Abstract
Purpose
The current models of reverse shoulder arthroplasty (RSA) expose the procedure to the risk of scapular notching, possibly leading to loosening of the glenoid. We compared the clinical and radiographic results obtained with a concentric or eccentric glenosphere to assess whether the eccentric design might give better clinical results and avoid or decrease the risk of scapular notching
Methods
Of our patients, 31 underwent RSA using a concentric glenosphere (group A), while 29 had an eccentric glenosphere (group B). Postoperatively, patients were followed-up at one to 12 months and annually thereafter, with the mean being 33 months in group A and 27.5 in group B. In both groups the minimum follow up (F-U) was 24 months. Preoperatively and at each F-U starting from six months, patients were assessed using the Constant score. On radiographs, prosthesis scapular neck angle (PSNA), distance between scapular neck and glenosphere (DBSNG) and peg-glenoid rim distance (PGRD) were calculated. The severity of notching was classified in four grades.
Results
In group A the mean Constant score increased by 30 points compared to the preoperative score and the active ROM increased considerably. At latest F-U, the mean PSNA, DBSNG and PGRD were, respectively, 87°, 3.4 mm and 19.8 mm. Glenoid notching was present in 42 % of cases. In group A, the mean Constant score increased by 34 points and the mean ROM was better than in group A. The average PSNA, PGRD and DBSNG were, respectively, 92°, 21.2 mm and 4.3 mm. Radiographs showed no inferior scapular notching.
Conclusions
The eccentric glenosphere yielded better clinical results than the concentric glenosphere and was associated with no scapular notching.
Keywords: Glenosphere, Eccentric, Concentric, Reverse total shoulder arthroplasty
Introduction
In 1983, Neer et al. [1] described the clinical and pathological features of a condition that they called cuff tear arthropathy (CTA). In 1987, Grammont et al. [2] conceived a new total shoulder prosthesis, called a reverse shoulder prosthesis, which was aimed simply at treating patients with cuff arthropathy. The reverse prosthesis that is presently used has changed in some ways over time, but both the design and the mechanism of action are still based on the original concept.
In the early 2000s, it was realised that the medialisation of the centre of rotation inherent in the prosthesis tends to result in mechanical impingement between the superomedial aspect of the humeral polyethylene insert and the scapular neck during arm adduction. This phenomenon, called scapular notching [3–5], involves osteolysis of the scapula neck, caused by polyethylene debris, which may be responsible for different degrees of glenoid erosion, possibly leading to loosening of the glenoid component. Several factors are responsible for scapular notching. Lévigne et al. [6] highlighted the role of preoperative predisposing factors, such as CTA grade 3 or 4, fatty infiltration of the infraspinatus muscle, excessive narrowing of the acromion–humeral distance or erosion of the upper glenoid bone. However, surgery-related factors have also been identified, essentially related to the positioning of the metaglene, i.e. higher than the inferior glenoid rim or implantation with a superior tilt. Nyffeler et al. [7] demonstrated that an inferior overhang of the glenosphere beyond the glenoid rim results in the greatest adduction, before impingement of humeral prosthesis against inferior scapular neck occurs. Simovitch et al. [8] confirmed that the craniocaudal positioning of the glenosphere, and the angular relationship between the glenosphere and the scapular neck, are highly correlated with the quality of the clinical outcome and the incidence or severity of scapular notching. To avoid this drawback, a new glenosphere was introduced in the Systema Multiplana Randelli (SMR) reverse shoulder prosthesis which has an eccentric shape (eccentric glenosphere), making it possible to lower the centre of rotation and theoretically decrease or avoid scapular notching compared with the current concentric glenosphere [7, 9].
Our investigation set out to assess the clinical and radiographic results obtained in patients undergoing a reverse prosthesis with a concentric glenosphere in comparison with those in whom an eccentric glenosphere was implanted. The aim of this comparative study, which, to our knowledge, is the first of its kind, was to determine whether or not the eccentric glenosphere implant would give better clinical results and avoid scapular notching.
