Abstract
Background
Cryptococcal infection occurs in HIV-seropositive patients and is associated with high mortality. However, limited information is available on the prevalence and outcomes of cryptococcal antigenemia among hospitalized HIV-seropositive patients in sub-Saharan Africa.
Objectives
To determine the prevalence of and risk factors for cryptococcal antigenemia among HIV-seropositive patients presenting to Mulago Hospital (Kampala, Uganda) with unexplained cough ≥2 weeks and suspected TB, and also to determine if antigenemia is associated with an increased mortality.
Methods
Between September 2009 and September 2010, we enrolled consecutive HIV-seropositive adults hospitalized at Mulago Hospital with cough ≥2 weeks and suspected TB. Banked serum was tested for cryptococcal antigen. We compared demographic, clinical characteristics and 2-month mortality in patients with and without cryptococcal antigenemia.
Results
Of 563 HIV-seropositive patients, 32 (5.7%) were CrAg-positive. None had Cryptococcus neoformans detected on fungal culture of BAL fluid (n=116). CrAg-positive patients had a lower median CD4-count compared to CrAg-negative patients (25 vs. 55 cells/uL, p=0.02) and a substantial proportion of CrAg-positive patients also had concurrent TB (31%). A positive CrAg test was not associated with increased mortality during the 2-month follow-up period (HR: 0.99, 95% CI: 0.63–1.54, p=0.95) after adjusting for CD4 count and ART use at enrollment and/or follow-up.
Conclusions
Occult cryptococcal antigenemia occurs commonly among hospitalized HIV-seropositive patients with suspected TB. CrAg testing should be considered in hospitalized, HIV-seropositive patients with CD4 count <50 cells/uL, coupled with longer follow-up to evaluate the diagnostic value of CrAg and therapeutic interventions in patients with asymptomatic cryptococcal antigenemia.
Keywords: Cryptococcus neoformans, antigenemia, tuberculosis, HIV, AIDS
INTRODUCTION
Cryptococcosis is a serious fungal infection that is a common cause of meningitis and death among patients with advanced human immunodeficiency virus (HIV) infection. Pneumonia with or without accompanying meningitis and isolated cryptococcal antigenemia are also common presentations. Recent estimates suggest that there are about 1 million new cases and at least 500,000 deaths annually due to HIV-associated cryptococcosis worldwide [1]. In more affluent countries, the incidence of HIV-associated cryptococcosis has decreased dramatically since the introduction of antiretroviral therapy (ART) [2], and mortality associated with this disease is generally <10%. Although the incidence has also decreased in sub-Saharan Africa with the increased use of ART [3], cryptococcosis remains a significant cause of morbidity and mortality [4].
The burden of cryptococcosis has previously been reported to be particularly high in patients with or suspected of having pulmonary TB. In South Africa, cryptococcal disease was associated with 75% of deaths from opportunistic infections in gold miners with pulmonary tuberculosis [5]. However, few previous studies have evaluated the burden and impact of cryptococcosis among hospitalized HIV-seropositive TB suspects in sub-Saharan Africa.
In sub-Saharan African settings, hospitalized HIV-seropositive patients without neurological symptoms are rarely tested or treated for cryptococcosis. Thus, the diagnosis may be missed in patients with isolated cryptococcal antigenemia. We hypothesized that unrecognized cryptococcosis may be prevalent in this population and may contribute to early mortality.
Therefore, we performed cryptococcal antigen testing on banked serum specimens from consecutive HIV-seropositive adult patients (≥18 years) with suspected tuberculosis (defined as a cough ≥2 weeks) at Mulago Hospital in Kampala, Uganda, who had been enrolled between September 2009 and September 2010. These patients were not suspected of cryptococcosis by their treating clinicians. Our objectives were to determine the prevalence and risk factors associated with cryptococcal antigenemia among HIV-seropositive patients presenting with cough. We also determined if cryptococcal antigenemia is associated with an increased mortality.
