Background
Acute Respiratory Distress Syndrome (ARDS) is a grave clinical problem afflicting up to 30% of severely injured trauma patients annually [1], the disease retains disturbingly high mortality[2], costs of care [3], and severe sequelae for survivors [4] in spite of decades of therapeutic research[5]. Trauma and hemorrhage result in massive systemic inflammation with attendant increases in vascular permeability leading to severe lung injury with pulmonary edema [6]. Resuscitation for hemorrhagic shock often requires transfusion of blood products, which are independently associated with the systemic inflammatory response syndrome (SIRS), acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) [7]. Thus traumatically injured patients with hemorrhagic shock are highly susceptible to development of ALI and ARDS.
Low tidal volume (LTV) ventilation is the only treatment strategy to emerge which appeared to be effective in reducing established-ARDS mortality in a large clinical trial [8]. However, more recent data demonstrate that even with application of LTV, the mortality of ARDS remains as high as 40–60% [2]. Furthermore trauma-induced ARDS remains significantly underrepresented in LTV ventilation clinical trials, with only 170 trauma patients in the 4,341 patient data base, which represents only <4% of the patient population in all currently published ARDSnet studies and makes extrapolating LTV benefits to this ARDS phenotype very limited[8]. The resistance of established-ARDS to the current standard of care treatment, and the limited applicability of LTV data to the trauma patient, suggest strategies for preventing ARDS before it becomes established must be sought.
Prevention is based on targeting the key early mechanisms of pathogenesis to interrupt disease progression. Early ARDS pathogenesis is driven by increased vascular permeability resulting in pulmonary edema, which deactivates surfactant, mechanical ventilation in this milieu causes alveolar instability which is both biologically and mechanically injurious to the lung [6] [9]. In our initial studies designed to prevent ARDS, the ventilation strategy consisted of applying a mechanical breath with an extended airway Pressure/Time Profile (P/TP) delivered via the airway pressure release ventilation (APRV) mode, utilizing a clinically applicable porcine sepsis-induced ARDS model. We hypothesized that extended P/TP alters the Starling forces of the lung reducing permeability, the most proximal pathologic event in the pathogenesis of ARDS, thereby preventing the downstream events of edema, surfactant deactivation and alveolar instability. Our group has recently shown that preemptive mechanical ventilation, applied before clinical signs of lung injury, can prevent the development of ARDS in a porcine model of Peritoneal Sepsis + Ischemia/Reperfusion (PS+I/R) induced lung injury [10, 11]. Although the end point (i.e. ARDS) is identical, the pathogenesis leading to acute lung injury may vary depending upon the source of the systemic inflammation – PS+I/R or T/HS. Therefore, we developed a rat T/HS model and tested the efficacy of our preemptive ventilation strategy at preventing lung injury specifically in the context of the traumatically injured patient. The results of the present study support our central hypothesis and build on our prior work in PS+I/R-induced ARDS by demonstrating that ARDS secondary to T/HS can be prevented, if the appropriate ventilation strategy is applied before clinical lung injury develops.
Methods
All techniques and procedures described were reviewed and approved by the Committee for the Humane Use of Animals at Upstate Medical University.
Surgery
Male Sprague-Dawley Rats (350–400g Taconic Farms) were anesthetized using intraperitoneal injection of a ketamine (90mg/mL) and xylazine (10mg/mL) mixture (10 mL/kg). Using aseptic technique, a tracheotomy was performed with a 14-gauge angiocatheter. Rats were attached to a Dräger ventilator (Evita Infinity v500) and allowed to spontaneous breathe on 100% FiO2. Respiratory pressure and volume were recorded every 30 minutes. The external jugular vein and internal carotid artery were then cannulated with polyethylene-50 (P.E. 50) tubing that had been previously flushed with heparinized saline (10U/ml).
Equilibration
The Time Line for the experiment is seen in Figure 1. Following surgery, rats were allowed to equilibrate to a normal physiologic range of body temperature (36.5–37.5 °C), heart rate (250–300 beats/min), mean arterial blood pressure (MAP) (70–90mmHg) and arterial oxygen tension (>300 mmHg on FiO2 100%). At baseline and equilibrium an arterial blood gas (3μL) was drawn from the carotid line and analyzed using a Cobas 221 blood gas analyzer (Roche Diagnostics). Inclusion parameters for the experiment were determined at equilibrium and were based on PaO2/FiO2 (>300), base excess (>−5.0), and lactate (<2.2). Rats were given intravenous Lactated Ringers Solution through the jugular line to maintain MAP >60 mmHg.
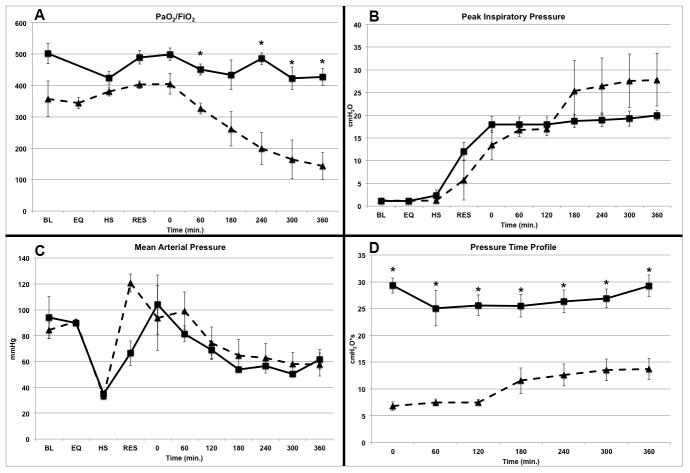
Figure 1.
