Abstract
Objective. To describe the public health impact of osteoporosis including the magnitude of the problem and important consequences of osteoporotic fractures.
Methods. Literature review of key references selected by author.
Results. Current demographic trends leading to an increased number of individuals surviving past age 65 will result in an increased number of osteoporotic fractures. Important consequences of osteoporotic fractures include an increased mortality that for hip fractures extends to 10 years after the fracture. Increased mortality risk also extends to major and minor fractures, especially, in those over 75 years. Hip and vertebral fractures have important functional consequences and reductions in quality of life. The economic impact of osteoporotic fractures is large and growing. Significant health care resources are required for all fractures.
Conclusions. To alleviate the public and private burden of osteoporosis related fractures, assessment of risk and reduction of individual risk is critical.
Key Words: Bone, Aging, Public health, Osteoporosis
The average age of the world’s population is increasing at an unprecedented rate, and this increase is changing the world. From 2010 to 2040, the world population ≥65 years of age will double from about 506 million in 2008 to 1.3 billion by 2040, accounting for 14% of the world’s total population; those aged 80 or older is projected to double from 2010 until 2050 (1). Developing nations will experience the most rapid increase in the older adult population. This explosion will affect the world and will lead to a greater number of individuals with osteoporosis and increasing number of fractures. It is estimated that at least 50% of hip fractures worldwide will occur in Asia by 2050 (2). This projected number may actually be underestimated, because while hip fracture rates are declining in the United States (3) and Canada (4), rates in Asia may actually be increasing (5).
Magnitude of Problem
In 2005, more than 2 million incident fractures were reported in the United States alone, with a total cost of $17 billion (6). Total costs including prevalent fractures exceeded $19 billion. Vertebral fractures account for 27% of all fractures: wrist fractures, 19%; hip fractures, 14%; and pelvic fractures, 7%. Women account for 71% of all fractures and 75% of all fracture-related costs. Among women, whites account for the majority of all fractures (89%), followed by blacks (4%), Hispanics (4%), and other women (3%). Even if rates stay the same, the aging of the world population is expected to increase the number of fractures and costs in the United States by 48%, to greater than 3 million fractures associated with a cost of $25.3 billion (6).
Fractures beget more fractures. Once an individual has a hip fracture, that individual is at high risk of suffering an additional fracture. Women who suffered an incident hip fracture had a 2.3% per year risk of a second hip fracture (7). Twenty six percent of individuals enrolled in the risedronate clinical trials that had an incident radiographic vertebral fracture, re-fractured within 1 year (new vertebral, 17.4%; hip, 3.6%; “other,” 3.5%; forearm/wrist, 1.0% (8)). In SOF, asymptomatic prevalent vertebral fractures also increased the risk of future hip fractures by almost threefold and any nonvertebral fracture by almost twofold (9). A prevalent vertebral fracture predicted the risk of a second fracture, even after 15 years (10). Thus, in evaluating the overall public health impact of a single fracture one needs to include the high risk of subsequent fractures. A systematic analysis of existing studies showed that history of prior fracture at any site is an important risk factor for future fractures (11).
Results from the U.S. National Health and Nutrition Examination Survey 2005–2008 estimated that the prevalence of low bone mass (T-score −1 to −2.5) at the femoral neck was 50.6%, 33.0%, and 43.9% in non-Hispanic whites, non-Hispanics blacks and Mexican American men, respectively (12). The prevalence of osteoporosis (T-score ≤ −2.5) was 9.6%, 6.0%, and 12.6% in non-Hispanic whites, non-Hispanics blacks and Mexican Americans, respectively. For men, the prevalence of low bone mass at the femoral neck was 32.2%, 18.6%, and 34% in non-Hispanic whites, non-Hispanics blacks, and Mexican American women, respectively (12). The prevalence of osteoporosis (T-score ≤ −2.5) was estimated at 2% for non-Hispanic white men. (All T-scores were calculated using non-Hispanic white women as the referent group). Overall, 19.3% of U.S. men and 30.8% of U.S. women aged 50 or older met the 2008 National Osteoporosis Foundation treatment thresholds (13). Low bone mineral density is related to most fractures (14) even traumatic fractures (15), widening the public health impact of osteoporosis. In a meta-analysis of 9,891 men and 29,082 women from 12 cohorts, the relative risk of all fractures per 1 SD decrease in the Z-score was 1.45 (95% confidence intervals [CI]), 1.39–1.51 (16).
Although the lifetime risk of fractures is lower in non-white women (17–19), the number of fractures is expected to increase largely, reflecting the greater improvements in overall life expectancy in minority women. In addition, although the majority of hip fractures occur in white women, a substantial number of other types of fractures occur in non-white women. For example, in the Women’s Health Initiative, we showed that the projected number of women who will experience a clinical fracture in 1 year exceeded the combined number of women who would experience incident breast cancer, myocardial infarction, or stroke in 1 year in women of all ethnic groups (20). Thus, osteoporosis prevention efforts should target all women irrespective of their race/ethnic background.
