Abstract
Objectives. We examined the effect on food purchases of adding recommended calorie intake per day or per meal to the mandated calorie information posted on chain restaurant menus.
Methods. Before and after New York City implemented calorie posting on chain restaurant menus in 2008, we provided daily, per-meal, or no calorie recommendations to randomized subsets of adult lunchtime customers (n = 1121) entering 2 McDonald’s restaurants, in Manhattan and Brooklyn, and collected receipts and survey responses as they exited. In linear and logistic regressions, with adjustment for gender, race, age, and day, we tested for simple differences in calories consumed and interactions between variables.
Results. Posting calorie benchmarks had no direct impact, nor did it moderate the impact of calorie labels on food purchases. The recommendation appeared to promote a slight increase in calorie intake, attributable to increased purchases of higher-calorie entrées.
Conclusions. These results do not support the introduction of calorie recommendations as a means of enhancing the impact of posted calorie information or reducing the contribution of restaurant dining to the obesity epidemic.
Obesity rates in the United States, having risen dramatically beginning in the 1980s,1 began to level off about a decade ago,2 albeit at the high rate of about one third of the population.3 Obesity increases the risk of chronic conditions such as diabetes and heart disease,4 accounting for an estimated 5% to 15% of annual deaths5,6 and $150 billion in annual health care costs in the United States.7 Such statistics have led policymakers to take a closer look at potential causes of, and opportunities for legislative response to, the obesity epidemic.
Restaurant meals are a natural target for policy interventions aimed at combating obesity. They have accounted for a growing fraction of calorie intake over time,8 and at the individual level, obesity is positively associated specifically with patronage of fast-food restaurants. These restaurants, which are especially popular with low-income individuals, who have a higher risk of obesity, encourage additional calorie consumption by promoting larger meals at minimal additional marginal cost.9,10 Although existing regulations require such restaurants to make calorie information available to customers, few customers seek out the information.11
To encourage use of calorie information by diners, several states and municipalities have introduced regulations that mandate posting of calorie information on the menus and menu boards of chain restaurants.12 New York City (Amended Health Code §81.50 2007); King County, Washington State (HB 3160 2008); Philadelphia, Pennsylvania (City Council Bill 080167 2008); San Francisco, California (Ordinance No. 40–08 2009); California State (SB 1420 2008); and Oregon (HB 2726 2009) have all implemented mandatory calorie-posting regulations, and nationwide regulations will soon go into effect as part of recent health care reform legislation (Pub L No. 111-148).
Existing literature on calorie labeling provides a mixed picture, at best, of its impact. Despite some promising laboratory studies,13 repeated and well-powered tests of menu labeling in situ have not been encouraging. Although consumers’ estimates of how many calories their meals contain improve,14 and those who report using labels tend to choose lower-calorie meals than those who report not using them,15,16 population-wide behavior has been found to respond little if at all to calorie posting.16–21
One commonly proposed reason for the apparent failure of menu labeling to change behavior, leading to a natural prescription for how to improve the effectiveness of such labeling, is that people lack guidelines about recommended calorie intake that could help them interpret the labels.22 Articulating such concerns, a year after introducing mandatory calorie posting, New York City augmented the policy with a campaign publicizing daily calorie recommendations.23 Going a step further, the mandatory calorie posting associated with national health care reform includes a requirement for restaurants to post daily recommended calories directly on menus. In the laboratory, a recommendation for daily calorie intake presented with dinner menus has been shown to reduce self-reported compensatory eating later in the evening,24 and in a field experiment it directly reduced meal calories when presented during meal choice.25 However, although both studies observed a direct effect of recommendations, neither found a significant interaction between calorie labeling and calorie recommendations, suggesting that the recommendation did not facilitate use of labels. Moreover, in the field study, the recommendation affected calorie intake by normal-weight restaurant patrons but had no impact on overweight diners.25
We examined whether providing calorie recommendations altered the impact of calorie posting on the calories purchased. Specifically, we explored the effectiveness of providing 1 of 2 levels of calorie recommendation, either the recommended number of calories per meal or the recommended number of calories per day. Our study was an experimental manipulation of the presence and type of calorie recommendation, embedded in a pre–post field study of New York City’s calorie-labeling regulations on consumer food purchases at 2 McDonald’s restaurants.21 We were interested in whether, consistent with earlier research, receiving such information at the point of purchase would affect calories purchased regardless of whether calorie information was posted or would interact with the menu labeling by aiding consumers in using the posted information. We considered not only the standard daily recommendation, but also recommended intake for the meal (lunch), in accordance with the mandate by the National School Lunch Act that school lunches provide at least one third of the daily recommended dietary allowances for key nutrients. We reasoned that meal rather than daily calorie recommendations might be more directly relatable, and hence more useful, in guiding decisions involving a single meal.
