Abstract
Objectives. To estimate the percentage of excess death for US Black and White men and women associated with high body mass, we examined the combined effects of age variation in the obesity–mortality relationship and cohort variation in age-specific obesity prevalence.
Methods. We examined 19 National Health Interview Survey waves linked to individual National Death Index mortality records, 1986–2006, for age and cohort patterns in the population-level association between obesity and US adult mortality.
Results. The estimated percentage of adult deaths between 1986 and 2006 associated with overweight and obesity was 5.0% and 15.6% for Black and White men, and 26.8% and 21.7% for Black and White women, respectively. We found a substantially stronger association than previous research between obesity and mortality risk at older ages, and an increasing percentage of mortality attributable to obesity across birth cohorts.
Conclusions. Previous research has likely underestimated obesity’s impact on US mortality. Methods attentive to cohort variation in obesity prevalence and age variation in obesity’s effect on mortality risk suggest that obesity significantly shapes US mortality levels, placing it at the forefront of concern for public health action.
Among health professionals there is widespread agreement that high rates of obesity present serious public health challenges in the United States. Yet the ultimate toll that obesity will take on the health and longevity of Americans remains a hotly contested issue. Disagreement on this point is driven largely by contradictory findings about the obesity–mortality association,1 as well as widely divergent estimates of the fraction of mortality in the US population that is attributable to overweight and obesity—also known as population attributable fractions (PAFs).1–7 Without a broader consensus in the research community, policymakers will lack clear guidance on how to prioritize and appropriately respond to the US obesity epidemic.
Our study helps resolve these debates by reassessing obesity–mortality associations and PAFs by using concepts and methods that better capture the complexity of the epidemic and its impact on US mortality. We note that a PAF is composed of 2 factors: (1) the individual-level association between body mass and mortality risk (i.e., the effect) and (2) patterns in US overweight and obesity prevalence (i.e., the population’s exposure to this effect).
Early estimates of obesity-attributable mortality were criticized for failing to account for either variability (e.g., by age) in obesity’s effect on mortality (component 1 of the PAF) or the divergent rates of obesity across subpopulations (component 2 of the PAF).7,8 More recent studies that attend to some of these issues have produced lower estimated fractions of US deaths attributable to overweight and obesity than found in earlier investigations.5–7 Although corrective actions taken in recent studies were useful and necessary, our main contention is that they underestimated the effects of obesity on US mortality for 2 main reasons.
First, survival models assessing mortality differences between the normal weight, overweight, and obese populations in recent studies failed to account for factors that potentially bias estimates of the obesity–mortality association. For example, older obese individuals are less likely than their normal-weight peers to participate in health surveys because of obesity-related health complications. Because previous studies have not accounted for this, associations between measures of high body mass (e.g., body mass index [BMI, defined as weight in kilograms divided by the square of height in meters], waist-to-thigh ratio) and mortality have been reported to be weaker than they likely really are. Because, in part, of such limitations, many existing studies have concluded that overweight and obesity confer only a modest increase in mortality risk.
Second, PAF estimates for overweight and obesity as causes of mortality are usually derived from equations that use average rates of obesity to indicate exposure.8 These population averages overlook substantial differences in obesity prevalence among persons belonging to different birth cohorts.9–11 Although obesity is certainly influenced by the biological aging process (i.e., age effects) and broad societal changes that have transpired in recent decades (i.e., period effects), it is also influenced by birth cohort membership (i.e., cohort effects)—the so-called “third dimension” of the obesity epidemic.11 Birth cohort membership is important because it represents the onset of exposure to obesogenic environments; newer birth cohorts tend to have earlier onset and, thus, higher rates of obesity than their predecessors. Although recent work suggests that birth cohort dynamics are key to understanding the future of US health and longevity,10,11 existing PAF estimates for obesity as a cause of US mortality omit them from consideration. As a result, these studies may underestimate the impact of rising obesity prevalence on US mortality.
In addition to these 2 main concerns, we also note that much previous research indicates that the obesity–mortality link diminishes with age, with some evidence suggesting that overweight may even provide a survival advantage at older ages.12–18 However, recent studies have shown that weaker associations between obesity and mortality at older ages likely reflect confounding from cohort variation in mortality risk,19 healthy participant effects (i.e., biases introduced by survey selection of healthy respondents),20 or duration of one’s life spent obese.21 In fact, contrary to current wisdom, the obesity–mortality association has been shown to grow significantly stronger with age after one accounts for these confounding factors.22 Estimates of PAF for obesity as a cause of US mortality need to be updated in light of these recent discoveries.