Osteoporosis related fractures impose a substantial burden of disability, costs, and mortality on postmenopausal women and older men. A central challenge in assessing the impact of osteoporotic fractures on mortality, disability and costs is distinguishing the effects of the fractures themselves from the comorbidities and other risk factors that contribute to both the fracture and the outcome. Even if studies controlled for the number of comorbidities, this will depend on how many and the specific comorbidities that were assessed. In most cases, studies are unable to adjust for severity of the comorbidity. In studies examining disability or functional outcomes post-hip fracture, most studies had no information on pre-fracture functional status and had to rely on self-report of pre-fracture function from the individual assessed after the fracture.
Mortality
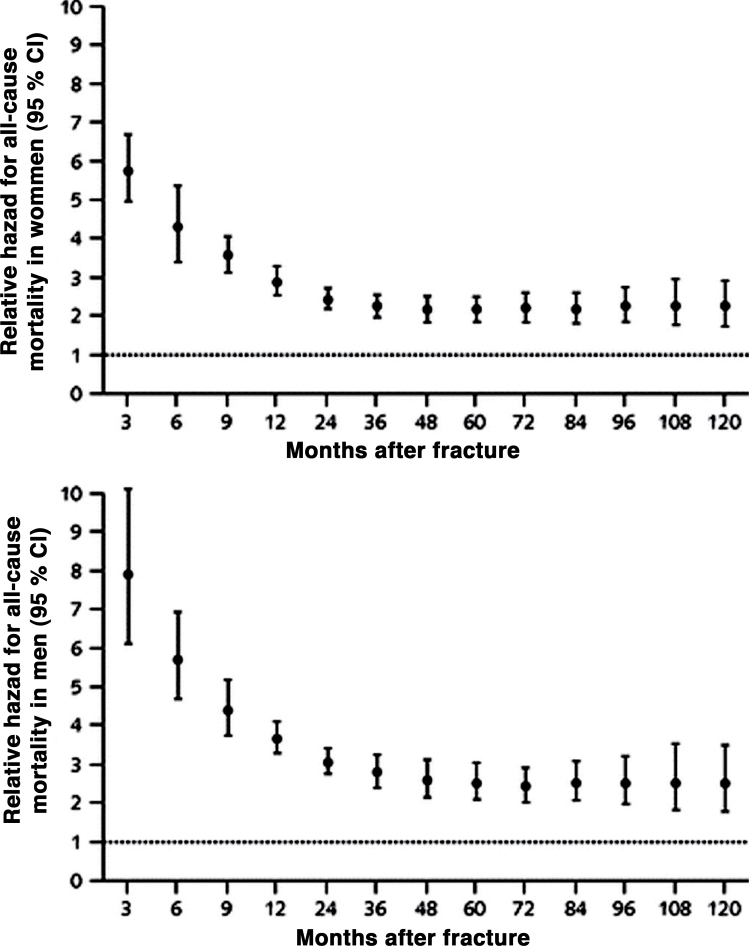
Mortality following hip fracture is a major consequence of osteoporosis. Two recent meta-analyses summarized the data on mortality following a hip fracture (21,22). Each meta-analysis applied different criteria for inclusion. Abrahamsen and coworkers included 54 studies that presented unadjusted mortality data (death as a proportion of the study population) and reported individual study results (20). The meta-analysis of Haentjens and coworkers limited their meta-analysis to 24 studies that met all inclusion criteria that is, prospective, life table approach with survival curves and excluded studies that pooled both genders (21). Pooled relative hazards (RH) are presented with tests for heterogeneity. Of these 24 studies in the Haentjens meta-analysis, 7 were also in the Abrahamsen review. Results of the meta-analyses were, however, remarkably similar. The mortality risk was greatest in the first 3 months after hip fracture, RH=5.75 (95% CI, 4.94–6.67) in women and 7.95 (95% CI, 1.13–10.30) in men (21). The RH of all-cause mortality decreased overtime but even 10 years after hip fracture the RH was elevated, RH=1.96 (95% CI, 1.30–2.95) in women and 1.79 (95% CI, 1.14–2.81) in men, (see Figure 1). The persistent excess mortality past 5 years was not, however, consistently seen in all studies (23,24) Generally, the mortality risk was greater in men than women but the gender difference was greatest in the first year after the hip fracture. Men appear to be at higher operative risk and have more postoperative complications and more comorbidities which may contribute their higher post hip fracture mortality (3,25). The pooled RH for 2 years and 6 years mortality after a hip fracture was 2.89 (95% CI, 2.27–3.68) and 3.83 (95% CI, 3.04–4.82) respectively, in women and 3.23 (95% CI, 1.95–5.36) and 4.99 (95% CI, 3.63–6.89) respectively, in men. Excess mortality following a hip fracture depends largely on age . At any age, excess mortality is greater in men but after age 80, the gender difference starts to decline (22). But, studies that calculated a standardized mortality ratio (SMR) comparing mortality risk following a hip fracture with what would be expected in an age-matched group generally showed that the SMRs tend to be greater in younger individuals because the absolute risk of dying is lower in these younger individuals (21). These studies were carried out in Europe, North and South America, and Australia, with one study from Singapore. There did not appear to be marked geographic variability in the risk of death following a hip fracture.
Figure 1.
Relative hazard of all-cause mortality for women and men with hip fracture versus control groups during a given follow-up period starting at the time of injury.
Solid circles represent the pooled relative hazard. Vertical bars represent the corresponding 95% CIs. The dotted horizontal line is the null effect (22).
