Abstract
Research evidence indicates that 2 forms of racial discrimination—perceived interpersonal discrimination and racial/ethnic residential segregation (a form of institutional discrimination)—may influence children’s health and disparities.
Although research on these 2 forms of discrimination and health has primarily focused on adults, smaller bodies of work have documented that perceived interpersonal discrimination and segregation have a negative effect on infants’ health, and that perceived interpersonal discrimination may negatively affect children’s mental health.
Three directions for research are (1) incorporating a life-course perspective into studies of discrimination and children’s health, (2) linking residential segregation with geography-of-opportunity conceptual frameworks and measures, and (3) considering residential segregation along with segregation in other contexts that influence children’s health (e.g., schools).
Racial/ethnic disparities in the health and development of US children are large and persistent over time.1,2 Because of demographic trends, such disparities affect a growing number of children. In 2011, 47% of children were racial/ethnic minorities, up from 26% in 1980 (authors’ calculations, US Census Bureau estimates3,4). These trends suggest that the health of minority children will have an increasing impact on population health over time.
The changing racial/ethnic composition of the US children’s population is occurring in the context of high levels of residential and school segregation, affecting a large proportion of Black and Latino children. In 2010, 81.6% of Black children residing in large metropolitan areas lived in areas with high Black–White residential segregation, and 77.8% lived in areas with high levels of school segregation; the respective percentages for Latino children were 32.6% and 54.2% (Table 1). In addition, national surveys indicate that large proportions of minority children report being discriminated against; 90% of Black adolescents have reported discrimination.7
TABLE 1—
Share of Racial/Ethnic Minority Children and Public Primary School Students in Metropolitan Areas With Segregation (Dissimilarity Indices) in Specified Ranges: 100 Largest US Metropolitan Areas, 2010
| Share of Children at Each Level of Residential Segregation |
Share of Primary School Students at Each Level of School Segregation |
|||||
| Segregation Level | Black | Latino | Asian | Black | Latino | Asian |
| Higha | 81.6 | 32.6 | 0.0 | 77.8 | 54.2 | 0.1 |
| Mediumb | 18.3 | 67.2 | 99.0 | 21.8 | 45.8 | 96.4 |
| Lowc | 0.0 | 0.2 | 1.0 | 0.5 | 0.1 | 3.5 |
| Average leveld | 67.6 | 54.7 | 49.4 | 67.1 | 60.0 | 47.5 |
Note. Dissimilarity indices reflect the share of specified minority children or students who would have to move to another census tract or school for each census tract or school to have the same share of specified minority and White children or students as the metropolitan area as a whole. A value of 0 would indicate complete desegregation, and a value of 100 would indicate complete segregation. Percentages may not sum to 100 because of rounding. Asians include Pacific Islanders; Latinos may be of any race. School data reflect 2009–2010 school year.
High segregation refers to levels ≥ 60.
Medium segregation refers to levels of 30–59.
Low segregation refers to levels < 30.
Average segregation level is weighted by the number of children or students of the specified race/ethnicity in each metropolitan area.
Source. diversitydata.org calculations from 2010 Census Redistricting File5 for residential segregation and from National Center for Education Statistics, Common Core of Data 2009–20106 for school segregation.
This backdrop and the fact that racial disparities in children’s health persist after accounting for socioeconomic status has led researchers to investigate the role that other factors, such as racial discrimination, may contribute to health disparities. Racial discrimination is defined by the National Research Council as (1) differential treatment on the basis of race that disadvantages a racial group, and (2) differential effect or treatment on the basis of factors other than race that disadvantages a racial group.8 The health literature has offered several definitions of discrimination, which underscore that discrimination occurs at multiple levels: interpersonal (manifested in interpersonal encounters) and institutional (manifested in institutional practices or policies that reproduce racial stratification).9–11 Definitions of interpersonal discrimination in the health literature often focus on the perception of discrimination. By contrast, definitions used in other fields do not require awareness (or perception) on the part of the victim, nor discriminatory intent on the part of the perpetrator.8,12 Indeed, discrimination may occur in the absence of prejudice (implicit bias), and, even if not perceived by the victim, it may have detrimental effects.8,13
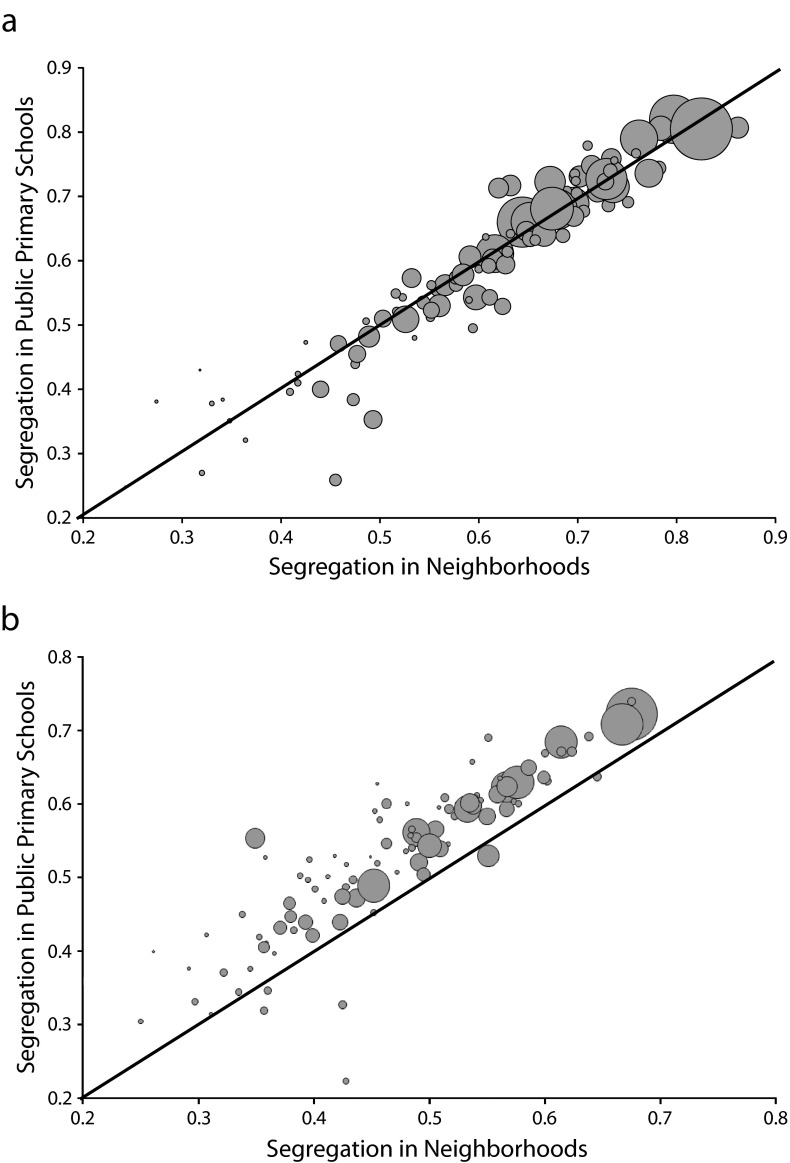
Discrimination can be conceptualized as a risk factor that has the potential to negatively affect a child’s developmental or health trajectory.14 As shown in Figure 1, discrimination may have negative effects on 4 different dimensions of a child’s health: stress (physiological responses), cognitive and socioemotional development, health behaviors, and ethnic identity development. The Institute of Medicine’s definition of child health emphasizes a life-course perspective—that is, the ability of children to develop their (health, developmental, academic) potential at, and through, each life stage.15–18 Ethnic identity may also be conceptualized as a health domain because it undergoes a developmental process during childhood, is in itself a developmental outcome, and may mediate or modify the effects of discrimination on mental health.19
FIGURE 1—
Influences of interpersonal and institutional discrimination on children’s health.