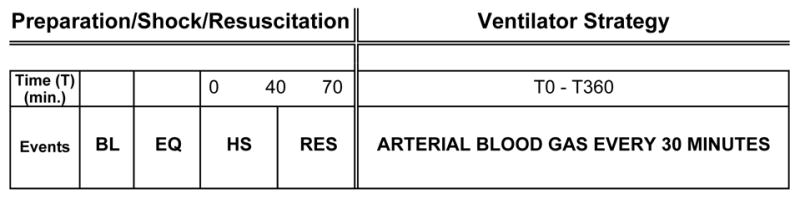
Time Line of experimental protocol. The experiment is broken into two Sections: Phase 1 – Preparation/Shock/Resuscitation: surgical preparation followed by Baseline measurements (BL) and an equilibrium period (EQ) to stabilize hemodynamics and body temperature. Following EQ, hemorrhagic shock (HS) is induced for 40min, followed by resuscitation (RES) with shed blood and Ringers Lactate. It takes approximately 70 min from the beginning of HS to the end of RES; Phase 2 – Ventilator Strategy: animals are randomized to their ventilation strategy (VC or APRV). Hemodynamics, blood gas and lung function measurements are made every 30 minutes until the end of the study at 360 minutes (T360) following RES. See Methods for detailed procedures.
Trauma/Hemorrhagic Shock (T/HS)
A traumatic injury was induced via a midline laparotomy (1cm), a Foley catheter (Size 8, DeRoyal Medical, TN) was placed in the abdomen for anesthesia delivery and temperature measurement, and the incision closed. Body temperature was maintained at 37°C (± 0.5°C) using a heating blanket and lamp. HS was induced by bleeding the rats through the jugular line at a rate no faster than 1ml/min. Rats were bled until a MAP of 30–40mmHg was reached. Animals were maintained in this MAP range by blood withdrawal or infusion for a period of 40 min (Figure 1).
Resuscitation
Rats were resuscitated using their shed blood mixed with twice the shed blood volume of Lactated Ringers. Vasopressors were not used in this study.
Protocol
Following resuscitation, rats were randomized to one of two ventilation modes.
-
Volume Cycled Ventilation (VC, n=5)- Volume cycled ventilation with the following parameters: a tidal volume (Vt) 10ml/kg, PEEP 0.5 cm H2O, RR 35–75/min. We chose the Vt and PEEP settings for the VC group to match the Vt and PEEP routinely delivered to patients undergoing surgery, which we felt would be most appropriate for our T/HS rat model [12–15]. These studies show that surgery patients are typically ventilated with Vt of 10 or greater with zero end expiratory pressure (ZEEP). In addition we did a PEEP titration to directly measure what level of PEEP stabilizes alveoli in the normal rat lung (see below).
In vivo PEEP calibration: Determination of PEEP applied in this group was based on a series of in vivo microscopy exercises. Rats (n=3) were surgically prepared as described above. Volume cycled ventilation with the following parameters were used: a tidal volume (Vt) 10ml/kg, RR 35–75/min, initial PEEP was 5 cm H2O. Our in Vivo microscopy methods are described below. While directly observing subpleural alveolar patency throughout the ventilation cycle PEEP was titrated down from 5 cm H2O to 0 cm H2O in 0.5 cm increments. At PEEP 0 cm H2O intratidal alveolar collapse was observed. It was observed that the lowest PEEP required to maintain alveolar patency throughout the ventilatory cycle was 0.5 cm H2O. PEEP was then titrated up from 0 cm H2O to 5 cm H2O in 0.5 cm H2O increments. Therefore 0.5 cm H2O PEEP was chosen for the VC group based on the direct evidence of alveolar stability using in vivo microscopy.
Airway pressure Release Ventilation (APRV, n=4)- with the following parameters: High Pressure (Phigh) was initially set similar to the Plateau Pressure on VC ventilation. Low Pressure (Plow) was set at 0 cmH2O for the entire 6 h to minimize expiratory resistance and maximize Peak Expiratory Flow Rate (PEFR). The Thigh (duration of Phigh) was set at 1.3–1.5 seconds to equal 90–95 % of the respiratory cycle. The Tlow (duration of release phase) ranged between 0.11–0.14 seconds in order to achieve a Termination of Peak Expiratory Flow Rate (T-PEFR) equal to 75% of PEFR. The Tlow was calculated and adjusted based on the angle of deceleration noted on the expiratory flow waveform as described previously [10, 11, 16]. The Phigh, Thigh, Tlow and FiO2 were titrated throughout the study per published guidelines [16] to minimize lung de-recruitment, optimize the efficiency of CO2 clearance, and minimize dead space ventilation.
In vivo Microscopy
This technique has been described in detail [17] but briefly, the right superior and the right middle lobe were used for in-vivo microscopy. The customized microscope (Olympus Medical, Center Valley, Pennsylvania) with a suction head was lowered onto the exposed lung surface. Subpleural alveoli were filmed in real time with a digital video camera (Allied Visions Stingray, F-145C 30fps) and stored in a custom built digital video recording system (MD-PC-V251B). Still photos from the movie stream of subpleural alveoli were digitized (StreamPix5) and subsequently analyzed to identify the profile of each alveolus in the photomicrograph, and their areas were measured directly with image analysis software (ImagePro, Media Cybernetics).
