Abstract
Compared with non-Hispanic Whites, Hispanics experience a disproportionate burden of chronic diseases. Understanding the factors influencing the success of health programs in Hispanics requires a clearer examination of the principles and components of tailored interventions. This research comprises a comprehensive literature review of randomized controlled trials testing nutrition and exercise interventions tailored for Hispanics and an examination of how these interventions were constructed. The review of 18 interventions meeting study criteria suggests that most tailored programs promoting nutrition and exercise in Hispanics are theory driven and are informed by formative research. Also, the findings indicate that salient culturally sensitive intervention components are (a) bilingual and bicultural facilitators and materials, (b) family-based activities, (c) literacy-appropriate materials, and (d) social support. A clear understanding of Hispanic cultural values is also required. Further empirical examination is warranted to determine the factors mediating or predicting the efficacy of culturally sensitive health programs for Hispanics.
Keywords: cultural, Hispanics, nutrition, exercise, interventions
Nutrition and regular exercise are major pillars of healthy living and aging because they reduce the risk of heart attack, colon cancer, diabetes, high blood pressure, and stroke (World Health Organization, 2007). Healthy lifestyle behaviors also help control weight; contribute to healthy bones, muscles, and joints; reduce depression and anxiety; and are associated with fewer hospitalizations and medications (Ignarro, Balestrieri, & Napoli, 2007; Kanaya & Narayan, 2003; Kriska, Delahanty, & Pettee, 2004). Despite the well-documented benefits of diet and exercise and the fact that the health status of Americans improved considerably in the past decades, the health of racial and ethnic minorities continues to lag behind that of Whites (Institute of Medicine, 2006; Liao et al., 2004). In particular, compared with non-Hispanic Whites, Hispanics report higher morbidity and mortality rates due to chronic diseases (e.g., diabetes, stroke, liver disease, and cirrhosis; Centers for Disease Control and Prevention, 2004) that could be prevented or their impact lessened by the promotion of healthy lifestyle behaviors in this population (Institute of Medicine, 2001).
The persistence of health disparities requires the adoption of a more culturally sensitive approach to illness prevention and behavioral intervention efforts that go beyond the mandated inclusion of women and minorities in health research (Caban, 1995). Health interventions adapted to the social and cultural context of ethnic minority populations are more likely to increase behavioral interventions’ external validity (Bernal, Bonilla, & Bellido, 1995) and to accelerate advances in minority health (Cooper, Hill, & Powe, 2002; Marin et al., 1995).
Both the growth and the diversity of the Hispanic population pose challenges in understanding the ways and extent to which culturally sensitive interventions can improve Hispanic health behaviors and outcomes. Hispanics are now the largest minority group in the United States, representing 14.2% of the total population (U.S. Census Bureau, 2007). Equally important is the diversity within this minority, which is composed of a variety of subgroups of different origin. Individuals of Mexican descent are the largest Hispanic subgroup, representing almost two thirds of this population (64%), followed by Puerto Ricans (9.6%), Central Americans (7.2%), South Americans (5.5%), and Cubans (3.6%; U.S. Census Bureau, 2007).
Despite the consensus that cultural context and ethnicity are key components in behavioral health interventions designed for minority populations, there is an ongoing debate over how to design efficacious culturally sensitive health interventions for minorities. Also, the principles and components of cultural sensitivity in minority behavioral health research have not been extensively described or empirically examined in studies related to nutrition and exercise (Betancourt, Green, Carrillo, & Ananeh-Firempong, 2003; Castro, Barrera, & Martinez, 2004; Stiffman, Freedenthal, Brown, Ostmann, & Hibbeler, 2005). Examining nutrition and exercise behaviors among Hispanics is of great importance. In 2003–2004, Hispanic adults and children had a higher prevalence of overweight and obesity (75.8% and 41.4%, respectively) than White adults and children had (64.2% and 35.4%, respectively; Ogden et al., 2006). Hispanics are also more likely than non-Hispanic Whites to have low levels of physical activity (Adams & Schoenborn, 2006; Bolen, Rhodes, Powell-Griner, Bland, & Holtzman, 2000; CDC, 2005).
The purpose of this literature review was to identify and examine the theoretical principles and components of culturally sensitive interventions tested in randomized controlled trials (RCTs) aimed at modifying eating and physical activity behaviors in Hispanics. This review is limited to RCTs because an RCT is the most rigorous research design to assess scientific evidence of behavioral intervention efficacy since it helps rule out threats to internal validity. The following research questions guided this review:
What is the theoretical foundation of nutrition- and exercise-related interventions tailored for Hispanics?
How are concepts of ethnicity and culture operationalized in these studies?
What are the main components and recruitment strategies used in these interventions?
Did these studies test the influence of cultural factors on intervention outcomes?
METHOD
Articles selected for this review met the following criteria: (a) they described an intervention that was tailored for Hispanics; (b) the intervention was aimed at modifying knowledge, beliefs, or behavior related to nutrition or exercise; (c) the intervention was tailored for Hispanics of any age group; (d) the study was based on the RCT research design; (e) the study was reported in a peer-reviewed journal; (f) the study was conducted in the United States; and (g) the study was published between 1990 and 2006. The articles reviewed were identified through Medline and PubMed databases by the use of the following keywords: Hispanic, Latino, Mexican, Puerto Rican, intervention, program, culturally, dietary, nutrition, eating, exercise, and physical activity. An initial search across databases yielded 319 potentially eligible references. The abstracts of these potentially eligible references were reviewed, and 46 abstracts were retained. We then retrieved and reviewed the full texts of the retained abstracts. Of the 46 articles reviewed, 30 studies describing 18 RCTs were finally selected for inclusion in this review. Two of us conducted the literature search and selected articles for inclusion. In cases of disagreement, the reviewers discussed any differences in opinion until reaching a consensus.
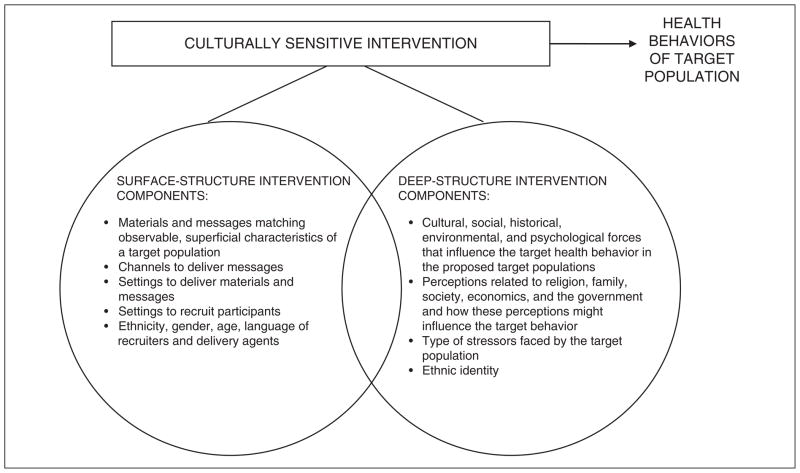
We categorized the components of the interventions reported in the reviewed studies using the cultural sensitivity framework proposed by Resnicow, Baranowski, Ahluwalia, & Braithwaite (1999) and shown in Figure 1. In cases of disagreement when categorizing the intervention components, we reached a consensus.
