Abstract
Structural interventions may help reduce racial/ethnic disparities in HIV. In 2009 to 2011, we randomized pharmacies participating in a nonprescription syringe access program in minority communities to intervention (pharmacy enrolled and delivered HIV risk reduction information to injection drug users [IDUs]), primary control (pharmacy only enrolled IDUs), and secondary control (pharmacy did not engage IDUs). Intervention pharmacy staff reported more support for syringe sales than did control staff. An expanded pharmacy role in HIV risk reduction may be helpful.
Evidence supports the efficacy of both structural interventions targeting policy, organizational, and other sociocontextual factors and multilevel interventions targeting both individual and structural factors.1–3 However, few robust studies of this type of intervention have contributed to the HIV literature.4,5 Amelioration of persistent racial disparities in HIV/AIDS may require structural and multilevel interventions in heavily burdened communities.5,6
The New York State Expanded Syringe Access Program (ESAP), a structural-level HIV prevention strategy that began in 2001 and allows nonprescription syringe sales in pharmacies to help reduce HIV transmission among injection drug users (IDUs), demonstrated improved access to sterile syringes,7 safe syringe disposal,8,9 and reduced syringe sharing.10 Minority IDUs, however, have less access to ESAP.6,11–14
The Pharmacies as Resources Making Links to Community Services intervention, a large-scale, randomized structural intervention targeting community members, pharmacy staff, and IDUs patronizing pharmacies in New York City neighborhoods with high proportions of minorities and significant drug activity, began in 2009.5 We investigated the impact of this intervention on pharmacy staff support of (1) ESAP, (2) in-pharmacy HIV testing, and (3) in-pharmacy vaccination.
METHODS
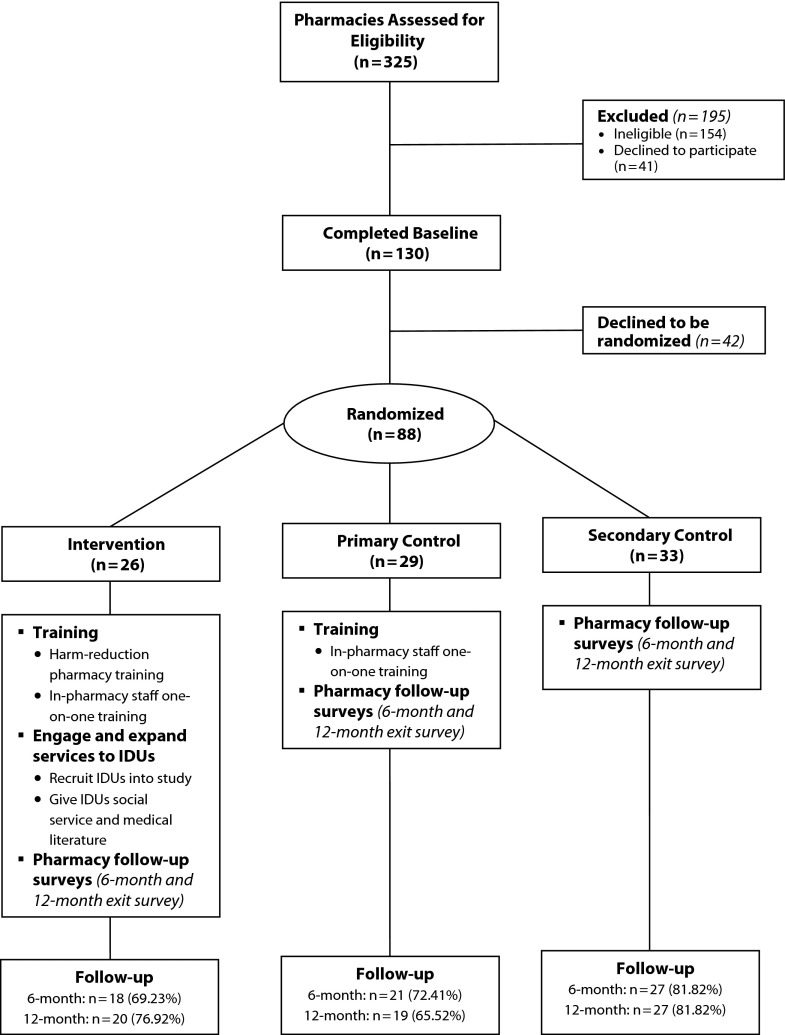
Our study methods are described elsewhere.15 Briefly, in 2009 we screened ESAP-registered pharmacies for eligibility by phone. Eligible pharmacies reported at least 1 new IDU syringe customer each month, had at least 1 new syringe customer who became a regular customer, and sold syringes to IDUs without additional requirements. Of 325 pharmacies screened, 172 were eligible, staff in 130 pharmacies completed a baseline interview (in 2009 or 2010), and 88 pharmacies were randomized by borough (Figure 1). Among those randomized, we found no differences in attrition by pharmacy-level or staff-level characteristics.