Despite lower absolute risks of hip fracture in African Americans, mortality following a hip fracture is greater in blacks compared with white women (26,27). These early reports used Medicare data from the 1980’s but more recent data confirm the higher mortality risk in blacks following a hip fracture (28). The reason for the higher mortality in black following a hip fracture is unknown, but one small study found that the number of comorbid conditions was higher at hospital admission for their hip fracture in blacks compared with whites (29).
Mortality after intertrochanteric hip fractures in a U.S. study was higher at 2 and 6 months after the fracture compared with femoral neck fractures but by 1 year, the percentage of those who died was similar for both types of hip fracture (30). In contrast, a study from Greece suggested that the higher risk of mortality associated with intertrochanteric fractures may persist for up to 10 years (31). The higher mortality rates with intertrochanteric hip fractures may be due to greater frailty before injury, older age and more severe osteoporosis (32,33).
The increased mortality following a hip fracture is likely multifactorial, but comorbidities at the time of the fracture play a major role (34). Less commonly, hip fractures are a direct cause of death. In the Study of Osteoporotic Fractures (SOF), the leading causes of death were coronary heart disease, cancer, and stroke in those both with and without a hip fracture (24). Wehren and coworkers suggested that deaths related to infections (pneumonia, influenza, and septicemia) were greater in men than women and accounted for the observed gender difference in post–hip fracture mortality (35). In SOF, there was no difference between hip fracture cases versus controls for sepsis deaths, but a greater proportion of hip fracture cases compared with controls died of pneumonia (10.5% vs 5.6%. p = <0.001) and cognitive disorders (9.3% vs 6.7%, p = 0.03). In contrast more controls died from cancer (11% vs 18.2%, p = <0.001) (24). Results from Australia also suggested a major impact of infection on short-term mortality in institutionalized persons following a hip fracture (36).
A recent meta-analysis of 64,613 patients identified 12 factors that were associated with an increased risk of mortality following a hip fracture, including advanced age, male gender, nursing home or facility residence, poor preoperative walking capacity, poor activities of daily living (ADLs) preoperatively, higher American Anesthesiologists Society score, poor mental state, more comorbidities, dementia or cognitive impairment, diabetes, cancer, and cardiac disease (37). These prognostic factors are likely not independent of each other, but further understanding of these factors might help to develop intervention strategies to reduce mortality post hip fracture. Of interest, there was conflicting evidence of whether race differentially influences mortality, but the bulk of the studies were in whites with little power to address the race question.
The good news, at least in the United States, is that mortality rates following hip fracture are declining (3). Age and risk (race, region and comorbid conditions) adjusted mortality in women declined from 1985–2005 by 11.9%, 14.9%, and 8.8% for the 30-, 180- and 360-day mortality, respectively. For men, the age and risk adjusted mortality decreased by 21.8%, 25.4%, and 20% for the 30-, 180- and 360-day mortality, respectively. Most of this decline occurred before 1998. Improved surgical and medical management of hip fracture likely contributed to the decline in mortality.
Other types of fracture have been associated with an increased risk of mortality: Vertebral fracture are the most common osteoporotic fracture, but only from one third (38) to one quarter (39) are clinically recognized and few are admitted to hospitals (40). Thus, identifying their mortality risk is more challenging. Excess mortality following both an incident and a prevalent radiographic fractures (41,42) has been reported. Excess mortality varies substantially after a clinical vertebral fracture with 1 year rates ranging from 1.9% to 42% (34). This wide range may affect the relatively small sample sizes in several of these studies. In the Dubbo Study, the SMR was elevated in both men and women following a clinically diagnosed vertebral fracture (43,44). For the most part, mortality risk following a vertebral fracture is lower than observed following a hip fracture. Frailty, comorbidities, smoking and poor physical function contribute to the risk of mortality following a vertebral fracture (44).
The SMR for major fractures (pelvis, distal femur, proximal tibia, three or more simultaneous ribs and proximal femur) in the Dubbo study was 1.65 (95% CI, 1.31–2.08) in women and 2.12 (95% CI, 1.66–2.72) in men after 10 years of fracture (44). Minor fractures (forearm, hand, other rib, lower limb, foot and clavicle) were also associated with an increased risk of death, SMR = 1.42 (95% CI, 1.19–1.70) in women and SMR = 1.33 (95% CI, 0.99–1.80) in men, especially in those aged 75 years and older (44). In SOF, examination of separate fracture sites found no increased mortality following wrist or foot/ankle fractures (45). In Dubbo (44), mortality risk following a subsequent fracture was associated with an increased mortality hazard ratio = 1.91 (95% CI, 1.54–2.37) in women and 2.99 (95% CI, 2.11−4.24), highlighting the need to prevent the subsequent fracture. Predictors of mortality following any fragility fracture included older age, low muscle strength, subsequent fracture, low bone mineral density and smoking history (44).
Functional Outcomes Following Fractures
Disability following hip fractures is well established (46,47). At the time of their hip fracture, 26% of hip fracture patients and age and gender adjusted controls had walking disability; 12%–14% had transferring disability and 6%–8% grooming disability. Twelve and 24 months post hip fracture, 50% of hip fracture patients were walking disabled compared with 21%–29% of controls even after adjusting for age, sex, comorbidities, and pre-fracture functional status. Given the excess disability associated with hip fracture, we would expect 26 additional cases with more disability per 100 persons. Hip fracture patients also showed more transferring and grooming disability than controls. Women who fell more often after their hip fracture reported decreased social participation independent of their physical function (48). Repeated fallers also reported a greater number in depressive symptoms that could have contributed to their decrease of social interactions.
