Abstract
Objectives. We examined the effect of estrogen avoidance on mortality rates among hysterectomized women aged 50 to 59 years.
Methods. We derived a formula to relate the excess mortality among hysterectomized women aged 50 to 59 years assigned to placebo in the Women’s Health Initiative randomized controlled trial to the entire population of comparable women in the United States, incorporating the decline in estrogen use observed between 2002 and 2011.
Results. Over a 10-year span, starting in 2002, a minimum of 18 601 and as many as 91 610 postmenopausal women died prematurely because of the avoidance of estrogen therapy (ET).
Conclusions. ET in younger postmenopausal women is associated with a decisive reduction in all-cause mortality, but estrogen use in this population is low and continuing to fall. Our data indicate an associated annual mortality toll in the thousands of women aged 50 to 59 years. Informed discussion between these women and their health care providers about the effects of ET is a matter of considerable urgency.
In the 1990s, estrogen therapy (ET) became the standard of treatment of the almost 600 000 women a year in the United States undergoing hysterectomy. Clinical studies had indicated ET was effective for treatment of menopausal symptoms and appeared to be bone protective and cardioprotective. More than 90% of hysterectomized women in their 50s used ET, with a continuance rate averaging 4 to 5 years.1–3
In July 2002, the Women’s Health Initiative (WHI) published the results of the Estrogen Plus Progestin Trial and announced that the study was being terminated ahead of schedule because of adverse effects in the women receiving hormones compared with those receiving placebo.4 The media impact was immediate, widespread, and persistent.5 The study’s treatment drug (Prempro) was often referred to as “HT” (hormone therapy) or “estrogen.” As a consequence, the findings were generalized to all varieties of hormone replacement, including estrogen alone, in women without a uterus although only women with a uterus were randomized in this study. Prescriptions for postmenopausal hormone replacement declined precipitously. Within 18 months, half of the women in the United States using systemic HT stopped treatment.1–3 Included were almost 2 000 000 women who had no uterus who were using ET and not using the study drug.
Subsequently, the findings of the WHI Estrogen-Alone Trial (WHI-ET) for women without a uterus were published for the intervention phase (2004) and the postintervention long-term follow-up phase (2011).6,7 These findings showed mortality benefits for ET compared with placebo. Preliminary subgroup analysis of the intervention phase data (2004) indicated reduced total mortality in the women aged 50 to 59 years. However, it is only in the postintervention data (2011) that an absolute total mortality risk reduction of 13 per 10 000 women per year was reported for these women. The mortality decrease was almost entirely owing to a decrease in coronary heart disease (CHD) although reduced cancer mortality and other cause mortalities were also reported among the women who received ET.7
Despite the positive findings for ET, prescriptions for all forms of systemic HT have continued to decline.3,8–11 Currently, less than one third of hysterectomized women are using ET.12 The decline in ET prescription and usage seems to reflect a generalized avoidance of any forms of HT not supported by the WHI data. This raises the possibility that there has been and continues to be a considerable resultant mortality toll. We therefore undertook an analysis, on the basis of published data, to determine the likely toll of excess, premature death among hysterectomized women aged 50 to 59 years in the United States following the WHI publication in 2002.
METHODS
The 2011 WHI publication indicated a 13 per 10 000 per year higher rate of mortality among hysterectomized women aged 50 to 59 years assigned to placebo than among those assigned to estrogen over a 10-year follow-up.7 We considered this figure a point estimate for the mortality burden associated with foregoing estrogen among members of this specific population.
To determine how this rate of excess mortality translated into an aggregate toll of premature death at the population level, we established the following formula to represent the mortality toll of estrogen avoidance (MTEA):
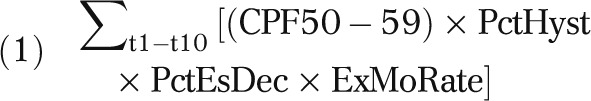 |
where
∑t1–t10 = sum for years 1 through 10 (2002–2011),
CPF50–59 = size of population of women, aged 50 to 59 years, from US Census data (2002–2011),
PctHyst = percentage of women in CPF50–59 who have undergone hysterectomy (specific to year and age),
PctEsDec = absolute percentage decline in rate of estrogen use in group of interest, by year, following publication of WHI results, and
ExMoRate = excess mortality rate in group of interest as a result of estrogen avoidance.