FIGURE 1—
Pharmacy enrollment, randomization, and study procedures: Pharmacies as Resources Making Links to Community Services, 2009–2011.
Note. IDU = injection drug user.
Pharmacies randomized to the intervention (n = 26) underwent group and individual training guided by a manual we developed after a pilot study; it focused on harm reduction, drug dependence, HIV prevention, and other needed services in the surrounding community, and best approaches for recruiting and providing HIV risk reduction materials to IDU syringe customers. Training sessions included role playing and were conducted quarterly to prevent protocol violations, which we assessed during random test buys. Primary control pharmacies (n = 29) did not perform intervention activities and therefore received training only on IDU syringe customer recruitment. We enrolled secondary control pharmacies (n = 33), which received no training and only underwent pharmacy staff surveys, to estimate an intervention effect that accounted for potential pharmacy participation bias that might result with the primary control group. All pharmacy staff completed a 40-minute baseline, 6-month, and 12-month computer-assisted interview.15 We measured intervention outcomes among both pharmacy staff and pharmacy-recruited syringe customers, but reported only pharmacy outcomes here. We terminated the participation of 1 intervention and 1 primary control pharmacy because of 2 or more protocol violations.
We examined support of ESAP, in-pharmacy HIV testing, and in-pharmacy vaccination over time by study arm and differences after the intervention by study arm. Because influenza vaccinations are becoming regularly available in pharmacies, willingness to provide vaccinations in the pharmacy may indicate greater access to these vaccinations as well as other important vaccinations such as Hepatitis B for IDUs. After baseline adjustment for support and clustering of staff within pharmacies, we estimated postintervention support levels with log-binomial regression models specifying a robust error to calculate prevalence ratios. We used SAS version 9.2 for these analyses.16
RESULTS
We found no differences in pharmacy (pharmacy type, borough) or staff (gender, position, perceived neighborhood drug activity) characteristics by study arm with exception of larger proportions of African American staff in the primary and secondary control pharmacies.