FIGURE 1. Components of Culturally Sensitive Interventions.
NOTE: Adapted from the culturally sensitive framework of Resnicow, Baranowski, Ahluwalia, and Braithwaite (1999). This framework was used to categorize the component interventions included in this review.
The main tenet of this framework is that cultural sensitivity is a bidimensional concept, and it categorizes intervention components as surface structure and deep structure. Surface structure components include intervention materials, messages, channels, settings, and recruitment strategies that match the characteristics of a priority population (e.g., familiar places, language, music, foods, and locations; Resnicow, Soler, Braithwaite, Ahluwalia, & Butler, 2000). Deep structure components are cultural, social, historical, environmental, and psychological factors influencing health behaviors.
For each intervention we aimed at identifying the theoretical framework, the formative research efforts conducted to design and implement the RCT, the ethnic term used to describe the priority population, operational constructs of culture, intervention components, recruitment and adherence strategies, and evidence indicating whether the association between the intervention components and the outcomes was tested for significance.
RESULTS
Theoretical Foundation
Most (70.6%) of the interventions reviewed described their theoretical foundation, and the prevalent theories were those focusing on individual and interpersonal health behaviors. The theory most frequently used to guide the interventions was the social learning theory (41.2%; Fitzgibbon, Stolley, Dyer, VanHorn, & KauferChristoffel, 2002; Poston et al., 2001; Rosal et al., 2005; Staten et al., 2004; Trevino et al., 2004; Vazquez, Millen, Bissett, Levenson, & Chipkin, 1998). Other theories or frameworks used were the social support framework (Avila & Hovell, 1994; Castro et al., 1995; Poston et al., 2001, 2003), a peer health worker model (Castro et al., 1995; Staten et al., 2004), self-change behavioral modification strategies (Avila & Hovell, 1994), a systems perspective (Castro et al., 1995), a self-determination theory and transtheoretical model (Fitzgibbon et al., 2002), a patient–provider communication model (Staten et al., 2004), a community organization framework (Thompson, Coronado, Chen, & Islas, 2006), socioecological theory (Trevino et al., 2004), social marketing and the Precede-Proceed Model (Wechsler, Basch, Zybert, & Shea, 1998), and a patient-centered counseling model (Rosal et al., 2005).
Conceptualizing Ethnicity and Culture
Although the studies reviewed were RCTs testing the efficacy of culturally based interventions tailored for Hispanics, none of the studies provided an operational definition of the cultural construct. However, authors used a varied terminology to describe the cultural qualification of the intervention: culturally appropriate (Elder et al., 2006; Poston et al., 2001, 2003; Thompson et al., 2006), culture specific (Elshaw, Young, Saunders, McGurn, & Lopez, 1994; Fitzgibbon, Stolley, Avellone, Sugerman, & Chavez, 1996; Rosal et al., 2005; Vazquez et al., 1998), or culturally focused (Castro et al., 1995).
Seven interventions in this review measured the acculturation level of participants (Cousins et al., 1992; Elder et al., 2006; Fitzgibbon et al., 1996; 2006; Fitzgibbon, Gapstur, & Knight, 2004; Lopez & Castro, 2006; Thompson et al., 2006). A few studies recorded the generation status of participants (Avila & Hovell, 1994) and their nativity (Fitzgibbon et al., 2004; Poston et al., 2001). Only one study examined the effects of acculturation on health outcomes (Balcazar, Castro, & Krull, 1995; Lopez & Castro, 2006), finding that highly acculturated, highly educated women had a stronger orientation to healthy eating than did the less acculturated. Also, different scales measuring acculturation were identified in the studies. The measurements most frequently used were the Acculturation Rating Scale for Mexican Americans (Cuellar, Arnold, & Maldonado, 1995) and the Short Acculturation Scale (Marin, Sabogal, Marin, Otero-Sabogal, & Perez-Stable, 1987).
Formative research, including focus groups, literature searches, and surveys (Castro et al., 1995; Elder et al., 2006; Fitzgibbon et al., 1996, 2004, 2006; Rosal et al., 2005; Thompson et al., 2006; Vazquez et al., 1998), guided the design and implementation of 44% of the interventions. Formative research in these studies aimed at identifying intervention needs; exploring health-related knowledge, attitudes, and barriers; and obtaining feedback from key informants about the cultural appropriateness of the intervention.
In this review, we found that there was no preference for the use of a monolithic ethnic term. The terms most frequently used were Hispanic (33%) and Latino (28%), although some studies included specific Hispanic subgroups, such as Mexican Americans (28%) or Latina Caribbean (6%).
Surface and Deep Structure Components
Virtually all studies mentioned the components of the intervention tailored for their Hispanic audience. Table 1 shows the intervention components, recruitment strategies, outcomes, and effects.
TABLE 1.