When a single best estimate was available in the peer-reviewed literature or government data for any given entry in the formula for the entire span of 10 years or the entire population of women across the age range, we used that. If more precise estimates specific to year or age were available, we entered these and we then aggregated the calculations across years and age groups. Because of a distinctly differential rate of hysterectomy for women in the lower than the upper half of the age range of interest, we conducted separate calculations for these 2 populations and aggregated the results. To enhance the accuracy of our calculation, we applied the relevant rates to portions of the specified range and generated an estimate for the entire age range by determining the weighted average.
We calculated the mortality toll estimates on the basis of population estimates from census data, age variability for hysterectomy prevalence reported in the peer-reviewed literature, and different rates of ET use before 2002 affected by whether the women had their ovaries removed (oophorectomy). We applied the WHI absolute mortality estimate for women aged 50 to 59 years (13/10 000/year) in all the calculations, along with the extremes of the 95% confidence interval (CI) around this point estimate.
We derived the annual populations of women aged 50 to 59 years from 2002 to 2011 US Census estimates.13,14 We derived the hysterectomy prevalence rates, with and without oophorectomy, from 1997 to 2005 National Hospital Discharge Survey data.15,16 For women aged 50 to 59 years the rates ranged from 33% to 40%. The rates are consistent with an average of almost 600 000 hysterectomies per year among women of all ages in the United States. The average age for hysterectomy is 46.1 years.15,16
An estimated 54% of women have their ovaries removed at the time of hysterectomy.16 Before 2002, the ET use rate for women posthysterectomy without ovaries was 90% and with ovaries was 53%.17 Therefore, we calculated the mortality associated with a decline in ET use separately for women with and those without ovaries.
Compared with 2001, use of oral estrogen only in women aged 50 to 59 years declined almost 60% by 2004, reached a 71% relative decline by 2006, and remained at that level through 2009.3 Since then there has been further decline in ET use, with 2010 and 2011 showing a 79% decline for these particular women.10,11 We used these figures to generate a year-by-year absolute percentage decline in the use of estrogen beginning with a baseline rate in 2002.
We entered best estimates for each component of the formula to generate a single aggregate estimate for the total excess in premature mortality attributable to estrogen avoidance in the population of interest. We made a particular effort to choose well-validated and conservative entries.
We identified the range of reasonable estimates around the best point estimate when possible for purposes of sensitivity analysis, that is, determining the sensitivity of the calculated estimate to variation in a given entry. For each entry in the MTEA formula, we attempted to identify well-validated figures representing reasonable low- and high-end values.
We calculated the 95% CI around the excess death rate as a result of estrogen aversion using the sample size from the WHI study to generate high- and low-end estimates for the excess mortality in the placebo group relative to the estrogen group.
The range of values we produced in the sensitivity analysis is reflected in the data tables, which indicate how we altered our assumptions, which led to specific estimates of MTEA. There were ranges of relevant values for the rate of hysterectomy, the rate of estrogen use, and the exact mortality excess as derived from the WHI-ET study. Our sensitivity analysis involved entering values at the extremes of the range for each of these parameters and calculating an MTEA estimate accordingly. We analyzed the data using SAS, version 9.1 (SAS Institute, Cary, NC).