METHODS
Participants and procedures
The current study is a sub-study of the International HIV-associated Opportunistic Pneumonias (IHOP) Study, a prospective observational cohort. The general study protocol has been previously described in detail [6, 7]. In brief, patients provided written informed consent and were interviewed to obtain demographic and clinical data. Chest radiographs and blood were obtained at enrollment. Blood was used for HIV testing and, if HIV-positive, for CD4+ T-lymphocyte count measurement. Patients submitted two sputum specimens (1 spot and 1 early morning) for acid-fast bacilli (AFB) smear and culture on Lowenstein-Jensen media, and those with negative sputum AFB results (using Ziehl Neelsen method) were referred for bronchoscopy with bronchoalveolar lavage (BAL). Bronchoscopy included inspection for endobronchial Kaposi sarcoma (KS). BAL fluid was examined for mycobacteria, Pneumocystis jirovecii (using modified Giemsa, Diff Quik method), Cryptococcus neoformans and other fungi (using Sabouraud medium). The follow-up period was two months after enrollment to assess vital status. After this 2-month follow-up period, final diagnoses were assigned by 2 study doctors according to pre-specified criteria (SDC Appendix 1), which included TB culture results, response to treatment, and other previously collected data [6, 7].
At time of enrollment, 3–4 mL of blood was collected from each patient into a vacutainer tube with clot activator and processed for serum as follows: blood was allowed to clot at room temperature for 30 minutes and centrifuged at 3000 RPM for 5 minutes. The resulting serum was used to confirm HIV status (200 µL) and the remainder (0.5–1.0 mL) was promptly transferred into cryovials and stored at −20°C. For this study, banked serum was thawed and tested for cryptococcal antigen.
Serum CrAg testing
CrAg testing was performed by a single individual (AA) who was blinded to all clinical and microbiologic data. CrAg testing was performed using a commercially-available test kit (Immuno-Mycologics, Inc. OK, USA) according to the manufacturer’s instructions. Testing included positive and negative controls with each batch, and testing was repeated if the results were indeterminate (i.e., failed positive or negative control). The qualitative test result was interpreted as non-reactive (negative) if it showed a smooth, milky suspension with absence of agglutination, and reactive (positive) if it showed distinct large clumps against a clear or lightly milky background or small but definite clumps against a milky background. CrAg titers were subsequently obtained in reactive specimens using standard serial dilutions. The titer of a particular sample was taken to be the highest dilution that showed agglutination.
Sample size determination and data analysis
The first objective of this study (to determine the prevalence of cryptococcal co-infection in HIV seropositive patients with suspected TB in Mulago Hospital) was used for the sample size and precision estimates. An 8% prevalence was reported in a cohort of adult ART-naive AIDS patients who were subsequently started on ART in Kampala, Uganda [8]. Using the Kish and Leslie formula [9], 452 serum samples would provide a prevalence estimate with 90% precision and a 95% confidence interval. However, to further increase our precision, we elected to analyze all 563 available banked serum samples from our HIV-seropositive patients.
Data analysis was performed using STATA release 10 (Stata Corporation, College Station, Texas, USA). We compared categorical variables using the chi-squared or Fisher’s exact tests, and continuous variables using Student’s t-test or the Mann–Whitney rank sum test. We performed backwards multivariate logistic regression analysis to determine factors associated with cryptococcal antigenemia. Variables that did not contribute significantly to the model, defined as a p-value less than 0.05, were removed from the model. We conducted survival analysis to determine whether cryptococcal antigenemia is independently associated with mortality. We controlled for both CD-4 count and ART use, variables that are known to impact survival. We defined significance in reference to the probability of a 2-tailed, type I error (p-value) less than 0.05.
Ethical considerations
Written informed consent was obtained from study participants and included permission to use banked specimens collected at enrollment for future studies. The Makerere University Faculty of Medicine Research and Ethics Committee, the Mulago Hospital Institutional Review Board, the Uganda National Council for Science and Technology, and the University of California San Francisco Committee on Human Research approved the protocol.