Hip fracture patients are heterogeneous and their functional outcomes depend largely on their age, number of independent instrumental ADLs, and pre-fracture comorbidities, especially whether they have dementia. Of the young old (<75 years) patients who were relatively independent in mobility and instrumental ADLs before fracture, less than 7% were unable to walk after their hip fracture compared with the oldest old patients (≥85 years) who also had dementia where 38% were unable to walk post hip fracture (49). In total, the authors found seven homogeneous subgroups based on characteristics of the patients at the time of hip fracture with measurably different 6-month functional outcomes. Interventions and services could be targeted to the various subgroups to improve outcomes.
A much higher percentage of black women with hip fracture (28%) were non-ambulatory at hospital discharge compared to white women with hip fracture (4%) but this study was based on only 37 hip fractures in black women (29). Graham et al studied 42,479 in-patient rehabilitation patients (92% white; 4% black; 4% Hispanic and 1% Asian) (50). Functional independence at discharge was lower among blacks and Hispanics than whites. Whites were also more likely to walk independently or with help at 6 months compared to not walking at all but there were no racial differences in independence with activities of daily living 6 months after hip fracture (28).
Several interventions and factors have been suggested to improve outcomes after hip fracture, including physical therapy immediately after hip fracture (49), social support (51), positive affect (52), and treatment of vitamin D deficiency (53). A meta-analysis of 23 randomized trials of 898 hip fracture patients suggested that oral protein and energy supplementation after hip fracture may reduce unfavorable outcomes. However, the majority of these trials had major flaws, such as, lack of analyzing outcomes according to intention to treat (54). High quality randomized clinical trials are needed to adequately test this hypothesis (54). A meta-analysis of extended exercise rehabilitation after hip fracture in 11 clinical trials showed that an extended rehabilitation had a significant impact on several measures of physical function, for example, knee extension strength, balance, physical performance test, timed “up and go test” and fast gait speed but not on normal gait speed, ADLs, instrumental ADLs, or the short-form health survey SF-36 (55). The intervention was for 6 months in 4 of these trials and 1 year in 4 trials. Results suggest that long-term interventions can, indeed, improve physical function after a hip fracture. A 12-month randomized clinical trial of an exercise program that included supervised and independently performed aerobic and resistance exercise with increasing intensity had no effect on physical performance: walking, balance, vitality, muscle strength, ADLs or physical and psychosocial functioning (56). This trial was limited to a relatively healthy group of women who had the potential to exercise safely and independently in their home. Thus, the participants may have been too healthy to see an effect on their function. Trials in more frail populations are warranted.
Incident vertebral fractures are also associated with increasing back pain and disability (57) and these associations are not limited to clinical vertebral fractures (57). This is important given that the lifetime risk of a vertebral fracture is higher than that of a hip fracture (58,59). Vertebral fractures also cause chronic back pain, limitations with common ADL, and reduced quality of life (60,61). Women with prevalent radiographic vertebral fractures have also been shown to have a higher rate of hospitalization not related solely to their fracture, HR=1.14 (95% CI, 1.02–1.27) even after adjusting for age, smoking status, physical activity, multiple comorbidities, body mass index, and bone mineral density (62). Quality of life scales can be used to calculate utilities; the utility is a value attached to a specific health state with “0” representing death and “1” representing perfect health. The presence of vertebral fractures and their number and severity were associated with a lower utility score (63).
Both prevalent and incident radiographic vertebral fractures were associated with declining health related quality of life (HRQOL) (64). There was a decrease in HRQOL with increasing number of prevalent vertebral fractures (64,65). As part of the Global Longitudinal Study of Osteoporosis in Women (GLOW), reductions in quality of life were observed especially after hip, spine and upper leg fractures (66). Similar results were reported earlier by Borgstrom et al (67). Indeed, both hip and spine fractures were associated with a lower quality of life after the fracture; however, hip fracture patients showed higher quality of life scores at 4 months and 12 months after their hip fracture than vertebral fracture patients.
Vertebral fractures are also associated with increasing kyphosis but only 36–37% of older persons with the worst kyphosis have vertebral fractures (68, 69). Other contributing causes of kyphosis could include muscle weakness, degenerative disk disease and postural changes. Nevertheless, kyphosis itself has been associated with an increasing decline in physical function (70), worsening mobility (71), injurious falls (72) and fractures (73). Kyphosis was also associated with an increased risk of pulmonary related deaths that was independent of vertebral fractures (74). Of note, vertebroplasty in patients with vertebral compression fractures was associated with improved respiratory function one month later (75).
Although hip fractures results in the highest percentage of subjects with any bed days or limited activity days after a fracture, the mean number of bed days and limited activity days appeared higher with lumbar vertebral fractures (76) compared to hip fracture. Substantial disability was also reported for fractures of the thoracic vertebral, humerus, distal forearm, ankle and foot (76). Recent data from SOF showed that wrist fractures are also accompanied with increasing disability. A wrist fracture increased the odds of having a clinically important functional decline by 48% (77). Thus, the three major osteoporotic fractures have important deleterious effects on physical function and disability and thus influence quality of life. Furthermore, all nonhip, nonspine fractures have a detrimental effect on quality of life (78).
