Abstract
Purpose
Mini invasive incisions in THA and femoral hip prostheses tend to minimise healing and recovery time. We have used a very posterior approach with technical modifications and precise skin landmarks to decrease surgical complexity, and we describe this experience here.
Methods
From 2010 to 2012, 140 patients aged 79 years (range 53–93 years) were operated upon by the same surgeon in a continuous series using the same minimally invasive skin incision and six different types of implants. The incision was very posterior in the hip allowing direct visualisation of the acetabulum in the hip flexion position and visualisation of the femoral shaft extremity in a leg flexion position.
Results
The mean operating time was 100 minutes (range 75–110 min). Estimated blood loss was 385 cc (20–585 cc). Twenty-six patients had blood transfusion. The mean hospital stay was 6.8 days (5–20 days) including the time waiting for a rehabilitation centre. No operative complications related to the technique were recorded. On the postoperative radiograph, the femoral stem was aligned with the femoral axis within 3° in all patients. The mean acetabular angle to the ground plane was 40° (35–48°).
No patient had a leg length discrepancy of more than four millimetres. The mean skin incision length was seven centimetres (six to eight centimetres). All patients were seen at the clinic after six weeks and the data were unchanged at this time point.
Conclusion
The method and skin landmarks we describe appear to be a safe way to perform minimally invasive total hip replacement.
Keywords: Minimally invasive incision, Total Hip Arthroplasty, Posterior, No complications
Introduction
Mini invasive incisions in total hip arthroplasty (THA) and femoral hip prostheses tend to minimise healing time, recovery time, hospital stay and surgical invasiveness, and also are something of a marketing tool for patients refusing a large lateral or anterior incision as a hip prosthesis flag. Available techniques may either increase or decrease surgical complexity and this is an important aspect to consider when making the final decision. We used a very posterior approach with technical modifications and very precise skin landmarks as a tool to decrease surgical complexity and improve patients’ outcomes. We hereby describe this experience on 140 cases with total hip replacements performed by the same surgeon as a continuous series.
Material and methods
Patients
From 2010 to 2012, 140 patients aged 79 years (53–93 years) were operated upon consecutively by the same surgeon. One hundred and eleven were female and 39 male. Reasons for hip replacement were a fracture in 102, primary hip arthritis in 27, and aseptic necrosis in 11. The operation was performed as an emergency in 104 cases (74 %). THA was performed on the right side in 61 (44 %) and the left side in 79 (56 %). The body mass index was 22.9 kg/m (14.5–31.1).
Implants
A total of six different types of implants from four different manufacturers were used. Implants were regular off-the-shelf hip prostheses with no particularities and no need for a specific implantation technique or ancillary modification. Uncemented femoral stems were used in 86 cases and cemented in 54. Acetabular components were dual mobility cups in 135 (101 with cement and 34 uncemented), cemented regular polyethylene in two and impacted titanium with ceramic insert in three cases.
Technique
The patients were anaesthetised and positioned in the lateral hip position using a regular operating table and normal restraints. The leg was positioned loosely in a 30° hip flexion, 60° knee flexion position on a curved support horizontal to the table and draped separately. Sterile draping was applied. The skin incision was six to eight centimetres in a very posterior position over the hip.
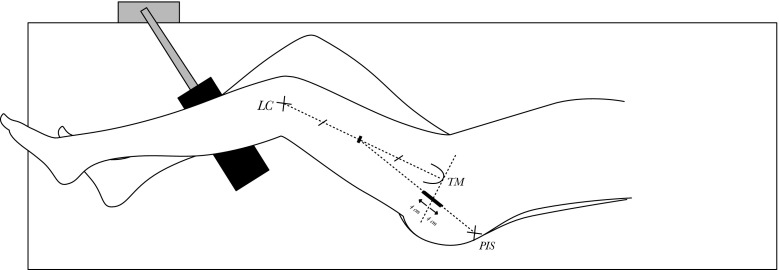
Precise skin landmarks were used to determine exactly the best position of the small skin incision to prevent difficulties. These landmarks were determined as the posterior iliac spine, the tip of the greater trochanter, and the lateral femoral condyle tubercle (see Fig. 1).