The pathways through which discrimination affects the child may vary depending on whether discrimination is perceived by the child (or caregivers), and on the level at which discrimination occurs (interpersonal or institutional). Discrimination may affect the child directly; for instance, perceived discrimination during an interpersonal interaction may generate a physiological stress response in the child. But discrimination may also have detrimental effects even if the child does not perceive it. For example, discrimination perceived by the parent or caregiver may lead to parental depression, which may negatively affect parent–child interactions and subsequently the child’s mental health. Discrimination may also lead to adaptive responses. For example, parents may socialize their children to recognize and resist racial discrimination; this socialization may have a protective effect on children.20,21
The effects of discrimination may play out across the life course and the effects may be amplified if experienced during critical developmental periods—that is, discrimination during childhood may have contemporary or delayed effects, including effects that reverberate across the life course.22
The research evidence in the literature has largely focused on 2 types of discrimination: perceived interpersonal discrimination and racial/ethnic residential segregation, a form of institutional discrimination. We note gaps in the literature in relation to the framework discussed previously. We suggest 3 directions for future research aligned with our framework: (1) developing further a life-course perspective in studies of discrimination and children’s health, (2) linking residential segregation with geography-of-opportunity conceptual frameworks and measures to improve our understanding of how segregation influences a child’s exposure to contextual risk or protective factors, and (3) considering residential segregation along with segregation in other contexts (e.g., schools) to improve our understanding of how cumulative or multiple levels of disadvantage may influence children’s health.
LITERATURE REVIEW
We searched for relevant articles by using MEDLINE and the following parameters: English-language articles focusing on children (aged 0–18 years) or older adolescents and young adults (aged 19–24 years), published after January 1, 2000. We used the following search items (in the title or abstract): “racial discrimination,” “racism,” and “residential segregation.” We focused on articles that treated discrimination as an exposure and examined effects on children’s health outcomes, excluding nonhealth developmental outcomes (e.g., cognitive development). The objective of the literature review was to guide this analytic essay by identifying definitions of discrimination, hypothesized pathways between discrimination and children’s health, and recent findings in the literature. Table 2 summarizes the findings of our segregation literature review. For perceived discrimination, we reviewed various empirical studies, but relied primarily on 4 recent reviews of the literature.31–34
TABLE 2—
Segregation and Child Health Studies Reviewed
| Citation | Geographic Area(s) Studied | Sample Information | Institutional Discrimination (Segregation) Measure(s) | Outcomes | Findings (P ≤ .05) |
| Kramer et al.23 | 231 MSAs with population ≥ 100 000 and ≥ 5000 non-Hispanic Black residents | Non-Hispanic White and Non-Hispanic Black women giving birth to singleton in 2000–2002 | Spatial adaptation of isolation indexSpatial adaptation of dissimilarity index (clustering) | Very PTB (< 32 wk)Moderately PTB (32–36 wk) | General: segregation is associated with increased risk of PTB in Black women, but independently accounts for only a small portion (8%) of the Black–White PTB disparityFindings for Black women:Increased isolation associated with increased odds of very PTB and moderately PTBIncreased clustering associated with increased odds of very PTB and moderately PTBWhen isolation and clustering are measured simultaneously, the isolation–very PTB association strengthens, and clustering becomes moderately protectiveConditional on clustering, the isolation–moderate PTB association is roughly half as strong as the isolation–very PTB associationFindings for White women: no association between segregation (isolation or clustering) and very PTB or moderately PTB |
| Osypuk et al.24 | 168 MSAs with population ≥ 100 000 and ≥ 5000 Mexican-origin residents | Hispanic/Latina women aged 15–45 y of Mexican origin giving birth to singleton in 2000 | Exposure indices | Birth weight (g or lb at birth) | For US-born women of Mexican origin:Living in MSAs with highest exposure to ethnic enclaves associated with lower birth weightsNo statistically significant association between exposure to immigrant enclaves and birth weightLiving in MSAs with highest exposure to neighborhood poverty associated with lower birth weightExposure to immigrant enclaves positively associated with birth weight after adjustment for the detrimental effect of exposure to ethnic enclaves (although detrimental effect of ethnic enclaves outweighed positive effects of immigrant enclave by magnitude of approximately 2)For Mexican immigrant women: |
| No significant association between ethnic enclave exposure or immigrant enclave exposure and birth weight | |||||
| No association between exposure to neighborhood poverty and birth weight | |||||
| Walton25 | MAs with population≥ 100 000 and ≥ 5000 of specified race/ethnicity groups144 MAs for Asian Americans208 MAs for Latino Americans 228 MAs for African Americans | Non-Hispanic Black, non-Hispanic Asian, and Hispanic women giving birth to singleton in 2000 | Isolation indexSpatial proximity or clustering | LBW | For Asian American women:Increased isolation lowers odds of having a LBW babyIncreased clustering lowers odds of having a LBW babyFor African American and Hispanic women: no statistically significant relationship between isolation or clustering on LBW found for either group |
| Hearst et al.26 | 64 cities with population > 250 000 residents (29 segregated, 35 nonsegregated) | Black infants born in 2000–2002 | Isolation index (dichotomized at 0.60) | Infant mortality rate (all-cause infant mortality, postneonatal mortality, and external causes of death) | No independent effect of segregation on Black infant mortality (after matching on propensity scores) |
| Kramer and Hogue27 | 168 MSAs with population ≥ 100 000 residents and ≥ 1000 race-specific births | Non-Hispanic White, non-Hispanic Black, and Hispanic women giving birth to singleton in 2002–2004 | Unevenness (Theil’s entropy index) Isolation index | Very PTB (< 32 wk gestation) | Subanalysis for Black women showed higher isolation associated with higher very PTB rates whereas higher unevenness associated with lower very PTB rates |