We address these problems in some previous research via analyses of a large, nationally representative data set composed of multiple birth cohorts that includes (1) previously unaccounted for confounders of the obesity–mortality association, and (2) cohort-specific estimates of obesity prevalence. Results from our models suggest that the obesity epidemic is worthy of its status as a leading public health concern in the United States.
METHODS
Data came from 19 consecutive waves of the National Health Interview Survey (NHIS), 1986 through 2004. These data were linked to follow-up mortality information at the National Death Index through the end of 2006 by the National Center for Health Statistics; we dropped respondents ineligible for matches from our sample. The 1986–2006 NHIS Linked Mortality Files are the most up-to-date data available, and the population-based sampling design of the NHIS allows us to produce survival estimates for the US non-Hispanic Black (henceforth “Black”) and non-Hispanic White (henceforth “White”) noninstitutionalized adult populations between January 1, 1986, and December 31, 2006.23
To focus on the association between obesity and adult mortality, the final sample includes respondents aged 40 to 84.9 years at any time between their survey date and December 31, 2006. We omitted respondents aged 85 years or older to safeguard against bias induced by the open-ended 85+ age coding in the NHIS. We also dropped respondents with BMI less than 18.5 (less than 1% of the sample) from the sample because “underweight” BMI is often indicative of preexisting illness, frailty, or increased mortality risk.7,24 Also, we excluded cases with missing values on height, weight, educational attainment, marital status, or region of residence. Our final sample consisted of 290 383 White men, 41 710 Black men, 324 131 White women, and 61 344 Black women. We stratified all analyses by race/ethnicity and sex; we omitted other race/ethnicity groups because of small sample sizes.
Outcome and Measures
All-cause mortality was the main outcome in our study. We estimated hazard ratios between study participants with high levels of BMI and participants with normal BMI by using Royston-Parmar survival models with time measured as respondents’ attained age, either at date of death or at the end of the follow-up period (right censoring occurred on December 31, 2006). We used the STSET command in Stata version 12 (StataCorp LP, College Station, TX) to account for left-censoring by declaring each respondent’s exposure time to begin at age at time of survey.
Covariates included educational attainment, household income, marital status, region of residence, age at time of survey, and birth cohort. We categorized educational attainment as less than high school, high-school graduate, some college, or bachelor’s degree or higher. We categorized family income, as coded in the NHIS, as earning less than the federal poverty level, greater than or equal to poverty but less than $45 000, or $45 000 or higher. Because of high nonresponse rates to questions about income, we created an additional “missing” income category. We divided marital status and region of residence each into 4 categories: married, divorced or separated, never married, and widowed; and Northeast, South, Midwest, and West.
Consistent with US federal guidelines, we coded respondents as having normal weight if BMI was calculated to be 18.5 to 24.9, overweight if BMI was calculated to be 25.0 to 29.9, and obese if BMI was calculated to be 30.0 or higher. Consistent with previous studies, we further divided the obesity category into “grade 1” obesity (BMI = 30.0–34.9) and “grade 2/3” obesity (BMI ≥ 35.0). Height and weight were self-reported in NHIS; we addressed biases in self-reporting by (1) correcting underestimates of body weight given by proxy respondents,25 and (2) adjusting NHIS estimates to match BMI levels and trends in the National Health and Nutrition Examinations and Surveys, which are based on clinical measures of height and weight.26 Descriptive statistics of all sample outcomes and covariates are provided in Table A (available as a supplement to the online version of this article at http://www.ajph.org).