RESULTS
Patient characteristics
Of 753 adult patients with cough ≥2 weeks and suspected TB who were enrolled, 563 tested positive for HIV antibodies and had banked serum available for this study (Figure 1). Two-month follow-up data was available for 430 patients. There were no significant differences between patients with and patients without 2-month follow-up data available for the following variables: gender (p=0.71), median age (p=0.35), median CD4-count (p=0.24), ART use on admission (p=0.88), cotrimoxazole prophylaxis use on admission (p=0.20), fever (p=0.87), weight loss >5 kg (p=0.76), dyspnea (p=0.78), or a final diagnosis of TB (p=0.12). Compared with patients who completed the 2-month follow-up period, patients who were lost to follow-up less often knew their HIV status at enrollment (59% vs. 69%, p=0.04) and more often had an unknown diagnosis for their cough (44% vs. 19%, p<0.001).
Figure 1.
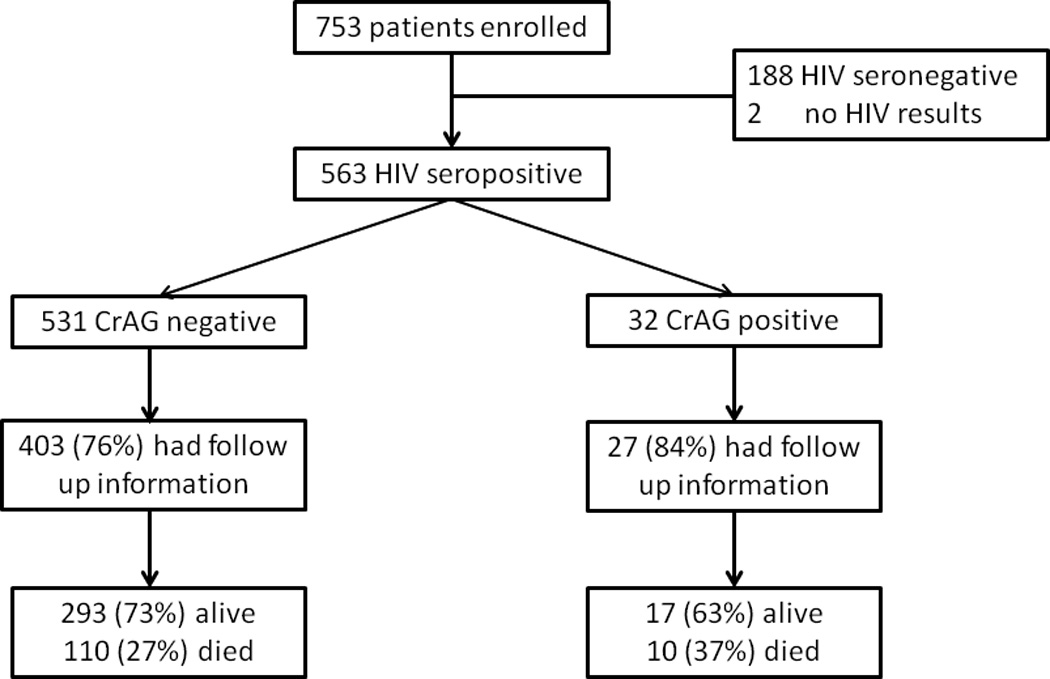
Study Population
Of the 563 HIV-seropositive patients who were included in this study, the majority were female (n=301, 53%) and young (median age=33 years, interquartile range, IQR=28–40 years) (Table 1). Approximately two-thirds (66%) were known to have HIV infection at the time of their presentation and the remaining one-third had HIV infection diagnosed during this hospitalization. Most patients had advanced HIV disease (median CD4-count=51 cells/uL, IQR=16–171 cells/uL). Despite this, only 28% (n=104) of the 375 patients known to have HIV infection were receiving antiretroviral therapy at the time of presentation; 73% (n=273) were receiving co-trimoxazole for PCP prophylaxis and none were receiving fluconazole. The majority of patients presented with fever (88%), weight loss >5 kg (73%), and dyspnea (56%). Cough, which was an inclusion criterion for the prospective study, was present in 100%. In most cases, these non-specific complaints were determined to be due to tuberculosis (60%). Other common diagnoses included bacterial pneumonia (11%), PCP (1%) and pulmonary Kaposi’s sarcoma (2%). A substantial proportion of patients had an unknown final diagnosis (17%).