Fig. 1.
Landmarks to determine the skin incisions. LC lateral femoral condyle, TM trochanter major, PIS posterior iliac spine
As a general principle, a line was drawn on the skin, from the lateral femoral condyle to the palpable tip of the greater trochanter. The middle of this line was used as a new landmark, and joined to the posterior iliac spine. On this line the perpendicular to the axis of the femur from the tip of the trochanter major was projected, and the skin incision was made along the oblique posterior iliac line three to four centimetres proximal and three to four centimetres distal to this point. The subcutaneous tissues were incised to the fascia of the gluteus maximus. The gluteus maximus muscle was divided between its middle and posterior heads to the submuscular fat layer and maintained with a self-retaining retractor. This plane gave way to the posterior aspect of the cervical neck through the short external rotator muscles and the capsule. This layer was divided, the piriformis tendon cut close to its insertion and the capsule was opened. The femoral neck was cut in situ in cases with no fracture, and the head was extracted.
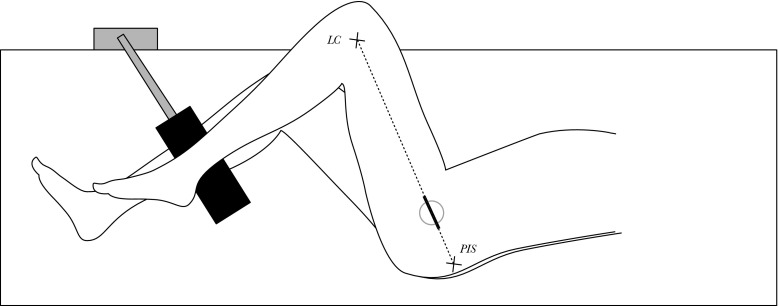
In the hip extension position, the small skin incision gave exposure to the posterior aspect of the femoral neck. In the hip flexion position over the U-shaped flat support, the posterior skin incision gave exposure to the acetabulum after femoral head removal (Fig. 2). Later during the procedure, the small incision exposed the femoral neck section just in front of the femoral diaphysis to prepare the femur and allow femoral stem insertion. The given exposure, although small, was sufficient for acetabular and femoral preparation using regular instruments.
Fig. 2.
In the hip flexion position with the ankle resting over the U-shaped flat support, the skin incision comes over the acetabulum allowing exposure and preparation. LC lateral femoral condyle, PIS posterior iliac spine
Closure of the incision only needed a deep X-shaped suture on the gluteus major muscle and skin suture. The posterior capsule and the piriformis tendon were sutured in all patients as a general practice.
Results
In 140 consecutive cases, the mean operating time was 100 minutes (75–110 min). Estimated blood loss was 385 cc (20–585 cc). Twenty-six patients (18.6 %) required blood transfusion of two to three units (mean 2.3 units). All operations took place uneventfully and no complications occurred. There were no acetabular or femoral fractures.
Postoperatively the mean hospital stay was 6.8 days (5–20 days) including the time waiting for a rehabilitation centre. No operative complication related to the technique was recorded. There was no infection, no postoperative dislocation or sciatic palsy in this series. One patient had a cerebrovascular infarction three days after the procedure that was ultimately fatal after nine days. One patient had a local wound infection that was treated non-operatively and resolved spontaneously with local dressing. All patients had full weight bearing within three days after the operation.
On the immediate postoperative radiograph, the femoral stem was aligned with the femoral axis within 3° in all patients. The mean acetabular angle to the ground plane was 40° (35–48°). No patient had a leg length discrepancy of more than four millimetres. The mean skin incision length was seven centimetres (six to eight centimetres) postoperatively. All patients were seen at the clinic after six weeks and the data were unchanged at this time. The visual analog scale at this time was 2.23 (0–4).
The technique attained its objectives without complication in all patients in this series.