Costs
Direct care costs during the first post fracture year have been estimated to be about $30,000 per patient for hip fracture; $11,300 for other nonvertebral fractures; and $8,380 for vertebral fractures (79). Total number of U.S. fractures and costs will increase over the next several decades, reflecting the growing proportion of Americans aged 50 years and older. Total management costs attributed to low trauma fractures was estimated to be $17 billion in 2003 in the United States. By 2025, treatment costs are estimated to exceed $25 billion (80). The corresponding figure for Europe (2003) is 36 billion euros (81). The Global Longitudinal Study of Osteoporosis showed that nonhip, nonspine fractures by virtue of their fivefold greater number require significantly more health care resources (82). Clinical vertebral fractures resulted in 617 days of hospitalization and 512 days of rehabilitation/nursing home care; hip fractures accounted for 1306 days of hospitalization and 1650 days of rehabilitation/nursing home care. In contrast, nonhip, nonspine fractures resulted in 3805 days in a hospital and 5186 days of rehabilitation/nursing home care.
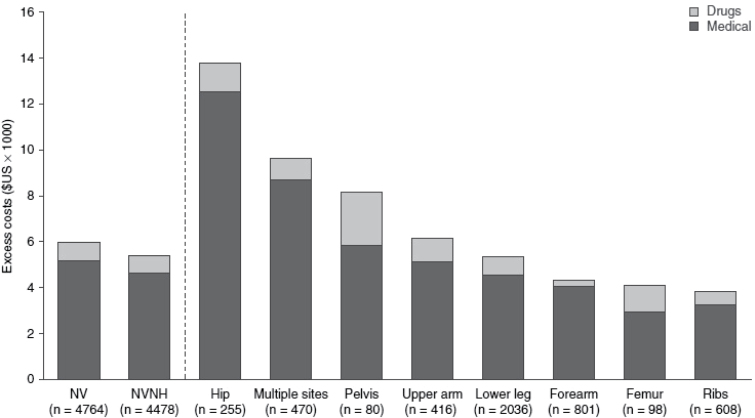
Mean annual direct costs for patients with nonvertebral fracture were estimated in 4764 privately insured individuals age 18–64 years and in 48,742 Medicare beneficiaries (83). Among the privately insured, total annual direct costs (2006 values) were $19,918 in fracture patients compared with $11,290 in controls. Among Medicare patients, the total annual direct costs (2006 values) were $25,906 in fracture patients and $15,147 in controls. Excess costs were highest for hip and multiple site fractures among Medicare enrollees but, even rib fractures were associated with excess costs, Figure 2.
Figure 2.
Excess direct costs (year 2006 values) for Medicare patients and controls with nonvertebral (NV) fractures, 1999–2006 (n = 48 742). Note that lower leg fractures include foot, ankle, tibia, fibula, and patella; forearm fractures include hand, wrist, radius, and ulna; upper arm fractures include humerus, clavicle, and scapula. NVNH = nonvertebral, nonhip.
Hip fracture patients (n = 255) in the privately insured sample had aggregate incremental annual direct costs of $3.5 million to employers compared with $24.1 million for NVNH patients (n = 4478). In the Medicare sample, aggregate incremental annual direct costs for hip fracture patients (n = 7997) were $204.1 million compared with $282.7 million for NVNH patients (n = 35 933) (83).
Thus, nonvertebral fractures impose substantial economic burden on the health care systems. In addition, the excess costs of osteoporosis related nonvertebral fractures extends beyond the first year in which the fracture occurred (84). Thus, significant health care resources are utilized for all fractures, thus, widening the public health impact of osteoporosis.
Direct medical costs of osteoporotic fractures (fractures of the axial skeleton, fractures of the proximal and distal, upper limbs, lower limbs and multiple fractures) and chronic pulmonary obstructive disease, stroke, acute myocardial infarction and heart failure were calculated using 2000 data in Switzerland (85). The number of hospital days for osteoporosis exceeded the number of days for chronic pulmonary obstructive disease, stroke, acute myocardial infarction and heart failure in women: there was greater than a twofold higher number of hospital days for osteoporosis (296,859) compared with chronic pulmonary obstructive disease (125,677) and sevenfold greater number of hospital days than myocardial infarction (40,874). In men, the greatest number of hospitalization days was due to chronic pulmonary obstructive disease (151,152) followed by osteoporosis (88,570).
Summary
In summary, the public health impact of osteoporotic fractures includes major and sustained effects on mortality, substantial increases in functional impairments and deceases in quality of life and lead to increased financial burden on our health care systems. Hip fractures are the most serious consequence of osteoporosis but vertebral fractures are more common and have substantial impact on mortality and morbidity. To alleviate the public and private burden of osteoporosis related fractures, assessment of risk and reduction of individual risk is crucial. Reducing fracture incidence in those who already have osteoporosis will reduce the public health impact of osteoporosis. In addition, identification and treatment of those individuals with low bone mineral density who have a higher risk of fracture will also reduce the burden.
Funding
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140. The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, and R01 AG027576.