Characteristics and Components of Interventions (N = 18)
| Author | Sample | Intervention Components
|
Recruitment Strategies | Outcomes | Effects | |
|---|---|---|---|---|---|---|
| Surface Structure | Deep Structure | |||||
| Avila & Hovell, 1994 | 44 obese Latinas, ≥18 years |
|
|
|
Attitudes, beliefs, in exercise, of exercise and diet; moderate and vigorous exercise rate | Significant increase walking, diet, and knowledge |
| Balcazar, Castro, & Krull, 1995; Castro et al., 1995; Lopez & Castro, 2006 | 14 churches (447 Hispanic women, ≥18 years) |
|
|
|
Diet-related attitudes and behaviors; cancer prevention knowledge, cancer screening behaviors; fear of cancer; family support | Not reported |
| Cousins et al., 1992 | 168 obese Mexican American women, ages 18–45 |
|
|
Weight loss | Significantly more weight loss in individual and family groups than in control group | |
| Diabetes Prevention Program Research Group, 2000, 2002; Knowler et al., 2002; Rubin et al., 2002 | 508 Hispanic adults |
|
|
Diet; weight loss; exercise | Significant weight loss and changes in exercise | |
| Elder et al., 2006 | 357 Latinas, ages 18–65 |
|
Not described | Not described | Dietary intake; acculturation; BMI and waist-to-hip ratio control groups, but no persistence of changes 12 months postintervention | Significant short-term changes in calorie and fat intake in intervention and |
| Elshaw, Young, Saunders, McGurn, & Lopez, 1994 | 152 older Mexican Americans |
|
|
|
Nutrient content food intake; weight | Significant weight loss experienced by most groups; significant decrease in calorie intake experienced by control men only; significant decrease in cholesterol intake experienced by control women only |
| Fitzgibbon, Stolley, Dyer, VanHorn, & KauferChristoffel, 2002; Fitzgibbon et al., 2006 | 401 preschool Latino children and their parents |
|
|
Schools | BMI; dietary intake, physical activity, television viewing | No significant differences |
| Fitzgibbon, Stolley, Avellone, Sugerman, & Chavez, 1996 | 38 Hispanic American mothers and children (ages 7–12) |
|
|
Diet; nutrition knowledge | Significant reduction in fat and increased parental support, exercise, and fruit and vegetable intake among mothers; increased fruit and dairy intake and a decrease in meat, sweets, and heart-unhealthy intake in older children; significant increase in nutrition knowledge in all children | |
| Fitzgibbon, Gapstur, & Knight, 2003, 2004 | 256 Latinas (ages 20–40) |
|
|
|
Dietary energy from fat; fruit, and vegetable consumption; depression; breast health behaviors; BMI | Significant decrease in fat intake and percentage of energy from fat; no significant differences in breast health behaviors |
| Flores, 1995 | 110 Hispanic children (ages 10–13) |
|
|
|
Timed mile run; resting heart rate; BMI; attitudes toward physical activity | Significant decrease in BMI and heart rate; significant improvement in physical activity behavior and attitudes among girls, but not boys |
| Poston et al., 2001 | 379 obese Mexican American women (ages 18–65) |
|
|
Not described | Physical activity; BMI; social support; locus of control | No significant overall improvement in physical activity levels |
| Poston et al., 2003 | 108 women of Mexican origin (ages 21–65) |
|
|
Not described |
|
Significant weight loss in experimental group |
| Rosal et al., 2005 | 25 Spanish-speaking individuals with type 2 diabetes (ages ≥18 years) |
|
|
|
No significant differences in dietary intake or physical activity; significant decrease in glycosylated hemoglobin and depression | |
| Staten et al., 2004 | 217 Hispanic women (ages ≥50) |
|
|
|
Blood pressure; cholesterol; glucose; physical activity; fruit and vegetable consumption | Significant increase in fruit and vegetable consumption and physical activity; significant decrease in systolic blood pressure |
| Thompson, Coronado, Chen, & Islas, 2006 | 20 communities with 918 Hispanics (ages ≥18) |
|
|
|
Cancer screening behaviors; fruit and vegetable consumption; and smoking | No significant differences in fruit and vegetable consumption or smoking; significant differences in use of screening services |
| Trevino, Hernandez, Yin, Garcia, & Hernandez, 2005; Trevino et al., 1998, 2004 | 27 schools (2,640 Mexican American children) |
|
|
|
Glucose level; percentage of body fat; physical fitness; fiber intake; and saturated fat intake | Significant changes in fitness and fiber intake and glucose level |
| Vazquez, Millen, Bissett, Levenson, & Chipkin, 1998 | 38 Latina Caribbean (ages 32–70) |
|
|
Energy, saturated fat, carbohydrate, and fiber intake | Significant changes in energy, total fat, saturated fat, carbohydrate, and fiber intake | |
| Wechsler, Basch, Zybert, & Shea, 1998 | 6,902 elementary school students (86% Latino) |
|
|
Increase low-fat milk consumption | Significant increase in low-fat milk consumption | |
NOTE: BMI = body mass index; promotoras = peer health workers.
Three studies provided a list of the components that characterized the cultural sensitivity or appropriateness of the intervention. Fitzgibbon et al. (2002) indicated that culturally specific components included easy and safe access to the program; efforts aimed at fostering identification between interventionists and participants; knowledge; attitudes; social support; cultural attitudes; unsafe neighborhoods; behavioral demonstrations; and literacy levels. Rosal et al. (2005) considered the following components: family involvement, culturally popular activities, ethnic foods, social support, and intervention materials delivered in the preferred language. Vazquez et al. (1998) listed literacy level, beliefs toward obesity and diets, culturally relevant nutrition behaviors, social support, fatalism, bilingual and bicultural interventionists, and home activities.
Based on the cultural sensitivity framework of Resnicow et al. (1999, 2000), we identified eight surface-structure intervention components, as shown in Table 1. The most prominent surface-structure component in interventions was the use of bilingual and bicultural materials and delivery agents (78%). Four interventions used a back-translation technique to prepare materials in English and Spanish (Cousins et al., 1992; Fitzgibbon et al., 2002; Fitzgibbon, Gapstur, & Knight, 2003; Puschel, Thompson, Coronado, Lopez, & Kimball, 2001). Other salient intervention surface-structure components were the inclusion of ethnic foods (33%), followed by working with promotoras (community health workers; 24%) and delivering the intervention in group settings (24%).
Involving the family in interventions (47%) was the dominant deep-surface component found in our review, including activities such as partner support techniques and parental training. Additional deep-structure components included the literacy level of participants (39%), use of social support and networks (29%), and incorporation of Hispanic cultural values in intervention design or implementation (29%). Hispanic values considered in the interventions included familism (Castro et al., 1995; Cousins et al., 1992; Fitzgibbon et al., 1996, 2003, 2006; Poston et al., 2003; Rosal et al., 2005; Trevino et al., 2004; Vazquez et al., 1998; Wechsler et al., 1998); trust, or confianza (Castro et al., 1995; Fitzgibbon et al., 2002); the need to establish smooth relationships, or simpatia (Fitzgibbon et al., 2003); and fatalism, or lack of empowerment (Vazquez et al., 1998).
Most studies in this review did not detail their recruitment strategies. A majority of the studies conducted their recruitment at or through community agencies, churches, schools, or the media. The effectiveness of recruitment activities was not examined in the majority of the studies. The Diabetes Prevention Program study, however, did report that phone recruitment was the most effective strategy with Hispanics (Rubin et al., 2002). Recruitment strategies are shown in Table 1.