Discussion
Total hip replacement implants have undergone many technical improvements from the first implantations; however, the surgical approach is somewhat similar to that initially described by Gibson in 1950 [1] and Moore in 1959 [2] as a posterior approach with external rotators section. The Charnley 1964 [3] anterior-lateral transtrochanteric approach was modified by Amstutz [4] introducing lateral positioning. The 1982 Hardinge lateral approach [5] puts the superior gluteal nerve at risk while cutting through the gluteus medius. The anterior Hueter incision as modified by Judet and Judet [6] is still used with a minimally invasive short incision; however, a dedicated specialised orthopaedic table is mandatory in this technique.
A minimally invasive hip incision is defined by a skin incision shorter than ten centimetres in THA [7]. Its aim is to minimise the surgical trauma while maintaining security.
Six different approaches have been described and used: the anterior [8, 9], antero-lateral [10, 11], posterior [12], postero-lateral [2], lateral [13, 14], and the double incision with fluoroscopy [15]. The posterior incision is well known [7, 16, 17] with advantages in minimising blood loss, postoperative pain, hospital stay and time to rehabilitation [18] with expected decrease in final procedure costs [19]. Complication rates may be identical to the regular procedure or not, with implant malpositioning [17, 20] or sciatic palsy [18].
In a study of 261 patients Dorr showed immediate postoperative improvements of the Harris hip score that did not last past the first six weeks [18]. Shitama et al. [21] and Nakamura et al. [22] showed the same conclusion after six months and DiGioia [23] one year after surgery. Flören et al. [24] showed that the minimal invasive posterior incision had the same clinical and radiological results as the standard techniques in 90 patients after ten to 13 years.
Ogonda et al. [25], in a comparative series of minimal versus standard in 219 hip arthroplasties, found no difference in blood loss, postoperative pain, time to autonomous walking and hospital stay. This was confirmed by Woolson et al. [17] in 135 patients and Sculco et al. [26].
Swanson [27], in 1,000 arthroplasties (759 patients) after 37 months with a posterior incision starting two centimetres posterior to the greater trochanter diverging 20° from the femoral axis, had 3 % dislocations and 0.6 % sciatic palsy. Body mass index in this study was not an exclusion criterion and ranged from 14.3 to 56.5 kg/cm². Operative time was 61 minutes and mean blood loss 317 ml, while 43.6 % had blood transfusion. Only 1.1 % had a per-operative femoral fracture, three in the greater trochanter, seven in the calcar and one spiral diaphyseal fracture. Just 2.1 % had an early reoperation for malposition of the acetabular (1.4 %) or the femoral (excessive varus) (0.1 %) component.
Swanson thus advised that this technique be confined to experienced surgeons with extensive THA background.
Other papers emphasise the long learning curve [20, 23, 28, 29] even for seasoned hip surgeons. Hartzband et al. [20] advised only surgeons operating on more than 50 hips per year to try the minimally invasive approach.
The posterior minimally invasive approach, being a modification of the standard Moore, has shown a very short learning curve in our experience.
Using specific instruments [20] and improving acetabular exposure through limb positioning [16] are recommended in techniques with imprecise initial incision landmarks. Cadaver studies show the pressure on wound edges from retractors to be twice as high in minimally invasive incisions [16, 30] compared to standard, and muscle trauma to be higher [31]. However, biology (creatine kinase) or functional recovery are not affected [32, 33].
The incision we describe projects itself just on the vertical from the acetabulum when the ankle is placed on the U-shaped support. The axis of the skin incision is the same as that of the standard acetabular instrumentation. Specific instrumentation remains minimal with only a curved self-retaining retractor maintaining low constraints on the soft tissues and gluteus maximus. In this position the axis of the femur shifted anteriorly necessitates no additional positioning to improve acetabular exposure. Then the skin incision axis is the same as the working channel to the femoral canal and the risk of missing the canal or skin trauma is much decreased. A very posterior skin incision may create concern about the sciatic nerve. However, no sciatic palsy or even paresthesia occurred in our series. The position of the inferior limb ankle on the U-shaped support shifts the greater sciatic nerve to a lower and posterior position as seen per-operatively. Cadaver studies are warranted to clarify these observations.
As stated by Lafosse et al. [34], direct visualisation of the lesser trochanter may prove difficult while using the posterior mini incision. However, we had no problem seeing this important landmark for the accurate femoral neck section [31] while using our approach due to the precision of the landmarks.
