesis and Synaptic Transmission in Developing Rat Brain. Anesthesiology. 2011;115:992–1002. doi: 10.1097/ALN.0b013e3182303a63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boscolo A, Starr JA, Sanchez V, Lunardi N, Digruccio MR, Ori C, Erisir A, Trimmer P, Bennett J, Jevtovic-Todorovic V. The abolishment of anesthesia-induced cognitive impairment by timely protection of mitochondria in the developing rat brain: The importance of free oxygen radicals and mitochondrial integrity. Neurobiol Dis. 2012;45:1031–41. doi: 10.1016/j.nbd.2011.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao Y, Liang G, Chen Q, Joseph DJ, Meng Q, Eckenhoff RG, Eckenhoff MF, Wei H. Anesthetic-induced neurodegeneration mediated via inositol 1,4,5-trisphosphate receptors. J Pharmacol Exp Ther. 2010;333:14–22. doi: 10.1124/jpet.109.161562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lemkuil BP, Head BP, Pearn ML, et al. Isoflurane neurotoxicity is mediated by p75NTR-RhoA activation and actin depolymerization. Anesthesiology. 2011;114:49–57. doi: 10.1097/ALN.0b013e318201dcb3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liang G, Ward C, Peng J, Zhao Y, Huang B, Wei H. Isoflurane causes greater neurodegeneration than an equivalent exposure of sevoflurane in the developing brain of neonatal mice. Anesthesiology. 2010;112:1325–34. doi: 10.1097/ALN.0b013e3181d94da5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bercker S, Bert B, Bittigau P, Felderhoff-Müser U, Bührer C, Ikonomidou C, Weise M, Kaisers UX, Kerner T. Neurodegeneration in newborn rats following propofol and sevoflurane anesthesia. Neurotox Res. 2009;16:140–7. doi: 10.1007/s12640-009-9063-8. [DOI] [PubMed] [Google Scholar]
- 18.Shu Y, Zhou Z, Wan Y, Sanders RD, Li M, Pac-Soo CK, Maze M, Ma D. Nociceptive stimuli enhance anesthetic-induced neuroapoptosis in the rat developing brain. Neurobiol Dis. 2012;45:743–50. doi: 10.1016/j.nbd.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 19.Liu JR, Liu Q, Li J, Baek C, Han XH, Athiraman U, Soriano SG. Noxious stimulation attenuates ketamine-induced neuroapoptosis in the developing rat brain. Anesthesiology. 2012;117:64–71. doi: 10.1097/ALN.0b013e31825ae693. [DOI] [PubMed] [Google Scholar]
- 20.Yon J-H, Carter LB, Reiter RJ, Jevtovic-Todorovic V. Melatonin reduces the severity of anesthesia-induced apoptotic neurodegeneration in the developing rat brain. Neurobiol Dis. 2006;21:522–530. doi: 10.1016/j.nbd.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Zou X, Sadovova N, Patterson TA, Divine RL, Hotchkiss CE, Ali SF, Hanig JP, Paule MG, Slikker W, Jr, Wang C. The effects of L-carnitine on the combination of, inhalation anesthetic-induced developmental, neuronal apoptosis in the rat frontal cortex. Neuroscience. 2008;151:1053–1065. doi: 10.1016/j.neuroscience.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 22.Lu LX, Yon J-H, Carter LB, Jevtovic-Todorovic V. General anesthesia activates BDNF-dependent neuroapoptosis in the developing rat brain. Apoptosis. 2006;11:1603–15. doi: 10.1007/s10495-006-8762-3. [DOI] [PubMed] [Google Scholar]
- 23.Sanders RD, Xu J, Shu Y, Januszewski A, Halder S, Fidalgo A, Sun P, Hossain M, Ma D, Maze M. Dexmedetomidine attenuates isoflurane-induced neurocognitive impairment in neonatal rats. Anesthesiology. 2009;110:1077–85. doi: 10.1097/ALN.0b013e31819daedd. [DOI] [PubMed] [Google Scholar]
- 24.Liu R, Liu IY, Bi X, Thompson RF, Doctrow SR, Malfroy B, Baudry M. Reversal of age-related learning deficits and brain oxidative stress in mice with superoxide dismutase/catalase mimetics. Proc Natl Acad Sci U S A. 2003;100:8526–31. doi: 10.1073/pnas.1332809100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baker K, Marcus CB, Huffman K, Kruk H, Malfroy B, Doctrow SR. Synthetic combined superoxide dismutase/catalase mimetics are protective as a delayed treatment in a rat stroke model: a key role for reactive oxygen species in ischemic brain injury. J Pharmacol Exp Ther. 1998;284:215–21. [PubMed] [Google Scholar]
