Abstract
Purpose
This study evaluates acetabular cup position in the setting of revision total hip arthroplasty (THA) with severe acetabular bone defects.
Methods
With a definition of safe zone of abduction (30–50°) and anteversion (5–25°), acetabular cup position was measured by a digital image analysis program for 34 patients with Paprosky type III acetabular bone defects.
Results
There were 24 cups (71 %) for abduction and 26 cups (76 %) for anteversion located in the safe zone. Nineteen cups (56 %) were within the safe zone for both abduction and anteversion. There was no dislocation, however one cup out of the safe zone resulted in early cup failure due to aseptic loosening.
Conclusions
The acetabular cup positioning in patients with Paprosky type III defects was 'optimal' in half of the cases. The prevalence of optimal acetabular cup position was similar to those reported in primary THA, suggesting that the presence of a large acetabular bone defect may not be a significant risk factor for suboptimal acetabular cup positioning in the setting of revision THA.
Keywords: Total hip arthroplasty, Revision, Acetabular bone defect, Paprosky type III, Cup position, Martell technique
Introduction
Optimal cup positioning is a fundamental requirement for satisfactory results of total hip arthroplasty (THA). Malposition of the acetabular cup can cause impingement, eccentric polyethylene wear and osteolysis, migration of acetabular component and dislocation of the joint, resulting in early failure of THA [1, 2].
In most primary or revision THA, the acetabular cup is supposed to be set in the “safe zone” of 30–50° of abduction and 5–25° of anteversion [3] although the definition of safe zone remains controversial [4]. However, optimal component position is sometimes difficult to obtain. Especially in situations of revision with significant bone defect, it may be more difficult to place the acetabular cup in an ideal position. Paprosky et al. [5] described a classification system for acetabular defects which differentiates defects based on the acetabular bone loss and inherent stability of the trial component. In Paprosky type III acetabular defect which involves an unsupportive acetabular rim, it may be even more important to achieve optimal cup positioning as the bony defect provides insufficient implant stability.
Recently, the prevalence of ‘optimal’ acetabular cup positioning in primary THA in a tertiary teaching hospital was reported to be 49 % [6]. The study reported that surgical approach, surgeon case numbers and obesity independently predicted malpositioned cups. While there are a number of papers describing clinical results of acetabular revision with large bone defect [7, 8], there is paucity of data regarding cup position in the setting of revision THA [6]. The purpose of this study was to evaluate the cup position in the setting of revision THA for Paprosky type III acetabular defect using the Martell digital image analysis technique.
Materials and methods
A retrospective institutional database search identified 288 acetabular revisions from 1997 to 2007. Of these 288 acetabular revisions, 44 hips (44 patients) were classified as Paprosky type III acetabular bone defects through preoperative radiographs. In order to ensure a valid comparison with the recent study reporting the prevalence of cup position in primary THA, the digital radiographs were evaluated using the Martell Hip Analysis Suite™ (HAS, Chicago, IL, USA) program [9] which provided accurate and reliable data for all radiographic measurements. Of the 44 patients, 34 were available for radiographs of sufficient digital quality to obtain digital image analysis and be included in this study.
There were 20 men and 14 women and the mean age at the time of revision surgery was 65 years (range 31–82 years). There were 19 left hips and 15 right hips. The diagnoses for the primary THA were osteoarthritis (n = 18), post-traumatic arthritis (n = 4), fractures (n = 3), Legg-Calvé-Perthes disease (n = 2), avascular necrosis (n = 2), unknown (n = 3) and others (n = 2). The mean time from the immediate prior hip surgery (primary or revision THA) to the acetabular revision was 15 years (range one to 29 years). The reasons for revision surgery were aseptic loosening of the acetabular component (n = 24), osteolysis (n = 6), instability (n = 3) and protrusio acetabuli (n = 1); 15 patients required only acetabular reconstruction and 19 patients required revision for both acetabular and femoral sides. Of 34 Paprosky type III defects, 22 patients were Paprosky type IIIA and 12 patients were Paprosky type IIIB.