Statistical Analyses
To estimate the proportion of early adult deaths in the United States between 1986 and 2006 attributable to each BMI level, we proceeded across 3 analytical steps: (1) estimate age-specific obesity rates among different birth cohorts, (2) estimate age-specific hazard ratios, and (3) use estimates (1) and (2) to estimate cohort-specific PAFs. First, to assess obesity prevalence we fitted hierarchical age–period–cohort cross-classified random effects models to obtain age, period, and cohort coefficient estimates for the likelihood of overweight, grade 1 obesity status, and grade 2/3 obesity status between 1986 and 2004.27 Linear and quadratic functional forms of age were modeled. The model is expressed as
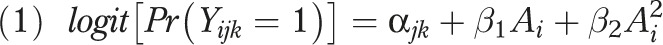 |
where  = 1 represents the existence of obesity for the ith respondent for i = 1,…,njk individuals in the jth survey year for j = 1,…,J years and the kth 5-year birth cohort for k = 1,…,K cohorts. The
= 1 represents the existence of obesity for the ith respondent for i = 1,…,njk individuals in the jth survey year for j = 1,…,J years and the kth 5-year birth cohort for k = 1,…,K cohorts. The  and
and  terms represent yearly age and age-squared, respectively, which were centered on 25 years of age at time of survey.
terms represent yearly age and age-squared, respectively, which were centered on 25 years of age at time of survey.
The random intercept in equation 1 is expressed as
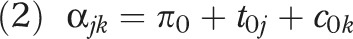 |
where  indicates that the overall mean logit of obesity varies for each survey year of observation j and each 5-year birth cohort k,
indicates that the overall mean logit of obesity varies for each survey year of observation j and each 5-year birth cohort k,  is the expected logit when the centered values of
is the expected logit when the centered values of  and
and  are zero,
are zero,  is the average period effect averaged over all birth cohorts with variance
is the average period effect averaged over all birth cohorts with variance  , and
, and  is the overall cohort effect averaged over all survey years with variance
is the overall cohort effect averaged over all survey years with variance  .
.
With the models specified in equations 1 and 2, we fitted a cross-classified random effects model of the logit of the probability of obesity separately for US Black and White men and women by using Stata version 12’s XTMELOGIT program, weighting the samples to be representative of the 1986–2004 US noninstitutionalized population.
Second, we used Royston-Parmar survival models to estimate instantaneous age-varying obesity hazard ratios for each sex–race/ethnicity subsample between ages 40 and 85 years. Respondents’ ages at time of survey were included in all models to account for biasing effects of age-based survey selection, and interactions between BMI levels and age-at-survey control for body weight differences in survey selection bias.22,28 We also accounted for cohort variation in mortality risk by including 5-year cohort dummy variables. Thus, unlike previous estimates of PAF for obesity as a cause of mortality, our hazard models controlled for cohort variation in mortality risk and BMI variation in age-related survey selection bias.
Using restricted cubic spline function of ln(t) with knots  , written as
, written as 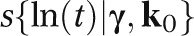 , we estimated Royston-Parmar models on the baseline log cumulative hazard scale. We incorporated age-varying effects of the 3 BMI categories by using interactions of the form
, we estimated Royston-Parmar models on the baseline log cumulative hazard scale. We incorporated age-varying effects of the 3 BMI categories by using interactions of the form 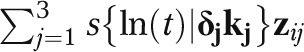 , resulting in the following model for the log cumulative hazard:
, resulting in the following model for the log cumulative hazard:
 |
for j = 1,…,3 BMI levels interacting with the spline terms using  number of knots for the jth covariate (see Royston and Lambert29 for a thorough discussion). We stratified models by sex and race/ethnicity and estimated with Stata version 12’s STPM2 program, using sample weights that are representative of the US noninstitutionalized population.
number of knots for the jth covariate (see Royston and Lambert29 for a thorough discussion). We stratified models by sex and race/ethnicity and estimated with Stata version 12’s STPM2 program, using sample weights that are representative of the US noninstitutionalized population.