Table 1.
Demographic and Clinical Characteristics
| Characteristic | Total (N=563) |
CrAg Positive (N=32) |
CrAg Negative (N=531) |
p- value |
|---|---|---|---|---|
| Demographics | ||||
| Female gender | 301 | 16 (50%) | 285 (54%) | 0.69 |
| Median age (years) | 33 (28–40) | 36 (29–41) | 33 (28–39) | 0.42 |
| HIV History | ||||
| Prior known HIV infection | 375 | 17 (53%) | 358 (67%) | 0.10 |
| Median CD4-count (cells/uL) | 51 (16–171) | 25 (8–77) | 55 (18–172) | 0.02 |
| ART on admission | 104 | 4 (13%) | 100 (19%) | 0.37 |
| Co-trimoxazole on admission | 273 | 13 (41%) | 260 (49%) | 0.36 |
| Fluconazole on admission | 0 | 0 | 0 | NA |
| Fluconazole at discharge * | 6 | 2 (7%) | 4 (1%) | 0.002 |
| Presenting symptoms** | ||||
| Fever | 493 | 29 (91%) | 464 (87%) | 0.59 |
| Weight loss >5 kg | 409 | 21 (66%) | 388 (73%) | 0.36 |
| Dyspnea | 315 | 18 (56%) | 297 (56%) | 0.97 |
| Final diagnosis | ||||
| Tuberculosis | 337 | 10 (31%) | 327 (62%) | 0.001 |
| Unknown diagnosis | 96 | 8 (25%) | 88 (16%) | 0.22 |
Data presented as number (%) or median (interquartile range)
Fluconazole use at discharge only known for 520 patients
Cough present in 100% (parent study inclusion criteria)
Prevalence of and risk factors for cryptococcal antigenemia
Overall, 32 (5.7%) of the 563 patients had a positive CrAg test. Among the 116 patients who underwent bronchoscopy, none had Cryptococcus neoformans detected on fungal culture of BAL fluid. Thus, if CrAg testing had been done prospectively, the positive serum CrAg result would have represented the sole diagnosis for cryptococcal disease.
All patients with a positive CrAg had a CD-4 count less than 200 cells/uL. The CrAg-positive patients had a lower median CD4-count (25 cells/uL, interquartile range, (IQR): 8–77 cells/uL) compared to those who had a negative CrAg test (55 cells/uL, IQR: 18–172 cells/uL, p=0.02) (Table 1). A substantial proportion of CrAg-positive patients had concurrent TB (31%) and thus, TB is a frequent co-pathogen in patients with cryptococcemia. The proportion of CrAg-positive patients who had TB was lower than the proportion in CrAg-negative patients (31% vs. 62%, p=0.001). Other clinical factors including gender, age, prior diagnosis of HIV infection, and taking ART or co-trimoxazole prophylaxis at admission were all not associated with a positive CrAg test. Presenting symptoms were also similar in CrAg-positive and CrAg-negative patients. In the final multivariate model, a CD4-count of <50 cells/µL was significantly associated with increased odds of cryptococcal antigenemia (adjusted Odds Ratio=2.38, p=0.034) while a diagnosis of tuberculosis was associated with a lower odds of antigenemia (adjusted Odds Ratio=0.24, p=0.001) (Table 2).
Table 2.
Risk factors for cryptococcal antigenemia
| Characteristic | Univariate OR (95% CI) |
Adjusted OR (95% CI) |
p-value |
|---|---|---|---|
| Female | 0.86 (0.40–1.89) | - | - |
| Age >33 | 1.66 (0.75–3.80) | - | - |
| Prior known HIV | 0.55 (0.25–1.21) | - | - |
| CD4 count <50 | 2.00 (0.90–4.76) | 2.38 (1.11–5.26) | 0.034 |
| ART use | 0.62 (0.15–1.82) | - | - |
| Co-trimoxazole use | 0.71 (0.32–1.56) | - | - |
| Tuberculosis | 0.28 (0.12–0.64) | 0.24 (0.11–0.52) | 0.001 |
| Unknown diagnosis | 1.68 (0.63–4.01) | - | - |
Overall, 10 CrAg-positive patients were diagnosed with TB and eight were classified as having an unknown final diagnosis but potentially having disseminated cryptococcal infection as the etiology of their presentation. In the absence of a specific diagnosis of cryptococcosis, 6 patients (2 CrAg-positive and 4 CrAg-negative) were treated with fluconazole during hospitalization because they had oral thrush or possible esophageal candidiasis, and were discharged on this medication. CrAg-positive patients were more often initiated on empiric fluconazole treatment during their hospitalization compared to CrAg-negative patients (7% vs. 1%, p=0.002).