| Osypuk and Acevedo-Garcia28 | 237 MAs with population ≥ 100 000 and ≥ 5000 Black residents | US-born non-Hispanic Black and non-Hispanic White women aged 15–45 y giving birth to singleton in 2000 | Hypersegregation (simultaneous high residential racial segregation across 4-5 dimensions of segregation) | PTB | Probability of PTB higher for Blacks born in hypersegregated MAsBlack–White disparities in PTB rates larger in hypersegregated MAsAssociation between PTB and maternal age more pronounced for older Black women living in hypersegregated MAs and Black–White disparities greater among older women in hypersegregated MAs |
| Bell et al.29 | 216 large MSAs with population ≥ 100 000 and ≥ 5000 Black residents | US-born, non-Hispanic African American women giving birth to singleton in 2002 | Isolation indexClustering (spatial proximity) indexCombined isolation–clustering (spatial proximity) indexMSAs grouped into low, medium, and high segregation | Self-reported cigarette smoking during pregnancy (yes or no) | Pregnant women who lived in areas of low and high segregation were more likely to smoke than those who lived in areas of moderate segregationNo statistically significant association between isolation (alone) and smokingPositive association between low clustering and high clustering and smoking during pregnancy (U-shaped association)Positive association between low and high levels of segregation (measured by combined isolation–clustering index) and smoking during pregnancy (U-shaped association) |
| Bell et al.30 | 225 large MSAs with population ≥ 100 000 and ≥ 5000 Black residents | US-born, non-Hispanic African American women giving birth to singleton in 2002 | Isolation index Clustering (spatial proximity) index MSAs grouped into very low, low, medium, and high segregation | Birth weight (continuous in grams) PTB Fetal growth restriction (birth weight < 10th percentile for gestational age) | Isolation-related:Low, moderate, and high isolation were associated with lower birth weight (compared with very low isolation); linear, monotonic relationshipLow, moderate, and high isolation were modestly associated with higher odds of fetal growth restriction (compared with very low isolation)Clustering-related: no statistically significant associations found between clustering and birth outcomes |
Notes. LBW = low birth weight (< 2500 g or < 5.5 lbs); MA = metropolitan area; MSA = metropolitan statistical area; PTB = preterm birth (< 37 wk gestation).
The majority of research on perceived interpersonal discrimination and health focuses on adults.34 A smaller body of literature on children and youth suggests that perceived interpersonal racial discrimination may adversely affect birth outcomes via maternal exposure (20% of studies), and adolescents’ mental health or behavioral outcomes, including depression, anxiety, self-esteem, and problem behaviors (65% of studies).31,34,35
The studies on the effects of institutional discrimination on children’s health have primarily examined the effects of racial residential segregation—which refers to the spatial separation between different racial/ethnic groups in where they live36—on birth outcomes. Segregation is considered a form of institutional discrimination because it arises not only from individual residential preferences, but also from discriminatory and exclusionary practices and policies in housing markets.37–40 Demographers measure residential segregation at the level of the metropolitan area, defined as a core area with a large population nucleus (central city), in combination with adjacent communities that have a high degree of economic and social integration with that core (suburban areas).41 Metropolitan areas are larger than cities, and are a conceptually relevant geographic unit because they approximate racially segmented housing and labor markets.37,38,42–45
In the majority of both perceived discrimination and segregation studies, the focus has largely been on the Black population in metropolitan and urban areas. Some studies have also examined Latinos and Asians. Native Americans and rural populations remain understudied.
Birth Outcomes
Black–White disparities in birth outcomes are high, persistent, and not entirely accounted for by differences in maternal education, prenatal health care, and behaviors.28 Two bodies of work have examined the role of racial discrimination in birth outcome disparities. One has focused on maternal perceptions of discrimination, and the other on the role of residential segregation. Importantly, both emphasize prenatal experiences, which is an increasingly accepted way of understanding children’s health in a life-course perspective.46
Perceived discrimination.
Evidence of whether perceived interpersonal discrimination experienced by women during pregnancy is associated with birth outcomes is mixed (i.e., nonstatistically significant findings47–49 and statistically significant adverse associations49–52). Studies have focused primarily on Black women. For example, Mustillo et al.51 found that adjusting for perceptions of discrimination substantially reduced Black–White disparities in preterm birth or low birth weight. Importantly, all studies on discrimination and birth outcomes modeled perceived discrimination as a maternal psychosocial stressor.
Segregation.
Evidence shows that high levels of racial residential segregation are associated with worse birth outcomes among Black infants. Higher residential segregation is associated with higher rates of preterm birth among Blacks,23 and with higher Black–White disparity in preterm birth rates.28 The segregation–preterm birth association is moderated by maternal age, which suggests that Black mothers may experience a weathering effect in highly segregated areas, that is a cumulatively stronger negative effect on Black women over the life course.28
The evidence is not entirely consistent, however. For instance, Hearst and Oakes26 found no statistically significant effect of segregation on Black infant mortality. However, this study may be limited by its focus on cities (instead of metropolitan areas) as the larger geographic unit of interest.53 Moreover, the authors controlled for causes of infant mortality that operate before the birth of the child, instead of considering these prenatal factors as part of the causal pathway by which segregation influences infant mortality (e.g., via preterm birth or fetal growth retardation53,54).