Materials and methods
Between January 2004 and December 2009, 60 reverse shoulder prostheses were performed by two experienced shoulder surgeons. Only patients with CTA or an irreparable rotator cuff lesion not eligible for tendon transfer were included in this study. Two patients, one who developed Alzheimer disease and one who died before the latest follow-up, and another two patients who could not be traced, were excluded from the study, thus leaving 56 participants.
In two different centres that were highly specialised in shoulder surgery 31 operations were performed to implant a concentric glenosphere (group A), whereas an eccentric glenosphere was used in 25 operations (group B). The demographic data and the pathological condition of the patients in the two groups are reported in Table 1. In both centres the same type of prosthesis was implanted (SMR reverse shoulder prosthesis, Lima Corporate, Udine, Italy).
Table 1.
Demographic data, length of follow-up and type of shoulder disease of patients
| Group | Type of glenosphere | No. patients | Mean age (range), years | Mean follow-up (range), months | Aetiology |
|---|---|---|---|---|---|
| Group A | 36-mm concentric | 31 (14 M; 17 F) | 73 (68–82) | 33 (25–52) | 24 CTA; 7 MRC |
| Group B | 36-mm eccentric | 25 (6 M; 19 F) | 75 (69–85) | 27.5 (24–46) | 25 CTA |
CTA cuff tear arthropathy, MRC massive rotator cuff tear, F female, M male
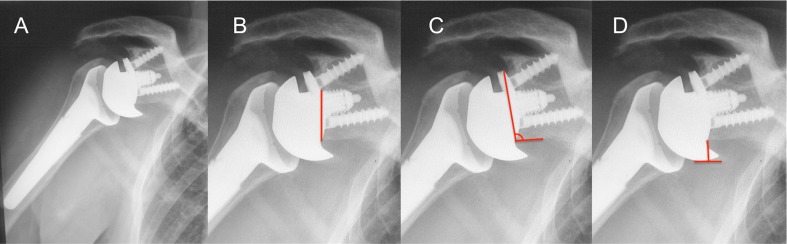
Before surgery, patients were clinically evaluated using Constant score to accurately assess the degree of active shoulder motion (Table 2). A score on a visual analogue scale (VAS) from 0 to 10 was also obtained in all cases. Postoperatively, patients were evaluated at one, three, six and 12 months and annually thereafter; the latest follow-up being carried out at a minimum of 24 months after surgery. The length of follow-up in both groups is reported in Table 1. At each follow-up, starting from that at six months up to the latest, all patients were evaluated using the Constant and Murley [10] system and anteroposterior and axillary radiographs were obtained. The measurements made on the radiographs were the prosthesis scapular neck angle (PSNA), the distance between the scapular neck and the glenosphere (DBSNG) and the peg–glenoid rim distance (PGRD) (Fig. 1; Table 3). The severity of scapular notching was assigned to one of four grades, according to Sirveaux’s classification [4].
Table 2.
Mean score on the Constant score and active range of motion preoperatively and at last follow-up in both groups
| Outcome | Group A | Group B | ||||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Gain | Preoperative | Postoperative | Gain | |
| Constant score (%) | 32 | 62 | 30 | 30 | 64 | 34 |
| Anterior elevation (°) | 62 | 129 | 67 | 66 | 148 | 82 |
| Abduction (°) | 65 | 116 | 51 | 60 | 115 | 55 |
| External rotation (°) | 8 | 15 | 7 | 5 | 16 | 11 |
| Internal rotation | S1 | L5 | S1 | L5 | ||
Fig. 1.
a Anteroposterior radiograph at 12 months follow-up. b The peg–glenoid rim distance. c The prosthesis–scapular neck angle. d The distance between the scapular neck and the glenosphere
Table 3.