METHODS
We collected data within 2 months prior to and following implementation of menu-labeling regulations in 2008, as part of a larger study.21 We embedded an experimental manipulation of calorie recommendations into both prelabeling (n = 624) and postlabeling (n = 497) data collection. We collected all data prior to the launch of the city’s later campaign to promote daily calorie recommendations, which began in 2009.
Participants were 1121 adult (aged ≥ 18 years) lunchtime customers of 2 McDonald’s restaurants, one in Manhattan and another in Brooklyn. The experimental manipulation encompassed 3 arms, to which we randomly assigned participants. Customers approaching the restaurant were (1) handed a slip that showed recommended daily calories (2000 for women or 2400 for men26), (2) handed a slip with recommended per-meal calories (650 or 800), or (3) given no recommendation (control condition). The information consisted of a simple, short statement, with a second-grade Flesch–Kincaid reading level and a Flesch reading ease index of 100%.27 We asked all entering customers to retain their receipt for participation in an exit survey, and the recommendation slips advised participants to return the slip, providing a rough indication of information delivery. To minimize potential contamination effects of customers seeing recommendations other than the one they were assigned to, we conducted the 3 recommendation conditions in 2-hour blocks of time, counterbalanced across days and separated by short periods in which stray recommendation slips were removed from the site. Because we collected all data during lunchtime hours, only 2 experimental conditions could be implemented on any given day. Exiting customers were invited to complete a survey and provide their receipt, for which they were paid $5. People dining together might have been influenced by their companions’ orders, an effect that we could not control for. However, by implementing the recommendation manipulation in blocks of time, we ensured that dining partners were always randomized to the same condition.
The survey asked participants to estimate their meal’s calories and how many calories they thought “a doctor or nutritionist would recommend that you should eat for your daily diet” and to report whether they had looked at the calorie information on the menu and taken it into consideration when ordering, both on 7-point scales. Five participants (0.5%) gave responses more than 3 SDs above the mean daily recommendation (between 6000 and 25 000 calories), giving this variable high skew (F(1,1066) = 102.12) and high kurtosis (F(1,1066) = 841.69). We omitted these 5 participants from analyses examining estimated recommended daily calories, reducing this variable’s skew (F(1,1061) = 3.53), and kurtosis (F(1,1061) = −3.49).
Demographic questions were age, gender, race, home zip code (used to estimate household income), weight and height (to calculate body mass index, defined as weight in kilograms divided by height in meters squared), and whether the respondent was currently dieting. We calculated individualized daily caloric recommendations for each participant with Mifflin–St Jeor equations,28 assuming a sedentary lifestyle and subtracting 500 calories for participants who indicated that they were dieting (a typical recommended reduction level, aiming for 1 pound of weight loss per week). About 3% of participants declined to state their age or gender; 12% to 13% declined to provide height, weight, dieting status, or zip code; and 26% did not provide their racial or ethnic group. We excluded participants with missing data only from analyses that used the missing variables, with the exception of race.