Next, we combined estimates of age-specific hazard ratios for overweight, grade 1 obesity, and grade 2/3 obesity with cohorts’ age-specific rates of overweight, grade 1, and grade 2/3 obesity to calculate the amount of US adult mortality between ages 40 and 85 years associated with overweight and obesity. These products were standardized by the age distributions of death in each race/ethnicity–sex population during the year 2000. Thus, to estimate the population-attributable risk fraction for high BMI as a cause of US mortality we incorporated sex, race/ethnicity, age, and cohort effect modifiers in PAF8 through the following equation:
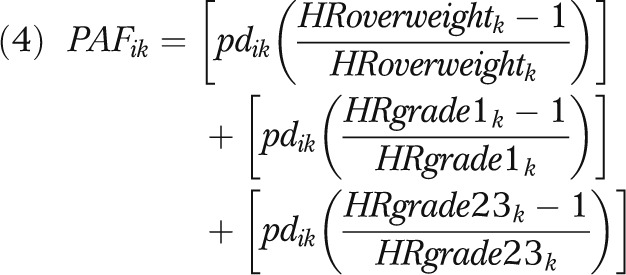 |
where PAFik represents the PAF for the exposed population at kth age and ith 5-year birth cohort, pdik is the fraction of total deaths that are exposed to the ith 5-year birth cohort at age k, HRoverweightk is the hazard ratio of overweight mortality risk to normal weight mortality risk at age k, HRgrade1k is the hazard ratio of grade 1 obesity mortality risk to normal weight mortality risk at age k, and HRgrade23k is the hazard ratio of grade 2/3 obesity mortality risk to normal weight mortality risk at age k. Thus, cohort variation is incorporated through cohorts’ age-specific exposures to obesity, and age variation is incorporated through both exposure and risk. We separately estimated the PAF for White and Black men and women to estimate sex- and race/ethnicity-specific PAFs across age groups in different birth cohorts.
RESULTS
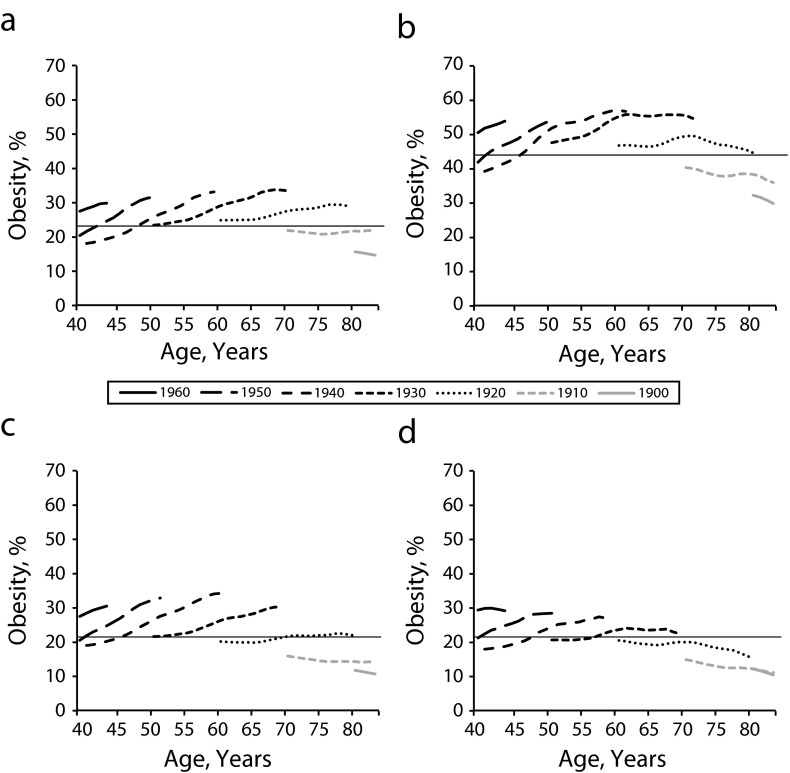
Results indicate substantial cohort variation independent of period change in the likelihood of overweight, grade 1 obesity, and grade 2/3 obesity, which is consistent with existing findings (Table B, available as a supplement to the online version of this article at http://www.ajph.org).9,11 Plots of estimated age-specific obesity prevalence (BMI ≥ 30) by birth cohort illustrate the degree to which obesity rates vary across birth cohorts (Figure 1). Average obesity prevalence between ages 40 and 85 years was 21.4% for both Black and White men, and 43.5% and 23.0% for Black and White women, respectively. Evident in Figure 1 is significant cohort heterogeneity in age-specific obesity rates around these mean values. These changes in US adult obesity rates do not reflect subtle shifts in BMI levels over time.2 Rather, they reflect rapid increases in obesity prevalence among more recent birth cohorts (also see online Figure A available as a supplement to the online version of this article at http://www.ajph.org, for the graph of obesity prevalence plotted with confidence intervals).
FIGURE 1—
Age-specific obesity rates by cohort among (a) White women, (b) Black women, (c) White men, and (d) Black men: National Health Interview Survey Linked Mortality Files, 1986–2004.