Radiographic measurements
| Measurement | Group A | Group B | ||
|---|---|---|---|---|
| Mean | Range | Mean | Range | |
| PSNA (°) | 87 | 84–97 | 92 | 68–124 |
| PGRD (mm) | 19.08 | 16–22.5 | 21.2 | 16.5–23.4 |
| DBSNG (mm) | 3.4 | 3.2–3.9 | 4.3 | 3.5–4.9 |
DBSNG distance between scapular neck and glenosphere, PGRD peg–glenoid rim distance, PSNA prosthesis scapular neck angle
Characteristics of the glenospheres
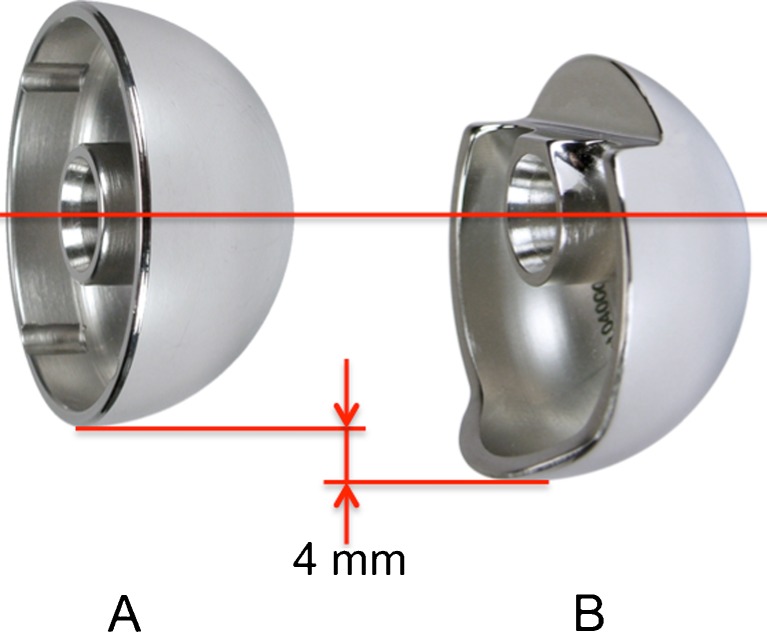
The concentric glenosphere, 36 mm in diameter, was made of CoCrMo, an alloy of copper, chromium and molybdenum (Fig. 2). To implant this glenosphere, the Kirshner guide wire was introduced into the glenoid a few millimetres below the anatomical centre of the cavity so that the inferior border of the baseplate, and hence of the glenosphere, was placed at the level of the inferior glenoid rim.
Fig. 2.
36-mm concentric and eccentric glenospheres
The eccentric glenosphere is 36 mm in diameter and at the time only the metallic type was available. It is linked to the baseplate by a double-Morse taper and a safety screw located in the polar position. It has a centre of rotation four millimetres lower than the baseplate axis. The articular surface has three different sections: the superior third is less than a hemisphere, the middle third is a true hemisphere, and the inferior third is greater than a hemisphere with a 5-mm inferior shield (Fig. 2). The glenosphere can be assembled on three different baseplate sizes. For the eccentric implants, a pointer was used to place a Kirshner guide wire at a distance of 14–16 mm—depending on the baseplate size—from the inferior glenoid rim to a position at the inferior border of the metal back over the caudal border of the glenoid.
Statistical analysis
All continuous variables were expressed as a mean ± standard deviation. The Wilcoxon test and Student’s t-test were performed to assess the significance of continuous data differences between preoperative and follow-up evaluations. The Mann–Whitney test was used to assess the significance of continuous data differences between the two treatment groups. A level of significance of p = 0.05 was set for all tests. Statistical analyses were performed using IBM SPSS Statistics, version 20.0 (SPSS Inc., Chicago, IL, USA).