Cryptococcal antigenemia and factors associated with 2-month mortality
Among the 430 patients with 2-month follow-up data available, 310 (72.1%) were found to be alive and 120 (27.9%) were determined to have died (Figure 1). Of the CrAg-positive patients, 37% had died at 2-month follow-up compared to 27% of the CrAg-negative patients, but this difference was not statistically significant (p=0.28). In survival analysis, there was no significant difference between CrAg-positive and CrAg-negative patients in time to death (Figure 2, p=0.47). In bivariate analysis, we did not find a significant association between CrAg positivity and 2-month mortality (HR: 1.0, 95% CI: 0.64–1.55, p=1.0), although we could not exclude the possibility of a clinically important increase or decrease in mortality because of the imprecision of our estimate. After adjusting for CD4-count, ART use at admission and/or follow-up, and TB diagnosis and/or unknown diagnosis, the association between CrAg result and mortality remained non-significant (HR: 0.99, 95% CI: 0.63–1.54, p=0.95).
Figure 2.
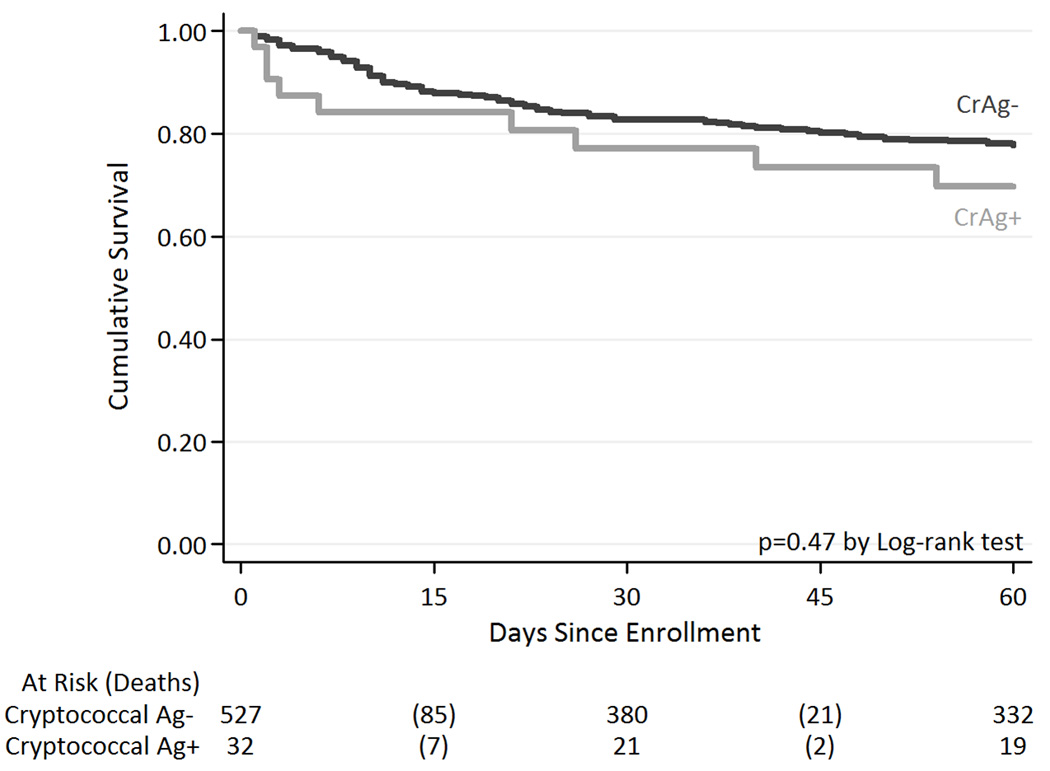
Among patients with a positive CrAg test, we compared mortality in 21 patients with low titers (titer ≤1:512) with mortality in 11 patients with high titers (titer >1:512). CrAg titer was not significantly associated with mortality in bivariate analysis (HR: 0.58, 95% CI: 0.17–1.97, p=0.38) nor after adjusting for CD4-count, ART use at admission and/or follow-up, and TB diagnosis and/or unknown diagnosis (HR: 1.02, 95% CI: 0.22–4.79, p=0.98).