RESULTS
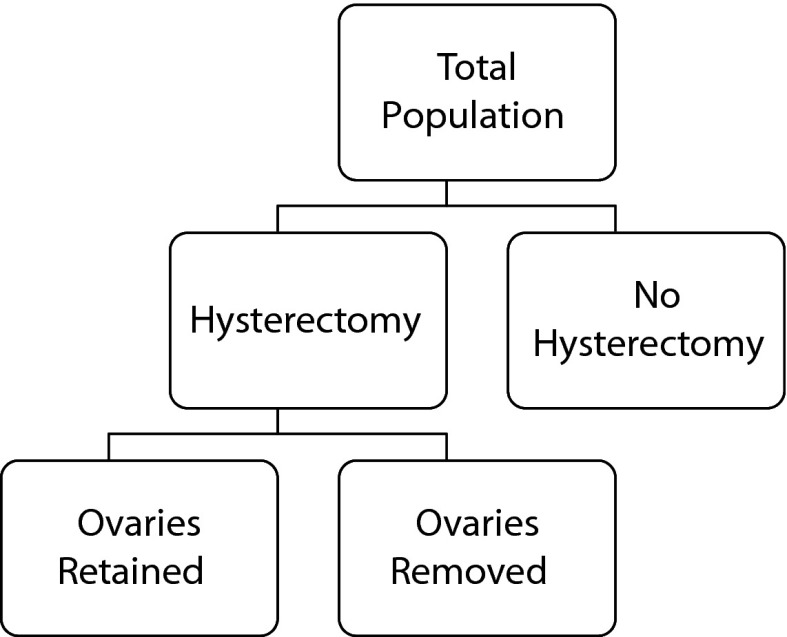
Table 1 displays the estimated mortality toll of estrogen avoidance among all women aged 50 to 59 years assuming the rate of estrogen use at baseline and decline in estrogen use over time were common to women both with and without oophorectomy at the time of hysterectomy (Figure 1). Applying the lower estimate for hysterectomy rate in the population,16 the best point estimate for excess mortality over 10 years is 49 128 excess deaths, and the extreme low estimate is 22 677 excess deaths. Applying a higher estimated rate of hysterectomy in the population,16 the best point estimate for excess mortality over 10 years is 59 549 excess deaths, and the extreme high estimate is 91 610.
TABLE 1—
Mortality Estimates for All Women Aged 50–59 Years Using 2 Different Rates of Hysterectomy: United States, 2002–2011
| Hysterectomy Rate,12 % | Population Size10 | Decline in Estrogen Use,4 % | Excess Mortality Estimate, No. (95% CI) |
| 33 | |||
| 2002 | 17 307 862 | 28 | 2115 (976, 3254) |
| 2003 | 17 801 925 | 45 | 3399 (1569, 5229) |
| 2004 | 18 413 377 | 53 | 4219 (1947, 6490) |
| 2005 | 19 094 469 | 58 | 4739 (2188, 7291) |
| 2006 | 19 769 666 | 58 | 4907 (2265, 7549) |
| 2007 | 20 071 964 | 63 | 5442 (2512, 8372) |
| 2008 | 20 472 322 | 63 | 5550 (2562, 8539) |
| 2009 | 20 853 904 | 63 | 5654 (2610, 8698) |
| 2010 | 21 506 008 | 70 | 6487 (2994, 9980) |
| 2011 | 21 933 149 | 70 | 6616 (3054, 10 179) |
| Cumulative total | 49 128 (22 677, 75 580) | ||
| 40 | |||
| 2002 | 17 307 862 | 28 | 2564 (1184, 3944) |
| 2003 | 17 801 925 | 45 | 4120 (1902, 6338) |
| 2004 | 18 413 377 | 53 | 5114 (2360, 7867) |
| 2005 | 19 094 469 | 58 | 5744 (2652, 8837) |
| 2006 | 19 769 666 | 58 | 5948 (2745, 9150) |
| 2007 | 20 071 964 | 63 | 6596 (3045, 10 147) |
| 2008 | 20 472 322 | 63 | 6727 (3105, 10 350) |
| 2009 | 20 853 904 | 63 | 6853 (3163, 10 543) |
| 2010 | 21 506 008 | 70 | 7863 (3163, 12 097) |
| 2011 | 21 933 149 | 70 | 8020 (3630, 12 337 |
| Cumulative total | 59 549 (27 488, 91 610) |
Note. CI = confidence interval. 95% CIs are derived from the 95% CI around the excess death rate. The excess death6 rate is 0.0013.
FIGURE 1—
Mortality toll of estrogen avoidance estimates flowchart.
Tables 2 and 3 show the differential mortality toll of estrogen avoidance for women with retained ovaries and ovaries removed, respectively. Estimates for the entire population thus require summing the totals from Tables 2 and 3 under similar assumptions. Applying the lower estimate for hysterectomy rate3 to both populations, the best point estimate for total excess mortality is 13 462 + 26 830, or 40 292. The low-end estimate is 6216 + 12 385, or 18 601 excess deaths. Applying the higher estimate for hysterectomy rate3 to both populations, the best point estimate for excess mortality is 16 316 + 32 519, or 48 835. The high-end point estimate is 25 098 + 50 027, or 75 125.