Results
Group A
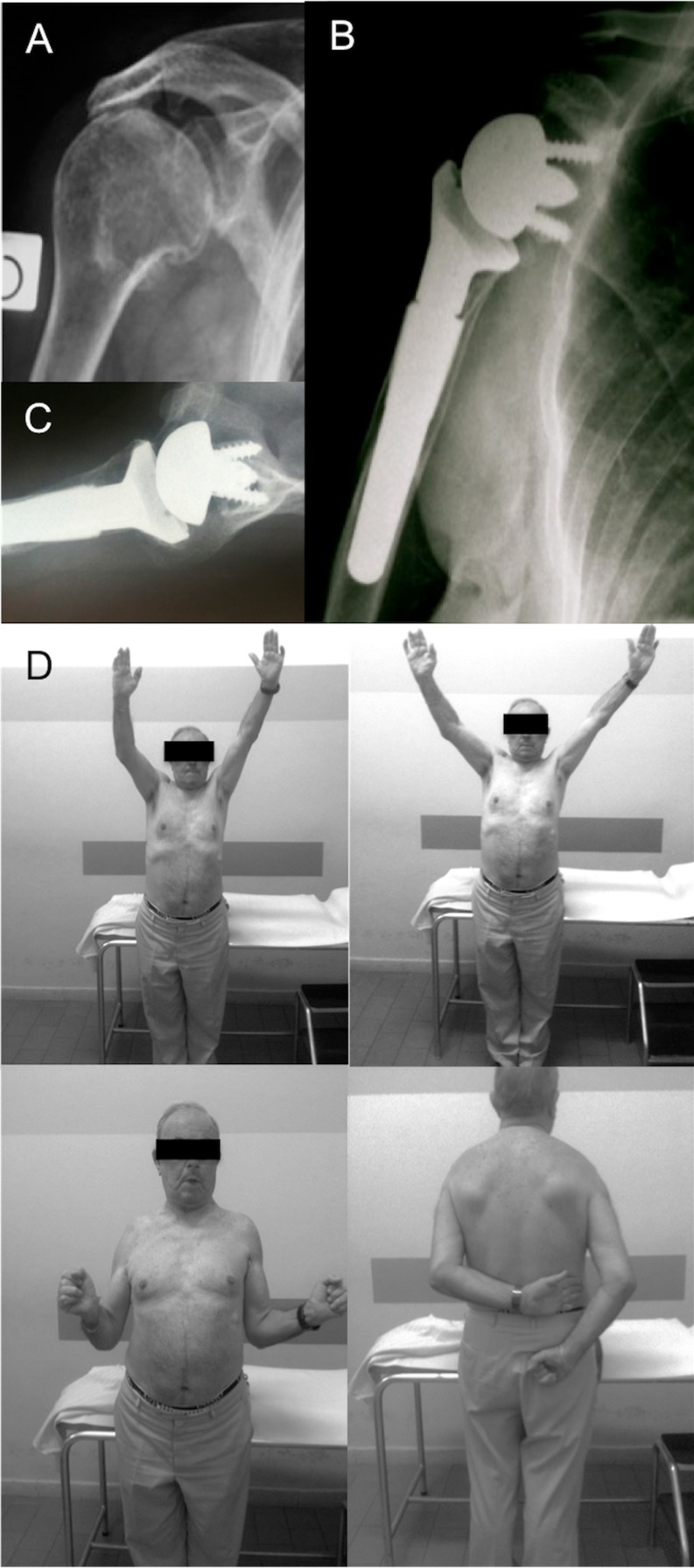
Before surgery, the mean score on the Constant scale was 32 points (range 21–40), while at the latest follow-up, the mean score was 62 (range 54–72), the difference being significant (p < 0.05). Active motion had increased considerably compared with the preoperative values (Table 2). The mean VAS score had significantly decreased from 8.2 ± 1.7 to 2.75 ± 1.38 postoperatively (p < 0.005) (Fig. 3).