Although the majority of studies of segregation and birth outcomes have focused on African Americans, some recent work has focused on Latinos24,55 and Asians.25 Studies of multiple racial/ethnic groups may inform the mechanisms by which segregation influences health. Segregation may be either detrimental or beneficial depending on the factors that lead to segregation, which vary by racial/ethnic group.56 For example, among groups with large proportions of immigrants (Latinos and Asians), segregation in ethnic enclaves may be the result of preferences for residing with coethnics who can offer material and social support.57 On the other hand, segregation among US-born minorities may not reflect primarily residential preferences but blocked social and spatial mobility, including housing discrimination.58–60
The evidence indicates that segregation may not have a uniformly adverse effect. Although there is an association between higher levels of Black segregation and higher rates of low birth weight among Black infants, the level of segregation may not influence Latino birth weight,24,25 and may have a beneficial effect on Asian birth weight.25 Some studies have further disaggregated whether the effect of segregation on birth outcomes varies by nativity. Osypuk et al.24 found that whereas neighborhood isolation had no effect on the birth weight of infants of Mexican-immigrant women, it had a detrimental effect on infants of US-born, Mexican-origin women.
In sum, the empirical evidence suggests that both maternal perceptions of discrimination and residential segregation have a detrimental effect on the birth outcomes of Black infants. Although less is known about how discrimination affects birth outcomes of other groups, there is indication of differential effects of segregation by race/ethnicity and nativity, possibly related to the salutary influence of residential enclaves on immigrants.
Children’s Mental Health
Recent reviews have found consistent detrimental effects of interpersonal discrimination on children’s mental health. The literature has focused primarily on African American adolescents’ subjective experiences of discrimination and mental health or problem behaviors. Despite the focus on adolescents, there are several developmental stages that lie between birth and adolescence, with the role of discrimination mattering differently at each stage.7,8 We did not find any studies of the effects of segregation on children’s mental health.
The predominance of research on adolescents suggests that measuring the experience of interpersonal discrimination among younger children may be difficult. However, younger children may be affected by discrimination—for example, if the child receives differential treatment by influential adults, or if caregiver stress because of anticipation or experience of discrimination affects the child. Therefore, a suggested direction for strengthening this line of inquiry is to develop measures of perceived discrimination that take into account a child’s developmental stages and contexts.21,31,34
There is limited research on the combined effects of interpersonal and institutional discrimination (segregation) on children’s mental health. Only a handful of studies have directly examined contextual variation in perceived interpersonal discrimination,61 yet this evidence suggests that neighborhood context (e.g., racial/ethnic composition) may influence children’s exposure to discrimination. Black adults report higher (perceived) interpersonal discrimination if they live in predominantly White (vs predominantly Black) neighborhoods. Therefore, predominantly minority neighborhoods might shield minorities from the negative health effects of perceived interpersonal discrimination, which might partially counteract the adverse effects of residential segregation on health.62
Children’s Physical Health
A life-course perspective suggests that, by affecting birth outcomes through maternal exposure, interpersonal discrimination and segregation may influence health trajectories over childhood and beyond.46 Birth outcomes are predictive of later-life health.17,63 That said, perceived discrimination and segregation do not only affect a child’s health via birth outcomes, but they can also exert influence during later stages of a child’s development.
Recent reviews of the literature on the role of perceived discrimination during later developmental stages have found that most studies focused on children’s mental, not physical, health. We did not identify any studies of segregation and children’s physical health.
THREE LINES OF INQUIRY FOR FUTURE RESEARCH
Our results from the literature reviews suggest 3 promising directions for future work on discrimination and children’s health: further developing a life-course perspective, a geography-of-opportunity focus, and considering school segregation in addition to that of residential areas.
Discrimination in a Life-Course Perspective
A life-course perspective to understand discrimination and health would highlight issues such as developmental trajectories and transitions, critical periods (effect modification), and accumulation of disadvantage.22,64
The child development literature suggests that both perceived discrimination and its effects may vary by developmental stage.7,21,65 For example, adolescent developmental processes such as cognitive development of formal reasoning and development of racial/ethnic identity could influence perceived discrimination.7,65
Discrimination may have stronger negative effects if experienced during critical or sensitive developmental periods in which stimuli (actions or experiences, or the lack thereof) are more influential for altering the developmental trajectory compared with other periods of exposure.22,66,67 For example, perceptions of interpersonal discrimination in late childhood (ages 8–11 years), a critical developmental period for establishing healthy behaviors, may lead to substance use in early adolescence (ages 13–16 years). In turn, early substance use may lead to subsequent abuse, other behavioral problems, and effects on other domains of life such as educational attainment.68 Institutional discrimination may negatively affect the child by limiting access to supportive developmental contexts. For example, residential segregation may constrain neighborhood choices leading minority families to live in neighborhoods with more adverse developmental contexts, for instance, neighborhoods with high crime rates, which, in turn, may negatively affect children’s health trajectories.69
Discrimination may also have stronger negative effects if experienced cumulatively across time (e.g., hiring, wage setting, promotion in the labor market), across generations (e.g., reduced wealth accumulation resulting from past discrimination in mortgage lending), or across contexts (e.g., housing discrimination can lead to reduced access to neighborhoods with high-quality schools).8,12,21,65
An ecological framework of child development suggests that a child is influenced by several developmental contexts at different levels.70,71 Research shows that exposure to adverse contexts at multiple levels is even more detrimental to children than exposure to adversity only at 1 level (e.g., family).72–74 An ecological framework of child development informs our understanding of how discrimination at multiple levels—from interpersonal to institutional—may affect the child. In addition, discrimination can result in harmful experiences across developmental contexts.43,75,76 For example, residential segregation is associated with racial/ethnic disparities in children’s simultaneous exposure to family and neighborhood poverty.75
Future research should examine whether the experience and effects of discrimination vary by developmental stage, including sensitive periods, and by whether discrimination is experienced cumulatively across time, and whether interpersonal and institutional discrimination may interact.
Geography of Opportunity and Children’s Health
Ecological,18,70 child-resilience,77 and biological-sensitivity-to-context78 models emphasize the importance of the multiple contexts (e.g., family, neighborhood, school) in which children grow and develop. Yet race is often missing from these models, although racial–spatial phenomena, such as residential and school segregation, have a strong influence on racial disparities in child developmental contexts, which in turn may affect developmental trajectories.21,79,80
Although a large body of evidence suggests that neighborhood characteristics are significantly associated with children’s health,76,81,82 and that residential segregation is associated with large racial/ethnic disparities in neighborhood context,35,75,83 the literature on the social determinants of children’s health does not have sufficient geographic or spatial focus to capture how segregation shapes children’s developmental contexts along both spatial and racial/ethnic lines.75,79 A framework such as the geography of children’s opportunity highlights the importance of such racial–spatial patterns.84 The geography of children’s opportunity is defined as the context of neighborhood-based opportunities that influence children’s health and development.62,75,79,85 These opportunities include services that support a child’s development (e.g., quality educational institutions) and services that support families, parents, and parenting and community engagement; healthy and safe physical environments (e.g., safe playgrounds); and healthy and safe social environments (e.g., safety, positive peer influences).