Influence of Intervention Tailoring
Although 13 studies produced significant differences in eating or exercise outcomes, the research design of most of these studies did not address whether the intervention was successful or not because of its Hispanic-tailored nature.
CONCLUSION
Health scholars and experts have underlined the importance of designing and implementing culturally sensitive interventions. This comprehensive literature review examined principles and components of interventions tailored for Hispanics that aimed at modifying eating or exercise behaviors and were based on an RCT design. We wanted to find out what theories guided the interventions, how ethnicity and culture were conceptualized, what the main intervention components were, and to what extent the studies tested the influence of cultural factors on intervention outcomes.
Culture and Theory
Most interventions in this review were minimally guided by cultural models or frameworks. The emphasis of using behavioral and socioecological theories found in the reviewed studies may be justified by the fact that most interventions aimed at affecting behavioral health outcomes. However, it was surprising to learn that only two studies in this review were guided by a cultural framework, particularly considering the extensive research examining cultural competency frameworks in health care services and systems (Anderson, Scrimshaw, Fullilove, Fielding, & Normand, 2003; Betancourt, Green, & Carrillo, 2002; Betancourt et al., 2003; Brach & Fraser, 2000; Howard, Andrade, & Byrd, 2001; Suh, 2004). Paucity of culturally sensitive models in behavioral health research should be of concern because the lack of such models could result in the implementation or replication of interventions based more on practitioners’ perceptions and intuitions about how to tailor interventions for Hispanics than on empirically tested culture-related theories.
Our review found that the intervention design in almost half the studies was guided by formative research, which suggests that this type of research should not be overlooked when designing and implementing a behavioral intervention for Hispanics. Furthermore, formative research has been identified by health research scholars as a basic element of intervention design (Needleman & Needleman, 1996; Resnicow et al., 1999).
Ethnicity and Acculturation
Although the way the Hispanic population is classified operationally has implications in health research (Mays, Ponce, Washington, & Cochran, 2003), the debate over the most appropriate generic label for this minority group is ongoing (Lopez, 2005; Mays et al., 2003). We found that studies in this review had a preference for the ethnic term Hispanic, followed by Latino, and some researchers specifically included Mexican Americans or Latina Caribbean. The acknowledgment of Hispanic subgroups has important research implications. Previous research underlines that overlooking ethnic variations and cultural differences within this minority population could become a barrier to appropriate health care and a factor sustaining health disparities. Access to health care services and the health status of Hispanics are influenced by English proficiency, country of origin, length of time living in the United States, immigration status, and acculturation (Weinick, Jacobs, Stone, Ortega, & Burstin, 2004; Zsembik & Fennell, 2005). Because the complex health patterns in the Hispanic population vary with ethnicity, diversity must be acknowledged to better serve the health needs of this group. Although our review showed that Hispanic subgroups were acknowledged in some studies, it also revealed an extreme sparseness of intervention research that includes smaller subgroups that are growing significantly and rapidly. Examples of these Hispanic subgroups are immigrants from Central America, with an increase of 44.6% in the past decade; South America, 47.2%; and Dominican Republic, 42.6% (Ramirez, 2004).
Although constructs are key elements that give specific or contextual meaning to a theoretical framework (Glanz, Rimer, & Lewis, 2002), our findings indicate that none of the studies in this review defined or operationalized the construct used to qualify the cultural nature of the intervention (e.g., culturally sensitive, appropriate, specific, or competent).
Our review shows that acculturation was measured in seven studies, and different measurement scales were applied. In addition, one study recorded the generation status of participants (e.g., first generation), and two others reported the country of origin. However, only one study examined the effects of acculturation level on health intervention outcomes (Balcazar et al., 1995; Lopez & Castro, 2006), even though it is well documented that acculturation and generation status are significantly associated with eating and exercise behaviors. Our findings are consistent with a study by Lindberg and Stevens (2007) that highlighted the need to use standardized acculturation measures and include nativity and other demographic information of participants in future interventions. Previous research has indicated that less acculturated Hispanics have a healthier food intake than those who are more acculturated (Bermúdez, Falcón, & Tucker, 2000; Lin, Bermudez, & Tucker, 2003; Mazur, Marquis, & Jensen, 2003; Neuhouser, Thompson, Coronado, & Solomon, 2004). In the case of exercise, the relationship with acculturation is not clear because of conflicting findings (Berrigan, Dodd, Troiano, Reeve, & Ballard-Barbash, 2006; Crespo, Smit, Carter-Pokras, & Andersen, 2001; Evenson, Sarmiento, & Ayala, 2004; Slattery et al., 2006). Additional research examining the influence of generation status on lifestyle found that nativity and longer duration of time in the United States are associated with unhealthy eating behaviors (Aldrich & Variyam, 2000; Allen et al., 2007; Dubowitz, Subramanian, Acevedo-Garcia, Osypuk, & Peterson, 2008; Gordon-Larsen, Harris, Ward, & Popkin, 2003; Guendelman & Abrams, 1995; Winkleby, Albright, Howard-Pitney, Lin, & Fortmann, 1994) and inactivity (Gordon-Larsen et al., 2003). Acculturation is a complex process that has many definitions and has been measured with varied instruments and dimensions (Lara, Gamboa, Kahramanian, Morales, & Bautista, 2005). The lack of consensus in defining and measuring acculturation suggests that more research in this field is needed.
Intervention Components and Outcomes
This review aimed at identifying the components of the tailored interventions. Based on the cultural sensitivity framework proposed by Resnicow et al. (1999), our findings indicate that the most prominent cultural component in the interventions was the use of bilingual and bicultural materials and delivery agents. However, only a few interventions in this review used the back-translation technique to prepare materials in English and Spanish. Back-translation is one of the most widely used translation techniques in research and has substantial source language transparency (Behling & Law, 2000). Another intervention component included in almost one quarter of the interventions was working with promotoras to recruit and deliver the program. Although the promotora outreach model is used in areas where low-income, uninsured Hispanics live with limited access to health care services (Eng, Parker, & Harlan, 1997), previous research has shown mixed results regarding the effectiveness of this outreach model in improving lifestyle behaviors in Hispanics (Rhodes, Foley, Zometa, & Bloom, 2007; Swider, 2002). In our review, only two (Elder et al., 2006; Staten et al., 2004) out of four interventions (Castro et al., 1995; Elder et al., 2006; Staten et al., 2004; Thompson et al., 2006) that worked with promotoras reported significant effects in health behaviors. Further research is warranted to examine more closely the effectiveness of promotoras’ role as behavioral intervention facilitators for Hispanics and in achieving sustained behavioral changes over time.