Minimally invasive hip approaches are defined by a skin incision smaller than ten centimetres and sparing hip muscles as the piriformis tendon [35]. Benefits from piriformis preservation are not known and we choose to section this tendon to improve direct view, and sutured the tendon at the time of closure as this does not improve time to walking [33] but reduces the dislocation rate [36, 37].
In this study, no patient had a BMI much greater than 31. This was not a result of selection; however, excluding major obese patients would seem sensible to reduce the risk of major per-operative complications such as femoral fractures and wound discharge [38]. Also, Sculo et al. [35] proposed a strategy where the total length of the skin incision is fixed as one third of the BMI in centimetres [39]. However, in a recent paper, Dienstknecht et al. [40] found that obese patients gain similar benefit from a minimally invasive incision as do non-obese patients.
Different and numerous skin incisions in posterior hip replacement surgery have been described. Most are direct lines joining two skin landmarks. The first landmark is on the postero superior extremity of the greater trochanter for Nakurama [22], or one [27] or two centimetres posterior to it. The second landmark is ten centimetres from the tip of the greater trochanter along the axis of the femur [27], or 15 cm [7], to six to nine centimetres [22], and as low as five centimetres [34]. These incisions with only the greater trochanter as a bony landmark do not provide the same exposure whether the patient is tall or short. Variability in the femur’s size amongst patients is a strong argument for using a skin incision with bony landmarks only, on the femur and iliac bone.
The skin incision we propose being based on these principles helps to attain correct exposure in all patients whatever their height and shape for the femur and the acetabulum.
Advantages concerning decreased operative blood loss, postoperative pain and faster recovery seemed the same as those reported in the literature [7, 16–18]. However, long delays in obtaining discharge to rehabilitation centres resulted in a substandard, very long mean hospital stay in this series.
Early ambulation and minimal scarring are components of the patients’ satisfaction in THA [41, 42]. However, Mow et al. [32] showed the total length of the incision ranked third in a poll study, after pain relief and the duration expectancy of the prosthesis.
Conclusion
The method and skin landmarks we describe appear to be a safe way to perform minimally invasive total hip replacement. No complication occurred and the technique was designed to decrease, not increase, the difficulties of the procedure.
References
- 1.Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br. 1950;32-B(2):183–186. doi: 10.1302/0301-620X.32B2.183. [DOI] [PubMed] [Google Scholar]
- 2.Moore AT. The Moore self-locking vitallium prothesis in fresh femoral neck fractures: a new low posterior approach (the southern exposure) AAOS Instr Course Lect. 1959;16:309. [Google Scholar]
- 3.Charnley J, Ferreiraade S. Transplantation of the greater trochanter in arthroplasty of the hip. J Bone Joint Surg Br. 1964;46:191–197. [PubMed] [Google Scholar]
- 4.Amstutz HC. Trapezoidal-28 total hip replacement. Clin Orthop Relat Res. 1973;95:158–167. [PubMed] [Google Scholar]
- 5.Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64(1):17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 6.Judet J, Judet R. The use of an artificial femoral head for arthroplasty of the hip joint. J Bone Joint Surg Br. 1950;32-B(2):166–173. doi: 10.1302/0301-620X.32B2.166. [DOI] [PubMed] [Google Scholar]
- 7.Procyk S. Initial results with a mini-posterior approach for total hip arthroplasty. Int Orthop. 2007;31(Suppl 1):S17–S20. doi: 10.1007/s00264-007-0435-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kennon R, Keggi J, Zatorski LE, Keggi KJ. Anterior approach for total hip arthroplasty: beyond the minimally invasive technique. J Bone Joint Surg Am. 2004;86-A(Suppl 2):91–97. doi: 10.2106/00004623-200412002-00013. [DOI] [PubMed] [Google Scholar]