Characterizing neighborhoods by using a geography-of-opportunity framework points to selecting indicators that either impede opportunity (e.g., high neighborhood poverty) or facilitate opportunity (e.g., availability of high-quality early childhood education). Neighborhood-based opportunity (or lack thereof) can be conceptualized as neighborhood-based protective (risk) factors for healthy children’s development, and one can examine its effects on children’s developmental trajectories. Applying this framework would imply creating an index of neighborhood opportunity for healthy children’s development by combining multiple indicators of risk and protective factors, mapping and ranking neighborhoods within a region according to this index, and examining the association of the index with health or developmental trajectories.79,86
Although an index of neighborhood-based opportunity is race-neutral on face (i.e., it does not include measures of race/ethnicity), its application can be used to understand racial/ethnic health disparities because, in practice, neighborhood opportunity varies significantly by race. Within metropolitan areas, minority children are more likely than White children to live in neighborhoods of low opportunity, and distributions of neighborhood opportunity within metropolitan areas differ considerably by race/ethnicity, such that the lower-opportunity neighborhoods for Whites are often better than the higher-opportunity neighborhood for Blacks and Latinos.43,62,80,85,87 Across metropolitan areas, racial disparities in access to neighborhoods of opportunity are larger in areas with higher levels of segregation.75 The inequitable distribution of neighborhood contexts has implications for children’s health because it signals disproportionate concentration of neighborhood-level risk factors (indicating lack of opportunity) in minority neighborhoods.69,80,88–90
In sum, although a large body of social science research has documented pervasive patterns of neighborhood inequality,38,87,91–95 and some empirical health studies have examined the geographic distribution of risk and protective factors relevant to children, greater specificity about racial/ethnic distributions of neighborhood risk and protective factors relevant to children would enhance our understanding of how and to what extent segregation may affect children’s health and health disparities. Therefore, a geography-of-opportunity framework may be a fruitful approach for understanding the role of place-based racial/ethnic inequality in children’s health disparities.
SCHOOL SEGREGATION AND HEALTH
The segregation–child health literature has focused on residential or neighborhood segregation. However, segregation in other contexts matters for health both during childhood and along the life course. Because attendance at most public elementary schools is neighborhood-based in the United States, residential segregation strongly affects school segregation, which in turn is associated with poor educational outcomes and disparities in achievement.2 At the same time, the importance of education in adult health has been widely documented.96 Because school segregation occurs in childhood and creates racial disparities in achievement, it may be associated with health disparities later in life. One longitudinal study found that school desegregation plans in the 1960s through 1980s had favorable effects on childhood exposure to school quality, and, subsequently, on Black adult educational attainment, earnings, probability of incarceration, and health. School desegregation did not affect those outcomes for Whites, but because it improved outcomes for Blacks, it contributed to reducing Black–White adult socioeconomic and health disparities among cohorts exposed to integrated schools during childhood.97 Another study found that school desegregation plans in the 1970s were associated with a significant reduction in the Black adolescent birth rate from 1970 to 1980.98
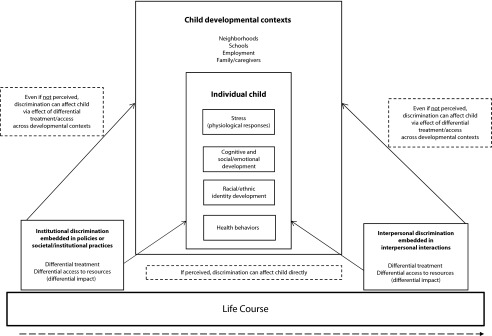
Figure 2 illustrates the variation in residential or school segregation across metropolitan areas, with significant positive correlations between children’s residential segregation and school segregation (Blacks: ρ = 0.96; P < .001; Latinos: ρ = 0.91; P < .001). Because residential and school segregation go hand in hand, so do vast racial and ethnic disparities in both neighborhood and school poverty.91,99 Such simultaneous disadvantage across multiple contexts may compromise the health of Black and Latino children. School segregation is associated with sharp disparities in exposure to schools with high poverty levels—in the 100 largest metropolitan areas, about 43% of Black and Latino students attend schools where more than 80% of the student population is poor, whereas only 4% of White students attend such highly disadvantaged schools.99 Differences in school exposure to poverty are associated with other school-level exposures—for instance, high-poverty schools are more likely to have inadequate buildings than low-poverty schools100—that may influence health.
FIGURE 2—
School and neighborhood segregation of (a) Black and White children and (b) Latino and White children: 100 largest US Metropolitan areas, 2010.
Note. Circle size reflects relative size of the specified minority child population. Segregation was defined by using dissimilarity indices, which reflect the percentage of specified minority children or students who would have to move to another census tract or school for each census tract or school to have the same share of specified minority and White children or students as the metropolitan area as a whole. School segregation was measured for public primary schools, defined as schools with lowest grade of prekindergarten–3 and highest grade of prekindergarten–8. Neighborhood segregation includes children aged < 18 years, with neighborhoods defined by census tracts.
Source. diversitydata.org calculations from 2010 Census Redistricting File5 for residential segregation and from National Center for Education Statistics, Common Core of Data 2009–20106 for school segregation.
Even though segregation across neighborhoods and schools is highly correlated, school segregation may be more relevant than neighborhood segregation because of more direct school effects on younger as well as older children (as opposed to indirect effects of neighborhoods on younger children).101
In sum, although schools are regarded as a key context for children’s development, research on school segregation and children’s health is only beginning to emerge.
CONCLUSIONS
Pervasive experiences of interpersonal and institutional discrimination may be key to understanding the developmental contexts and health trajectories of minority children. To inform the field on the importance of discrimination for children’s health, future studies should expand beyond a focus on only adults, adopt life-course models, and incorporate perspectives from the field of racial inequality such as geography of opportunity and segregation in other children’s contexts.
Acknowledgments
The authors gratefully acknowledge support from the W. K. Kellogg Foundation for diversitydata.org and diversitydatakids.org (D. A.-G., PI).
Human Participant Protection
No protocol approval was needed for this study because it did not involve human participants.