TABLE 2—
Mortality Estimates of Hysterectomized Women Aged 50–59 Years With Retained Ovaries Using 2 Different Rates of Hysterectomy: United States, 2002–2011
| Hysterectomy and Ovaries Retained, %12 | Population Size10 | Decline in Estrogen Use, %4 | Excess Mortality Estimate, No. (95% CI) |
| 15.18 | |||
| 2002 | 17 307 862 | 17 | 580 (268, 892) |
| 2003 | 17 801 925 | 27 | 931 (430, 1433) |
| 2004 | 18 413 377 | 32 | 1156 (534, 1778) |
| 2005 | 19 094 469 | 34 | 1299 (600, 1998) |
| 2006 | 19 769 666 | 34 | 1345 (621, 2068) |
| 2007 | 20 071 964 | 38 | 1491 (688, 2294) |
| 2008 | 20 472 322 | 38 | 1521 (702, 2339) |
| 2009 | 20 853 904 | 38 | 1549 (715, 2383) |
| 2010 | 21 506 008 | 42 | 1777 (821, 2734) |
| 2011 | 21 933 149 | 42 | 1813 (837, 2789) |
| Cumulative total | 13 462 (6216, 20 708) | ||
| 18.4 | |||
| 2002 | 17 307 862 | 17 | 703 (325, 1081) |
| 2003 | 17 801 925 | 27 | 1129 (521, 1737) |
| 2004 | 18 413 377 | 32 | 1401 (647, 2155) |
| 2005 | 19 094 469 | 34 | 1574 (727, 2421) |
| 2006 | 19 769 666 | 34 | 1630 (752, 2507) |
| 2007 | 20 071 964 | 38 | 1807 (834, 2780) |
| 2008 | 20 472 322 | 38 | 1843 (851, 2835) |
| 2009 | 20 853 904 | 38 | 1878 (867, 2888) |
| 2010 | 21 506 008 | 42 | 1878 (995, 3314) |
| 2011 | 21 933 149 | 42 | 2197 (1014, 3380) |
| Cumulative total | 16 316 (7533, 25 098) |
Note. CI = confidence interval. 95% CIs are derived from the 95% CI around the excess death rate. The excess death6 rate is 0.0013.
TABLE 3—
Mortality Estimates of Hysterectomized Women Aged 50–59 Years With Ovaries Removed Using 2 Different Rates of Hysterectomy: United States, 2002–2011
| Hysterectomy Ovaries Removed, %12 | Population Size10 | Decline in Estrogen Use, %4 | Excess Mortality Estimate, No. (95% CI) |
| 17.82 | |||
| 2002 | 17 307 862 | 29 | 1155 (533, 1777) |
| 2003 | 17 801 925 | 45 | 1856 (857, 2851) |
| 2004 | 18 413 377 | 54 | 2304 (1064, 3544) |
| 2005 | 19 094 469 | 59 | 2588 (1195, 3982) |
| 2006 | 19 769 666 | 59 | 2680 (1237, 4122) |
| 2007 | 20 071 964 | 64 | 2972 (1372, 4572) |
| 2008 | 20 472 322 | 64 | 3031 (1399, 4663) |
| 2009 | 20 853 904 | 64 | 3088 (1425, 4750) |
| 2010 | 21 506 008 | 71 | 3543 (1635, 5450) |
| 2011 | 21 933 149 | 71 | 3613 (1668, 5558) |
| Cumulative total | 26 830 (12 385, 41 274) | ||
| 21.6 | |||
| 2002 | 17 307 862 | 29 | 1400 (647, 2154) |
| 2003 | 17 801 925 | 45 | 2250 (1039, 3461) |
| 2004 | 18 413 377 | 54 | 2793 (1289, 4296) |
| 2005 | 19 094 469 | 59 | 3137 (1448, 4826) |
| 2006 | 19 769 666 | 59 | 3248 (1499, 4997) |
| 2007 | 20 071 964 | 64 | 3602 (1663, 5541) |
| 2008 | 20 472 322 | 64 | 3674 (1696, 5652) |
| 2009 | 20 853 904 | 64 | 3742 (1727, 5757) |
| 2010 | 21 506 008 | 71 | 4294 (1982, 6606) |
| 2011 | 21 933 149 | 71 | 4379 (2022, 6737) |
| Cumulative total | 32 519 (15 012, 50 027) |
Note. CI = confidence interval. 95% CIs are derived from the 95% CI around the excess death rate. The excess death6 rate is 0.0013.