Various treatment options exist in the face of significant bone loss of acetabular revision, including structural allograft [10], porous metal cup with/without augments [7], impaction allografting with a cemented shell [11], anti-protrusio cages [12], jumbo shells [13], oblong shells [8] and proximal and medial reconstructions [14]. In this study, the decision on the treatment option for surgical reconstruction was made by each surgeon independently. Seventeen patients were treated with a jumbo cup as defined by Whaley et al. [15] and five patients were treated with impaction bone graft and a cemented cup. One patient was treated with high placement of the acetabular component without cement as described by Dearborn and Harris [16] and another patient was treated with a cage and cup reconstruction. The remaining ten patients were treated with porous (n = 6) or non-porous (n = 4) metal acetabular shells that were smaller diameter than those included in the jumbo cup criteria. Each surgeon in this series independently selected a method of operative technique and these techniques have not changed during the study period. All 34 patients received allogenic chip bone graft for the acetabular reconstruction. The average volume of allograft was 81 ml (range 30–270 ml). In addition to bone grafting, on average three (range zero to seven) screws were used for cup fixation. In seven patients screws were not used for cup fixation (Table 1).
Table 1.
Data of angle measurement and follow-up results
| Cup position | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case number | Sex | Age at surgery | Type of defects | Allograft (ml) | Cup size (mm) | Number of screws | Abduction (°) | Version (°) | F/U (years) | Complications | F/U results |
| 1 | M | 55 | IIIB | 270 | 64 | 0 | 45.17 | 13.36 | 9.4 | ||
| 2 | M | 80 | IIIA | 90 | 66 | 3 | 31.64 | 11.07 | 3.2 | ||
| 3 | F | 62 | IIIB | 180 | 58 | 0 | 36.93 | 17.56 | 4.2 | ||
| 4 | F | 31 | IIIA | 45 | 60 | 0 | 45.65 | 2.25 | 9.7 | ||
| 5 | M | 65 | IIIB | 45 | 60 | 0 | 55.74 | 17.16 | 7.3 | ||
| 6 | M | 82 | IIIB | 45 | 56 | 0 | 44.50 | 12.39 | 6.7 | ||
| 7 | M | 33 | IIIA | 180 | 64 | 2 | 50.54 | 6.80 | 6.6 | ||
| 8 | F | 79 | IIIA | 45 | 52 | 0 | 41.36 | 22.32 | 4.9 | ||
| 9 | M | 61 | IIIA | 150 | 66 | 5 | 51.70 | 7.67 | 4.9 | ||
| 10 | F | 77 | IIIA | 90 | 68 | 4 | 45.60 | 22.70 | 6.2 | Infection I/D ×2 | |
| 11 | M | 72 | IIIA | 45 | 66 | 5 | 38.87 | 10.00 | 7.1 | Haematoma I/D | Died |
| 12 | F | 73 | IIIA | 120 | 66 | 4 | 53.45 | 29.51 | 6.7 | ||
| 13 | F | 73 | IIIA | 180 | 58 | 3 | 11.08 | 33.30 | 3.2 | Failed | |
| 14 | F | 65 | IIIA | 180 | 56 | 3 | 31.31 | 2.73 | 3.2 | ||
| 15 | F | 56 | IIIB | 90 | 68 | 6 | 35.66 | 44.43 | 4.4 | ||
| 16 | F | 55 | IIIB | 45 | 68 | 4 | 45.40 | 12.04 | 9.9 | Vessel injury | |