Euthanasia and Necropsy
All rats were euthanatized using sodium pentobarbital. The left lung was injected via tracheal instillation with 2.5ml 0.9% NaCl, and the bronchoalveolar lavage fluid (BALF) collected for analysis and frozen in a −70°C freezer. The right inferior lobe was isolated, clamped at peak inspiration and submerged in 10% formalin for histology.
Histologic Assessment
The quantitative histological assessment of the lung was based on image analysis of 90 photomicrographs (10 per animal), made at high-dry magnification following a validated, unbiased, systematic sampling protocol. Each photomicrograph was scored using a 4-point scale for each of 5 parameters: atelectasis, fibrinous deposits, blood in air spaces, vessel congestion, alveolar wall thickness, and leukocyte infiltration, as previously described [10, 11].
BALF and Lung Tissue data
The left lobe of the lung was lavaged with 2.5 ml of normal saline, spun at 1734g at 4°C, and snap frozen for later analysis. Western blot analyses of surfactant proteins A & B (SPA & SP-B) expression in the BALF as well as of Epithelial Cadherin (E-cadherin) in lung tissue homogenates were performed, as previously described [18, 19]. The SP-B assay of one rat was excluded since the rat died only 3hrs into the experiment secondary to the rapid development of ARDS. Total protein in the BALF was determined using the bicinchonic acid method.
P/TP Calculation
P/TP was calculated using equation-1 below, where P=Pressure (cmH2O), and T=Time (sec) over the period of one breath was defined as extending from the beginning of inspiration (Tinsp) to the end of expiration (Texp) [11].
| (Eq 1) |
Statistics
Data were expressed as mean ± SE. Repeated Measures ANOVA with rat number and treatment as random effects were performed to compare differences within and between treatment groups for continuous parameters. Probability values <0.05 were considered significant. Post hoc Tukey’s tests were performed on continuous data at specific time points only if significance was found in the group*time effect using RM ANOVA. Categorical data were compared using an unpaired Student’s t-test.
Results
Lung and Hemodynamic Function
Oxygenation was dramatically improved with preemptive application of APRV (Fig 2A). In the VC group the P/F ratio began to decline significantly at T180 and continued to fall until the end of the experiment (T360). At T360 the P/F was 143.3 ± 42.4 in VC animals, meeting gas exchange criteria for ARDS[8]. The APRV group maintained P/F above 400 for the entire experiment with a FiO2 of 0.31%±0.09 (Fig 2A). The improved P/F was not secondary to the peak inspiratory pressures, which were similar in both groups throughout the study (Fig 2B). The MAP was similar in both groups (Fig 2C).
Figure 2.
(A–D) – A: PaO2/FiO2 ratio (P/F) over time in the volume cycled ventilation (VC=▲) and airway pressure release ventilation (APRV=■) groups. There was a significant fall in P/F in the VC as compared with APRV group, with the P/F falling below 200 at T300 indicating the development of ARDS. B: Peak airway pressure (PIP) over time in the volume cycled ventilation (VC=▲) and airway pressure release ventilation (APRV=■) groups. C: Mean arterial blood pressure (MAP) over time in the volume cycled ventilation (VC=▲) and airway pressure release ventilation (APRV=■) groups. D: Airway Pressure/Time Profile (P/TP) over time in the volume cycled ventilation (VC=▲) and airway pressure release ventilation (APRV=■) groups. P/TP was significantly elevated in the APRV as compared with VC group throughout the entire experiment. BL=Baseline, EQ=Equilibrium, HS=Hemorrhagic Shock, RES=Resuscitation. Data±SEM. *=p<0.05 vs. VC group.
P/TP
Application of APRV significantly increased the P/TP above that delivered by VC immediately following application (T0) and remained significantly higher for the entire experiment (T360) (Fig 2D).
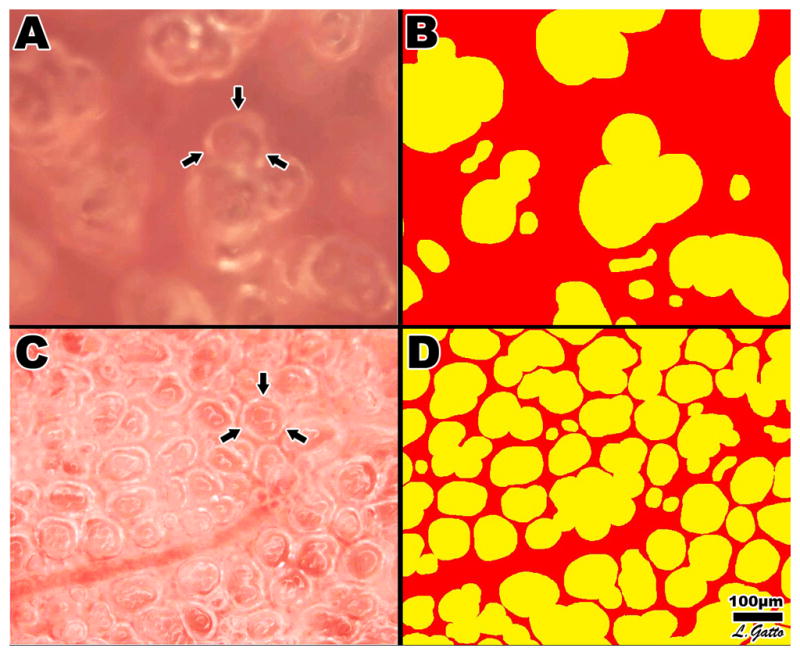
In vivo Microscopy
Subpleural alveoli were photographed at peak inspiration in the VC (Fig 3A, B) and APRV (Fig 3C, D) groups. There were significantly fewer alveoli at peak inspiration in the VC (Fig 3A, B, Table 1) than in the APRV (Fig 3C, D, Table 1) group.