Family involvement, social support, and literacy level were components found in many of the interventions reviewed. Considerable research has shown that family and social support correlate significantly with healthy eating in Hispanics of various ages, such as children (Ayala et al., 2007), pregnant women (Gutierrez, 1999), and adults with type 2 diabetes (Morales López, Burrowes, Gizis, & Brommage, 2007; Orzáez Villanueva, Rodríguez Cisneros, Morales Ruiz, & Martinéz Rincón, 2006; Wen, Parchman, & Shepherd, 2004). Eyler et al. (1999) also found that family and social support were strong predictors of exercise in Hispanic women.
This review also found that more than half of the reviewed studies took into account Hispanic cultural values in intervention design or implementation. Familism was the cultural value most frequently considered in the interventions. This construct is defined as individuals’ strong identification with and attachment to their nuclear and extended family (Marin & Marin, 1991).
Recruitment and adherence strategies are also critical elements in behavioral interventions. Most studies in this review, however, did not provide a detailed account of these strategies. This might be because of a lack of documentation during intervention implementation or to limited publication space provided by journals.
In summary, we found that three components were common to most of the interventions that produced significant differences in behavioral outcomes: involvement of family or social support, literacy-level appropriateness, and cultural values. However, the studies reviewed did not provide evidence that would allow us to draw valid scientific conclusions about what specific components (e.g., family-based activities, group settings, and other) mediate or predict behavioral outcomes of a culturally sensitive intervention for Hispanics. Also, it is not clear which tailored intervention elements that proved effective with one Hispanic subgroup could be systematically applicable to other subgroups. For example, would working with peer health workers be as effective with affluent, urban Hispanics as it has been with low-income, rural Hispanics?
RECOMMENDATIONS
Based on this critical analysis, we offer the following recommendations for health researchers and practitioners interested in designing and implementing lifestyle behavioral interventions for Hispanics:
This review highlights the importance of using theory to design behavioral interventions for Hispanics. A theoretical framework may help researchers and practitioners design interventions in a more articulate way based on scientific knowledge and with the possibility of interpreting individual and social determinants influencing behavioral modifications. But the question of how to select the most appropriate theory still remains. Burdine and McLeroy (1992) suggested a “theory of the problem approach”: (a) Instead of starting with theory, one would determine a specific health issue for which an intervention is needed; (b) one would identify the theories from a socioecological perspective and select the most appropriate one for understanding causal factors and processes of specific health behaviors; (c) one would determine potential points of interventions suggested by the selected theory or framework; and (d) one would consider “the field’s collective wisdom on what interventions work with what populations under what conditions” (p. 337). In addition, the cultural sensitivity framework of Resnicow et al. (1999) may be useful in deciding what intervention components should be considered.
Formative research plays an important role in the design and implementation of an intervention for Hispanics. Health assessments, focus group discussions, literature searches, and interviews are tools for tailoring an intervention by identifying attitudes, beliefs, language use, and other opinions of the priority population in relation to specific health issues or behaviors (Morgan, 1998; Resnicow et al., 1999). In addition, formative research should be applied to examine socioecological contextual factors not identified in this review and that could influence the feasibility and efficacy of an intervention for Hispanics (e.g., influence of the built environment on physical activity; Leslie et al., 2005).
The diversity of the Hispanic population must be acknowledged in intervention design. Further experimental and prospective studies in behavioral health that take into account not only ethnic variations, but also acculturation and generation status factors may broaden our understanding of how to promote healthy behaviors effectively among different groups of Hispanics. It is important to keep in mind that about one third of Hispanics in the United States are foreign born (U.S. Census, 2007) and that acculturation, nativity, and duration in the country influence the lifestyle of Hispanics.
-
Although further empirical examination is warranted to determine the efficacy of cultural components of intervention and which individual or combined components could be systematically applied to various Hispanic subgroups to improve their lifestyle behaviors, intervention components that may be considered when designing nutrition or exercise interventions for Hispanics may include the following:
Intervention delivery agents and materials that not only meet the language needs of Hispanics but also reflect their cultural values and the ways these values influence health behavior. Preferably, interventions should rely on bicultural facilitators and prepare materials using the back-translation technique or another method that will ensure language transparency and cultural equivalency in materials and instruments.
Family and social support.
An extensive understanding of the degree to which Hispanic cultural values influence health behaviors. For instance, research indicates that familism is a central value among many Hispanics and thus may influence eating or exercise behaviors. It is important to note that understanding cultural values is not enough and that formative research is required to determine how these values should be included in an intervention.
Assessment of the literacy level of participants in order to develop appropriate materials and evaluation questionnaires.
Effective recruitment sites may include community or governmental agencies such as churches, health agencies, and schools. Nevertheless, more extensive research is needed to determine the most effective recruitment and adherence methods in culturally sensitive behavioral interventions for Hispanics.
Acknowledgments
This research was supported by the National Institutes of Health, National Institute of Child Health and Human Development (3 R01HD047143-01S1), and the Health Science Center, Texas A&M University System Research Development and Enhancement Awards Program.
Contributor Information
Nelda Mier, Associate professor in the Department of Social and Behavioral Health, School of Rural Public Health, Texas A&M Health Science Center, in McAllen, Texas.
Marcia G. Ory, Professor in the Department of Social and Behavioral Health, School of Rural Public Health, Texas A&M Health Science Center, in College Station, Texas.
Alvaro A. Medina, Research assistant in the Department of Social and Behavioral Health, School of Rural Public Health, Texas A&M Health Science Center, in McAllen, Texas.