References
- 1. Kinsella K, Wan H. International Population Reports, P95/09-1, An Aging World: 2008. Washington, DC: US Census Bureau, US Government Printing Office; 2009. [Google Scholar]
- 2. Cooper C, Cole ZA, Holroyd CR, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22 (5) 1277–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–1579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leslie WD, O’Donnell S, Jean S, et al. Osteoporosis Surveillance Expert Working Group Trends in hip fracture rates in Canada. JAMA. 2009;302:883–889 [DOI] [PubMed] [Google Scholar]
- 5. Xia WB, He SL, Xu L, et al. Rapidly increasing rates of hip fracture in Beijing, China. J Bone Miner Res. 2012;27:125–129 [DOI] [PubMed] [Google Scholar]
- 6. Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475 [DOI] [PubMed] [Google Scholar]
- 7. Chapurlat RD, Bauer DC, Nevitt M, Stone K, Cummings SR. Incidence and risk factors for a second hip fracture in elderly women. The Study of Osteoporotic Fractures. Osteoporos Int. 2003;14:130–136 [DOI] [PubMed] [Google Scholar]
- 8. Lindsay R, Burge RT, Strauss DM. One year outcomes and costs following a vertebral fracture. Osteoporos Int. 2005;16:78–85 [DOI] [PubMed] [Google Scholar]
- 9. Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999;14:821–828 [DOI] [PubMed] [Google Scholar]
- 10. Cauley JA, Hochberg MC, Lui LY, et al. Long-term risk of incident vertebral fractures. JAMA. 2007;298:2761–2767 [DOI] [PubMed] [Google Scholar]
- 11. Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15(4):721–739 [DOI] [PubMed] [Google Scholar]
- 12. Looker AC, Melton LJ, 3rd, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res. 2010;25(1):64–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dawson-Hughes B, Looker AC, Tosteson AN, Johansson H, Kanis JA, Melton LJ., 3rd The potential impact of new National Osteoporosis Foundation guidance on treatment patterns. Osteoporos Int. 2010;21:41–52 [DOI] [PubMed] [Google Scholar]
- 14. Stone KL, Seeley DG, Lui LY, et al. Osteoporotic Fractures Research Group BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res. 2003;18:1947–1954 [DOI] [PubMed] [Google Scholar]
- 15. Mackey DC, Lui LY, Cawthon PM, et al. Study of Osteoporotic Fractures (SOF) and Osteoporotic Fractures in Men Study (MrOS) Research Groups High-trauma fractures and low bone mineral density in older women and men. JAMA. 2007;298:2381–2388 [DOI] [PubMed] [Google Scholar]
- 16. Johnell O, Kanis JA, Oden A, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20:1185–1194 [DOI] [PubMed] [Google Scholar]
- 17. Fang J, Freeman R, Jeganathan R, Alderman MH. Variations in hip fracture hospitalization rates among different race/ethnicity groups in New York City. Ethn Dis. 2004;14(2):280–284 [PubMed] [Google Scholar]
- 18. Baron JA, Karagas M, Barrett J, et al. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7:612–618 [DOI] [PubMed] [Google Scholar]
- 19. Wright NC, Saag KG, Curtis JR, et al. Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res. 2012;27(11):2325–2332 [DOI] [PubMed] [Google Scholar]
- 20. Cauley JA, Wampler NS, Barnhart JM, et al. Women’s Health Initiative Observational Study Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19:1717–1723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20:1633–1650 [DOI] [PubMed] [Google Scholar]
- 22. Haentjens P, Magaziner J, Colón-Emeric CS, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152:380–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tosteson AN, Gottlieb DJ, Radley DC, Fisher ES, Melton LJ., 3rd Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18:1463–1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. LeBlanc ES, Hillier TA, Pedula KL, et al. Hip fracture and increased short-term but not long-term mortality in healthy older women. Arch Intern Med. 2011;171:1831–1837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Poor G, Atkinson EJ, O’Fallon WM, Melton LJ., 3rd Determinants of reduced survival following hip fractures in men. Clin Orthop Relat Res. 1995;319:260–265 [PubMed] [Google Scholar]
- 26. Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992;82:1147–1150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lu-Yao GL, Baron JA, Barrett JA, Fisher ES. Treatment and survival among elderly Americans with hip fractures: a population-based study. Am J Public Health. 1994;84:1287–1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Penrod JD, Litke A, Hawkes WG, et al. The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci. 2008;63(8):867–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Furstenberg AL, Mezey MD. Differences in outcome between black and white elderly hip fracture patients. J Chronic Dis. 1987;40:931–938 [DOI] [PubMed] [Google Scholar]
- 30. Fox KM, Magaziner J, Hebel JR, Kenzora JE, Kashner TM. Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. J Gerontol A Biol Sci Med Sci. 1999;54:M635–M640 [DOI] [PubMed] [Google Scholar]
- 31. Karagiannis A, Papakitsou E, Dretakis K, et al. Mortality rates of patients with a hip fracture in a southwestern district of Greece: ten-year follow-up with reference to the type of fracture. Calcif Tissue Int. 2006;78:72–77 [DOI] [PubMed] [Google Scholar]