Thus, across a reasonable range of all assumptions, the excess mortality was between 18 601 and 91 610. Using the best available point estimate values with year-by-year adjustment and adjustment for differential rates of estrogen use among women with and without retained ovaries at hysterectomy, the range was 40 292 to 48 835.
DISCUSSION
Our analysis suggests that between 2002 and 2011 a minimum of 18 601 and as many as 91 610 excess deaths occurred among hysterectomized women aged 50 to 59 years following the publication of the original WHI findings because of the resulting aversion to hormone replacement therapy of all kinds that ensued among doctors and patients alike. The actual toll of excess mortality is likely to be between 40 292 and 48 835.
These numbers translate the WHI statistic for excess mortality in hysterectomized women aged 50 to 59 years who received placebo versus estrogen into an actual number of deaths. We believe that a mortality toll will better communicate the meaning and significance of the WHI-ET findings to women, health care providers (HCPs), and the media. The reported reduction in mortality for women aged 50 to 59 years in the WHI-ET reports was exactly the same (HR = 0.73) in 2004 and 2011.6,7 Neither the 2004 nor the 2011 WHI-ET reports reversed the decline in use of ET. The 2011 report of the 10.7 years of follow-up of ET-treated women, which included the absolute risk reduction in mortality rate of 13 per 10 000 per year in the hysterectomized women aged 50 to 59 years, was barely noticed. Decline in ET use has continued since its publication. Currently, it appears that only about one third of women having a hysterectomy with removal of their ovaries, regardless of age, are using ET.12 Before 2002, 90% of these women used systemic hormone replacement.17,18
Estrogen Therapy and Mortality
ET reduces total mortality primarily through reducing CHD-related deaths. Since 1959 there have been many reports showing increased risk of CHD mortality after early surgical menopause and especially after oophorectomy.19–21 Essentially, estradiol inhibits the development of atherosclerosis and helps maintain normal arterial blood flow.22,23
A 1998 meta-analysis of 25 observational studies reported a 30% lower risk of CHD in ET users.24 The California Teachers Study, in which 97% of the oophorectomized women used HT (almost entirely ET), shows an all-cause mortality reduction similar to the WHI-ET results.25
The WHI-ET and the California Teachers Study results indicate that the decrease in CHD events and all-cause mortality are limited to hysterectomized women younger than 60 years or within 10 years of menopause. A meta-analysis of 23 trials found that HT significantly reduced CHD events in these women.26 In fact, for CHD, the WHI-ET findings among women aged 50 to 59 years are in line with the reduced risks reported in the observational studies and support a “timing hypothesis” for ET cardioprotection when ET is started close to the time of menopause.27,28 The current thinking is that by age 60 years, pathological changes in vascular endothelial cells compromise the ability of estrogen to inhibit atherosclerosis and promote blood flow.27,28
Although prevention of cardiovascular mortality is by far the major benefit from ET in younger women, the WHI-ET and the California Teachers Study also show a reduction in cancer deaths. In 2012, the WHI-ET investigators reported a 63% reduction in mortality because of invasive breast cancer in the almost 12 years of follow-up in the postintervention study of ET users versus placebo users.29
Lack of Impact of the WHI–Estrogen-Alone Trial Findings
Continuing decline in ET prescriptions through 2011 attests to the WHI-ET data’s lack of impact.3,10,11 Numerous reasons for this can be suggested. Knowing the history of HT in the United States helps in understanding why there has been a strong reaction against the use of ET. In the 1960s, enthusiasm about using estrogen for menopause symptoms led to widespread use. In 1975 it was reported that unopposed estrogen in women with a uterus increased the risk of endometrial cancer. These findings led to fear of using estrogen. However, in the 1970s and 1980s, research on the addition of a progestin to ET showed that endometrial hyperplasia and carcinoma could be all but eliminated. At the same time, other research indicated that estrogen had bone-protective and cardioprotective effects. Confidence was restored, and once again there was widespread use of HT.