After participants completed the survey, a researcher examined their restaurant receipt, looking for discrepancies and ambiguous entries, which were then resolved through consultation with the participant. For example, if a receipt contained items purchased for more than 1 customer, we annotated it to indicate who ordered each item. We calculated total calories for each meal item, including alterations (e.g., no cheese), with online, company-provided nutritional information. We excluded data for 27 participants (2.4%) who were missing important meal information (e.g., whether a soda was diet) that made it impossible to calculate the calories in their meal, leaving a total sample of 1094 persons.
We conducted simple correlations to determine which demographic and environmental variables correlated with total meal calories and thus should be controlled for. All findings remained at the same significance level irrespective of whether covariates were included. We incorporated these findings into an ordinary least squares linear regression to predict total meal calories from (1) calorie posting, (2) provision of either daily or per-meal recommendation, (3) a dummy variable for per-meal recommendation, and (4) study site (Brooklyn = 1). We controlled for data collection on Friday, female gender, African American race, and age, all covariates that emerged as significant correlates with the main outcome measure. Participants who declined to report their race were retained in the analysis, with values set to zero for that variable. A second model added the 2-way interaction terms of calorie posting with calorie recommendation (to test the hypothesized facilitation effect of recommendations), with per-meal recommendation, and with study site, as well as the interaction terms of study site with calorie recommendation and with per-meal recommendation. (We included study site as a covariate because of its strong interaction with the effect of menu labeling.) We conducted a series of linear and logistic regressions with these same predictors to explore their impact on components of the meal and perceptions of its calories as well as the accuracy of participants' personalized estimates of daily recommended calories. Regressions also tested whether any effects that emerged interacted with weight; we split the sample into overweight or obese (body mass index ≥ 25 kg/m2) versus normal or underweight (body mass index < 25 kg/m2) to determine whether the effects might be stronger or weaker for overweight individuals, who presumably need intervention the most. (Full regression tables are in Appendix A, available as a supplement to this article at http://www.ajph.org.)
RESULTS
The sample ranged in age from 18 to 89 years (mean = 36 years; SD = 14 years). Table 1 presents a detailed breakdown of demographic categories, along with mean calories purchased. We additionally compared participants who purchased what appeared to be their lunch against those merely buying a drink or a dessert (who might have been adding this purchase to a lunch acquired elsewhere). This variable did not interact with our randomized recommendation treatment, nor did it change our results, so we did not include it in any subsequent analyses. However, for interpretation of mean caloric intake it is important to note that among participants who purchased a meal, more than half exceeded the recommended caloric intake according to our guidelines: meals purchased by women averaged 824 calories and by men, 890 calories. About one third of our entire sample purchased meals with more than 1000 calories.
TABLE 1—
Descriptive Statistics of Participants in Study of Reactions to Menu Labeling and Calorie Recommendations: New York City, 2008
| Characteristic | No. (%) | Calories |
| Sample (excluding missing data) | 1094 | 765 |
| Type of purchase** | ||
| Drink or dessert only | 195 (18) | 355 |
| Any lunch food | 899 (82) | 854 |
| Gender | ||
| Men | 476 (44) | 756 |
| Women | 585 (53) | 766 |
| Not reporteda | 33 (3) | 756 |
| Race/ethnicity** | ||
| African American | 393 (36) | 814 |
| Asian | 41 (4) | 739 |
| Hispanic | 158 (14) | 807 |
| Whiteb | 170 (16) | 624 |
| Multiple selected | 20 (2) | 906 |
| Other | 28 (3) | 888 |
| Not reporteda | 284 (26) | 740 |
| BMI,* kg/m2 | ||
| ≤ 25 | 405 (37) | 730 |
| > 25 | 538 (49) | 797 |
| Not reporteda | 151 (14) | 747 |
Note. BMI = body mass index.
Observations with unreported values were excluded from these analyses.