- 32. Duboeuf F, Hans D, Schott AM, et al. Different morphometric and densitometric parameters predict cervical and trochanteric hip fracture: the EPIDOS Study. J Bone Miner Res. 1997;12:1895–1902 [DOI] [PubMed] [Google Scholar]
- 33. Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics. Clin Orthop Relat Res. 2004;425: 64–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Teng GG, Curtis JR, Saag KG. Mortality and osteoporotic fractures: is the link causal, and is it modifiable? Clin Exp Rheumatol. 2008;26(5 Suppl 51):S125–S137 [PMC free article] [PubMed] [Google Scholar]
- 35. Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J. Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res. 2003;18:2231–2237 [DOI] [PubMed] [Google Scholar]
- 36. Cameron ID, Chen JS, March LM, et al. Hip fracture causes excess mortality owing to cardiovascular and infectious disease in institutionalized older people: a prospective 5-year study. J Bone Miner Res. 2010;25:866–872 [DOI] [PubMed] [Google Scholar]
- 37. Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43:676–685 [DOI] [PubMed] [Google Scholar]
- 38. Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ., 3rd Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res. 1992;7:221–227 [DOI] [PubMed] [Google Scholar]
- 39. Fink HA, Milavetz DL, Palermo L, et al. Fracture Intervention Trial Research Group What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res. 2005;20:1216–1222 [DOI] [PubMed] [Google Scholar]
- 40. Gehlbach SH, Bigelow C, Heimisdottir M, May S, Walker M, Kirkwood JR. Recognition of vertebral fracture in a clinical setting. Osteoporos Int. 2000;11:577–582 [DOI] [PubMed] [Google Scholar]
- 41. Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220 [DOI] [PubMed] [Google Scholar]
- 42. Kado DM, Duong T, Stone KL, et al. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14:589–594 [DOI] [PubMed] [Google Scholar]
- 43. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882 [DOI] [PubMed] [Google Scholar]
- 44. Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513–521 [DOI] [PubMed] [Google Scholar]
- 45. Browner WS, Pressman AR, Nevitt MC, Cummings SR. Mortality following fractures in older women. The study of osteoporotic fractures. Arch Intern Med. 1996;156:1521–1525 [PubMed] [Google Scholar]
- 46. Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol. 2003;157:1023–1031 [DOI] [PubMed] [Google Scholar]
- 47. Fredman L, Magaziner J, Hawkes W, et al. Female hip fracture patients had poorer performance-based functioning than community-dwelling peers over 2-year follow-up period. J Clin Epidemiol. 2005;58:1289–1298 [DOI] [PubMed] [Google Scholar]
- 48. Miller RR, Ballew SH, Shardell MD, et al. Repeat falls and the recovery of social participation in the year post-hip fracture. Age Ageing. 2009;38:570–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Penrod JD, Litke A, Hawkes WG, et al. Heterogeneity in hip fracture patients: age, functional status, and comorbidity. J Am Geriatr Soc. 2007;55:407–413 [DOI] [PubMed] [Google Scholar]
- 50. Graham JE, Chang PF, Berges IM, Granger CV, Ottenbacher KJ. Race/ethnicity and outcomes following inpatient rehabilitation for hip fracture. J Gerontol A Biol Sci Med Sci. 2008;63(8):860–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cummings SR, Phillips SL, Wheat ME, et al. Recovery of function after hip fracture. The role of social supports. J Am Geriatr Soc. 1988;36:801–806 [DOI] [PubMed] [Google Scholar]
- 52. Fredman L, Hawkes WG, Black S, Bertrand RM, Magaziner J. Elderly patients with hip fracture with positive affect have better functional recovery over 2 years. J Am Geriatr Soc. 2006;54:1074–1081 [DOI] [PubMed] [Google Scholar]
- 53. LeBoff MS, Hawkes WG, Glowacki J, Yu-Yahiro J, Hurwitz S, Magaziner J. Vitamin D-deficiency and post-fracture changes in lower extremity function and falls in women with hip fractures. Osteoporos Int. 2008;19:1283–1290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Avenell A, Handoll HH. A systematic review of protein and energy supplementation for hip fracture aftercare in older people. Eur J Clin Nutr. 2003;57:895–903 [DOI] [PubMed] [Google Scholar]
- 55. Auais MA, Eilayyan O, Mayo NE. Extended exercise rehabilitation after hip fracture improves patients’ physical function: a systematic review and meta-analysis. Phys Ther. 2012;92:1437–1451 [DOI] [PubMed] [Google Scholar]
- 56. Orwig DL, Hochberg M, Yu-Yahiro J, et al. Delivery and outcomes of a yearlong home exercise program after hip fracture: a randomized controlled trial. Arch Intern Med. 2011;171:323–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Nevitt MC, Thompson DE, Black DM, et al. Effect of alendronate on limited-activity days and bed-disability days caused by back pain in postmenopausal women with existing vertebral fractures. Fracture Intervention Trial Research Group. Arch Intern Med. 2000;160:77–85 [DOI] [PubMed] [Google Scholar]
- 58. Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149(11):2445–8 [PubMed] [Google Scholar]
- 59. Harvey N, Dennison E, Cooper C. Osteoporosis: impact on health and economics. Nat Rev Rheumatol 2010;6(2):99–105 [DOI] [PubMed] [Google Scholar]
- 60. Oleksik A, Lips P, Dawson A, et al. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res. 2000;15:1384–1392 [DOI] [PubMed] [Google Scholar]