| 17 | F | 71 | IIIB | 30 | 56 | 4 | 46.97 | 22.86 | 14.7 | ||
| 18 | F | 79 | IIIA | 60 | 52 | 0 | 54.71 | 9.87 | 11.3 | Trochanteric fx | Died |
| 19 | F | 41 | IIIA | 45 | 78 | 2 | 49.79 | 7.78 | 12.6 | ||
| 20 | M | 66 | IIIA | 45 | 68 | 4 | 40.29 | 8.72 | 10.2 | Died | |
| 21 | M | 81 | IIIB | 45 | 66 | 3 | 47.90 | 7.47 | 10.4 | Died | |
| 22 | M | 79 | IIIA | 45 | 68 | 3 | 35.01 | 13.36 | 6.4 | ||
| 23 | M | 62 | IIIB | 45 | 66 | 3 | 50.67 | 12.20 | 4.9 | ||
| 24 | M | 75 | IIIA | 90 | Cage 68a | 7 | 61.70 | 27.60 | 9.5 | ||
| 25 | M | 70 | IIIA | 45 | 68 | 2 | 46.30 | 2.44 | 5.3 | ||
| 26 | M | 71 | IIIA | 90 | 68 | 4 | 31.49 | 17.76 | 7.7 | ||
| 27 | F | 64 | IIIA | 90 | 64 | 3 | 42.38 | 22.06 | 8.7 | ||
| 28 | M | 57 | IIIA | 45 | 66 | 3 | 48.30 | 5.01 | 9.3 | ||
| 29 | M | 54 | IIIA | 45 | 62 | 4 | 40.08 | 5.03 | 10.1 | Died | |
| 30 | M | 70 | IIIB | 30 | 80 | 2 | 40.83 | 5.85 | 8.2 | ||
| 31 | M | 67 | IIIA | 30 | 62 | 2 | 46.88 | 2.82 | 8.9 | ||
| 32 | M | 64 | IIIB | 45 | 64 | 2 | 58.93 | 10.99 | 7.1 | ||
| 33 | F | 59 | IIIB | 90 | 60 | 7 | 57.58 | 8.03 | 4.0 | ||
| 34 | M | 65 | IIIA | 45 | 62 | 3 | 39.56 | 18.75 | 8.9 | ||
F/U follow-up, M male, F female, I/D irrigation/debridement, fx fracture
aA 68-mm diameter cup was used with cage
Acetabular cup position was measured by the Martell Hip Analysis Suite™ program using the latest follow-up radiographs of the pelvis anteroposterior and shoot-through hip lateral view. Optimal cup position (safe zone) was defined as 40 ± 10° for abduction and 15 ± 10° for anteversion based on Lewinnek et al. [3]. Patients’ medical records were followed up longitudinally and related complications were identified and recorded. Five patients died of medical causes unrelated to the surgery during the follow-up. Re-revision of the cup for any reason or dislocation was defined as failure. The mean time from the acetabular revision to the latest follow-up was 7.6 years (range 3.2–14.7 years).
Statistical analysis was performed using SPSS version 17.0 (SPSS Inc/IBM, Chicago, IL, USA). Fisher’s exact and Student’s t test were used to compare the proportions and means of variables between groups. Multivariable logistic regression analysis was performed to identify risk factors for cup malpositioning. Two-tailed p value <0.05 was considered statistically significant.
Results
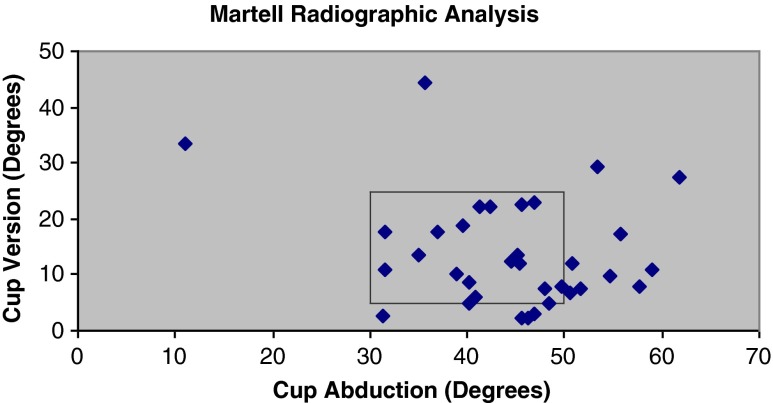
The measurements of acetabular abduction angle ranged from 11.08 to 61.70° with an average of 42.79°. The anteversion angle ranged from 2.25 to 44.43° with an average of 12.90°. Of 34 cups, 24 (71 %) were placed in the safe zone of abduction and 26 of 34 cups (76 %) were placed in the safe zone of anteversion. When both parameters are combined, 19 of 34 (56 %) cups were placed in the safe zone of both abduction and anteversion (Fig. 1).