- 26.Sayeed I, Parvez S, Winkler-Stuck K, Seitz G, Trieu I, Wallesch CW, Schönfeld P, Siemen D. Patch clamp reveals powerful blockade of the mitochondrial permeability transition pore by the D2-receptor agonist pramipexole. FASEB J. 2006;20:556–8. doi: 10.1096/fj.05-4748fje. [DOI] [PubMed] [Google Scholar]
- 27.Cassarino DS, Fall CP, Smith TS, Bennett JP., Jr Pramipexole reduces reactive oxygen species production in vivo and in vitro and inhibits the mitochondrial permeability transition produced by the parkinsonian neurotoxin methylpyridinium ion. J. Neurochem. 1998;71:295–301. doi: 10.1046/j.1471-4159.1998.71010295.x. [DOI] [PubMed] [Google Scholar]
- 28.Le WD, Jankovic J, Xie W, Appel SH. Antioxidant property of pramipexole independent of dopamine receptor activation in neuroprotection. J Neural Transm. 2000;107:1165–73. doi: 10.1007/s007020070030. [DOI] [PubMed] [Google Scholar]
- 29.Zou L, Xu J, Jankovic J, He Y, Appel SH, Le W. Pramipexole inhibits lipid peroxidation and reduces injury in the substantia nigra induced by the dopaminergic neurotoxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine in C57BL/6 mice. Neurosci Lett. 2000;281:167–70. doi: 10.1016/s0304-3940(00)00853-3. [DOI] [PubMed] [Google Scholar]
- 30.Shih J, May LD, Gonzalez HE, Lee EW, Alvi RS, Sall JW, Rau V, Bickler PE, Lalchandani GR, Yusupova M, Woodward E, Kang H, Wilk AJ, Carlston CM, Mendoza MV, Guggenheim JN, Schaefer M, Rowe AM, Stratmann G. Delayed environmental enrichment reverses sevoflurane-induced memory impairment in rats. Anesthesiology. 2012;116:586–602. doi: 10.1097/ALN.0b013e318247564d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paule MG, Li M, Allen RR, Liu F, Zou X, Hotchkiss C, Hanig JP, Patterson TA, Slikker W, Jr, Wang C. Ketamine anesthesia during the first week of life can cause long-lasting cognitive deficits in rhesus monkeys. Neurotoxicol Teratol. 2011;33:220–30. doi: 10.1016/j.ntt.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paule MG, Chelonis JJ, Buffalo EA, et al. Operant test battery performance in children: correlation with IQ. Neurotoxicol Teratol. 1999;21:223–30. doi: 10.1016/s0892-0362(98)00045-2. [DOI] [PubMed] [Google Scholar]
- 33.Wilder RT, Flick RP, Sprung J, et al. Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology. 2009;110:796–804. doi: 10.1097/01.anes.0000344728.34332.5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sun LS, Li G, Dimaggio C, et al. Anesthesia and neurodevelopment in children: time for an answer? Anesthesiology. 2008;109:757–61. doi: 10.1097/ALN.0b013e31818a37fd. [DOI] [PubMed] [Google Scholar]
- 35.Chorne N, Leonard C, Piecuch R, Clyman RI. Patent ductus arteriosus and its treatment as risk factors for neonatal and neurodevelopmental morbidity. Pediatrics. 2007;119:1165–1174. doi: 10.1542/peds.2006-3124. [DOI] [PubMed] [Google Scholar]
- 36.Hintz SR, Kendrick DE, Stoll BJ, et al. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics. 2005;115:696–703. doi: 10.1542/peds.2004-0569. [DOI] [PubMed] [Google Scholar]
- 37.Block RI, Thomas JJ, Bayman EO, Choi JY, Kimble KK, Todd MM. Are anesthesia and surgery during infancy associated with altered academic performance during childhood? Anesthesiology. 2012;117:494–503. doi: 10.1097/ALN.0b013e3182644684. [DOI] [PubMed] [Google Scholar]
- 38.Sprung J, Flick RP, Katusic SK, Colligan RC, Barbaresi WJ, Bojanić K, Welch TL, Olson MD, Hanson AC, Schroeder DR, Wilder RT, Warner DO. Attention-deficit/hyperactivity disorder after early exposure to procedures requiring general anesthesia. Mayo Clin Proc. 2012;87:120–9. doi: 10.1016/j.mayocp.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sprung J, Flick RP, Wilder RT, Katusic SK, Pike TL, Dingli M, Gleich SJ, Schroeder DR, Barbaresi WJ, Hanson AC, Warner DO. Anesthesia for cesarean delivery and learning disabilities in a population-based birth cohort. Anesthesiology. 2009;111:302–10. doi: 10.1097/ALN.0b013e3181adf481. [DOI] [PMC free article] [PubMed] [Google Scholar]