References
- Adams P, Schoenborn C. Health behaviors of adults: United States, 2002–04. National Center for Health Statistics. Vital Health Statistics. 2006;10(230) Retrieved November 17, 2008, from http://www.cdc.gov/nchs/data/series/sr_10/sr10_230.pdf. [PubMed] [Google Scholar]
- Aldrich L, Variyam JN. Acculturation erodes the diet quality of U.S. Hispanics. Food Review. 2000;23:51–55. [Google Scholar]
- Allen ML, Elliott MN, Morales LS, Diamant AL, Hambarsoomian K, Schuster MA. Adolescent participation in preventive health behaviors, physical activity, and nutrition: Differences across immigrant generations for Asians and Latinos compared with Whites. American Journal of Public Health. 2007;97(2):337–343. doi: 10.2105/AJPH.2005.076810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. Culturally competent healthcare systems: A systematic review. American Journal of Preventive Medicine. 2003;24(3 Suppl):68–79. doi: 10.1016/s0749-3797(02)00657-8. [DOI] [PubMed] [Google Scholar]
- Avila P, Hovell MF. Physical activity training for weight loss in Latinas: A controlled trial. International Journal of Obesity and Related Metabolic Disorders. 1994;18(7):476–482. [PubMed] [Google Scholar]
- Ayala GX, Baquero B, Arredondo EM, Campbell N, Larios S, Elder JP. Association between family variables and Mexican American children’s dietary behaviors. Journal of Nutrition Education and Behavior. 2007;39(2):62–69. doi: 10.1016/j.jneb.2006.08.025. [DOI] [PubMed] [Google Scholar]
- Balcazar H, Castro FG, Krull JL. Cancer risk reduction in Mexican American women: The role of acculturation, education, and health risk factors. Health Education Quarterly. 1995;22(1):61–84. doi: 10.1177/109019819502200107. [DOI] [PubMed] [Google Scholar]
- Behling O, Law KS. Translating questionnaires and other research instruments: Problems and solutions. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Bermúdez OI, Falcón LM, Tucker KL. Intake and food sources of macronutrients among older Hispanic adults: Association with ethnicity, acculturation, and length of residence in the United States. Journal of the American Dietitians Association. 2000;100(6):665–673. doi: 10.1016/s0002-8223(00)00195-4. [DOI] [PubMed] [Google Scholar]
- Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: Issues for the cultural adaptation and development of psychosocial treatments with Hispanics. Journal of Abnormal Child Psychology. 1995;23(1):67–82. doi: 10.1007/BF01447045. [DOI] [PubMed] [Google Scholar]
- Berrigan D, Dodd K, Troiano RP, Reeve BB, Ballard-Barbash R. Physical activity and acculturation among adult Hispanics in the United States. Research Quarterly Exercise Sport. 2006;77(2):147–157. doi: 10.1080/02701367.2006.10599349. [DOI] [PubMed] [Google Scholar]
- Betancourt JR, Green AR, Carrillo JE. Cultural competence in health care: Emerging frameworks and practical approaches. 576. New York: Commonwealth Fund; 2002. [Google Scholar]
- Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O., II Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports. 2003;118(4):293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolen JC, Rhodes L, Powell-Griner EE, Bland SD, Holtzman D. State-specific prevalence of selected health behaviors, by race and ethnicity: Behavioral Risk Factor Surveillance System, 1997. Morbidity and Mortality Weekly Reports Surveillance Summaries. 2000;49(2):1–60. [PubMed] [Google Scholar]
- Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Medical Care Research Review. 2000;57(Suppl 1):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdine JN, McLeroy KR. Practitioners’ use of theory: Examples from a workgroup. Health Education Quarterly. 1992;19(3):331–340. doi: 10.1177/109019819201900305. [DOI] [PubMed] [Google Scholar]
- Caban CE. Hispanic research: Implications of the National Institutes of Health guidelines on inclusion of women and minorities in clinical research. Journal of the National Cancer Institute Monographs. 1995;18:165–169. [PubMed] [Google Scholar]
- Castro FG, Barrera M, Jr, Martinez CR., Jr The cultural adaptation of prevention interventions: Resolving tensions between fidelity and fit. Prevention Science. 2004;5(1):41–45. doi: 10.1023/b:prev.0000013980.12412.cd. [DOI] [PubMed] [Google Scholar]
- Castro FG, Elder J, Coe K, Tafoya-Barraza HM, Moratto S, Campbell N, et al. Mobilizing churches for health promotion in Latino communities: Companeros en la Salud. Journal of the National Cancer Institute Monographs. 1995;18:127–135. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Health disparities experienced by Hispanics: United States. Mortality and Morbidity Weekly Reports. 2004;53(40):935–937. Retrieved August 15, 2006, from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5340a1.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral risk factor surveillance system survey data. 2005 Retrieved October 17 2006, from http://apps.nccd.cdc.gov/brfss/race.asp?cat=PA&yr=2005&qkey=4418&state=UB.
- Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. Journal of General Internal Medicine. 2002;17(6):477–486. doi: 10.1046/j.1525-1497.2002.10633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousins JH, Rubovits DS, Dunn JK, Reeves RS, Ramirez AG, Foreyt JP. Family versus individually oriented intervention for weight loss in Mexican American women. Public Health Reports. 1992;107(5):549–555. [PMC free article] [PubMed] [Google Scholar]
- Crespo CJ, Smit E, Carter-Pokras O, Andersen R. Acculturation and leisure-time physical inactivity in Mexican American adults: Results from NHANES III, 1988–1994. American Journal of Public Health. 2001;91(8):1254–1257. doi: 10.2105/ajph.91.8.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuellar I, Arnold B, Maldonado R. Acculturation Rating Scale for Mexican Americans II: A revision of the original ARSMA Scale. Hispanic Journal of Behavioral Sciences. 1995;17:275–304. [Google Scholar]
- Diabetes Prevention Program Research Group. The Diabetes Prevention Program: Baseline characteristics of the randomized cohort. Diabetes Care. 2000;23(11):1619–1629. doi: 10.2337/diacare.23.11.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25(12):537–544. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz T, Subramanian SV, Acevedo-Garcia D, Osypuk TL, Peterson KE. Individual and neighborhood differences in diet among low-income foreign and U.S.-born women. Women’s Health Issues. 2008;18(3):181–190. doi: 10.1016/j.whi.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, Ayala GX, Campbell NR, Arredondo EM, Slymen DJ, Baquero B, et al. Long-term effects of a communication intervention for Spanish-dominant Latinas. American Journal of Preventive Medicine. 2006;31(2):159–166. doi: 10.1016/j.amepre.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Elshaw EB, Young EA, Saunders MJ, McGurn WC, Lopez LC. Utilizing a 24-hour dietary recall and culturally specific diabetes education in Mexican Americans with diabetes. Diabetes Educator. 1994;20(3):228–235. doi: 10.1177/014572179402000309. [DOI] [PubMed] [Google Scholar]
- Eng E, Parker E, Harlan C. Lay health advisor intervention strategies: A continuum from natural helping to paraprofessional helping. Health Education & Behavior. 1997;24:413–417. doi: 10.1177/109019819702400402. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Sarmiento OL, Ayala GX. Acculturation and physical activity among North Carolina Latina immigrants. Social Science & Medicine. 2004;59(12):2509–2522. doi: 10.1016/j.socscimed.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity social support and middle-and older-aged minority women: Results from a US survey. Social Science & Medicine. 1999;49(6):781–789. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Gapstur SM, Knight SJ. Mujeres Felices por Ser Saludables: A breast cancer risk reduction program for Latino women. Preventive Medicine. 2003;36(5):536–546. doi: 10.1016/s0091-7435(03)00015-x. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Gapstur SM, Knight SJ. Results of Mujeres Felices por ser Saludables. Annals of Behavioral Medicine. 2004;28(2):95–104. doi: 10.1207/s15324796abm2802_4. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Avellone ME, Sugerman S, Chavez N. Involving parents in cancer risk reduction: A program for Hispanic American families. Health Psychology. 1996;15(6):413–422. doi: 10.1037//0278-6133.15.6.413. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Dyer AR, VanHorn L, KauferChristoffel K. A community-based obesity prevention program for minority children: Rationale and study design for Hip-Hop to Health Jr. Preventive Medicine. 2002;34(2):289–297. doi: 10.1006/pmed.2001.0977. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity. 2006;14(9):1616–1625. doi: 10.1038/oby.2006.186. [DOI] [PubMed] [Google Scholar]