In posthoc tests with a Sidak correction, White participants were significantly different from African Americans, Hispanics, and participants reporting multiple categories (P < .05). No other posthoc comparisons were statistically significant.
*P < .05; **P < .01.
Recommendations
More than two thirds of recommendation slips were returned, indicating that participants paid fairly good attention to their written content. Calories ordered did not differ between those who did and did not return the slips. Our intent-to-treat approach incorporated all participants in their assigned condition. Further evidence that the recommendation information was generally understood came from its effect on estimated daily calorie intake guidelines. Participants randomized to receive a recommendation had less error in their estimates of their own daily recommended calorie intake, as a function of the absolute difference between their estimates and the individualized calculated recommendation (mean error = 759) than control participants (mean error = 954; P = .001) and participants who received the per-meal recommendation (mean error = 891; P = .009). (The full regression is shown in Table A, available as a supplement to this article at http://www.ajph.org.) This relative improvement provides a manipulation check for delivery of the recommendation. Not surprisingly, the meal recommendation did not improve estimates of daily guidelines (P = .519). Consistent with previous work showing that people tend to underestimate their recommended daily calorie intake,14,25 we found that participants who received daily calorie target information gave higher estimates than did those who received no recommendation (1608 vs 1168 for men; 1369 vs 1147 for women), rather than lower as would have been expected if people tended to overestimate recommended calorie intake.
Providing a calorie recommendation did not appear to alter the use of posted calorie information: we detected no significant interaction between the recommendation and calorie posting (P = .74; Table 2). We also found no interaction between calorie posting and the per-meal recommendation or any main effect of the per-meal recommendation. A trend that approached significance (P = .07) suggested that the calorie recommendations might have a direct effect on purchases, although it was in the opposite direction from what would be desired.
TABLE 2—
Regressions Predicting Number of Calories Purchased, Testing Main Effects and Interactions Among Fast-Food Consumers Who Received a Per-Meal or Per-Day Calorie Recommendation or No Recommendation, Before and After the 2008 Implementation of Calorie Labeling in New York City
| Variable | Model 1: Main Effects, Calories (SE) | Model 2: Interactions, Calories (SE) |
| Constant | 743.15** (49.08) | 704.59** (56.52) |
| Calories posted | 17.74 (28.20) | 103.97a (58.30) |
| Either recommendationb | 61.44a (34.22) | 49.79 (53.19) |
| Per-meal recommendationc | −20.05 (33.07) | 26.81 (51.45) |
| Brooklyn | 83.61** (28.67) | 172.53** (57.43) |
| Friday | 30.37 (27.82) | 35.63 (27.84) |
| Women | −10.34 (28.33) | −11.24 (28.36) |
| African American | 63.64* (29.47) | 57.32a (29.64) |
| Age | −2.77** (0.99) | −2.73** (0.99) |
| Calories posted × either recommendation | 22.68 (69.51) | |
| Calories posted × per-meal recommendation | −72.17 (67.00) | |
| Calories posted × Brooklyn | −166.08** (56.66) | |
| Brooklyn × either recommendation | −1.48 (69.62) | |
| Brooklyn × per-meal recommendation | −39.82 (67.03) | |
| Model statistics | ||
| Omnibus F test | F(8,1027) = 3.59 | F(13,1022) = 2.99 |
| R2 | 0.027 | 0.037 |
Note. The sample size was n = 1036.
Data approached significance at P < .1.
Dummy code comparing the presence of either of the 2 calorie recommendation conditions to the control condition.
Dummy code comparing the per-meal recommendation to either of the other conditions.
*P < .05; **P < .01.