When the first WHI report came out in 2002 its findings about the health risks of postmenopausal HT were startling and frightening.5 Almost no one emphasized or even seemed to recognize the fact that the worst findings might not apply to hormones other than Prempro or might not apply to all age groups. Deciding not to use HT appeared to be the most appropriate and rational choice for almost all women. Aversion to all forms of HT became almost automatic, and the idea that there might actually be positive health outcomes of ET use was often dismissed.
There are other influences on women’s decisions about ET that are important but are beyond the scope of this study. These include HCPs paying little attention to WHI-ET reports; failure to differentiate between the findings of the 2 different WHI studies; mistrust of pharmaceutical companies and their products; peer group pressure to avoid estrogen; nonhormonal alternative therapies for hot flashes, prevention of osteoporosis, and sleep disturbance; the use of bioidentical hormones not approved by the US Food and Drug Administration; and pendulum swings in medical recommendations, which have created general skepticism about medical treatments.
Presenting Complex Biomedical Findings to the Public
Research findings are often nuanced and need to be reported accordingly in both the peer-reviewed literature and the popular press.30 It is the responsibility of biomedical researchers to report findings in a way that the media and the general public can clearly understand. With most medical interventions, as with hormone replacement, the findings and implications are not merely about what is done. They are also informed by how the intervention is delivered, exactly what preparation is used, under what particular circumstances, and in just what population. When findings pertain to specific preparations or populations, this should be stated explicitly and emphatically. Special effort should be made to explain the study nuances to HCPs. It is also the responsibility of the media and HCPs to convey this information so that it is clearly understood. Distortion of details can prove to be nothing less than lethal.
The WHI findings need to be presented so that the very important differences between the 2 treatment modalities are emphasized and the benefits for hysterectomized women aged 50 to 59 years are appreciated. This effort has clearly been inadequate to date.5,31
Limitations
The growing practice of performing hysterectomy outside hospitals using a laparoscopic transvaginal approach has decreased the number of hospital-based procedures. The prevalence estimate, therefore, may be less than the actual number of hysterectomized women aged 50 to 59 years.15 If so, our mortality estimates are all biased downward.
We used the decline in use of oral ET for our estimates. We did not include data for use of transdermal estradiol, nonsystemic estrogens, and bioidentical preparations, although millions of postmenopausal women currently use 1 or more of these preparations.
We did not include transdermal ET use in the WHI studies. The use of transdermal estradiol in the United States has declined since 2002. Transdermal estradiol has been reported to be more effective than are oral estrogens in preventing cardiovascular events, so decline in its use could contribute further to the mortality toll.
Vaginal estrogen use did show a substantial increase between 2001 and 2009.3 The effects of vaginal estrogen are thought to be local and nonsystemic. However, a recent report shows an unexpected finding of a reduced rate for myocardial infarction in women using vaginal estrogen. Whether vaginal estrogen has an effect on mortality needs further study.
There has also been an increase in the use of bioidentical hormone preparations since 2002, but we are not aware of mortality data for these compounds.
The WHI cohort of hysterectomized women aged 60 to 69 years showed no significant mortality difference between estrogen use versus placebo. For this reason, we did not do a calculation for this age group. For women aged 70 to 79 years in the WHI study, there is an increased absolute death rate of 19 per 10 000,7 and this age group has shown a 78% decrease use in ET since 2002.3 As a result, some reduction in mortality could be calculated because of not using estrogen. However, compared with the younger women, the overall population in this age group is much smaller and the percentage of hysterectomized women living into their 70s is less. Also, the use of ET before 2002 was much lower in these women.2
We did not include women younger than 50 years, as there were no comparable WHI data for this age group. Nevertheless, hysterectomy occurs most often before aged 50 years (the average age is 46.1 years).16 Mortality is increased in younger women who have a hysterectomy and oophorectomy who do not use ET. Therefore, it is likely that nonuse of ET in women younger than aged 50 years has an additional mortality toll. For example, in the California Teachers Study, women aged 36 to 59 years show a 46% reduction in mortality among current ET users.18 This exclusion biases our estimates downward.