Fig. 3.
a Preoperative radiograph. b Anteroposterior radiograph at one year follow up. c Axial lateral view at one year follow up. d One year clinical follow up
On postoperative radiographs the mean PSNA was 87° (range 84–97°) and the mean values of DBSNG and PGRD were, respectively, 3.4 mm and 19.8 mm (range 17.5–23) (Table 3). Glenoid notching was found in 13 patients (42 %). In seven of them the notching was evident at a mean of 17 months after surgery, while in six it was observed only at the latest follow-up. The grade of notching was I in 11 patients, II in one and IV in one. No significant differences in the clinical results were found between the patients with and without notching, except for the patient with grade IV glenoid erosion. A significant correlation emerged between the presence of scapular notching and higher PSNA and PGRD (p < 0.01). Conversely, higher values of DBSNG were found in those with no notching (p < 0.01).
No deep or superficial infection occurred. Three patients had dislocation of the prosthesis, which, in one case, was reduced by manipulation under general anaesthesia, while in two the polyethylene insert of the humeral component was replaced with a retentive component. No re-dislocation occurred.
Group B
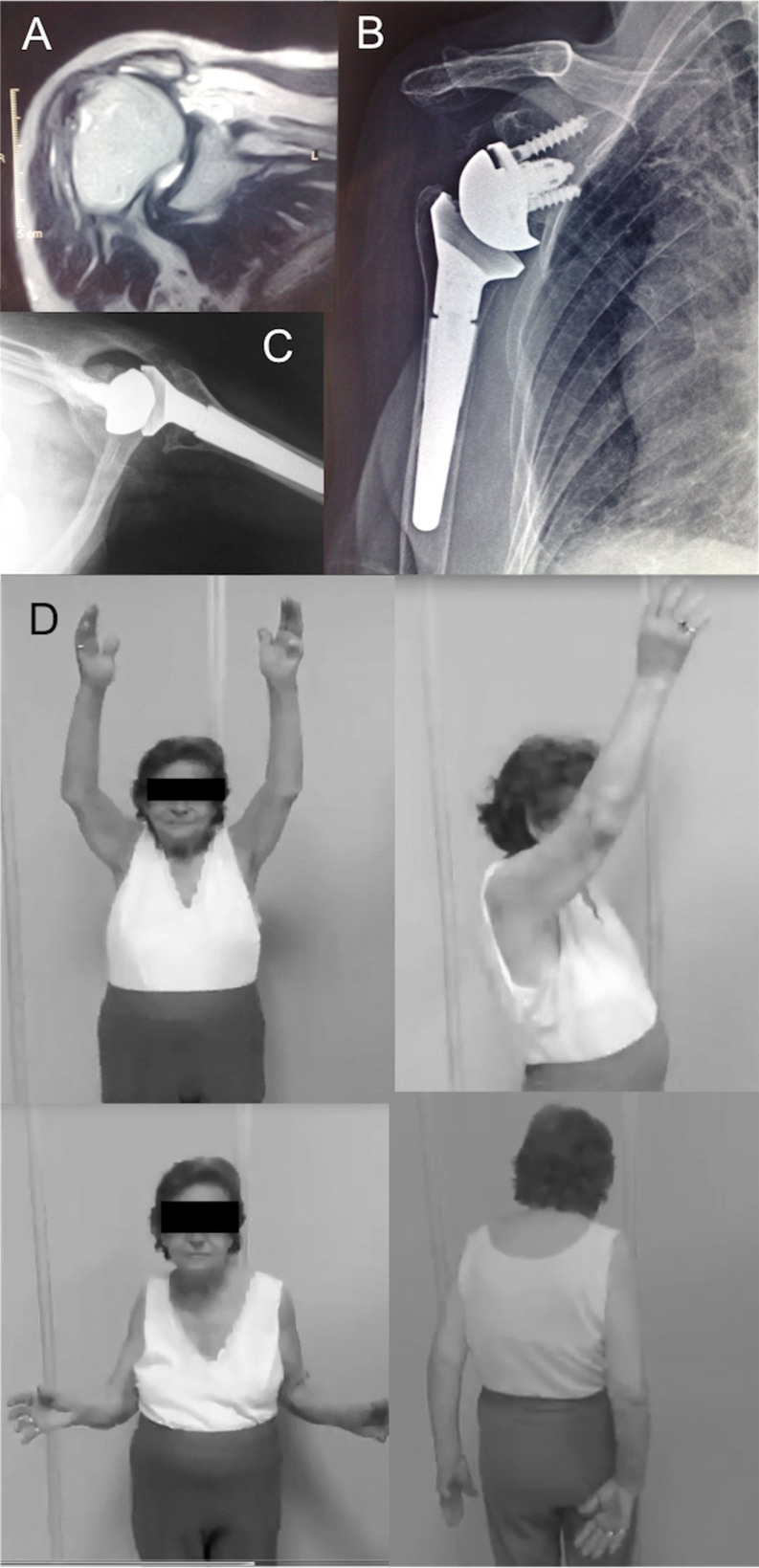
The mean score on the Constant scale, which was 30 (range 20–40) preoperatively, increased to 64 points (range 56–64) at the latest follow-up (p < 0.01). The considerable mean increase in the active range of shoulder motion is shown in Table 2. The mean VAS score decreased from 7.69 ± 1.88 to 2.55 ± 2.38 (p < 0.005) (Fig. 4).