Note. Obesity defined as body mass index ≥ 30 kg/m2. Black horizontal line indicates average obesity rate for each subpopulation. Estimated from sample aged ≥ 25 years at the time of the survey.
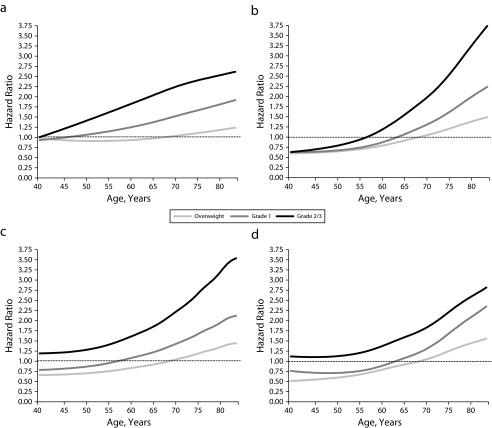
Obesity and Individual-Level Mortality Risk
Results from Royston-Parmar survival models are presented in Tables C and D (available as supplements to the online version of this article at http://www.ajph.org), and estimated hazard ratios are graphically depicted in Figure 2. Results indicate that overweight, grade 1 obesity, and grade 2/3 obesity were all significantly associated with US men’s and women’s adult mortality between 1986 and 2006. The strength of these associations varies significantly by age, sex, and race/ethnicity. Importantly, counter to most extant research, obesity’s effect on mortality risk grows stronger with increasing age. Estimated coefficients of the interactions between the cubic splines and overweight, grade 1 obesity, and grade 2/3 obesity in Tables C and D are statistically significant (also see Figure B available as a supplement to the online version of this article at http://www.ajph.org, for the graph of grade 1 obesity hazard ratios plotted with confidence intervals).
FIGURE 2—
Fitted mortality hazard ratios by body mass index level, race/ethnicity, and sex for (a) White women, (b) Black women, (c) White men, (d) and Black men: National Health Interview Survey Linked Mortality Files, 1986–2004.
Note. Overweight defined as body mass index 25.0–29.9 kg/m2, grade 1 obesity as 30–34.9 kg/m2, and grade 2/3 obesity as ≥ 35 kg/m2.
These age patterns in the obesity–mortality associations became evident only after we controlled for obesity variation in the effect of respondents’ ages-at-survey on mortality risk, suggesting that age-related survey selection strongly influences the estimates of obesity’s effect on age-specific mortality risk.19–22
Percentage of US Deaths Associated With Obesity
We combined estimates of age-specific hazard ratios for overweight and obesity with cohorts’ age-specific rates of overweight, grade 1 obesity, and grade 2/3 obesity and then standardized them by the 2000 age distribution of deaths for US Black and White men and women to estimate the percentage of adult mortality attributable to each BMI level (Table 1).
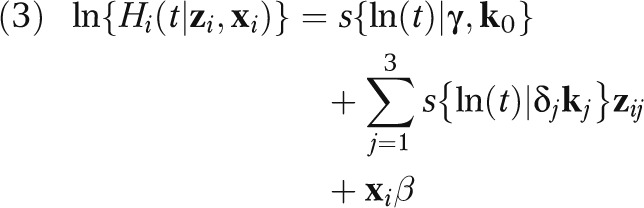
TABLE 1—
Estimated Percentage of US Deaths Between Ages 40.0 and 84.9 Years for Birth Cohorts 1900–1960 Associated With Overweight, Grade 1 Obesity, and Grade 2/3 Obesity: National Health Interview Survey Linked Mortality Files, 1986–2006
| Gender and Race | Overweight, % (95% CI) | Grade 1 Obesity, % (95% CI) | Grade 2/3 Obesity, % (95% CI) | Total, % (95% CI) |
| Black women | 2.5 (–4.7, 10.0) | 9.1 (2.5, 16.2) | 15.2 (9.6, 21.2) | 26.8 (7.3, 47.4) |
| White women | 3.5 (0.2, 6.8) | 10.0 (7.6, 12.5) | 8.2 (6.6, 10.0) | 21.7 (14.4, 29.3) |
| Black men | −1.5 (–7.8, 5.0) | 3.0 (–0.4, 6.9) | 3.5 (1.4, 6.4) | 5.0 (–6.8, 18.3) |
| White men | 3.4 (–0.4, 7.2) | 7.3 (5.2, 9.5) | 4.9 (3.7, 6.2) | 15.6 (8.6, 22.9) |
Note. CI = confidence interval. Overweight defined as body mass index 25.0–29.9 kg/m2, grade 1 obesity as 30–34.9 kg/m2, and grade 2/3 obesity as ≥ 35 kg/m2.