We do not address the issue of estrogen plus progestogen therapy for women with a uterus except to recognize that the treatment is different from ET as are the mortality results.
Conclusions
Decline in use of ET since 2002 has resulted in a significant increase in mortality for hysterectomized women aged 50 to 59 years. Avoidance of all forms of HT is persistent despite the positive findings for treatment with estrogen alone. Women, HCPs, and the media should be offered clear and accurate information about the positive effects of estrogen-alone therapy in these women.
Our analysis suggests that failure to differentiate among populations of women and preparations of HT has cost thousands of lives.
Acknowledgments
The Centers for Disease Control and Prevention funded this article (grant 5U48DP001945). P. M. Sarrel has served as a Medical Consultant for Noven Therapeutics.
Human Participant Protection
Human participants were not involved in the preparation of this article; therefore, it is exempt from review.
References
- 1.Hersh AL, Stefanick ML, Stafford RS. National use of postmenopausal hormone therapy: annual trends and response to recent evidence. JAMA. 2004;291(1):47–53. doi: 10.1001/jama.291.1.47. [DOI] [PubMed] [Google Scholar]
- 2.Wysowski DK, Governale LA. Use of menopausal hormones in the United States, 1992 through June, 2003. Pharmacoepidemiol Drug Saf. 2005;14(3):171–176. doi: 10.1002/pds.985. [DOI] [PubMed] [Google Scholar]
- 3.Tsai SA, Stefanick ML, Stafford RS. Trends in menopausal hormone therapy use of US office-based physicians, 2000–2009. Menopause. 2011;18(4):385–392. doi: 10.1097/gme.0b013e3181f43404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rossouw JE, Anderson GL, Prentice RL et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 5.Brown S. Shock, terror and controversy: how the media reacted to the Women’s Health Initiative. Climacteric. 2012;15(3):275–280. doi: 10.3109/13697137.2012.660048. [DOI] [PubMed] [Google Scholar]
- 6.Anderson GL, Limacher M, Assaf AR et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 7.LaCroix AZ, Chlebowski RT, Manson JE et al. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy: a randomized controlled trial. JAMA. 2011;305(13):1305–1314. doi: 10.1001/jama.2011.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silverman BG, Kokia ES. Use of hormone replacement therapy, 1998–2007: sustained impact of the Women’s Health Initiative findings. Ann Pharmacother. 2009;43(2):251–258. doi: 10.1345/aph.1L438. [DOI] [PubMed] [Google Scholar]
- 9.Taylor HS, Manson JE. Update in hormone therapy use in menopause. J Clin Endocrinol Metab. 2011;96(2):255–264. doi: 10.1210/jc.2010-0536. [DOI] [PubMed] [Google Scholar]
- 10.Steinkellner AR, Denison SE, Eldridge SL, Lenzi LL, Chen W, Bowlin SJ. A decade of postmenopausal hormone therapy prescribing in the United States: long-term effects of the Women’s Health Initiative. Menopause. 2012;19(6):616–621. doi: 10.1097/gme.0b013e31824bb039. [DOI] [PubMed] [Google Scholar]
- 11.Sprague BL, Trentham-Dietz A, Cronin KA. A sustained decline in postmenopausal hormone use: results from the National Health and Nutrition Examination Survey, 1999–2010. Obstet Gynecol. 2012;120(3):595–603. doi: 10.1097/AOG.0b013e318265df42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chubaty A, Shandro MT, Schuurmans N, Yuksel N. Practice patterns with hormone therapy after surgical menopause. Maturitas. 2011;69(1):69–73. doi: 10.1016/j.maturitas.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Profile of general population and housing characteristics. US Census Bureau. 2010. Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_DP_DPDP1&prodType=table. Accessed June 12, 2012.
- 14.National characteristics: vintage 2009. US Census Bureau. Available at: http://www.census.gov/popest/data/national/asrh/2009/index.html. Accessed June 8, 2012.