References
- 1.Satcher D, Fryer GJ, McCann J, Troutman A, Woolf S, Rust G. What if we were equal? A comparison of the Black–White mortality gap in 1960 and 2000. Health Aff (Millwood). 2005;24(2):459–464 [DOI] [PubMed] [Google Scholar]
- 2.Farkas G. Racial Disparities and Discrimination in Education: What Do We Know, How Do We Know It, and What Do We Need to Know? Prepared for the Workshop on Measuring Disparities in Education, Division of Behavioral and Social Sciences and Education, Committee on National Statistics, National Research Council, Washington, DC. University Park, PA: Pennsylvania State University; 2002.
- 3. Monthly population estimates by age, sex, race, and Hispanic origin for the United States: April 1, 2010 to July 1, 2011 (with short-term projections to dates in 2012). Washington, DC: US Census Bureau, Population Division. Release date: May 2012. Available at: http://www.census.gov/popest/data/national/asrh/2011/2011-nat-res.html. Accessed November 18, 2012.
- 4. US population estimates by age, sex, race, and Hispanic origin: 1980 to 1999 (with short-term projection to dates in 2000). Washington, DC: US Census Bureau, Population Division. Internet release date: April 11, 2000. Available at: http://www.census.gov/popest/data/national/asrh/1980s/80s_nat_detail.html. Accessed November 18, 2012.
- 5. 2010 Census Redistricting Data, PL 94-171 [machine-readable data files]. Washington, DC: US Census Bureau; 2011.
- 6. Common Core of Data. Public Elementary/Secondary School Universe Survey Data: 2009–2010. US Department of Education. Washington, DC: Institute of Education Sciences, National Center for Education Statistics. Available at: http://nces.ed.gov/ccd/pubschuniv.asp. Accessed November 18, 2012.
- 7.Seaton EK, Caldwell CH, Sellers RM, Jackson JS. The prevalence of perceived discrimination among African American and Caribbean Black youth. Dev Psychol. 2008;44(5):1288–1297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blank RM, Dabady M, Citro CF. Committee on National Statistics, National Research Council, Measuring Racial Discrimination. Washington, DC: National Academy Press; 2004 [Google Scholar]
- 9.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212–1215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smedley BD, Stith AY, Nelson AR, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Institute of Medicine Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003 [PubMed] [Google Scholar]
- 11.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pager D, Shepherd H. The sociology of discrimination: racial discrimination in employment, housing, credit, and consumer markets. Annu Rev Sociol. 2008;34:181–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jolls C, Sunstein CR. The law of implicit bias. Calif Law Rev. 2006;94:969–996 [Google Scholar]
- 14.Walker SP, Wachs TD, Grantham-McGregor Set al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011;378(9799):1325–1338 [DOI] [PubMed] [Google Scholar]
- 15.Maggi S, Irwin LJ, Siddiqi A, Hertzman C. The social determinants of early child development: an overview. J Paediatr Child Health. 2010;46(11):627–635 [DOI] [PubMed] [Google Scholar]
- 16.Sachser N, Hennessy MB, Kaiser S. Adaptive modulation of behavioural profiles by social stress during early phases of life and adolescence. Neurosci Biobehav Rev. 2011;35(7):1518–1533 [DOI] [PubMed] [Google Scholar]
- 17.Palloni A. Reproducing inequalities: luck, wallets, and the enduring effects of childhood health. Demography. 2006;43(4):587–615 [DOI] [PubMed] [Google Scholar]
- 18.Shonkoff JP, Phillips DA, From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: National Academies Press; 2000 [PubMed] [Google Scholar]
- 19.French SE, Seidman E, Allen L, Aber JL. The development of ethnic identity during adolescence. Dev Psychol. 2006;42(1):1–10 [DOI] [PubMed] [Google Scholar]
- 20.Caughy MOB, Nettles SM, O’Campo PJ, Lohrfink KF. Neighborhood matters: racial socialization of African American children. Child Dev. 2006;77(5):1220–1236 [DOI] [PubMed] [Google Scholar]
- 21.García Coll C, Lamberty G, Jenkins Ret al. An integrative model for the study of developmental competencies in minority children. Child Dev. 1996;67(5):1891–1914 [PubMed] [Google Scholar]
- 22.Gee GC, Walsemann KM, Brondolo E. A life course perspective on how racism may be related to health inequities. Am J Public Health. 2012;102(5):967–974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kramer MR, Cooper HL, Drews-Botsch CD, Waller LA, Hogue CR. Metropolitan isolation segregation and Black–White disparities in very preterm birth: a test of mediating pathways and variance explained. Soc Sci Med. 2010;71(12):2108–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Osypuk TL, Bates LM, Acevedo-Garcia D. Another Mexican birthweight paradox? The role of residential enclaves and neighborhood poverty in the birthweight of Mexican-origin infants. Soc Sci Med. 2010;70(4):550–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walton E. Residential segregation and birth weight among racial and ethnic minorities in the United States. J Health Soc Behav. 2009;50(4):427–442 [DOI] [PubMed] [Google Scholar]
- 26.Hearst MO, Oakes JM. The effect of racial residential segregation on Black infant mortality. Am J Epidemiol. 2008;168(11):1247–1254 [DOI] [PubMed] [Google Scholar]
- 27.Kramer MR, Hogue CR. Place matters: variation in the Black/White very preterm birth rate across U.S. metropolitan areas, 2002–2004. Public Health Rep. 2008;123(5):576–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osypuk TL, Acevedo-Garcia D. Are preterm birth racial disparities larger in hypersegregated areas? Am J Epidemiol. 2008;167(11):1295–1304 [DOI] [PubMed] [Google Scholar]
- 29.Bell JF, Zimmerman FJ, Mayer JD, Almgren GR, Huebner CE. Associations between residential segregation and smoking during pregnancy among urban African-American women. J Urban Health. 2007;84(3):372–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med. 2006;63(12):3030–3045 [DOI] [PubMed] [Google Scholar]