DISCUSSION
In this study, we found an overall cryptococcal antigenemia prevalence of 5.7% in HIV-infected adults hospitalized at Mulago Hospital (Kampala, Uganda) with cough ≥2 weeks and suspected tuberculosis. None of the 116 patients who underwent bronchoscopy as part of their diagnostic evaluation had Cryptococcus neoformans detected on fungal culture of BAL fluid. We did not identify a difference in mortality or time to death between CrAg-positive and CrAg-negative patients at 2 months of follow-up.
The moderate prevalence of cryptococcosis observed in this cohort is lower than that reported among hospitalized patients in South Africa and Cambodia [10, 11] where cryptococcal antigenemia prevalence was reported to be 13% and 20%, respectively. The lower rates that we observed may be due to the fact that the majority of patients enrolled in these previous studies were terminally ill and had symptoms of cryptococcosis. In contrast, our study selected a different population: although hospitalized, patients in our cohort did not have Cryptococcus-specific symptoms and were not clinically suspected to have cryptococcal infection. Furthermore, patients with an altered mental status or confusion were excluded from our study because they were unable to provide informed consent for study participation. Therefore, patients with symptomatic cryptococcal neurologic disease would not have been enrolled. Surprisingly, the prevalence that we noted in our hospitalized cohort was comparable to cryptococcal antigenemia prevalences previously described among asymptomatic HIV-seropositive outpatients in Uganda. In the Infectious Diseases Institute in Kampala and in a rural community clinic setting in Tororo, cryptococcal antigenemia prevalences were 8% and 5.8%, respectively [8, 12].
None of the CrAg-positive patients who underwent bronchoscopy in our prospective study were diagnosed with concurrent cryptococcal pneumonia. This finding was unexpected as we found Cryptococcus neoformans in 11.4% of HIV-infected patients undergoing bronchoscopy in a previous cohort (September 2007 through July 2008) of 132 patients with cough ≥2 weeks and suspected tuberculosis [6]. Nevertheless, our findings demonstrate that cryptococcal antigenemia can occur in the absence of cryptococcal pneumonia based on BAL culture results.
Even in the absence of diagnosis and specific treatment of cryptococcosis, CrAg-positive patients in our cohort were not more likely to die before 2-month follow-up than CrAg-negative patients. These findings differ from other studies that reported on HIV-positive patients with and without cryptococcal antigenemia. Jarvis and colleagues reported on patients accessing an ART program in South Africa and found that CrAg-positive patients were at far higher risk of mortality than antigen-negative patients during a one-year follow-up period (HR=4.75, 95% CI 2.6–8.8, p<0.001) [10]. Similarly, French et al reported a poor survival of patients after diagnosis of cryptococcal antigenemia (median survival 26 days, range 0–138 days), though this study was done in the period before ART was available in Africa [3]. The fact that we failed to show an association with mortality may be because we had a relatively small sample size and a comparatively short follow-up period.
Overall, CrAg testing identified 32 patients with cryptococcal antigenemia, including 10 with concurrent TB and eight classified as having an unknown final diagnosis but potentially having disseminated cryptococcal infection as the etiology of their presentation. In these individuals, CrAg testing at the time of presentation may have been beneficial. However, evaluation of the possible benefits of such an intervention requires an understanding of the clinical course of patients with cryptococcal antigenemia. Cryptococcal antigenemia in the context of advanced HIV infection has been assumed to indicate disseminated disease and the progression to symptomatic cryptococcosis has been thought to be inevitable unless appropriate anti-fungal treatment is given [13, 14]. During our relatively short 2-month follow-up period, we were unable to confirm symptomatic cryptococcosis in any of these individuals, and it is unclear whether a longer follow-up period would have detected subsequent progression in these individuals.