- Flores R. Dance for health: Improving fitness in African American and Hispanic adolescents. Public Health Reports. 1995;110(2):189–193. [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Rimer BK, Lewis FM. Theory, research, and practice in health behavior and health education. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory, research, and practice. 3. San Francisco: Jossey-Bass; 2002. pp. 22–44. [Google Scholar]
- Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: The National Longitudinal Study of Adolescent Health. Social & Science Medicine. 2003;57(11):2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Guendelman S, Abrams B. Dietary intake among Mexican-American women: Generational differences and a comparison with white non-Hispanic women. American Journal of Public Health. 1995;85(1):20–25. doi: 10.2105/ajph.85.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez YM. Cultural factors affecting diet and pregnancy outcome of Mexican American adolescents. Journal of Adolescent Health. 1999;25(3):227–237. doi: 10.1016/s1054-139x(99)00016-6. [DOI] [PubMed] [Google Scholar]
- Howard CA, Andrade SJ, Byrd T. The ethical dimensions of cultural competence in border health care settings. Family & Community Health. 2001;23(4):36–49. doi: 10.1097/00003727-200101000-00006. [DOI] [PubMed] [Google Scholar]
- Ignarro LJ, Balestrieri ML, Napoli C. Nutrition, physical activity, and cardiovascular disease: an update. Cardiovascular Research. 2007;73(2):326–340. doi: 10.1016/j.cardiores.2006.06.030. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Health and behavior: The interplay of biological, behavioral, and societal influences. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- Institute of Medicine. Examining the health disparities research plan of the National Institutes of Health: Unfinished business. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- Kanaya AM, Narayan KM. Prevention of type 2 diabetes: Data from recent trials. Primary Care. 2003;30(3):511–526. doi: 10.1016/s0095-4543(03)00034-4. [DOI] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriska AM, Delahanty LM, Pettee KK. Lifestyle intervention for the prevention of type 2 diabetes: Translation and future recommendations. Current Diabetes Reports. 2004;4(2):113–118. doi: 10.1007/s11892-004-0066-9. [DOI] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie E, Saelens B, Frank L, Owen N, Bauman A, Coffee N, et al. Residents’ perceptions of walkability attributes in objectively different neighbourhoods: A pilot study. Health Place. 2005;11(3):227–236. doi: 10.1016/j.healthplace.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Liao Y, Tucker P, Okoro CA, Giles WH, Mokdad AH, Harris VB. REACH 2010 surveillance for health status in minority communities: United States, 2001–2002. Morbidity and Mortality Weekly Reports Surveillance Summaries. 2004;53(6):1–36. [PubMed] [Google Scholar]
- Lin H, Bermudez OI, Tucker KL. Dietary patterns of Hispanic elders are associated with acculturation and obesity. Journal of Nutrition. 2003;133(11):3651–3657. doi: 10.1093/jn/133.11.3651. [DOI] [PubMed] [Google Scholar]
- Lindberg NM, Stevens VJ. Review: Weight-loss interventions with Hispanic populations. Ethnicity & Disease. 2007;17:397–402. [PubMed] [Google Scholar]
- Lopez IH. Race on the 2010 census: Hispanics and the shrinking white majority. Daedalus. 2005;134(1):42–52. [Google Scholar]
- Lopez VA, Castro FG. Participation and program outcomes in a church-based cancer prevention program for Hispanic women. Journal of Community Health. 2006;31(4):343–362. doi: 10.1007/s10900-006-9016-6. [DOI] [PubMed] [Google Scholar]
- Marin G, Marin BV. Research with Hispanic populations. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9(2):183–205. [Google Scholar]
- Marin GBL, Connell CM, Gielen AC, Helitzer-Allen D, Lorig K, Morisky DE, et al. A research agenda for health education among underserved populations. Health Education Quarterly. 1995;22(3):346–363. doi: 10.1177/109019819402200307. [DOI] [PubMed] [Google Scholar]
- Mays VM, Ponce NA, Washington DL, Cochran SD. Classification of race and ethnicity: Implications for public health. Annual Review of Public Health. 2003;24:83–110. doi: 10.1146/annurev.publhealth.24.100901.140927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazur RE, Marquis GS, Jensen HH. Diet and food insufficiency among Hispanic youths: Acculturation and socioeconomic factors in the third National Health and Nutrition Examination Survey. American Journal of Clinical Nutrition. 2003;78(6):1120–1127. doi: 10.1093/ajcn/78.6.1120. [DOI] [PubMed] [Google Scholar]
- Morales López C, Burrowes JD, Gizis F, Brommage D. Dietary adherence in Hispanic patients receiving hemodialysis. Journal of Renal Nutrition. 2007;17(2):138–147. doi: 10.1053/j.jrn.2006.12.004. [DOI] [PubMed] [Google Scholar]
- Morgan DL. The focus group guidebook. Vol. 1. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Needleman C, Needleman ML. Qualitative methods for intervention research. American Journal Indian Medicine. 1996;29(4):329–337. doi: 10.1002/(SICI)1097-0274(199604)29:4<329::AID-AJIM10>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- Neuhouser ML, Thompson B, Coronado GD, Solomon CC. Higher fat intake and lower fruit and vegetable intakes are associated with greater acculturation among Mexicans living in Washington State. Journal of American Dietitians Association. 2004;104(1):51–57. doi: 10.1016/j.jada.2003.10.015. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Orzáez Villanueva MT, Rodríguez Cisneros A, Morales Ruiz E, Martinéz Rincón C. Determinación de los factores condicionantes en la adhesión y cumplimiento de la dieta de protección renal en pacientes con insuficiencia renal crónica: estudio previo para la elaboración de una guía dietética [Identification of conditioning factors in the adherence and compliance to a renal protective diet in patients with chronic renal insufficiency: Exploratory study for designing a diet guide] Nutricion Hospitalaria. 2006;21(2):145–154. [PubMed] [Google Scholar]
- Poston WS, Haddock CK, Olvera NE, Suminski RR, Reeves RS, Dunn JK, et al. Evaluation of a culturally appropriate intervention to increase physical activity. American Journal of Health Behavior. 2001;25(4):396–406. doi: 10.5993/ajhb.25.4.5. [DOI] [PubMed] [Google Scholar]
- Poston WS, Reeves RS, Haddock CK, Stormer S, Balasubramanyam A, Satterwhite O, et al. Weight loss in obese Mexican Americans treated for 1-year with Orlistat and lifestyle modification. International Journal of Obesity. 2003;27(12):1486–1493. doi: 10.1038/sj.ijo.0802439. [DOI] [PubMed] [Google Scholar]
- Puschel K, Thompson B, Coronado GD, Lopez LC, Kimball AM. Factors related to cancer screening in Hispanics: A comparison of the perceptions of Hispanic community members, health care providers, and representatives of organizations that serve Hispanics. Health Education Behavior. 2001;28(5):573–590. doi: 10.1177/109019810102800505. [DOI] [PubMed] [Google Scholar]
- Ramirez R. We the people: Hispanics in the United Sates. Census 2000 Special Reports. 2004 Retrieved on March 15 2006, from http://www.census.gov/prod/2004pubs/censr-18.pdf.