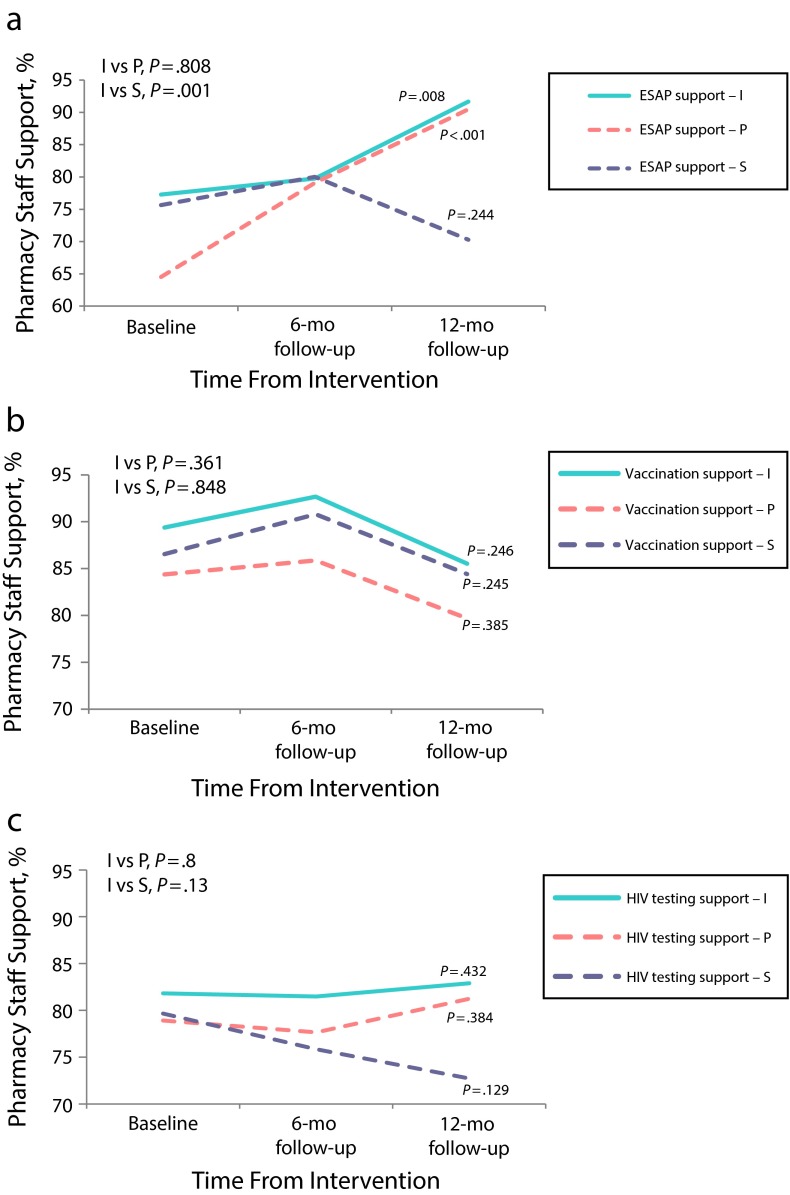
Even with high levels of ESAP support among pharmacy staff at baseline (65%–77%), support significantly increased in both intervention and primary control pharmacies following the intervention (Figure 2). After adjustment, ESAP support was significantly higher in the intervention than the secondary control pharmacies after the intervention (Table 1). We observed no intervention effect on support for in-pharmacy vaccination or HIV testing.
FIGURE 2—
Pharmacy staff support of extended pharmacy services for injection drug user syringe customers, before and after intervention, for (a) ESAP, (b) in-pharmacy vaccination, and (c) in-pharmacy HIV testing: Pharmacies as Resources Making Links to Community Services, 2009–2011.
Note. ESAP = New York State Expanded Syringe Access Program; I = intervention; P = primary control; S = secondary control. Sample size of pharmacy staff was n = 383. These data represent pharmacy staff in 26 intervention, 29 primary control, and 33 secondary control sites at baseline; 18 intervention, 21 primary control, and 27 secondary control sites at 6-mo follow-up; and 20 intervention, 19 primary control, and 27 secondary control sites at 12-mo follow-up. P values represent group differences at 12-mo follow-up (I vs P; I vs S) or the trend in pharmacy support over time (individual values).
TABLE 1—
Adjusted Associations of Pharmacy Staff Postintervention Support for the New York State Expanded Syringe Access Program: Pharmacies as Resources Making Links to Community Services, 2009–2011
| ESAP Support | Model 1,a PR (95% CI) | Model 2,b PR (95% CI) | Model 3,c PR (95% CI) |
| Intervention vs primary control group | 1.04 (0.93, 1.16) | 1.05 (0.94, 1.16) | 1.05 (0.94, 1.16) |
| Intervention vs secondary control group | 1.36** (1.15, 1.60) | 1.27** (1.11, 1.46) | 1.27** (1.11, 1.47) |
Note. CI = confidence interval; ESAP = Expanded Syringe Access Program; PR = prevalence ratio.