Fig. 4.
a Preoperative MRI in a CTA. b Anteroposterior radiograph at one year follow up. c Axial lateral view at one year follow up. d One year clinical follow up
At the latest follow-up, the average PSNA and PGRD were, respectively, 92° (range 68–124°) and 21.2 mm (range 16.5–23.4). The average DBSNG was 4.3 mm (range 3.5–4.9) (Table 3).
Radiographs showed no inferior scapular notching, and no radiolucent lines were visible around the metalback components, i.e. baseplate, central peg or screws used for supplementary fixation of the baseplate.
No deep infection occurred, but one patient had a superficial infection that resolved in three weeks with appropriate antibiotic treatment. One patient had an anterior dislocation of the prosthesis, which occurred during the fourth month after surgery following a fall. The dislocation was treated successfully by closed reduction, followed by immobilisation of the shoulder for four months. No re-dislocation occurred in the three-year follow-up. No prosthesis underwent revision.
There was no significant difference in terms of clinical outcome (score on the Constant scale) between group A and group B.
Discussion
Inferior scapular notching is a frequent complication associated with reverse shoulder arthroplasty [4, 6, 8, 11–16]. Sirveaux et al. [4] found scapular notching in 49 of 77 patients (63.6 %) at a mean follow-up of 44.5 months. In another series, scapular notching was detected in 62 % of 337 shoulders at an average follow-up of 47 months [6]. In a recent systematic review of the literature, in which 782 cases were analysed, the incidence of the complication was 35.4 % [14]. It has been reported that mild or moderate scapular notching may have few or no clinical implications in the short- or medium-term following implantation. However, the long-term effects are unclear, and thus there is concern over the possibility that severe notching may jeopardise the stability of the glenoid component and affect the functional outcome [6, 8].
Several attempts have been made to reduce the incidence of this drawback by changing the position of the metaglene or conceiving new prosthetic designs. Attempts have been made to decrease the risk of notching by placing the metaglene more distally on the glenoid cavity, thus allowing the glenosphere to extend below the inferior border of the glenoid. The effect of the distalisation of the glenosphere is to significantly improve the abduction and adduction motion, which would decrease contact between the humeral polyethylene cup and the scapular neck [7, 9, 17]. However, a recent study has shown that this technique alone is not sufficient to avoid notching [13]. Frankle [18] has conceived a model of reverse prosthesis with an increased lateral offset of the glenosphere and/or baseplate. However, the lateralisation of the glenoid component that is achieved has the drawback of increasing the torque or shear force on the glenoid, and thus could potentially increase the risk of loosening of the component. To avoid the increase in torque or shear force, Boileau et al. [19] proposed the bony increased-offset reverse shoulder arthroplasty (bio-RSA), which keeps the centre of rotation at the glenoid bone–prosthesis interface once the bone graft has healed. However, the incidence of notching was 19 % at a mean follow-up of 28 months.