Despite the lack of association between cryptococcal antigenemia and mortality in our study, the preponderance of evidence suggests that prospective testing for cryptococcal antigenemia in severely immunosuppressed HIV-seropositive patients with suspected TB in the absence of prior cryptococcal disease should have a role in the diagnostic evaluation. With the new point-of-care lateral flow assay (LFA) for cryptococcal antigen, this testing could even be performed at peripheral health facilities that the majority of patients visit prior to hospitalization [15]. In addition, such testing with subsequent intervention may prevent unmasking of subclinical cryptococcal infection that could present as meningitis or pneumonitis after ART initiation. Screening for serum cryptococcal antigen is highly sensitive and specific [16], and Meya et al., described the cost benefit of this strategy in preventing death in HIV-infected patients with CD4 counts ≤100 cells/µL [8]. This screening strategy may also be beneficial in hospital-based cohorts such as ours that are composed of HIV-infected patients with advanced immunosuppression and high 2-month mortality [7].
Our study had limitations. First, the screening test used (CrAg) does not differentiate between acute and old infections. Cryptococcal antigen can persist in the blood up to 48 months after successful treatment for cryptococcosis [17]. It is therefore possible that some of the patients who tested positive might have had prior cryptococcal infection, since we mainly relied on patient recall to rule out any history of cryptococcal infection and fluconazole use. That said, none of the patients reported current fluconazole use at the time of hospital admission. Second, the short period (two months) of follow-up, and the fact that the CrAg analyses were conducted six months after the last patient was seen made it impossible to determine if the cases we identified were either disseminated cryptococcal infection that progressed or transient pneumonitis but with negative BAL cultures.
In summary, we report a moderately high prevalence (5.7%) of cryptococcal antigenemia among HIV-infected patients who were hospitalized with suspected TB. Cryptococcal disease was not suspected in these patients prior to CrAg testing and none of the CrAg-positive patients who underwent bronchoscopy had concurrent cryptococcal pneumonia diagnosed. As a result, the positive CrAg test may have represented the sole diagnosis of disseminated cryptococcal infection and our results suggest a potential role for serum CrAg screening in this hospitalized population. No significant association between CrAg positivity and 2-month mortality among patients suspected of TB was established but longer-term follow-up studies are needed.
Supplementary Material
Acknowledgments
We would like to thank Sylvia Kaswabuli, Patrick Byanyima, John Kiidha, Rachel Kyeyune and Leatitia Kampiire for enrolling and caring for the patients included in this study. We would also like to thank the Mulago Hospital administration and staff for their approval and support of the research.
Financial Support: This work was supported by grant numbers K24 HL087713 (LH), R01 HL 090335 (LH), U01 AI089244-01 (COAT study), K23 AI080147 (JLD) from the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None
References
- 1.Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23:525–530. doi: 10.1097/QAD.0b013e328322ffac. [DOI] [PubMed] [Google Scholar]
- 2.CDC. Cryptococcosis. 2000 [Google Scholar]
- 3.French N, Gray K, Watera C, Nakiyingi J, Lugada E, Moore M. Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. AIDS. 2002;16:1031–1038. doi: 10.1097/00002030-200205030-00009. [DOI] [PubMed] [Google Scholar]