Between 1986 and 2006, we estimate that 5.0% (95% confidence interval [CI] = −6.8, 18.3) of adult deaths among Black men and 15.6% (95% CI = 8.6, 22.9) of deaths among White men were associated with overweight and obese BMI levels. Furthermore, 26.8% (95% CI = 7.3, 47.4) of deaths among Black women and 21.7% (95% CI = 14.4, 29.3) of deaths among White women were associated with overweight and obese BMI levels during this time period. We found the PAF for overweight BMI as a cause of US adult mortality to be significant only for White women, and the combined PAF for overweight and obesity was not significant for Black men (only the PAF for grade 2/3 obesity was significant). When aggregated and standardized by the race/ethnicity and sex distribution of US deaths in year 2000, these results suggest that overweight and obesity were likely responsible for about 18.2% of US Black and White men’s and women’s adult deaths between 1986 and 2006.
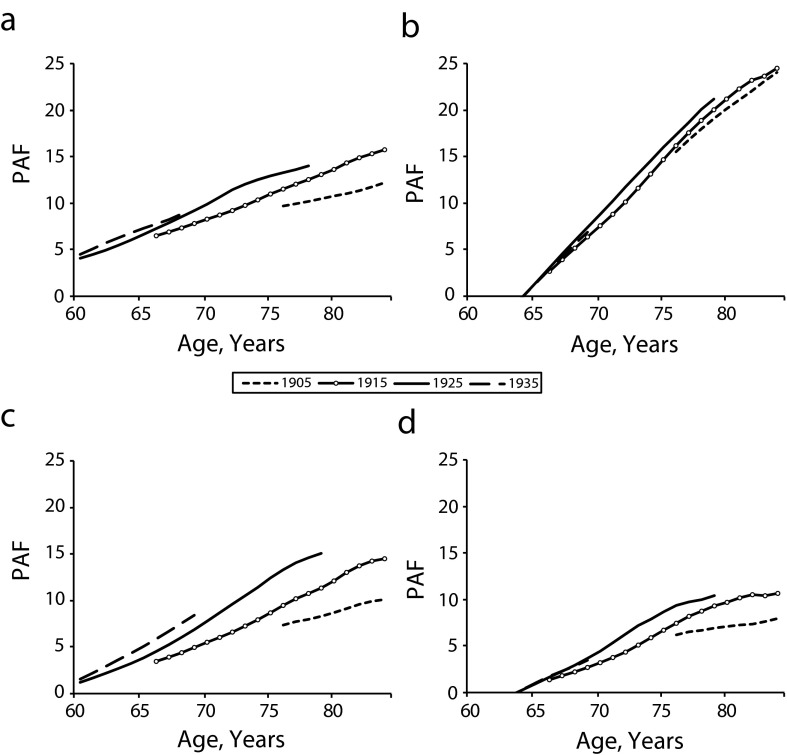
Our estimates of the amount of US adult mortality associated with elevated body mass were higher than those reported in recent studies,5–8,12 and reveal an essential link between mortality and the cohort dimension of the obesity epidemic.11,19,21,22 To illustrate how this “third dimension” of the obesity epidemic shapes the relationship between obesity and US adult mortality levels, Figure 3 presents 5-year birth cohort-specific PAF estimates for high body mass as a cause of death across each cohort’s respective age range among older NHIS respondents, where mortality is most concentrated.
FIGURE 3—
Grade 1 obesity–attributable mortality by age, cohort, race/ethnicity, and sex for (a) White women, (b) Black women, (c) White men, (d) and Black men: National Health Interview Survey Linked Mortality Files, 1986–2004.
Note. PAF = population attributable fraction. Grade 1 obesity defined as body mass index 30–34.9 kg/m2.