The eccentric glenosphere introduced in the SMR reverse shoulder prosthesis represents a further attempt to resolve the problem of the glenoid notching. In an in vitro biomechanical study that compared a standard SMR 36-mm concentric glenosphere with a similarly sized eccentric glenosphere [20], the latter was found to improve adduction by 14.5° and to decrease the mechanical impingement leading to the scapular notching. A further biomechanical study on SMR reverse shoulder prosthesis [21], which analysed the micromotion of the baseplate and its relationship to the risk of loosening, found that the 36-mm eccentric glenosphere increases micromotion of the metal back. However, the amount of micromotion was 16 μm, which is well within the plastic absorption of the cancellous bone of the glenoid [22].
In our study comparing concentric with eccentric glenospheres we observed 43 % of glenoid notching, although mostly grade I on Sirvaux’s classification [4], in patients undergoing SMR reverse shoulder prosthesis with a concentric glenosphere. In contrast, no notching was detected in those with an eccentric glenosphere at a minimum follow-up of 24 months (range 25–56 months), which confirms the result of our previous study with shorter follow-ups [23]. Furthermore, the patients who had an eccentric glenosphere showed a significantly better range of motion in flexion and abduction of the arm than those with a concentric glenosphere. The difference that we found, which appears to be related to the different design of the eccentric implant on the longitudinal axis, is consistent with the results of a biomechanical study which found that, compared with the concentric glenosphere, the eccentric design significantly improves the range of shoulder motion by allowing a higher degree of adduction [21]. On radiographs we have found that there was only one millimetre of difference in the glenoid overhang of the glenosphere. We believe that it is difficult to attribute the absence of inferior scapular notching in this short follow-up to only the distalisation of the implant. In fact, Mizuno et al. [24] published a series of 47 reverse shoulder arthroplasties with an eccentric glenosphere allowing two millimetres of overhang with an average follow-up of 30.4 months. They reported 40.4 % of notching, concluding that the eccentric glenosphere does not prevent scapular notching but decreases the severity of scapular notching at early follow-up.
What is peculiar in the SMR eccentric glenosphere is the shape of its lower part—it has an inferior five millimetre horizontal shield. This distinctive characteristic provides a mechanical protection for the scapular neck and, in addition, adds a further element to avoid scapular notching.
De Wilde et al. [25] highlighted the importance of the shape of the horizontal part of the scapular pillar and how this could influence the adduction angle. In fact, in a scapula without a horizontal scapular pillar a distalisation of the base plate by two millimetres allows a decrease in the adduction angle by eight degrees. While in a scapula with five millimetres of horizontal scapular pillar neck the same two millimetres of base plate distalisation allows a decrease of 20° in the adduction angle.
One of the limitations of this study is that the mean follow-up of 35 and 28 months in group A and B, respectively, is relatively short to assess the results of arthroplasty, and thus evaluations over longer periods of time are necessary to determine the longevity of both the prosthesis and the short-term clinical results. A further limitation concerns the limited number of cases that we assessed, but this is not dissimilar to the populations evaluated in most previous studies on reverse shoulder arthroplasty.
Conclusions
In summary, modern designs of reverse shoulder arthroplasty yield encouraging results in the treatment of cuff-deficient shoulder conditions. Although it is too early to reliably predict the effects of differing prosthetic designs on long-term outcomes, our early experience with the SMR RSA shows favourable results and a low rate of complications. In particular, the eccentric design type showed encouraging results and may reduce mechanical impingement and the risk of scapular notching.