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: Defined and demystified. Ethnicity & Disease. 1999;9(1):10–21. [PubMed] [Google Scholar]
- Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance abuse prevention. Journal of Community Psychology. 2000;28(3):271–290. [Google Scholar]
- Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: A qualitative systematic review. American Journal of Preventive Medicine. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: A pilot study. Annals of Behavioral Medicine. 2005;29(3):225–235. doi: 10.1207/s15324796abm2903_9. [DOI] [PubMed] [Google Scholar]
- Rubin RR, Fujimoto WY, Marrero DG, Brenneman T, Charleston JB, Edelstein SL, et al. The Diabetes Prevention Program: Recruitment methods and results. Controlled Clinical Trials. 2002;23(2):157–171. doi: 10.1016/s0197-2456(01)00184-2. [DOI] [PubMed] [Google Scholar]
- Slattery ML, Sweeney C, Edwards S, Herrick J, Murtaugh M, Baumgartner K, et al. Physical activity patterns and obesity in Hispanic and non-Hispanic white women. Medicine Science Sports Exercise. 2006;38(1):33–41. doi: 10.1249/01.mss.0000183202.09681.2a. [DOI] [PubMed] [Google Scholar]
- Staten LK, Gregory-Mercado KY, Ranger-Moore J, Will JC, Giuliano AR, Ford ES, et al. Provider counseling, health education, and community health workers: The Arizona WISEWOMAN project. Journal of Women’s Health. 2004;13(5):547–556. doi: 10.1089/1540999041281133. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Freedenthal S, Brown E, Ostmann E, Hibbeler P. Field research with underserved minorities: The ideal and the real. Journal of Urban Health. 2005;82(2 Suppl 3):iii56–66. doi: 10.1093/jurban/jti064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suh EE. The model of cultural competence through an evolutionary concept analysis. Journal of Transcultural Nursing. 2004;15(2):93–102. doi: 10.1177/1043659603262488. [DOI] [PubMed] [Google Scholar]
- Swider SM. Outcome effectiveness of community health workers: An integrative literature review. Public Health Nursing. 2002;19(1):11–20. doi: 10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- Thompson B, Coronado G, Chen L, Islas I. Celebremos la Salud! A community randomized trial of cancer prevention. Cancer Causes Control. 2006;17(5):733–746. doi: 10.1007/s10552-006-0006-x. [DOI] [PubMed] [Google Scholar]
- Trevino RP, Hernandez AE, Yin Z, Garcia OA, Hernandez I. Effect of the Bienestar Health Program on physical fitness in low-income Mexican American children. Hispanic Journal of Behavioral Sciences. 2005;27(1):120–132. [Google Scholar]
- Trevino RP, Pugh JA, Hernandez AE, Menchaca VD, Ramirez RR, Mendoza M. Bienestar: A diabetes risk-factor prevention program. Journal of School Health. 1998;68(2):62–67. doi: 10.1111/j.1746-1561.1998.tb07192.x. [DOI] [PubMed] [Google Scholar]
- Trevino RP, Yin Z, Hernandez A, Hale DE, Garcia OA, Mobley C. Impact of the Bienestar school-based diabetes mellitus prevention program on fasting capillary glucose levels: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2004;158:911–917. doi: 10.1001/archpedi.158.9.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. The American community: Hispanics: 2004. American Community Survey Reports. 2007 Retrieved on March 29, 2007, from http://www.census.gov/prod/2007pubs/acs-03.pdf.
- Vazquez IM, Millen B, Bissett L, Levenson SM, Chipkin SR. Buena Alimentacion, Buena Salud: A preventive nutrition intervention in Caribbean Latinos with type 2 diabetes. American Journal of Health Promotion. 1998;13(2):116–119. doi: 10.4278/0890-1171-13.2.116. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Basch CE, Zybert P, Shea S. Promoting the selection of low-fat milk in elementary school cafeterias in an inner-city Latino community: Evaluation of an intervention. American Journal of Public Health. 1998;88(3):427–433. doi: 10.2105/ajph.88.3.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinick RM, Jacobs EA, Stone LC, Ortega AN, Burstin H. Hispanic healthcare disparities: Challenging the myth of a monolithic Hispanic population. Medical Care. 2004;42(4):313–320. doi: 10.1097/01.mlr.0000118705.27241.7c. [DOI] [PubMed] [Google Scholar]
- Wen LK, Parchman ML, Shepherd MD. Family support and diet barriers among older Hispanic adults with type 2 diabetes. Family Medicine. 2004;36(6):423–430. [PubMed] [Google Scholar]
- Winkleby MA, Albright CL, Howard-Pitney B, Lin J, Fortmann SP. Hispanic/white differences in dietary fat intake among low educated adults and children. Preventive Medicine. 1994;23(4):465–473. doi: 10.1006/pmed.1994.1064. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Diet and physical activity: A public health priority. 2007 Retrieved February 28, 2007, from http://www.who.int/dietphysicalactivity/en/
- Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Social Science & Medicine. 2005;61(1):53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]