Fig. 1.
Scatter plot of each hip’s abduction and version angles within the safe zone of Lewinnek et al. (30°–50° abduction, 5°–25° anteversion) [3]
Four patients required additional surgery for complications: infection (n = 1), haematoma formation (n = 1), intraoperative vessel injury (n = 1) and trochanteric fracture (n = 1). Infection and haematoma were managed by irrigation/debridement and haematoma evacuation. Vessel injury was managed by interruption of the revision procedure with vascular repair and subsequent delayed acetabular revision. Trochanteric fracture was converted to extended trochanteric osteotomy intraoperatively.
There was one failure of the cup due to aseptic loosening, which was outside the safe zone with 11.08° of abduction and 33.30° of anteversion. The cup was re-revised by staged acetabular reconstruction with allogenic bone graft and reimplantation of a cementless cup. There was no dislocation in this study group.
Uni- and multivariate logistic regression was performed to assess possible predictors of malpositioning and no significant independent factors were identified: age (p = 0.30), gender (p = 0.56), laterality (p = 0.79), type of defect (p = 0.83), bone graft (p = 0.10), cup size (p = 0.18) and screw fixation (p = 0.94) (Table 2).
Table 2.
Comparison between patients with and without acceptable cup positioning
| Variable | Acceptable results (n = 19) | Cup malpositioning (n = 15) | Univariate p valuea |
|---|---|---|---|
| Age at revision, years | 0.49 | ||
| ≤65 | 8 (42 %) | 9 (60 %) | |
| >65 | 11 (58 %) | 6 (40 %) | |
| Gender | 0.73 | ||
| Male | 12 (63 %) | 8 (53 %) | |
| Female | 7 (37 %) | 7 (47 %) | |
| Laterality | 1.00 | ||
| Left | 11 (58 %) | 8 (53 %) | |
| Right | 8 (42 %) | 7 (47 %) | |
| Bone defect | 1.00 | ||
| Type IIIA | 12 (63 %) | 10 (67 %) | |
| Type IIIB | 7 (37 %) | 5 (33 %) | |
| Bone graft | 0.20 | ||
| ≤90 ml | 17 (90 %) | 10 (67 %) | |
| >90 ml | 2 (10 %) | 5 (33 %) | |
| Cup size | 0.30 | ||
| Large | 7 (37 %) | 9 (60 %) | |
| Extra large | 12 (63 %) | 6 (40 %) | |
| Screw fixation | 1.00 | ||
| No | 4 (21 %) | 3 (20 %) | |
| Yes | 15 (79 %) | 12 (80 %) | |
| Age, years | 67.4 ± 11.3 | 62.2 ± 13.8 | 0.23 |
| Bone graft, ml | 71.8 ± 59.5 | 93.0 ± 55.6 | 0.30 |
| Cup size, mm | 65 ± 7 | 63 ± 5 | 0.24 |
Fisher’s exact test was used to compare groups for categorical data and Student’s t test for continuous variables. Plus-minus data are mean ± SD
aNo significant factors associated with malpositioning by univariate analysis
Discussion
Malposition of the acetabular component has been associated with increased risk of complications including dislocation, impingement, acetabular component migration, wear and osteolysis [3, 17]. As the cup position probably is the most sensitive single variable within the surgeon’s control to minimise risk of complications, the importance of correct cup positioning cannot be overemphasised. However, proper placement of acetabular components can potentially be compromised in the setting of revision because loss of normal bony landmarks is frequently encountered. While there are a number of reports of cup position in primary THA, data of cup position in revision THA are limited [6]. Therefore the current study investigated acetabular cup position in the revision situation with large bone defects.