- 61. Nevitt MC, Ettinger B, Black DM, et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128:793–800 [DOI] [PubMed] [Google Scholar]
- 62. Ensrud KE, Thompson DE, Cauley JA, et al. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc. 2000;48:241–249 [DOI] [PubMed] [Google Scholar]
- 63. van Schoor NM, Ewing SK, O’Neill TW, Lunt M, Smit JH, Lips P. Impact of prevalent and incident vertebral fractures on utility: results from a patient-based and a population-based sample. Qual Life Res. 2008;17:159–167 [DOI] [PubMed] [Google Scholar]
- 64. Silverman SL, Minshall ME, Shen W, Harper KD, Xie S. The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the Multiple Outcomes of Raloxifene Evaluation Study. Arthritis Rheum. 2001;44(11):2611–2619 [DOI] [PubMed] [Google Scholar]
- 64. Sambrook PN, Silverman SL, Cauley JA, et al. Health-related quality of life and treatment of postmenopausal osteoporosis: results from the HORIZON-PFT. Bone. 2011;48(6):1298–1304 [DOI] [PubMed] [Google Scholar]
- 66. Adachi JD, Adami S, Gehlbach S, et al. Impact of prevalent fractures on quality of life: baseline results from the global longitudinal study of osteoporosis in women. Mayo Clin Proc. 2010;85(9):806–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Borgstrom F, Zethraeus N, Johnell O, et al. Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int. 2006;17(5):637–650 [DOI] [PubMed] [Google Scholar]
- 68. Schneider DL, von Muhlen D, Barrett-Connor E, Sartoris DJ. Kyphosis does not equal vertebral fractures: the Rancho Bernardo study. J Rheumatol. 2004;31(4):747–752 [PubMed] [Google Scholar]
- 69. Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Intern Med. 2007;147(5):330–338 [DOI] [PubMed] [Google Scholar]
- 70. Katzman WB, Huang MH, Lane NE, Ensrud KE, Kado DM. Kyphosis and Decline in Physical Function Over 15 Years in Older Community-Dwelling Women: The Study of Osteoporotic Fractures. J Gerontol A Biol Sci Med Sci. 2013. April 30 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Katzman WB, Vittinghoff E, Ensrud K, Black DM, Kado DM. Increasing kyphosis predicts worsening mobility in older community-dwelling women: a prospective cohort study. J Am Geriatr Soc. 2011;59(1):96–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Kado DM, Huang MH, Nguyen CB, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and risk of injurious falls in older persons: the Rancho Bernardo Study. J Gerontol A Biol Sci Med Sci. 2007;62(6):652–657 [DOI] [PubMed] [Google Scholar]
- 73. Huang MH, Barrett-Connor E, Greendale GA, Kado DM. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res. 2006;21(3):419–423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kado DM, Huang MH, Karlamangla AS, Barrett-Connor E, Greendale GA. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: a prospective study. J Am Geriatr Soc. 2004;52(10):1662–1667 [DOI] [PubMed] [Google Scholar]
- 75. Tanigawa N, Kariya S, Komemushi A, Nakatani M, Yagi R, Sawada S. Added value of percutaneous vertebroplasty: effects on respiratory function. AJR Am J Roentgenol. 2012;198(1):W51–W54 [DOI] [PubMed] [Google Scholar]
- 76. Fink HA, Ensrud KE, Nelson DB, et al. Disability after clinical fracture in postmenopausal women with low bone density: the fracture intervention trial (FIT). Osteoporos Int. 2003;14(1):69–76 [DOI] [PubMed] [Google Scholar]
- 77. Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA. Functional decline after incident wrist fractures–Study of Osteoporotic Fractures: prospective cohort study. BMJ. 2010;341:c3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Roux C, Cooper C, Diez-Perez A, et al. Prevalence of osteoporosis and fractures among women prescribed osteoporosis medication in five European countries: the POSSIBLE EU study. Osteoporos Int. 2011;22(4):1227–1236 [DOI] [PubMed] [Google Scholar]
- 79. Tosteson AN, Melton LJ, 3rd, Dawson-Hughes B, et al. Cost-effective osteoporosis treatment thresholds: the United States perspective. Osteoporos Int. 2008;19(4):437–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. National Osteoporosis Foundation America’s bone health: the state of osteoporosis and low bone mass in our nation In: Washington DC; 2002; p. 1–55 [Google Scholar]
- 81. Kanis JA, Johnell O. Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int. 2005;16(3):229–238 [DOI] [PubMed] [Google Scholar]
- 82. Ioannidis G, Flahive J, Pickard L, et al. Non-hip, non-spine fractures drive healthcare utilization following a fracture: the Global Longitudinal Study of Osteoporosis in Women (GLOW). Osteoporos Int. 2013;24(1):59–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Pike C, Birnbaum HG, Schiller M, Sharma H, Burge R, Edgell ET. Direct and indirect costs of non-vertebral fracture patients with osteoporosis in the US. Pharmacoeconomics. 2010;28(5): 395–409 [DOI] [PubMed] [Google Scholar]
- 84. Pike CT, Birnbaum HG, Schiller M, Swallow E, Burge RT. Edgell ET. Prevalence and costs of osteoporotic patients with subsequent non-vertebral fractures in the US. Osteoporos Int. 2011;22(10): 2611–2621 [DOI] [PubMed] [Google Scholar]
- 85. Lippuner K, Golder M, Greiner R. Epidemiology and direct medical costs of osteoporotic fractures in men and women in Switzerland. Osteoporos Int. 2005;16 Suppl 2:S8–S17 [DOI] [PubMed] [Google Scholar]