Figure 3.
In vivo photomicrographs and image analysis of inflated subpleural alveoli in the VC (A, B) and APRV (C, D) groups. Measurement of the % Air Space was accomplished by circling the inflated alveoli using computer image analysis. All inflated alveoli were then assigned the color yellow and noninflated areas were assigned the color red generating a sharp contrast for the image analysis software to identify and measure the % of inflated alveoli/microscopic field. Arrows (A, C) identify a single alveolus.
Table 1.
Quantitative Histopathology
| Lesion | VC | APRV |
|---|---|---|
| % Air Space | 40.8 ± 5.7 | 72.0 ± 6.4* |
| Fibrinous Deposits | 1.82 ± 0.15 | 0.00 ± 0.17* |
| Hemorrhage in air space | 0.22 ± 0.09 | 0.65 ± 0.10* |
| Capillary congestion | 0.92 ± 0.16 | 0.58 ± 0.18 |
| Thickened alveolar walls | 2.00 ± 0.14 | 0.85 ± 0.15* |
| Cellular infiltration | 1.98 ± 0.11 | 0.35 ± 0.12* |
Volume Cycled ventilation (VC) and Airway Pressure Release Ventilation (APRV) groups. % Air Space is the percent of the microscopic field occupied by inflated alveoli measured with the in vivo microscope at peak inspiration. All other lesions were measured on histologic sections. See Methods for description of Lesions and for scoring method. Histologic lesions score range = 0 to 4; Number of microscopic fields examined: VC n=50 and APRV n=40. % Air Space measured as the percent of inflated alveoli/microscopic filed; Number of microscopic fields examined: VC n=5 and APRV n=4. Data are Mean ± SEM.
p<0.05
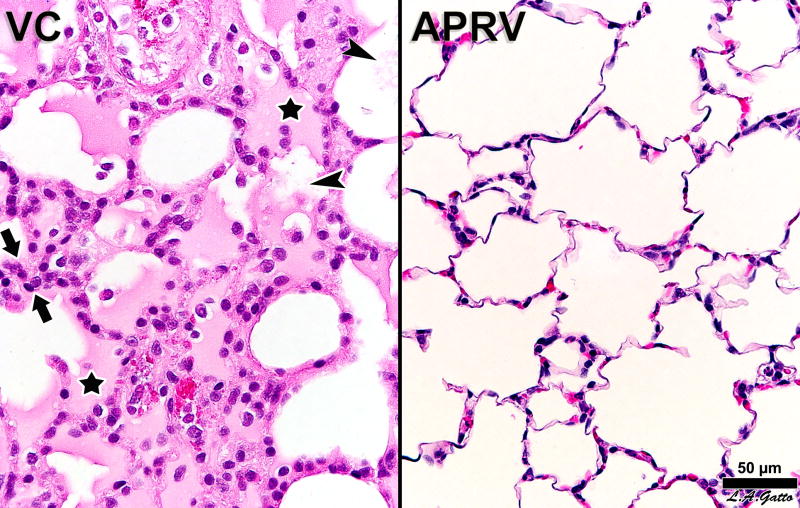
Histopathology
The lungs of rats receiving VC were marked by substantial amounts of edema (Fig 4), as several rats exhibited areas where alveolar lumina appeared uniformly filled with fluid. In addition, all VC animals had fibrinous deposits in the air compartment. Alveolar walls in the VC animals were thickened by the presence of wandering cells, mostly hematogenous macrophages. In contrast, APRV animals featured slender alveolar walls and open alveoli with little or no fibrin in the lumen. The incidence of hemorrhage or capillary congestion was minimal and not significantly different between the treatment conditions (Table 1, Fig 4). Lung protection in the APRV group was not secondary to lower Vt. The Vt was significantly higher in the APRV (12.9±0.2 ml/kg) as compared with the VC (9.5±0.2 ml/kg) group (p<0.05)
Figure 4.
Histological comparison of a rats receiving Volume Cycled Ventilation (VC) vs. airway pressure release ventilation (APRV). The VC animal exhibits hallmarks of ARDS, including alveolar flooding (stars), fibrinous deposits in the air compartment (arrowheads) and high cellularity (between arrows). The APRV animal shows patent alveoli with notable preservation of nearly normal histology.
BALF and Lung Tissue data
BALF concentration of surfactant protein-A (SP-A) was higher in the APRV group but did not reach statistical significance, whereas the levels of SP-B, total protein of BALF, and E-cadherin in lung tissue homogenates, were all significantly different between groups (Table 2).
Table 2.