- 31.Pachter LM, Coll CG. Racism and child health: a review of the literature and future directions. J Dev Behav Pediatr. 2009;30(3):255–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Giurgescu C, McFarlin B, Lomax J, Craddock C, Albrecht A. Racial discrimination and the Black–White gap in adverse birth outcomes: a review. J Midwifery Womens Health. 2011;56(4):362–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sanders-Phillips K. Racial discrimination: a continuum of violence exposure for children of color. Clin Child Fam Psychol Rev. 2009;12(2):174–195 [DOI] [PubMed] [Google Scholar]
- 34.Sanders-Phillips K, Settles-Reaves B, Walker D, Brownlow J. Social inequality and racial discrimination: risk factors for health disparities in children of color. Pediatrics. 2009;124(Suppl 3):S176–S186 [DOI] [PubMed] [Google Scholar]
- 35.Jones CP, Jones CY, Perry GS, Barclay G, Jones CA. Addressing the social determinants of children’s health: a cliff analogy. J Health Care Poor Underserved. 2009;20(4 Suppl):1–12 [DOI] [PubMed] [Google Scholar]
- 36.Acevedo-Garcia D. Residential segregation and the epidemiology of infectious diseases. Soc Sci Med. 2000;51(8):1143–1161 [DOI] [PubMed] [Google Scholar]
- 37.Acevedo-Garcia D, Osypuk TL. Impacts of housing and neighborhoods on health: pathways, racial/ethnic disparities, and policy directions. : Carr J, Kutty N, Segregation: The Rising Costs for America. New York, NY: Routledge; 2008:197–235 [Google Scholar]
- 38.Massey DS. Origins of economic disparities: historical role of housing segregation. : Carr J, Kutty N, Segregation: The Rising Costs for America. New York, NY: Routledge; 2008 [Google Scholar]
- 39.Pendall R. Local land use regulation and the chain of exclusion. J Am Plann Assoc. 2000;66:125–142 [Google Scholar]
- 40.Rothwell JT, Massey DS. Density zoning and class segregation in U.S. metropolitan areas. Soc Sci Q. 2010;91(5):1123–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.American Factfinder Glossary, Central City and Metropolitan Statistical Area. Washington, DC: US Census Bureau; 2008 [Google Scholar]
- 42.Jargowsky PA. Stunning progress, hidden problems: the dramatic decline of concentrated poverty in the 1990s. In: Center on Urban and Metropolitan Policy, ed. The Living Cities Census Series. Washington, DC: Brookings Institution; 2003. [Google Scholar]
- 43.Osypuk TL, Galea S, McArdle N, Acevedo-Garcia D. Quantifying separate and unequal: racial–ethnic distributions of neighborhood poverty in metropolitan America. Urban Aff Rev Thousand Oaks Calif. 2009;45(1):25–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Charles CZ. The dynamics of racial residential segregation. Annu Rev Sociol. 2003;29:167–207 [Google Scholar]
- 46.Misra DP, Guyer B, Allston A. Integrated perinatal health framework: a multiple determinants model with a life span approach. Am J Prev Med. 2003;25(1):65–75 [DOI] [PubMed] [Google Scholar]
- 47.Collins JW, David RJ, Symons R, Handler A, Wall SN, Dwyer L. Low-income African-American mothers’ perception of exposure to racial discrimination and infant birth weight. Epidemiology. 2000;11(3):337–339 [DOI] [PubMed] [Google Scholar]
- 48.Shiono PH, Rauh VA, Park M, Lederman SA, Zuskar D. Ethnic differences in birthweight: the role of lifestyle and other factors. Am J Public Health. 1997;87(5):787–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rosenberg L, Palmer JR, Wise LA, Horton NJ, Corwin MJ. Perceptions of racial discrimination and the risk of preterm birth. Epidemiology. 2002;13(6):646–652 [DOI] [PubMed] [Google Scholar]
- 50.Collins JW, David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94(12):2132–2138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black–White differences in preterm and low-birthweight deliveries: the CARDIA study. Am J Public Health. 2004;94(12):2125–2131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon M, Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157(1):14–24 [DOI] [PubMed] [Google Scholar]
- 53.Acevedo-Garcia D, Osypuk TL. Residential segregation and health: the complexity of modeling separate social contexts. Am J Epidemiol. 2008;168(11):1255–1258 [DOI] [PubMed] [Google Scholar]
- 54.Gravlee CC. How race becomes biology: embodiment of social inequality. Am J Phys Anthropol. 2009;139(1):47–57 [DOI] [PubMed] [Google Scholar]
- 55.Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med. 2007;65(7):1524–1535 [DOI] [PubMed] [Google Scholar]
- 56.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian S. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pearl M, Braveman P, Abrams B. The relationship of neighborhood socioeconomic characteristics to birthweight among 5 ethnic groups in California. Am J Public Health. 2001;91(11):1808–1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Portes A. The New Second Generation. New York, NY: Russell Sage Foundation; 1996 [Google Scholar]
- 59.Portes A, Rumbaut RG. Not Everyone Is Chosen: Segmented Assimilation and Its Determinants. Berkeley and Los Angeles, CA, and New York, NY: University of California Press, Russell Sage Foundation; 2001 [Google Scholar]
- 60.Portes A, Rumbaut RG. Immigrant America: A Portrait. 3rd ed Berkeley, CA: University of California Press; 2006 [Google Scholar]
- 61.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92(4):615–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: a geography of opportunity perspective for understanding racial/ethnic health disparities. Health Place. 2010;16(6):1113–1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Case A, Paxson C. Children’s health and social mobility. Future Child. 2006;16(2):151–173 [DOI] [PubMed] [Google Scholar]
- 64.Kuh D, Ben-Shlomo Y, Lynch J, Hallquist J, Power C. Life course epidemiology. J Epidemiol Community Health. 2003;57(10):778–783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Szalacha L, Erkut S, García Coll C, Alarcón O, Fields J, Ceder I. Discrimination and Puerto Rican children and adolescents’ mental health. Cultur Divers Ethnic Minor Psychol. 2003;9(2):141–155 [DOI] [PubMed] [Google Scholar]
- 66.Gluckman P, Hanson M. The Fetal Matrix: Evolution, Development, and Disease. Cambridge, England: Cambridge University Press; 2005 [Google Scholar]
- 67.Thomas RM. Comparing Theories of Child Development. Belmont, CA: Wadson/Thomson Learning; 2000 [Google Scholar]