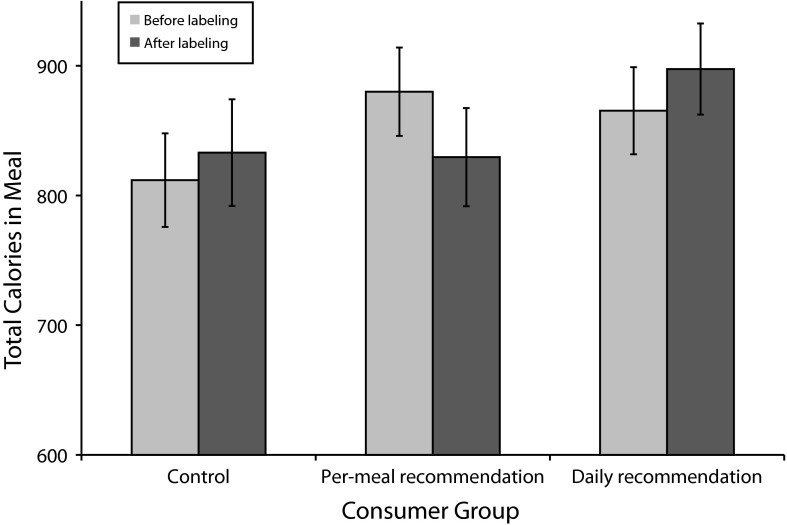
The recommendation is intended to guide those who are purchasing a meal, but 18% of participants (n = 195) were only purchasing a drink and thus might not be expected to respond to the recommendations. However, even excluding these participants, no interaction emerged between calorie posting and the recommendation (P = .81). Figure 1 depicts the marginal means for meal calories purchased across the 3 recommendation conditions, before and after calorie posting.
FIGURE 1—
Mean caloric content of meals purchased by fast-food consumers who received a per-meal or daily calorie recommendation or no recommendation, before and after the 2008 implementation of calorie labeling in New York City.
Note. Error bars indicate 1 SE.
Explanatory Analyses
Although the tendency for customers to order more when presented with calorie recommendations was not statistically significant, we considered the unexpected tendency for recommendations to backfire to be worthy of exploration. The comparisons with which we investigated this effect were, however, unplanned and should be interpreted with caution in light of the large number of statistical tests.
First, although calorie recommendations did not help overall, they could be seen as beneficial if they selectively led overweight people to either consume fewer calories (which would lead to a 2-way interaction between weight status and recommendations) or to use calorie labels more effectively (which would manifest as a 3-way interaction between weight status, labeling, and recommendation), even if they had a small or even negative impact on normal-weight people. When we entered weight status into the regression model (Table B, available as a supplement to this article at http://www.ajph.org), a main effect emerged such that overweight people ordered 68 more calories than normal-weight people (t(892) = 2.25; P = .03), and the detrimental main effect of the recommendation again approached significance (P = .06). Overweight status did not interact with the recommendation (P = .98), nor was there a 3-way interaction between overweight status, recommendation, and labeling (P = .47), suggesting that any effects of the recommendation were similar for normal-weight and overweight participants.
Next we explored whether the recommendation affected individual components of the meal or facilitated use of calorie labels differentially for different parts of the meal. Table 3 reports means of meal components before and after menu labeling went into effect, with and without a recommendation provided; the significance level of the main effect of the recommendation and its interaction with calorie posting are shown. The only effect to emerge was a main effect of calorie recommendation on entrée calories: participants who received a recommendation purchased entrées with 49 additional calories (t(1027) = 2.20; P = .028).