Bronchoalveolar Lavage (BALF) and Lung Tissue Analysis
| VC (n=5) | APRV (n=4) | |
|---|---|---|
| Relative SP-A | 0.15 ± 0.04 | 0.22 ± 0.06 |
| Relative SP-B | 0.17 ± 0.07 | 0.59 ± 0.13* |
| Total Protein (μg/ml of BAL) | 4579.4 ± 572.8 | 2201.0 ± 825.2* |
| Relative E-cadherin | 1.0 ± 0.6 | 3.4 ± 0.6* |
Volume Cycled ventilation (VC) and Airway Pressure Release Ventilation (APRV) groups. BALF: Surfactant protein A (SP-A) and B (SP-B), Total Protein Concentration. Tissue Homogenate: Endothelial Cadherin (E-cadherin), Data Mean±SEM.
p<0.05 (APRV vs VC).
Fluid Balance
VC and APRV groups received a similar volume of fluid resuscitation with Lactated Ringer’s (VC 176.1 ± 12.7 and APRV 169.3 ± 17.5 ml, p=NS).
Discussion
The most important finding in this study was that a preemptive ventilation strategy with an extended airway P/TP applied following T/HS and prior to onset of acute lung injury, prevented the development of ARDS. This was evidenced by both lung function measurements and histopathology of lung tissue. The mechanisms of this protection include preventing the development of pulmonary edema (histology), which may have been secondary to a decrease in endothelial (Total Protein), and epithelial (E-cadherin) permeability resulting in maintenance of normal surfactant function (SP-B). Lastly, in vivo microscopy of the subpleural alveoli demonstrated that APRV preserved alveolar patency and stability, which could be secondary to the extended time at PHigh as well as the preventing loss of SP-B, preserving surfactant function. These data support the conclusions of two previous studies utilizing a porcine peritoneal sepsis and gut ischemia/reperfusion (PS+I/R)-induced ARDS model [10, 11] that preemptive APRV can prevent ARDS. The present study builds on this past work demonstrating that preemptive application of APRV is also effective at blocking lung injury in a T/HS-induced ARDS model. Lung protection in the T/HS model appears to be by mechanisms similar to the lung protection in the PS+I/R model (i.e. preventing increased permeability, alveolar edema, surfactant deactivation, and alveolar instability). Furthermore the in vivo microscopy data in the present study allows direct visual confirmation of alveolar stability imparted by APRV, which was not possible in the porcine model. This study therefore represents an expanded application of our preemptive ventilation strategy to the trauma/hemorrhagic shock population.
The Need for a Preventive Approach
Two recent reviews of therapeutic clinical trials for ARDS spanning three decades show that LTV is the only treatment strategy that can be recommended [5, 20]. However this current standard of care for management of ARDS, ventilation with LTV, has recently been shown to still have an unacceptably high mortality (40–60%) [2]. In addition, longitudinal study of ARDS survivors has revealed that they suffer debilitating lifelong sequelae including function-limiting pulmonary, psychological [4], and neurologic [21] dysfunction. Since no treatment has been shown effective for established-ARDS [5, 20], including LTV [2] and many patients that do survive have lifelong disabilities [4] [21] preventing ARDS development would have a tremendous positive impact on patient care.
Successful prevention of ARDS requires a temporal “window of opportunity” during disease onset in which treatment strategies can interrupt disease progression. However the current perception is that ARDS is a binary construct, the disease seen as either present or absent. The patient’s lungs are considered ‘healthy’ before the diagnosis of ARDS and ‘sick’ thereafter [8]. Therefore, treatment of ARDS often does not begin until the disease is fully developed [22]. However, the recent shift in ARDS definition by the Berlin Conference suggests a staged disease with Mild, Moderate or Severe ARDS [23]. Our group has suggested an even earlier stage, before the development of clinical symptoms, and has termed this the Occult stage [10]. This novel reconception of ARDS as a progressive injury is supported by the finding that ARDS is rarely present at the time of hospital admission but rather develops over a period of hours to days in the hospital [24]. Furthermore, the findings of Shari et al [24] suggest a ‘window of opportunity’ exists during which application of preventative strategies may block progression from occult lung injury to ARDS. Experimental data from our group including the present study support this hypothesis, demonstrating that an appropriate ventilator technique targeting early pathologic mechanisms during this Occult stage can prevent disease progression to established-ARDS [10, 11].
Pressure-Time Profile (P/TP)
The key early event in the pathogenesis of ARDS is the increase in vascular permeability that results from massive systemic inflammation[6]. Increased permeability leads to proteinaceous edema fluid flooding the alveolar space, which deactivates surfactant. Application of mechanical ventilation to the lung in the context of this pathologic milieu results in alveolar instability with associated mechanical and biological trauma [6]. Ventilation with extended P/TP appears to block the increase in permeability thereby blocking the subsequent downstream events that would lead to ARDS.
There are four basic components that can be manipulated during the mechanical breath: Time (TI) and Pressure (PI) at Inspiration and Time (TE) and Pressure (PE) at expiration along with the transition time between inspiration and expiration (ΔPI/PE). Airway P/TP represents the integration of these quantities, as calculated by Equation 1, and therefore reflects the forces applied at the alveolar surface by the ventilator. The impact of P/TP on lung fluid balance (i.e. pulmonary edema), surfactant function, and alveolar stability are the proposed mechanism of preemptive extended airway P/TP induced lung protection. Our study supports early physiology literature that studied the effect of increased Positive End-Expiratory Pressure (PEEP) on lung fluid balance and showed that PEEP-induced modification of the Starling forces are the likely mechanism of edema prevention [25–35].