In this study, the result of cup position demonstrated the challenges of proper component placement. Only 19 of 34 (56 %) cups fell in the optimal safe zone when both abduction and anteversion were combined. However, these results were similar to those of previous reports of cup position after primary THA [18–20], which showed a wide range of cup position using the same criteria of safe zone by Lewinnek [3]. In the literature, Saxler et al. [20], in their retrospective computed tomography (CT)-controlled measurement, reported that only 25.7 % (27/105) of cups in primary THA were placed within the safe zone. DiGioia et al. [19] also demonstrated that 78 % (59/74) of cups implanted in primary THA using a mechanical guide were outside the safe zone. On the other hand, Bosker et al. [18] showed that the 70.5 % of cups in primary THA were positioned within the safe zone by a freehand technique. In recent studies, improved cup position using computer navigation [21, 22] and its accuracy [23] have been reported.
In a setting of revision THA, Callanan et al. [6] described that 57 % of revised cups were optimally positioned in their analysis. Although the authors they used a stricter definition of acceptable ranges (abduction 30–45° and version 5–25°) in their study the success rate of optimal cup positioning was similar to the current study results. The traditional bony architectures are frequently distorted or absent in the setting of revision. However, very careful patient positioning, wide exposure of the acetabulum to understand the geometry and repeat trial with intraoperative radiographic evaluation may have contributed to the relatively similar prevalence of optimal cup positioning in the revision situation.
For measurement of cup position, a wide variety of parameters for the abduction and anteversion has been suggested [6, 24–26]. Wan et al. [4] pointed out the effects of pelvic tilt in angle measurement and recommended all inclination and anteversion be converted to the radiographic inclination and anteversion based on the coronal plane. In the current study, the safe zone as defined by Lewinnek et al. [3] was utilized, which has been widely accepted, although a cup in the safe zone by one definition may be out of the safe zone by another definition. Furthermore, in the current study, a digital image analysis program (Martell Hip Analysis Suite™) was used. This technique was initially developed for determination of polyethylene wear in THA, but it also provides an effective way to accurately determine abduction and version angles of the cup. This is the first study the authors are aware of that uses the Martell technique to evaluate acetabular component position in the setting of revision THA with large bone defects.
Surgical approach, surgeon case numbers and obesity have been reported as factors correlated to malpositioned cup in a previous study [6]. This was further investigated using various patient and surgical factors to find out possible independent predictors in the setting of large bone defect, but it did not appear that acceptable results versus cup malpositioning were related to any of the variables tested: age, gender, laterality, type of defect, amount of bone graft, cup size and screw fixation.
There are limitations to this study. Firstly, the definition of optimal cup position may vary and there is no consensus, specifically in terms of revision surgery. In addition, a combined version should also be considered in conjunction with the femoral component. Secondly, during the long-term study period, various techniques of acetabular reconstruction were used, which might have led to inconsistent treatment outcome. Although this may have been a confounding factor, the focus of this study was to evaluate the cup positioning. Lastly, this study has a relatively small number of patients, although this is the first study to report the cup position in the setting of revision THA with large bone defect to the authors knowledge.