Age patterns of PAFs for Black and White men and women show that grade 1 obesity accounts for a rising share of older adult deaths across successive birth cohorts. For instance, estimates suggest that grade 1 obesity accounted for about 3.4% of deaths at age 66 for White men born 1915 to 1919. For White men born 1925 to 1929, however, grade 1 obesity accounted for about 4.5% of deaths at age 66, and for White men born 1935 to 1939, it accounted for about 5.8% of deaths at age 66. These steady rises in PAF for class 1 obesity as a cause of adult mortality reflect more recent cohorts’ greater exposure to obesity across their respective life courses.
DISCUSSION
Recent evidence suggests that researchers ought to account for “three dimensions” of time (age, period of observation, and birth cohort membership) when fitting trend models of population health and mortality.11 To accurately estimate PAFs for obesity as a cause of US mortality, careful consideration must be given to the cohort dimensions of the US obesity epidemic. Consistent with past research, we have shown that the prevalence of US obesity varies not just by age and period of observation, but also by birth cohort membership.9,30 When this fact is included in PAF estimates of obesity as a cause of US adult mortality, the results indicate that obesity has accounted for an increasing share of US deaths in more recent birth cohorts than in earlier birth cohorts.
We have also found evidence consistent with previous research indicating that the effect of high BMI on mortality risk grows significantly stronger with increasing age.22 Although the bulk of existing public health literature has suggested that the association between obesity status and mortality risk is either age-invariable or substantially weakens with increasing age, it has not accounted for some important factors that likely distort the estimates. After we accounted for one prominent factor, namely, age-related survey selection bias, by BMI level we found that the effects of overweight, grade 1 obesity, and grade 2/3 obesity on mortality risk for US men and women grow substantially stronger with age.
Together, our findings add to the obesity–mortality literature in 4 ways: First, we built on recent research by demonstrating the need to use cohort-based prevalence of obesity when estimating the percentage of US mortality attributable to obesity.10,11 Second, we showed substantial age-, period-, cohort-, racial/ethnic-, and sex-based variation in PAF estimates for obesity as a cause of US mortality. Policymakers need to be mindful of the disparate effects obesity has on the health and longevity of different subgroups of the US population, and correspondingly enact appropriate obesity-relevant policies to serve those populations. Third, contrary to prevailing wisdom regarding the effect of the obesity epidemic on US longevity,5–7 our findings revealed that obesity accounted for a large share of US adult mortality in recent decades—about 18% of all deaths between ages 40 and 85 years during the time period 1986 to 2006. Fourth, our study suggests that the cumulative effect of the obesity epidemic on US adult mortality will likely increase in the near future, as younger cohorts with earlier onset and higher prevalence of obesity age across their respective life courses. Although US obesity incidence has slowed in recent years and some evidence suggests it has stalled for some age groups,31 obesity-related goals in Healthy People 2010 were not met and the cohort dimension of the obesity epidemic will likely carry forward the health and mortality implications of the epidemic for many years to come.32
Our findings attend to the complexity of the of the obesity epidemic as it spreads through the population and therein signals that our concern about its population-level health effects should be substantial. The message we deliver stands in sharp contrast to conclusions from some previous research that did not attend to the “third” cohort dimension of the epidemic, and by doing so substantially underestimated the epidemic’s effects on US mortality. The large mortality burden we document suggests that current projections of US life expectancy should be modified to account for the impact of rising obesity prevalence, especially among more recent birth cohorts.10 We believe that it is imperative for the US public and those who construct policy for that public to recognize that population health and more than a century of steady gains in life expectancy are being jeopardized by the obesity epidemic. Indeed, evidence has already implicated high rates of obesity as a significant contributor to the United States’ relatively low life expectancy among high-income countries.33 Addressing this problem will require careful attention to all 3 temporal dimensions of the obesity epidemic, particularly the disconcertingly high prevalence of obesity among today’s younger Americans.
Acknowledgments
We thank the Robert Wood Johnson Foundation Health and Society Scholars program for its financial support.
An earlier version of this work was presented at the Population Association of America’s Annual Meeting; May 3–5, 2012; San Francisco, CA.
We thank Robert A. Hummer for helpful comments on this draft.
Human Participant Protection
No protocol approval was necessary because the data used were made publicly available by the National Center for Health Statistics.