Adjusted for clustering of individuals within pharmacies.
Adjusted for clustering of individuals within pharmacies and baseline differences in ESAP support.
Adjusted for clustering of individuals within pharmacies, baseline differences in ESAP support, and race.
*P ≤ .05; **P ≤ .01.
DISCUSSION
These data suggest that a multilevel intervention approach that targets individual pharmacy staff (providing education and training) and pharmacy practice (coupling syringe sales with HIV prevention information and referrals) may strengthen the potential for an intervention effect. This is supported by (1) the significant increase in ESAP support in intervention pharmacies, where pharmacy staff were required to dedicate additional time and effort (vs control pharmacies), and (2) an intervention effect emerging in the presence of high baseline prevalence of support.
Some study limitations may have influenced our findings. Individual characteristics (other than race/ethnicity) could have been unevenly distributed across study arms following randomization. However, we explored factors that we were aware of from previous reports and found they did not differ by study arm. Selection bias could have influenced the results. For example, pharmacies with more positive beliefs about ESAP might have opted to participate, making it more difficult to detect an effect for the other outcomes under study; if true, effects might be greater in communities where support is lower. Finally, external validity is limited to pharmacies in New York City neighborhoods with high levels of drug activity.
Multilevel interventions should be considered in the delivery of HIV prevention services, particularly among populations with unmet health care needs.15,17–22
Acknowledgments
This study was funded by the National Institute on Drug Abuse (R01 DA022144) and the Robert Wood Johnson Health and Society Scholars program.
We also thank Pharmacies as Resources Making Links to Community Services (PHARM-Link) research and staff, the PHARM-Link Community Working Group (Wesley Badillo, New York State Department of Health AIDS Institute; Ann Boyer, Mount Sinai Medical Center; Dwight Brown, VIP Community Services; Nadine Ranger, Brooklyn AIDS Task Force; Jose Martin Garcia Orduna, East Harlem HIV Care Center; Laurell Lasenburg, Bronx District Public Health Office; Stuart Feldman, Touro College of Pharmacy; Camagu Tuswa, Swan Pharmacy), and PHARM-Link participants.
Human Participant Protection
Columbia University Medical Center and the New York Academy of Medicine institutional review boards approved the study. Informed consent was provided by all participants.
References
- 1.Friedman SR, Neaigus A, Des Jarlais DC et al. Social intervention against AIDS among injecting drug users. Br J Addict. 1992;87(3):393–404. doi: 10.1111/j.1360-0443.1992.tb01940.x. [DOI] [PubMed] [Google Scholar]
- 2.Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural interventions: concepts, challenges and opportunities for research. J Urban Health. 2006;83(1):59–72. doi: 10.1007/s11524-005-9007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blankenship KM, Bray SJ, Merson MH. Structural interventions in public health. AIDS. 2000;14(suppl 1):S11–S21. doi: 10.1097/00002030-200006001-00003. [DOI] [PubMed] [Google Scholar]
- 4.Manhart LE, Holmes KK. Randomized controlled trials of individual-level, population-level, and multilevel interventions for preventing sexually transmitted infections: what has worked? J Infect Dis. 2005;191(suppl 1):S7–S24. doi: 10.1086/425275. [DOI] [PubMed] [Google Scholar]
- 5.Fuller CM, Galea S, Caceres W, Blaney S, Sisco S, Vlahov D. Multilevel community-based intervention to increase access to sterile syringes among injection drug users through pharmacy sales in New York City. Am J Public Health. 2007;97(1):117–124. doi: 10.2105/AJPH.2005.069591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.HIV/AIDS Surveillance Report, 2007. Atlanta, GA: Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 7.Deren S, Cleland CM, Fuller C, Kang SY, Des Jarlais DC, Vlahov D. The impact of syringe deregulation on sources of syringes for injection drug users: preliminary findings. AIDS Behav. 2006;10(6):717–721. doi: 10.1007/s10461-006-9096-4. [DOI] [PubMed] [Google Scholar]