References
- 1.Neer CS, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg. 1983;65:1232–1244. [PubMed] [Google Scholar]
- 2.Grammont P, Trouilloud P, Laffay J, Deries X. Concept study and realization of a new total shoulder prosthesis. Rhumatologie. 1987;39:407–418. [Google Scholar]
- 3.Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for 5–10 years. J Bone Joint Surg Am. 2006;88:1742–1747. doi: 10.2106/JBJS.E.00851. [DOI] [PubMed] [Google Scholar]
- 4.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molè D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–395. doi: 10.1302/0301-620X.86B3.14024. [DOI] [PubMed] [Google Scholar]
- 5.Scarlat MM. Complications with reverse total shoulder arthroplasty and recent evolutions. Int Orthop. 2013;37(5):843–851. doi: 10.1007/s00264-013-1832-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lévigne C, Boileau P, Favard L, Garaud P, Mole D, Sirveaux F, Walch G. Scapular notching in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2008;17:925–935. doi: 10.1016/j.jse.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 7.Nyffeler RW, Werner CM, Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg. 2005;14:524–528. doi: 10.1016/j.jse.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89:588–600. doi: 10.2106/JBJS.F.00226. [DOI] [PubMed] [Google Scholar]
- 9.Kelly JD, Humphrey CS, Norris TR. Optimizing glenosphere position and fixation in reverse shoulder arthroplasty. Part one: the twelve-mm rule. J Shoulder Elbow Surg. 2008;17:589–594. doi: 10.1016/j.jse.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 11.Farshad M, Gerber C. Reverse total shoulder arthroplasty from the most to the least common complication. Int Orthop. 2010;34:1075–1082. doi: 10.1007/s00264-010-1125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]
- 13.Wall B, Nove-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 14.Zumstein AM, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–157. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:147S–161S. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–540. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Gutiérrez S, Levy JC, Frankle MA, Cuff D, Keller TS, Pupello DR, Lee WE., 3rd Evaluation of abduction range of motion and avoidance of inferior scapular impingement in a reverse shoulder model. J Shoulder Elbow Surg. 2008;17:608–615. doi: 10.1016/j.jse.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 18.Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum 2-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87:1697–1705. doi: 10.2106/JBJS.D.02813. [DOI] [PubMed] [Google Scholar]
- 19.Boileau P, Moineau G, Roussanne Y, O’Shea K. Bony increased offset reversed shoulder arthroplasty: minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res. 2011;9:2558–2567. doi: 10.1007/s11999-011-1775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chou J, Malak SF, Anderson IA, Astley T, Poon PC. Biomechanical evaluation of different designs of glenospheres in the SMR reverse total shoulder prosthesis: range of motion and risk of scapular notching. J Shoulder Elbow Surg. 2009;18:354–359. doi: 10.1016/j.jse.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Poon PC, Chou J, Young D, Malak SF, Anderson IA. Biomechanical evaluation of different designs of glenospheres in the SMR reverse shoulder prosthesis: micromotion of the baseplate and risk of loosening. Shoulder Elbow. 2010;2:94–99. doi: 10.1111/j.1758-5740.2010.00059.x. [DOI] [PubMed] [Google Scholar]
- 22.Jasty M, Bragdon C, Burke D, O’Connor D, Lowenstein J, Harris WH. In vivo skeletal responses to porous-surfaced implants subjected to small induced motions. J Bone Joint Surg Am. 1997;79:707–714. doi: 10.2106/00004623-199705000-00010. [DOI] [PubMed] [Google Scholar]
- 23.De Biase CF, Delcogliano M, Borroni M, Castagna A. Reverse total shoulder arthroplasty: radiological and clinical result using an eccentric glenosphere. Musculoskelet Surg. 2012;96:S27–S34. doi: 10.1007/s12306-012-0193-4. [DOI] [PubMed] [Google Scholar]
- 24.Mizuno N, Denard PJ, Raiss P, Walch G. The clinical and radiographical results of reverse total shoulder arthroplasty with eccentric glenosphere. Int Orthop. 2012;36:1647–1653. doi: 10.1007/s00264-012-1539-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Wilde LF, Poncet D, Middernacht B, Ekelund A. Prosthetic overhang is the most effective way to prevent scapular conflict in a reverse total shoulder prosthesis. Acta Orthop. 2010;81:719–726. doi: 10.3109/17453674.2010.538354. [DOI] [PMC free article] [PubMed] [Google Scholar]