- 4.Kambugu A, Meya DB, Rhein J, O'Brien M, Janoff EN, Ronald AR, Kamya MR. Outcomes of cryptococcal meningitis in Uganda before and after the availability of highly active antiretroviral therapy. Clin Infect Dis. 2008;46(11):1694–1701. doi: 10.1086/587667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Churchyard GJ, Kleinschmidt I, Corbett EL, Murray J, Smit J, de Cock KM. Factors associated with an increased case-fatality rate in HIV-infected and non-infected South African gold miners with pulmonary tuberculosis. Int J Tuberc Lung Dis. 2000;4:705–712. [PubMed] [Google Scholar]
- 6.Yoo SD, Worodria W, Davis JL, Cattamanchi A, den Boon S, Kyeyune R, Kisembo H, Huang L. The Prevalence and Clinical Course of HIV-Associated Pulmonary Cryptococcosis in Uganda. J Acquir Immune Defic Syndr. 2010;54:269–274. doi: 10.1097/QAI.0b013e3181ce6b19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kyeyune R, den Boon S, Cattamanchi A, Davis JL, Worodria W, Yoo SD, Huang L. Causes of early mortality in HIV-infected TB suspects in an East African referral hospital. J Acquir Immune Defic Syndr. 2010;55(4):446–450. doi: 10.1097/qai.0b013e3181eb611a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meya DB, Munabe YC, Castelnuovo B, Bethany AC, Ali ME, Kambugu A. Cost-Effectiveness of Serum Cryptococcal Antigen Screening to Prevent Deaths among HIV-Infected Persons with a CD4+ Cell Count _100 Cells/mL Who Start HIV Therapy in Resource-Limited Settings. Clinical Infectious Diseases. 2010;51(4):448–455. doi: 10.1086/655143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kish, Leslie . Survey Sampling. New York: John Wiley and Sons, Inc.; 1965. [Google Scholar]
- 10.Jarvis JN, Lawn SD, Vogt M, Bangani N, Wood R, Harrison TS. Screening for cryptococcal antigenemia in patients accessing an antiretroviral treatment program in South Africa. Clin Infect Dis. 2009;48(7):856–862. doi: 10.1086/597262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Micol R, Lortholary O, Sar B, Laureillard D, Ngeth C, Dousset JP. Prevalence, determinants of positivity, and clinical utility of cryptococcal antigenemia in Cambodian HIV-infected patients. J Acquir Immune Defic Syndr. 2007;45(5):555–559. doi: 10.1097/QAI.0b013e31811ed32c. [DOI] [PubMed] [Google Scholar]
- 12.Liechty CA, Solberg P, Were W, Ekwaru JP, Ransom RL, Weidle PJ. Asymptomatic serum cryptococcal antigenemia and early mortality during antiretroviral therapy in rural Uganda. Trop Med Int Health. 2007;12(8):929–935. doi: 10.1111/j.1365-3156.2007.01874.x. [DOI] [PubMed] [Google Scholar]
- 13.Feldmesser M, Harris C, Reichberg S, Khan S, Casadevall A. Serum cryptococcal antigen in patients with AIDS. Clin Infect Dis. 1996;23(4):827–830. doi: 10.1093/clinids/23.4.827. [PubMed: 8909854]. [DOI] [PubMed] [Google Scholar]
- 14.Yuen C, Graziani A, Pietroski N, Macgregor R, Schuster M. Cryptococcal antigenemia in HIV-infected patients. Clin Infect Dis. 1994;19:579. [abstract no. 93] [Google Scholar]
- 15.Lindsley MD, Mekha N, Baggett HC, Surinthong Y, Autthateinchai R, Sawatwong P, Harris JR, Park BJ, Chiller T, Arunmozhi SB, Poonwan N. Evaluation of a Newly Developed Lateral Flow Immunoassay for the Diagnosis of Cryptococcosis. Clin Infect Dis. 2011;(4):321–325. doi: 10.1093/cid/cir379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uwe KF, Nishimura SL, Li NC, Sugai K, Majko DM, Hadly K, NG VL. Evaluation of an Enzyme Immunoassay for Detection of Cryptococcal Capsular Polysaccharide Antigen in Serum and Cerebrospinal Fluid. Journal of Clinical Microbiology. 1993;31(1):97–101. doi: 10.1128/jcm.31.1.97-101.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lortholary O, Poizat G, Zeller V, Neuville S, Boibieux A, Alvarez M, Dellamonica P, Botterel F, Dromer F, Chêne G. Long-term outcome of AIDS-associated cryptococcosis in the era of combination antiretroviral therapy. AIDS. 2006;20(17):2183–2191. doi: 10.1097/01.aids.0000252060.80704.68. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