- 9.Siguier T, Siguier M, Brumpt B. Mini-incision anterior approach does not increase dislocation rate: a study of 1037 total hip replacements. Clin Orthop Relat Res. 2004;426:164–173. doi: 10.1097/01.blo.0000136651.21191.9f. [DOI] [PubMed] [Google Scholar]
- 10.Bertin KC, Rottinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res. 2004;429:248–255. doi: 10.1097/01.blo.0000150294.81825.8c. [DOI] [PubMed] [Google Scholar]
- 11.Jerosch J, Theising C, Fadel ME. Antero-lateral minimal invasive (ALMI) approach for total hip arthroplasty technique and early results. Arch Orthop Trauma Surg. 2006;126(3):164–173. doi: 10.1007/s00402-006-0113-x. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein WM, Branson JJ, Berland KA, Gordon AC. Minimal-incision total hip arthroplasty. J Bone Joint Surg Am. 2003;85-A(Suppl 4):33–38. doi: 10.2106/00004623-200300004-00004. [DOI] [PubMed] [Google Scholar]
- 13.Berger RA. Mini-incision total hip replacement using an anterolateral approach: technique and results. Orthop Clin North Am. 2004;35(2):143–151. doi: 10.1016/S0030-5898(03)00111-1. [DOI] [PubMed] [Google Scholar]
- 14.Howell JR, Masri BA, Duncan CP. Minimally invasive versus standard incision anterolateral hip replacement: a comparative study. Orthop Clin North Am. 2004;35(2):153–162. doi: 10.1016/S0030-5898(03)00137-8. [DOI] [PubMed] [Google Scholar]
- 15.Berger RA, Duwelius PJ. The two-incision minimally invasive total hip arthroplasty: technique and results. Orthop Clin North Am. 2004;35(2):163–172. doi: 10.1016/S0030-5898(03)00110-X. [DOI] [PubMed] [Google Scholar]
- 16.Swanson TV. Posterior single-incision approach to minimally invasive total hip arthroplasty. Int Orthop. 2007;31(Suppl 1):S1–S5. doi: 10.1007/s00264-007-0436-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ. Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg Am. 2004;86-A(7):1353–1358. doi: 10.2106/00004623-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty. A prospective, randomized, blinded study. J Bone Joint Surg Am. 2007;89(6):1153–1160. doi: 10.2106/JBJS.F.00940. [DOI] [PubMed] [Google Scholar]
- 19.de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, Hutchison J, Grant A, Coyle D, Coyle K, Vale L (2008) A systematic review of the clinical effectiveness and cost-effectiveness and economic modeling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip. Health Technol Assess 12(26):iii–iv, ix–223 [DOI] [PubMed]
- 20.Hartzband MA. Posterolateral minimal incision for total hip replacement: technique and early results. Orthop Clin North Am. 2004;35(2):119–129. doi: 10.1016/S0030-5898(03)00119-6. [DOI] [PubMed] [Google Scholar]
- 21.Shitama T, Kiyama T, Naito M, Shiramizu K, Huang G. Which is more invasive-mini versus standard incisions in total hip arthroplasty? Int Orthop. 2009;33(6):1543–1547. doi: 10.1007/s00264-008-0708-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nakamura S, Matsuda K, Arai N, Wakimoto N, Matsushita T. Mini-incision posterior approach for total hip arthroplasty. Int Orthop. 2004;28(4):214–217. doi: 10.1007/s00264-004-0570-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DiGioia AM, 3rd, Plakseychuk AY, Levison TJ, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty. 2003;18(2):123–128. doi: 10.1054/arth.2003.50025. [DOI] [PubMed] [Google Scholar]
- 24.Floren M, Lester DK. Durability of implant fixation after less-invasive total hip arthroplasty. J Arthroplasty. 2006;21(6):783–790. doi: 10.1016/j.arth.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 25.Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O'Brien S, Beverland D. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87(4):701–710. doi: 10.2106/JBJS.D.02645. [DOI] [PubMed] [Google Scholar]