P/TP and Edema
The literature investigating the effect of airway P/TP on lung fluid balance has almost exclusively focused on only one of the four P/TP components – the pressure at expiration (i.e. PEEP). It has been shown that if PEEP is applied following lung injury, then the accumulated edema is not decreased but rather redistributed within the lung[36, 37]. However, if preemptive PEEP is applied to the normal lung before the insult has been applied the development of pulmonary edema will be significantly reduced [25–33] [34, 35]. These data demonstrate that elevated P/TP in the form of PEEP prevents development of pulmonary edema if applied to the normal lung. The technique of APRV used in the present study significantly extends P/TP by sustaining a relatively constant airway pressure (PHigh) for > 90% of the duration of the breath (Thigh) with a sub-second release (Tlow) to allow for CO2 clearance. We postulate that it is this sustained pressure on the pulmonary interstitium that is the key mechanism of reduced pulmonary edema in the APRV group. This study demonstrates that an extended airway P/TP applied early can be protective; additional studies are underway to further analyze each component of the airway P/TP and identify which are critical to lung protection.
Critique of the Study
This pilot study demonstrates that preemptive application of APRV will prevent ARDS development in a rat T/HS model. These data combined with the results from our sepsis and a gut I/R model [10, 11] suggest that ARDS can be prevented regardless if the origin of lung injury is T/HS or sepsis. One limitation of this study is that we did not include a Control Ventilator-Only group. The reason for not including a Ventilator-Only Group was that this preliminary study was not designed to differentiate between the degree of lung injury caused by systemic inflammation, (i.e. T/HS), and the lung injury caused directly by mechanical ventilation. Future studies in which rats are mechanically ventilated but not subjected to T/HS and rats subjected to T/HS without mechanical ventilation will be necessary to obtain this information. The data from this study are still highly significant since they show that preemptive application of a protective mechanical ventilation strategy following systemic inflammation (T/HS) but before the beginning of lung injury will block disease progression and prevent ARDS. These data suggest that ARDS may be prevented in patients at risk.
Nor was this study designed to compare multiple preemptive ventilator strategies, but rather to show that progression of lung injury could be blocked with an appropriate mechanical ventilation strategy secondary to reduction in the four key drivers of ARDS pathophysiology (i.e. increased permeability, alveolar edema, surfactant deactivation and alveolar instability). We chose the ventilator settings in the VC group to be similar to those often used in surgery patients [12–15] since our model of T/HS simulates the trauma patient who would often undergo surgery and subsequently be treated in the Surgical Intensive Care Unit (SICU). However, it is very possible that preemptive application of VC with a low Vt and higher PEEP might also prevent ARDS development, similar to APRV. Further research is necessary before the optimal mechanical breath P/TP necessary to prevent ARDS is determined.
Conclusion
This study suggests that T/HS-induced ARDS can be prevented by preemptive application of a mechanical breath with an extended airway pressure P/TP delivered via the APRV mode. This pilot study demonstrates proof-of-concept that prevention of progressive lung injury is possible in the T/HS setting. To our knowledge this is the first trauma/hemorrhagic shock-induced lung injury model in a rat, which demonstrates that ARDS can be prevented with appropriate preemptive mechanical ventilation. These data expand on prior work from our lab, which showed the effectiveness of early APRV in preventing PS+I/R-induced ARDS and thus extends the applicability of a preemptive ventilation strategy to the trauma population. Having established this small animal T/HS -induced ARDS model, and proof-of-concept of prevention; future studies will focus on optimizing a variety of preemptive ventilation strategies. This novel therapeutic approach, if successful in humans, would change the clinical paradigm from treating to preventing ARDS. Indeed, Villar and Slutsky recently commented that, “ARDS is no longer a syndrome that must be treated, but is a syndrome that should be prevented [38]”.
Acknowledgments
This work was funded in part by NIH 1R21HL092801-01
Footnotes
There are no conflicts of interest.
Contributor Information
Shreyas K. Roy, Email: shreyas.roy@gmail.com.
Bryanna Emr, Email: bryemr@gmail.com.
Benjamin Sadowitz, Email: sadowtizbd@gmail.com.
Louis A. Gatto, Email: Louis.Gatto@cortland.edu.
Auyon Ghosh, Email: Auyon.Ghosh@gmail.com.
Joshua M. Satalin, Email: satalinj@upstate.edu.
Kathy P. Snyder, Email: snyderk@upstate.edu.
Lin Ge, Email: gel@upstate.edu.
Guirong Wang, Email: wangg@upstate.edu.
William Marx, Email: William.Marx@va.gov.
David Dean, Email: David_Dean@URMC.Rochester.edu.
Penny Andrews, Email: plandrews@intensivecareonline.com.
Anil Singh, Email: dsanil01@gmail.com.
Thomas Scalea, Email: tscalea@umm.edu.
Nader Habashi, Email: nmhabashi@gmail.com.
Gary F. Nieman, Email: niemang@upstate.edu.