- 8.Cleland CM, Deren S, Fuller CM et al. Syringe disposal among injection drug users in Harlem and the Bronx during the New York State Expanded Syringe Access Demonstration Program. Health Educ Behav. 2007;34(2):390–403. doi: 10.1177/1090198106288560. [DOI] [PubMed] [Google Scholar]
- 9.Jones TS, Coffin PO. Preventing blood-borne infections through pharmacy syringe sales and safe community syringe disposal. J Am Pharm Assoc (Wash) 2002;42(6 suppl 2):S6–S9. doi: 10.1331/1086-5802.42.0.s6.jones. [DOI] [PubMed] [Google Scholar]
- 10.Pouget ER, Deren S, Fuller CM et al. Receptive syringe sharing among injection drug users in Harlem and the Bronx during the New York State Expanded Syringe Access Demonstration Program. J Acquir Immune Defic Syndr. 2005;39(4):471–477. doi: 10.1097/01.qai.0000152395.82885.c0. [DOI] [PubMed] [Google Scholar]
- 11.Fuller CM, Galea S, Blaney S et al. Explaining the relationship between race/ethnicity and pharmacy purchased syringes among injection drug users in New York City. Ethn Dis. 2004;14(4):589–596. [PubMed] [Google Scholar]
- 12.New York City HIV/AIDS Annual Surveillance Statistics. New York: New York City Department of Health and Mental Hygiene; 2010. [Google Scholar]
- 13.Cooper HL, Bossak BH, Tempalski B, Friedman SR, Des Jarlais DC. Temporal trends in spatial access to pharmacies that sell over-the-counter syringes in New York City health districts: relationship to local racial/ethnic composition and need. J Urban Health. 2009;86(6):929–945. doi: 10.1007/s11524-009-9399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper HL, Des Jarlais DC, Ross Z, Tempalski B, Bossak B, Friedman SR. Spatial access to syringe exchange programs and pharmacies selling over-the-counter syringes as predictors of drug injectors’ use of sterile syringes. Am J Public Health. 2011;101(6):1118–1125. doi: 10.2105/AJPH.2009.184580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rivera AV, Blaney S, Crawford ND et al. Individual- and neighborhood-level factors associated with nonprescription counseling in pharmacies participating in the New York State Expanded Syringe Access Program. J Am Pharm Assoc (2003) 2010;50(5):580–587. doi: 10.1331/JAPhA.2010.09202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Facilities EL, editor. SAS 9.2. Cary, NC: SAS Institute Inc; 2008. [Google Scholar]
- 17.Fuller CM, Ahern J, Vadnai L et al. Impact of increased syringe access: preliminary findings on injection drug user syringe source, disposal, and pharmacy sales in Harlem, New York. J Am Pharm Assoc (Wash) 2002;42(6 suppl 2):S77–S82. doi: 10.1331/1086-5802.42.0.s77.fuller. [DOI] [PubMed] [Google Scholar]
- 18.Vlahov D, Fuller C, Finkelstein R . New York State Expanded Syringe Access Demonstration Program: Evaluation Report to the Governor and the New York State Legislature. New York, NY: New York Academy of Medicine; 2003. [Google Scholar]
- 19.Crawford ND, Blaney S, Amesty S et al. Individual- and neighborhood-level characteristics associated with support of in-pharmacy vaccination among ESAP-registered pharmacies: pharmacists’ role in reducing racial/ethnic disparities in influenza vaccinations in New York City. J Urban Health. 2011;88(1):176–185. doi: 10.1007/s11524-010-9541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284(16):2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 21.Liddicoat RV, Horton NJ, Urban R, Maier E, Christiansen D, Samet JH. Assessing missed opportunities for HIV testing in medical settings. J Gen Intern Med. 2004;19(4):349–356. doi: 10.1111/j.1525-1497.2004.21251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Branson B. Current HIV epidemiology and revised recommendations for HIV testing in health-care settings. J Med Virol. 2007;79(suppl 1):S6–S10. doi: 10.1002/jmv.20972. [DOI] [PubMed] [Google Scholar]