- 26.Sculco TP, Jordan LC, Walter WL. Minimally invasive total hip arthroplasty: the Hospital for Special Surgery experience. Orthop Clin North Am. 2004;35(2):137–142. doi: 10.1016/S0030-5898(03)00116-0. [DOI] [PubMed] [Google Scholar]
- 27.Swanson TV. Early results of 1000 consecutive, posterior, single-incision minimally invasive surgery total hip arthroplasties. J Arthroplasty. 2005;20(7 Suppl 3):26–32. doi: 10.1016/j.arth.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 28.Goldstein WM, Branson JJ. Posterior-lateral approach to minimal incision total hip arthroplasty. Orthop Clin North Am. 2004;35(2):131–136. doi: 10.1016/S0030-5898(03)00108-1. [DOI] [PubMed] [Google Scholar]
- 29.Levine BR, Klein GR, Di Cesare PE. Surgical approaches in total hip arthroplasty: a review of the mini-incision and MIS literature. Bull NYU Hosp Jt Dis. 2007;65(1):5–18. [PubMed] [Google Scholar]
- 30.Noble PC, Johnston JD, Alexander JA, Thompson MT, Usrey MM, Heinrich EM, Landon GC, Mathis KB. Making minimally invasive THR safe: conclusions from biomechanical simulation and analysis. Int Orthop. 2007;31(Suppl 1):S25–S28. doi: 10.1007/s00264-007-0432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Woolson ST, Hartford JM, Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14(2):159–164. doi: 10.1016/S0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]
- 32.Mow CS, Woolson ST, Ngarmukos SG, Park EH, Lorenz HP. Comparison of scars from total hip replacements done with a standard or a mini-incision. Clin Orthop Relat Res. 2005;441:80–85. doi: 10.1097/01.blo.0000191317.85422.c3. [DOI] [PubMed] [Google Scholar]
- 33.Ward SR, Jones RE, Long WT, Thomas DJ, Dorr LD. Functional recovery of muscles after minimally invasive total hip arthroplasty. Instr Course Lect. 2008;57:249–254. [PubMed] [Google Scholar]
- 34.Laffosse JM, Accadbled F, Molinier F, Chiron P, Hocine B, Puget J. Anterolateral mini-invasive versus posterior mini-invasive approach for primary total hip replacement. Comparison of exposure and implant positioning. Arch Orthop Trauma Surg. 2008;128(4):363–369. doi: 10.1007/s00402-007-0385-9. [DOI] [PubMed] [Google Scholar]
- 35.Khan RJ, Fick D, Khoo P, Yao F, Nivbrant B, Wood D. Less invasive total hip arthroplasty: description of a new technique. J Arthroplasty. 2006;21(7):1038–1046. doi: 10.1016/j.arth.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 36.Kim YS, Kwon SY, Sun DH, Han SK, Maloney WJ. Modified posterior approach to total hip arthroplasty to enhance joint stability. Clin Orthop Relat Res. 2008;466(2):294–299. doi: 10.1007/s11999-007-0056-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang Y, Tang Y, Zhang C, Zhao X, Xie Y, Xu S. Modified posterior soft tissue repair for the prevention of early postoperative dislocation in total hip arthroplasty. Int Orthop. 2013;37(6):1039–1044. doi: 10.1007/s00264-013-1874-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McGrory BJ, Finch ME, Furlong PJ, Ruterbories J. Incision length correlates with patient weight, height, and gender when using a minimal-incision technique in total hip arthroplasty. J Surg Orthop Adv. 2008;17(2):77–81. [PubMed] [Google Scholar]
- 39.Sculco TP, Boettner F. Minimally invasive total hip arthroplasty: the posterior approach. Instr Course Lect. 2006;55:205–214. [PubMed] [Google Scholar]
- 40.Dienstknecht T, Luring C, Tingart M, Grifka J, Sendtner E. A minimally invasive approach for total hip arthroplasty does not diminish early post-operative outcome in obese patients: a prospective, randomised trial. Int Orthop. 2013;37(6):1013–1018. doi: 10.1007/s00264-013-1833-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Duwelius PJ, Dorr LD. Minimally invasive total hip arthroplasty: an overview of the results. Instr Course Lect. 2008;57:215–222. [PubMed] [Google Scholar]
- 42.Wright JM, Crockett HC, Delgado S, Lyman S, Madsen M, Sculco TP. Mini-incision for total hip arthroplasty: a prospective, controlled investigation with 5-year follow-up evaluation. J Arthroplasty. 2004;19(5):538–545. doi: 10.1016/j.arth.2003.12.070. [DOI] [PubMed] [Google Scholar]