In conclusion, the prevalence of 'optimal' cup positioning in revision THA with Paprosky type III acetabular bone defects was only in half of cases based on Martell digital image analysis. However, the prevalence of optimal acetabular cup position was similar to those reported in primary THA, suggesting that the presence of a large acetabular bone defect may not necessarily be a significant risk factor for suboptimal acetabular cup positioning in the setting of revision surgery.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Moskal JT, Capps SG. Improving the accuracy of acetabular component orientation: avoiding malposition. J Am Acad Orthop Surg. 2010;18:286–296. doi: 10.5435/00124635-201005000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Wera GD, Ting NT, Moric M, Paprosky WG, Sporer SM, Della Valle CJ. Classification and management of the unstable total hip arthroplasty. J Arthroplasty. 2012;27:710–715. doi: 10.1016/j.arth.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 4.Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009;467:32–42. doi: 10.1007/s11999-008-0597-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 6.Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319–329. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Del Gaizo DJ, Kancherla V, Sporer SM, Paprosky WG. Tantalum augments for Paprosky IIIA defects remain stable at midterm followup. Clin Orthop Relat Res. 2012;470:395–401. doi: 10.1007/s11999-011-2170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herrera A, Martínez AA, Cuenca J, Canales V. Management of types III and IV acetabular deficiencies with the longitudinal oblong revision cup. J Arthroplasty. 2006;21:857–864. doi: 10.1016/j.arth.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 9.Martell JM, Berdia S. Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Joint Surg Am. 1997;79:1635–1641. doi: 10.2106/00004623-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Sporer SM, O’Rourke M, Chong P, Paprosky WG. The use of structural distal femoral allografts for acetabular reconstruction. Average ten-year follow-up. J Bone Joint Surg Am. 2005;87:760–765. doi: 10.2106/JBJS.D.02099. [DOI] [PubMed] [Google Scholar]
- 11.Garcia-Cimbrelo E, Cruz-Pardos A, Garcia-Rey E, Ortega-Chamarro J. The survival and fate of acetabular reconstruction with impaction grafting for large defects. Clin Orthop Relat Res. 2010;468:3304–3313. doi: 10.1007/s11999-010-1395-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berry DJ, Müller ME. Revision arthroplasty using an anti-protrusio cage for massive acetabular bone deficiency. J Bone Joint Surg Br. 1992;74:711–715. doi: 10.1302/0301-620X.74B5.1527119. [DOI] [PubMed] [Google Scholar]
- 13.Jasty M. Jumbo cups and morselized graft. Orthop Clin North Am. 1998;29:249–254. doi: 10.1016/S0030-5898(05)70323-0. [DOI] [PubMed] [Google Scholar]
- 14.Hansen E, Ries MD. Revision total hip arthroplasty for large medial (protrusio) defects with a rim-fit cementless acetabular component. J Arthroplasty. 2006;21:72–79. doi: 10.1016/j.arth.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 15.Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. 2001;83-A:1352–1357. doi: 10.2106/00004623-200109000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Dearborn JT, Harris WH. High placement of an acetabular component inserted without cement in a revision total hip arthroplasty. Results after a mean of ten years. J Bone Joint Surg Am. 1999;81:469–480. doi: 10.2106/00004623-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Moskal JT, Capps SG. Acetabular component positioning in total hip arthroplasty: an evidence-based analysis. J Arthroplasty. 2011;26:1432–1437. doi: 10.1016/j.arth.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Bosker BH, Verheyen CC, Horstmann WG, Tulp NJ. Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch Orthop Trauma Surg. 2007;127:375–379. doi: 10.1007/s00402-007-0294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Digioia AM, 3rd, Jaramaz B, Plakseychuk AY, Moody JE, Jr, Nikou C, Labarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364. doi: 10.1054/arth.2002.30411. [DOI] [PubMed] [Google Scholar]
- 20.Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grützner PA, Steffen R, von Knoch M, Holland-Letz T, Bernsmann K. The accuracy of free-hand cup positioning–a CT based measurement of cup placement in 105 total hip arthroplasties. Int Orthop. 2004;28:198–201. doi: 10.1007/s00264-004-0542-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haaker RG, Tiedjen K, Ottersbach A, Rubenthaler F, Stockheim M, Stiehl JB. Comparison of conventional versus computer-navigated acetabular component insertion. J Arthroplasty. 2007;22:151–159. doi: 10.1016/j.arth.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 22.Ybinger T, Kumpan W. Enhanced acetabular component positioning through computer-assisted navigation. Int Orthop. 2007;31(Suppl 1):S35–S38. doi: 10.1007/s00264-007-0430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumar MA, Shetty MS, Kiran KG, Kini AR. Validation of navigation assisted cup placement in total hip arthroplasty. Int Orthop. 2012;36:17–22. doi: 10.1007/s00264-011-1268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dorr LD. Acetabular cup position: the imperative of getting it right. Orthopedics. 2008;31:898–899. doi: 10.3928/01477447-20080901-10. [DOI] [PubMed] [Google Scholar]
- 25.Harris WH. Advances in surgical technique for total hip replacement: without and with osteotomy of the greater trochanter. Clin Orthop Relat Res. 1980;146:188–204. [PubMed] [Google Scholar]
- 26.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]