References
- 1.Treggiari MM, Hudson LD, Martin DP, Weiss NS, Caldwell E, Rubenfeld G. Effect of acute lung injury and acute respiratory distress syndrome on outcome in critically ill trauma patients. Critical care medicine. 2004;32(2):327–331. doi: 10.1097/01.CCM.0000108870.09693.42. [DOI] [PubMed] [Google Scholar]
- 2.Villar J, Blanco J, Anon JM, Santos-Bouza A, Blanch L, Ambros A, Gandia F, Carriedo D, Mosteiro F, Basaldua S, et al. The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive care medicine. 2011;37(12):1932–1941. doi: 10.1007/s00134-011-2380-4. [DOI] [PubMed] [Google Scholar]
- 3.Cheung AM, Tansey CM, Tomlinson G, Diaz-Granados N, Matte A, Barr A, Mehta S, Mazer CD, Guest CB, Stewart TE, et al. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. American journal of respiratory and critical care medicine. 2006;174(5):538–544. doi: 10.1164/rccm.200505-693OC. [DOI] [PubMed] [Google Scholar]
- 4.Herridge MS, Tansey CM, Matte A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, et al. Functional disability 5 years after acute respiratory distress syndrome. The New England journal of medicine. 2011;364(14):1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 5.McIntyre RC, Jr, Pulido EJ, Bensard DD, Shames BD, Abraham E. Thirty years of clinical trials in acute respiratory distress syndrome. Critical care medicine. 2000;28 (9):3314–3331. doi: 10.1097/00003246-200009000-00034. [DOI] [PubMed] [Google Scholar]
- 6.Ware LB. Pathophysiology of acute lung injury and the acute respiratory distress syndrome. Seminars in respiratory and critical care medicine. 2006;27(4):337–349. doi: 10.1055/s-2006-948288. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed A, Kojicic M, Herasevich V, Gajic O. Early identification of patients with or at risk of acute lung injury. The Netherlands journal of medicine. 2009;67(9):268–271. [PubMed] [Google Scholar]
- 8.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. The New England journal of medicine. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 9.Otto CM, Markstaller K, Kajikawa O, Karmrodt J, Syring RS, Pfeiffer B, Good VP, Frevert CW, Baumgardner JE. Spatial and temporal heterogeneity of ventilator-associated lung injury after surfactant depletion. Journal of applied physiology. 2008;104(5):1485–1494. doi: 10.1152/japplphysiol.01089.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roy S, Sadowitz B, Andrews P, Gatto LA, Marx W, Ge L, Wang G, Lin X, Dean DA, Kuhn M, et al. Early stabilizing alveolar ventilation prevents acute respiratory distress syndrome: a novel timing-based ventilatory intervention to avert lung injury. The journal of trauma and acute care surgery. 2012;73(2):391–400. doi: 10.1097/TA.0b013e31825c7a82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roy S, Habashi N, Sadowitz B, Andrews P, Ge L, Wang G, Roy P, Ghosh A, Kuhn M, Satalin J, et al. Early Airway Pressure Release Ventilation Prevents Ards-a Novel Preventive Approach to Lung Injury. Shock. 2013;39(1):28–38. doi: 10.1097/SHK.0b013e31827b47bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Michelet P, D’Journo XB, Roch A, Doddoli C, Marin V, Papazian L, Decamps I, Bregeon F, Thomas P, Auffray JP. Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology. 2006;105(5):911–919. doi: 10.1097/00000542-200611000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Wrigge H, Zinserling J, Stuber F, von Spiegel T, Hering R, Wetegrove S, Hoeft A, Putensen C. Effects of mechanical ventilation on release of cytokines into systemic circulation in patients with normal pulmonary function. Anesthesiology. 2000;93(6):1413–1417. doi: 10.1097/00000542-200012000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Wrigge H, Uhlig U, Zinserling J, Behrends-Callsen E, Ottersbach G, Fischer M, Uhlig S, Putensen C. The effects of different ventilatory settings on pulmonary and systemic inflammatory responses during major surgery. Anesthesia and analgesia. 2004;98(3):775–781. doi: 10.1213/01.ane.0000100663.11852.bf. table of contents. [DOI] [PubMed] [Google Scholar]
- 15.Lipes J, Bojmehrani A, Lellouche F. Low Tidal Volume Ventilation in Patients without Acute Respiratory Distress Syndrome: A Paradigm Shift in Mechanical Ventilation. Critical care research and practice. 2012;2012:416862. doi: 10.1155/2012/416862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Habashi NM. Other approaches to open-lung ventilation: airway pressure release ventilation. Critical care medicine. 2005;33(3 Suppl):S228–240. doi: 10.1097/01.ccm.0000155920.11893.37. [DOI] [PubMed] [Google Scholar]