- 68.Gibbons FX, Yeh H-C, Gerrard Met al. Early experience with racial discrimination and conduct disorder as predictors of subsequent drug use: a critical period hypothesis. Drug Alcohol Depend. 2007;88(Suppl 1):S27–S37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Timberlake JM, Kirk DS. A Spatio-Temporal Assessment of Exposure to Neighborhood Violence. Washington, DC: Population Association of America; 2011 [Google Scholar]
- 70.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979 [Google Scholar]
- 71.Bronfenbrenner U. Ecology of the family as a context for human development: research perspectives. Dev Psychol. 1986;22(6):723–742 [Google Scholar]
- 72.Evans GW, Kim P, Ting AH, Tesher HB, Shannis D. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev Psychol. 2007;43(2):341–351 [DOI] [PubMed] [Google Scholar]
- 73.Crosnoe R, Leventhal T, Wirth R, Pierce KM, Pianta RC, NICHD Early Child Care Research Network Family socioeconomic status and consistent environmental stimulation in early childhood. Child Dev. 2010;81(3):972–987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dupere V, Leventhal T, Crosnoe R, Dion E. Understanding the positive role of neighborhood socioeconomic advantage in achievement: the contribution of the home, child care, and school environments. Dev Psychol. 2010;46(5):1227–1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. Towards a policy relevant analysis of geographic and racial/ethnic disparities in child health. Health Aff (Millwood). 2008;27(2):321–333 [DOI] [PubMed] [Google Scholar]
- 76.Sampson RJ. Neighborhood context of well-being. Perspect Biol Med. 2003;46(3 Suppl):S53–S64 [PubMed] [Google Scholar]
- 77.Loucks E. Biological markers in housing–health research. Presented at: Harvard School of Public Health Symposium on Housing, Neighborhoods, & Health: State of the Evidence; June 26, 2003; Boston, MA. [Google Scholar]
- 78.Obradović J, Stamperdahl J, Bush N, Adler N, Boyce W. Biological sensitivity to context: the interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Dev. 2010;81(1):270–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Acevedo-Garcia D, Rosenfeld LE, McArdle N, Osypuk TL. The geography of opportunity: a framework for child development. : Velasco CE, Jr, Changing Places: How Communities Will Improve the Health of Boys of Color. Berkeley, CA: University of California Press; 2010: 358–406 [Google Scholar]
- 80.Sampson RJ, Sharkey P, Raudenbush SW. Durable effects of concentrated disadvantage on verbal ability among African-American children. Proc Natl Acad Sci USA. 2008;105(3):845–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126(2):309–337 [DOI] [PubMed] [Google Scholar]
- 82.Brooks-Gunn J, Duncan GJ, Klebanov PK, Sealand N. Do neighborhoods influence child and adolescent development? Am J Sociol. 1993;99(2):353–395 [Google Scholar]
- 83.Galster GC, Killen SP. The geography of metropolitan opportunity: a reconnaissance and conceptual framework. Housing Policy Debate. 1995;6(1):7–43 [Google Scholar]
- 84.Rose G. The Strategy of Preventive Medicine. New York, NY: Oxford University Press; 1992 [Google Scholar]
- 85.Acevedo-Garcia D, Osypuk TL, McArdle N. Racial/ethnic integration and child health disparities. : Hartman C, Squires G, The Integration Debate Competing Futures for American Cities. New York, NY: Routledge; 2009: 131–152 [Google Scholar]
- 86.Jason Reece SG, Powell JA, Grant-Thomas A. The Geography of Opportunity: Building Communities of Opportunity in Massachusetts: Massachusetts Legal Services Programs. Columbus, OH: Kirwan Institute for the Study of Race and Ethnicity; 2009 [Google Scholar]
- 87.Logan JR, Oakley D, Smith P, Stowell J, Stults B. Separating the Children. Albany, NY: Lewis Mumford Center for Comparative Urban and Regional Research; 2001 [Google Scholar]
- 88.Massey DS. Segregation and stratification: a biosocial perspective. Du Bois Rev. 2004;1(1):7–25 [Google Scholar]
- 89.Morenoff JD. Neighborhood mechanisms and the spatial dynamics of birth weight. Am J Sociol. 2003;108(5):976–1017 [DOI] [PubMed] [Google Scholar]
- 90.Krivo LJ, Peterson RD, Payne DD. Segregation, racial structure, and neighborhood crime. Am J Sociol. 2009;114(6):1765–1802 [DOI] [PubMed] [Google Scholar]
- 91.Logan JR. Choosing segregation: racial imbalance in American public schools, 1990–2000. Albany, NY: Lewis Mumford Center for Comparative Urban and Regional Research; 2002 [Google Scholar]
- 92.Logan JR. Hispanic Populations and Their Residential Patterns in the Metropolis. Albany, NY: State University of New York at Albany, Lewis Mumford Center for Comparative Urban and Regional Research; 2002 [Google Scholar]
- 93.Massey DS. Residential segregation and neighborhood conditions in U.S. metropolitan areas. In: Smelser NJ, Wilson WJ, Mitchell F, National Research Council, eds. America Becoming: Racial Trends and Their Consequences. Washington, DC: National Academy Press; 2001: 391–434. [Google Scholar]
- 94.Massey DS, Condran GA, Denton NA. The effect of residential segregation on Black social and economic well-being. Soc Forces. 1987;66:29–56 [Google Scholar]
- 95.Massey DS, Fischer MJ. How segregation concentrates poverty. Ethn Racial Stud. 2000;23:670–691 [Google Scholar]
- 96.Kimbro RT, Bzostek S, Goldman N, Rodriguez G. Race, ethnicity, and the education gradient in health. Health Aff (Millwood). 2008;27(2):361–372 [DOI] [PubMed] [Google Scholar]
- 97.Johnson RC. Long-Run Impacts of School Desegregation & School Quality on Adult Attainments. Cambridge, MA: National Bureau of Economic Research; 2011. NBER working paper 16664 [Google Scholar]
- 98.Liu SY, Linkletter CD, Loucks EB, Glymour MM, Buka SL. Decreased births among Black female adolescents following school desegregation. Soc Sci Med. 2012;74(7):982–988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.McArdle N, Acevedo-Garcia D. Segregation and Exposure to High-Poverty Schools in Large Metropolitan Areas: 2008–09. DiversityData Report. Boston, MA: DiversityData.org; 2011. Report no. 2 [Google Scholar]
- 100.Filardo MW, Vincent JM, Sung P, Stein T. Growth and Disparity: A Decade of U.S. Public School Construction. Washington, DC: Building Educational Success Together; 2006 [Google Scholar]
- 101.Leventhal T, Dupéré V, Brooks-Gunn J. Neighborhood influences on adolescent development. : Lerner R, Steinberg L, Handbook of Adolescent Psychology. Hoboken, NJ: Wiley; 2009: 411–443 [Google Scholar]