TABLE 3—
Calorie Consumption and Estimation Among Fast-Food Consumers Who Received a Per-Meal or Per-Day Calorie Recommendation or No Recommendation, Before and After the 2008 Implementation of Calorie Labeling in New York City
| Before Labeling |
After Labeling |
|||||
| No Recommendation, % or Mean (SD) | Per-Meal or Per-Day Recommendation, % or Mean (SD) | No Recommendation, % or Mean (SD) | Per-Meal or Per-Day Recommendation, % or Mean (SD) | Recommendation,a P | Interaction Effect,b P | |
| Entrée calories | 334 (274) | 369 (283) | 348 (324) | 410 (273) | .028 | .896 |
| Ordered drinkc | 42 | 48 | 55 | 58 | .131 | .314 |
| Ordered fries | 44 | 47 | 52 | 55 | .495 | .62 |
| Ordered dessert | 26 | 24 | 18 | 15 | .919 | .542 |
| Estimated caloriesd | 482 (487) | 563 (525) | 549 (414) | 648 (512) | .001 | .33 |
| Estimation errore | 436 (408) | 468 (411) | 348 (333) | 412 (379) | .932 | .564 |
| Looked for calories | 3.01 (2.0) | 3.10 (2.1) | 3.64 (2.1) | 3.30 (2.2) | .634 | .138 |
| Considered calories | 3.21 (2.1) | 3.32 (2.1) | 3.75 (2.1) | 3.47 (2.2) | .626 | .066 |
Significance levels for the main effect of receiving either recommendation (logistic regression for binary variables).
Significance levels for the interaction term between the pre- vs postlabeling measure and receiving either recommendation.
Excluding drinks with negligible calories (water, black coffee, diet soda).
Because the distribution of calorie estimates was highly skewed, estimates were log transformed for analysis; simple means are reported.
Absolute difference between log-transformed estimates of calories ordered and log-transformed actual calories.
Finally, we tested whether the recommendation enhanced the impact of menu labeling on customers’ beliefs about the calories in their meal. (On average, customers underestimated the calories in their meals in all conditions.) The calorie recommendations had a direct effect on estimated calories: recipients of a recommendation gave higher estimates of the calories in their meal (t(943) = 3.34; P = .001), but no interaction emerged between recommendation and menu labeling (t(938) < 1). This increase in estimation did not translate into any effect for estimation error (t(943) < 1), suggesting that participants may have been aware that they were ordering meals that were larger (although the difference was only marginally significant) when they received the recommendation.
DISCUSSION
Providing calorie recommendation benchmarks—such as calories per day or calories per meal—did not reduce calories purchased, nor did it appear to help participants to better use the calorie information posted on menus. In fact, we found some evidence that recommendations may even have promoted purchase of higher-calorie items. One might speculate that the recommendation provided an anchor against which to judge the main meal component (the entrée, such as a burger or other sandwich). The fact that many popular entrées are below the recommended guidelines (e.g., a Big Mac contains 570 calories) may provide a false sense of staying within the calorie allowance, which could license larger purchases and allow consumers to ignore the calorie load of other components of the meal, which would push the meal total beyond the recommended amount.
These results provide little hope that calorie recommendations will salvage the apparent weak or nonexistent effect of menu labeling in the field. As with previous research,25 providing a recommendation appeared to have its own, direct effect on consumption rather than making it easier for participants to use calorie information. In that study, the main effect was a beneficial one that seemed to be driven by the increased attention to the need to watch calories and was limited to normal-weight participants.25 It is unclear why the effects in our study tended to be in the opposite direction, but perhaps it is relevant that the different restaurant chains used in these 2 studies (McDonald’s in our study and Subway in Wisdom et al.) have different reputations for healthful fare, and, as a result, may attract different clientele. Interestingly, both studies found that recommendations tend to increase estimates of calorie allowances, further calling into question the anticipated value of providing this information. It is important to note, however, that in neither study did calorie recommendations facilitate use of menu labeling.
Limitations
Our study was subject to constraints similar to those of other field studies of menu-labeling legislation. We studied only customers patronizing fast-food establishments and did not measure whether participants consumed all purchased calories or whether their consumption later in the day changed. Our manipulation of the calorie recommendation was somewhat artificial, consisting of a very conspicuous slip of paper given to customers in the recommendation conditions; it is not known whether other methods for providing a recommendation (e.g., posting on menus) would have a different effect or whether repeated exposure to this information would increase the effect over time.