- 17.Pavone L, Albert S, DiRocco J, Gatto L, Nieman G. Alveolar instability caused by mechanical ventilation initially damages the nondependent normal lung. Critical care. 2007;11(5):R104. doi: 10.1186/cc6122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang G, Taneva S, Keough KM, Floros J. Differential effects of human SP-A1 and SP-A2 variants on phospholipid monolayers containing surfactant protein B. Biochimica et biophysica acta. 2007;1768(9):2060–2069. doi: 10.1016/j.bbamem.2007.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Machado-Aranda D, Adir Y, Young JL, Briva A, Budinger GR, Yeldandi AV, Sznajder JI, Dean DA. Gene transfer of the Na+, K+-ATPase beta1 subunit using electroporation increases lung liquid clearance. American journal of respiratory and critical care medicine. 2005;171(3):204–211. doi: 10.1164/rccm.200403-313OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cepkova M, Matthay MA. Pharmacotherapy of acute lung injury and the acute respiratory distress syndrome. J Intensive Care Med. 2006;21(3):119–143. doi: 10.1177/0885066606287045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mikkelsen ME, Christie JD, Lanken PN, Biester RC, Thompson BT, Bellamy SL, Localio AR, Demissie E, Hopkins RO, Angus DC. The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. American journal of respiratory and critical care medicine. 2012;185(12):1307–1315. doi: 10.1164/rccm.201111-2025OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, Rana R, St Sauver JL, Lymp JF, Afessa B, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Critical care medicine. 2004;32 (9):1817–1824. doi: 10.1097/01.ccm.0000133019.52531.30. [DOI] [PubMed] [Google Scholar]
- 23.Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni L, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive care medicine. 2012;38 (10):1573–1582. doi: 10.1007/s00134-012-2682-1. [DOI] [PubMed] [Google Scholar]
- 24.Shari G, Kojicic M, Li G, Cartin-Ceba R, Alvarez CT, Kashyap R, Dong Y, Poulose JT, Herasevich V, Garza JA, et al. Timing of the onset of acute respiratory distress syndrome: a population-based study. Respiratory care. 2011;56(5):576–582. doi: 10.4187/respcare.00901. [DOI] [PubMed] [Google Scholar]
- 25.Bshouty Z, Ali J, Younes M. Effect of tidal volume and PEEP on rate of edema formation in in situ perfused canine lobes. Journal of applied physiology. 1988;64 (5):1900–1907. doi: 10.1152/jappl.1988.64.5.1900. [DOI] [PubMed] [Google Scholar]
- 26.Piacentini E, Lopez-Aguilar J, Garcia-Martin C, Villagra A, Saenz-Valiente A, Murias G, Fernandez-Segoviano P, Hotchkiss JR, Blanch L. Effects of vascular flow and PEEP in a multiple hit model of lung injury in isolated perfused rabbit lungs. The Journal of trauma. 2008;65(1):147–153. doi: 10.1097/TA.0b013e31813e0904. [DOI] [PubMed] [Google Scholar]
- 27.Schumann S, Kirschbaum A, Schliessmann SJ, Wagner G, Goebel U, Priebe HJ, Guttmann J. Low pulmonary artery flush perfusion pressure combined with high positive end-expiratory pressure reduces oedema formation in isolated porcine lungs. Physiological measurement. 2010;31(2):261–272. doi: 10.1088/0967-3334/31/2/011. [DOI] [PubMed] [Google Scholar]
- 28.Fernandez Mondejar E, Vazquez Mata G, Cardenas A, Mansilla A, Cantalejo F, Rivera R. Ventilation with positive end-expiratory pressure reduces extravascular lung water and increases lymphatic flow in hydrostatic pulmonary edema. Critical care medicine. 1996;24(9):1562–1567. doi: 10.1097/00003246-199609000-00022. [DOI] [PubMed] [Google Scholar]
- 29.Myers JC, Reilley TE, Cloutier CT. Effect of positive end-expiratory pressure on extravascular lung water in porcine acute respiratory failure. Critical care medicine. 1988;16(1):52–54. doi: 10.1097/00003246-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Colmenero-Ruiz M, Fernandez-Mondejar E, Fernandez-Sacristan MA, Rivera-Fernandez R, Vazquez-Mata G. PEEP and low tidal volume ventilation reduce lung water in porcine pulmonary edema. American journal of respiratory and critical care medicine. 1997;155(3):964–970. doi: 10.1164/ajrccm.155.3.9117033. [DOI] [PubMed] [Google Scholar]
- 31.Russell JA, Hoeffel J, Murray JF. Effect of different levels of positive end-expiratory pressure on lung water content. Journal of applied physiology. 1982;53(1):9–15. doi: 10.1152/jappl.1982.53.1.9. [DOI] [PubMed] [Google Scholar]
- 32.Goldberg HS, Mitzner W, Batra G. Effect of transpulmonary and vascular pressures on rate of pulmonary edema formation. Journal of applied physiology. 1977;43(1):14–19. doi: 10.1152/jappl.1977.43.1.14. [DOI] [PubMed] [Google Scholar]
- 33.Luecke T, Roth H, Herrmann P, Joachim A, Weisser G, Pelosi P, Quintel M. PEEP decreases atelectasis and extravascular lung water but not lung tissue volume in surfactant-washout lung injury. Intensive care medicine. 2003;29(11):2026–2033. doi: 10.1007/s00134-003-1906-9. [DOI] [PubMed] [Google Scholar]
- 34.Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. The American review of respiratory disease. 1974;110(5):556–565. doi: 10.1164/arrd.1974.110.5.556. [DOI] [PubMed] [Google Scholar]
- 35.Dreyfuss D, Soler P, Basset G, Saumon G. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. The American review of respiratory disease. 1988;137(5):1159–1164. doi: 10.1164/ajrccm/137.5.1159. [DOI] [PubMed] [Google Scholar]
- 36.Pare PD, Warriner B, Baile EM, Hogg JC. Redistribution of pulmonary extravascular water with positive end-expiratory pressure in canine pulmonary edema. The American review of respiratory disease. 1983;127(5):590–593. doi: 10.1164/arrd.1983.127.5.590. [DOI] [PubMed] [Google Scholar]
- 37.Malo J, Ali J, Wood LD. How does positive end-expiratory pressure reduce intrapulmonary shunt in canine pulmonary edema? Journal of applied physiology. 1984;57(4):1002–1010. doi: 10.1152/jappl.1984.57.4.1002. [DOI] [PubMed] [Google Scholar]
- 38.Villar J, Slutsky AS. Is acute respiratory distress syndrome an iatrogenic disease? Critical care. 2010;14(1):120. doi: 10.1186/cc8842. [DOI] [PMC free article] [PubMed] [Google Scholar]