- 15.Merrill RM. Hysterectomy surveillance in the United States, 1997 through 2005. Med Sci Monit. 2008;14(1):CR24–CR31. [PubMed] [Google Scholar]
- 16.Whiteman MK, Hillis SD, Jamieson DJ et al. Inpatient hysterectomy surveillance in the United States, 2000–2004. Am J Obstet Gynecol. 2008;198(1):34. doi: 10.1016/j.ajog.2007.05.039. e1–34.e7. [DOI] [PubMed] [Google Scholar]
- 17.Gallicchio L, Whiteman MK, Tomic D, Miller KP, Langenberg P, Flaws JA. Type of menopause, patterns of hormone therapy use, and hot flashes. Fertil Steril. 2006;85(5):1432–1440. doi: 10.1016/j.fertnstert.2005.10.033. [DOI] [PubMed] [Google Scholar]
- 18.Stram DO, Liu Y, Henderson KD et al. Age-specific effects of hormone therapy use on overall mortality and ischemic heart disease mortality among women in the California Teachers Study. Menopause. 2011;18(3):253–261. doi: 10.1097/gme.0b013e3181f0839a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robinson RW, Higano N, Cohen WD. Increased incidence of coronary heart disease in women castrated prior to the menopause. Arch Intern Med. 1959;104:908–913. doi: 10.1001/archinte.1959.00270120064010. [DOI] [PubMed] [Google Scholar]
- 20.Rocca WA, Grossardt BR, de Andrade M, Malkasian GD, Melton LJ., 3rd Survival patterns after oophorectomy in premenopausal women: a population-based cohort study. Lancet Oncol. 2006;7(10):821–828. doi: 10.1016/S1470-2045(06)70869-5. [DOI] [PubMed] [Google Scholar]
- 21.Parker WH, Broder MS, Chang E et al. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses’ health study. Obstet Gynecol. 2009;113(5):1027–1037. doi: 10.1097/AOG.0b013e3181a11c64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gerhard M, Ganz P. How do we explain the clinical benefits of estrogen? From bedside to bench. Circulation. 1995;92(1):5–8. doi: 10.1161/01.cir.92.1.5. [DOI] [PubMed] [Google Scholar]
- 23.Mendelsohn ME, Karas RH. The protective effects of estrogen on the cardiovascular system. N Engl J Med. 1999;340(23):1801–1811. doi: 10.1056/NEJM199906103402306. [DOI] [PubMed] [Google Scholar]
- 24.Barrett-Connor E, Grady D. Hormone replacement therapy, heart disease, and other considerations. Annu Rev Public Health. 1998;19:55–72. doi: 10.1146/annurev.publhealth.19.1.55. [DOI] [PubMed] [Google Scholar]
- 25.Duan L, Xu X, Koebnick C et al. Bilateral oophorectomy is not associated with increased mortality: the California Teachers Study. Fertil Steril. 2012;97(1):111–117. doi: 10.1016/j.fertnstert.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salpeter SR, Walsh JM, Greyber E, Salpeter EE. Brief report: coronary heart disease events associated with hormone therapy in younger and older women. A meta-analysis. J Gen Intern Med. 2006;21(4):363–366. doi: 10.1111/j.1525-1497.2006.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pal L, Manson JE. The Women’s Health Initiative: an unforgettable decade. Menopause. 2012;19(6):597–599. doi: 10.1097/gme.0b013e31825397f0. [DOI] [PubMed] [Google Scholar]
- 28.Allison MA, Manson JE. Age, hormone therapy use, coronary heart disease, and mortality. Menopause. 2011;18(3):243–245. doi: 10.1097/gme.0b013e3182099c5b. [DOI] [PubMed] [Google Scholar]
- 29.Anderson GL, Chlebowski RT, Aragaki AK et al. Conjugated equine oestrogen and breast cancer incidence and mortality in postmenopausal women with hysterectomy: extended follow-up of the Women’s Health Initiative randomised placebo-controlled trial. Lancet Oncol. 2012;13(5):476–486. doi: 10.1016/S1470-2045(12)70075-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katz DL. Medicine and media: state of the union? Am J Prev Med. 2008;34(1):83–84. doi: 10.1016/j.amepre.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 31.Burger HG, MacLennan AH, Huang KE, Castelo-Branco C. Evidence-based assessment of the impact of the WHI on women’s health. Climacteric. 2012;15(3):281–287. doi: 10.3109/13697137.2012.655564. [DOI] [PubMed] [Google Scholar]