It may be worth considering other strategies for promoting the use of posted calorie information. For example, in a pilot study we found that consumers were more likely to use calorie information when options were organized into a simple, ordered list. By contrast, changing behavior through daily calorie recommendations would require consumers to perform fairly complex analyses, comparing the current meal to consumption behavior earlier in the day and intentions later in the day and adjusting for typical behavior on other days. We had expected that providing a per-meal recommendation might, by nature of the simplicity of the comparison, have a more beneficial effect, but it was of no more help than the daily recommendation. Most of the findings on this topic suggest that consumers are simply not making precise calculations when choosing restaurant meals, and so providing them with tools to make their computation more accurate misses an opportunity to intervene in a qualitatively different way, perhaps in a manner that would help with the decision that is actually being made.
Conclusions
Regardless of whether menu labeling has the intended effect of reducing calorie consumption, we are in agreement with policymakers that increased transparency in product labeling is inherently desirable.29 However, our results suggest that the effects of informational strategies on behavior are complex. Rather than increasing consumer burden with ever more information and education, policy efforts might gain more traction if directed toward avenues that make it easier for people to make healthier decisions. One such avenue could be the controversial use of bans or limits,30 but perhaps a more promising approach would be to incentivize restaurants and manufacturers to promote high-margin, healthier items.31 This could include, for example, a small discount for a person ordering a combo meal along with a diet soft drink or water rather than a regular soft drink.32
Our study has limited but clear policy implications. Our results do not support the introduction of calorie recommendations as a means of enhancing the impact of posted calorie information.
Acknowledgments
This research was supported by the US Department of Agriculture Economic Research Service (grants 58400060114 and 59400080077) and by a grant from the Center for Behavioral Decision Research, Carnegie Mellon University.
We gratefully acknowledge Anu Radhika Bhooshan, Michele Bradshaw, Margaret C. Della Vecchia, Terry Fedigan, Kamaria Hayden, Peter Kriss, Deborah Kuk, Jacqueline J. Lee, Diane Palladino, and Oleg Trofimov for help with data collection and entry.
Human Participant Protection
This research was approved by the institutional review board at Carnegie Mellon University.
References
- 1.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132(6):2087–2102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 2.Rokholm B, Baker JL, Sørensen TIA. The levelling off of the obesity epidemic since the year 1999—a review of evidence and perspectives. Obes Rev. 2010;11(12):835–846. doi: 10.1111/j.1467-789X.2010.00810.x. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999—2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 4.Burke GL, Bertoni AG, Shea S et al. The impact of obesity on cardiovascular disease risk factors and subclinical vascular disease: The Multi-Ethnic Study of Atherosclerosis. Arch Intern Med. 2008;168(9):928–935. doi: 10.1001/archinte.168.9.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 6.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: actual causes of death in the United States, 2000 [for JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. JAMA. 2005;293(3):293–294. [DOI] [PubMed] [Google Scholar]
- 7.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood) 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 8.Variyam JN. Nutrition Labeling in the Food-Away-From-Home Sector, An Economic Assessment. Washington, DC: US Department of Agriculture; 2005. Economic Research Report 4. [Google Scholar]
- 9.Bowman SA, Vinyard BT. Fast food Consumption of US adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr. 2004;23(2):163–168. doi: 10.1080/07315724.2004.10719357. [DOI] [PubMed] [Google Scholar]
- 10.Chou SY, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ. 2004;23(3):565–587. doi: 10.1016/j.jhealeco.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Roberto CA, Agnew H, Brownell KD. An observational study of consumers’ accessing nutritional information in chain restaurants. Am J Public Health. 2009;99(5):820–821. doi: 10.2105/AJPH.2008.136457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pomeranz JL, Brownell KD. Legal and public health considerations affecting the success, reach, and impact of menu-labeling laws. Am J Public Health. 2008;98(9):1578–1583. doi: 10.2105/AJPH.2007.128488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harnack LJ, French SA. Effect of point-of-purchase calorie labeling on restaurant and cafeteria food choices: a review of the literature. Int J Behav Nutr Phys Act. 2008;5:51. doi: 10.1186/1479-5868-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elbel B. Consumer estimation of recommended and actual calories at fast food restaurants. Obesity (Silver Spring) 2011;19(10):1971–1978. doi: 10.1038/oby.2011.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bassett MT, Dumanovsky T, Huang C et al. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am J Public Health. 2008;98(8):1457–1459. doi: 10.2105/AJPH.2008.135020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dumanovsky T, Huang CY, Nonas CA, Matte TD, Bassett MT, Silver LD. Changes in energy content of lunchtime purchases from fast food restaurants after introduction of calorie labelling: cross sectional customer surveys. BMJ. 2011;343 doi: 10.1136/bmj.d4464. d4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bollinger B, Leslie P, Sorensen A. Calorie posting in chain restaurants. Am Econ J Econ Policy. 2011;3(1):91–128. [Google Scholar]
- 18.Elbel B, Kersh R, Brescoll VL, Dixon BL. Calorie labeling and food choices: a first look at the effects on low-income people in New York City. Health Aff (Millwood) 2009;28(6):w1110–w1121. doi: 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 19.Elbel B, Gyamfi J, Kersh R. Child and adolescent fast-food choice and the influence of calorie labeling: a natural experiment. Int J Obes (Lond) 2011;35(4):493–500. doi: 10.1038/ijo.2011.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finkelstein EA, Strombotne KL, Chan NL, Krieger J. Mandatory menu labeling in one fast-food chain in King County, Washington. Am J Prev Med. 2011;40(2):122–127. doi: 10.1016/j.amepre.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 21.Wisdom J. Changing Eating Behaviors: Traditional and Behavioral Economic Approaches. Pittsburgh, PA: Carnegie Mellon University; 2011. [dissertation] [Google Scholar]
- 22. Nestle M. Why we shouldn’t ditch calorie labeling. Atlantic. October 7, 2009. Available at: http://business.theatlantic.com/2009/10/why_we_shouldnt_ditch_calorie_labeling.php. Accessed July 5, 2011.
- 23. New York City Department of Health and Mental Hygiene. Health Department launches calorie education campaign. 2008. Available at: http://www.nyc.gov/html/doh/html/pr2008/pr066-08.shtml. Accessed July 5, 2011.
- 24.Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. Am J Public Health. 2010;100(2):312–318. doi: 10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wisdom J, Downs JS, Loewenstein G. Promoting healthy choices: information vs convenience. Am Econ J Appl Econ. 2010;99(2):164–178. [Google Scholar]
- 26.Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: US Department of Agriculture and US Department of Health and Human Services; 2010. [Google Scholar]
- 27.Kincaid JP, Fishburne RP, Rogers RL, Chissom BS. Derivation of New Readability Formulas (Automated Readability Index, Fog Count, and Flesch Reading Ease Formula) for Navy Enlisted Personnel. Research Branch report 8-75. Memphis, TN: Naval Air Station; 1975. [Google Scholar]
- 28.Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc. 2005;105(5):775–789. doi: 10.1016/j.jada.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 29.Ludwig DS, Brownell KD. Public health action amid scientific uncertainty: the case of restaurant calorie labeling regulations. JAMA. 2009;302(4):434–435. doi: 10.1001/jama.2009.1045. [DOI] [PubMed] [Google Scholar]
- 30.Farley T, Just DR, Wansink B. Clinical decisions. Regulation of sugar-sweetened beverages. N Engl J Med. 2012;367(15):1464–1466. doi: 10.1056/NEJMclde1210278. [DOI] [PubMed] [Google Scholar]
- 31.Chandon P, Wansink B. Does food marketing need to make us fat? A review and solutions. Nutr Rev. 2012;70(10):571–593. doi: 10.1111/j.1753-4887.2012.00518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wansink B, Huckabee M. De-marketing obesity. Calif Manage Rev. 2005;47(4):6–18. [Google Scholar]