References
- 1.Manson JE, Bassuk SS, Hu FB et al. Estimating the number of deaths due to obesity: can the divergent findings be reconciled? J Womens Health (Larchmt) 2007;16(2):168–176. doi: 10.1089/jwh.2006.0080. [DOI] [PubMed] [Google Scholar]
- 2.Campos P, Saguy A, Ernsberger P, Oliver E, Gaesser G. The epidemiology of overweight and obesity: public health crisis or moral panic? Int J Epidemiol. 2006;35(1):55–60. doi: 10.1093/ije/dyi254. [DOI] [PubMed] [Google Scholar]
- 3.Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282(16):1530–1538. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 4.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 5.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 6.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298(17):2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 7.Mehta NK, Chang VW. Mortality attributable to obesity among middle-aged adults in the United States. Demography. 2009;46(4):851–872. doi: 10.1353/dem.0.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flegal KM, Graubard BI, Williamson DF. Methods of calculating deaths attributable to obesity. Am J Epidemiol. 2004;160(4):331–338. doi: 10.1093/aje/kwh222. [DOI] [PubMed] [Google Scholar]
- 9.Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69(10):1439–1448. doi: 10.1016/j.socscimed.2009.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olshansky SJ, Passaro DJ, Hershow RC et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 11.Reither EN, Olshansky SJ, Yang Y. New forecasting methodology indicates more disease and earlier mortality ahead for today’s younger Americans. Health Aff (Millwood) 2011;30(8):1562–1568. doi: 10.1377/hlthaff.2011.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289(2):187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 13.Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Woods JL. The effect of age on the association between body-mass index and mortality. N Engl J Med. 1998;338(1):1–7. doi: 10.1056/NEJM199801013380101. [DOI] [PubMed] [Google Scholar]
- 14.Kuk JL, Arden CI. Influence of age on the association between various measures of obesity and all-cause mortality. J Am Geriatr Soc. 2009;57(11):2077–2084. doi: 10.1111/j.1532-5415.2009.02486.x. [DOI] [PubMed] [Google Scholar]
- 15.Bender R, Jöckel KH, Trautner C, Spraul M, Berger M. Effect of age on excess mortality in obesity. JAMA. 1999;281(16):1498–1504. doi: 10.1001/jama.281.16.1498. [DOI] [PubMed] [Google Scholar]
- 16.Adams KF, Schatzkin A, Harris TB et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355(8):763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 17.Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obes Rev. 2007;8(1):41–59. doi: 10.1111/j.1467-789X.2006.00248.x. [DOI] [PubMed] [Google Scholar]
- 18.Al Snih S, Ottencacher KJ, Markides KS, Kuo YF, Eschbach K, Goodwin JS. The effect of obesity on disability vs. mortality in older Americans. Arch Intern Med. 2007;167(8):774–780. doi: 10.1001/archinte.167.8.774. [DOI] [PubMed] [Google Scholar]
- 19.Yu Y. Reexamining the declining effect of age on mortality differentials associated with excess body mass: evidence of cohort distortions in the United States. Am J Public Health. 2012;102(5):915–922. doi: 10.2105/AJPH.2011.300237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Medes de Leon CF. Aging and the elapse of time: a comment on the analysis of change. J Gerontol. 2007;62B(3):S198–S202. doi: 10.1093/geronb/62.3.s198. [DOI] [PubMed] [Google Scholar]
- 21.Abdullah A, Wolfe R, Stoelwinder JU et al. The number of years lived with obesity and the risk of all-cause and cause-specific mortality. Int J Epidemiol. 2011;40(4):985–996. doi: 10.1093/ije/dyr018. [DOI] [PubMed] [Google Scholar]
- 22.Masters RK, Powers DA, Link BG. Obesity and mortality risk across the adult life course. Am J Epidemiol. 2013;177(5):431–442. doi: 10.1093/aje/kws325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics, Office of Analysis and Epidemiology. National Health Interview Survey (1986–2004) linked mortality files: analytic guidelines. 2010. Available at: http://www.cdc.gov/nchs/data_access/data_linkage/mortality/nhis_linkage.htm#description. Accessed May 30, 2013.
- 24.Willet WC, Hu FB, Colditz GA, Manson JE. Underweight, overweight, obesity, and excess deaths. JAMA. 2005;294(5):551. doi: 10.1001/jama.294.5.551-a. [DOI] [PubMed] [Google Scholar]
- 25.Reither EN, Utz RL. A procedure to correct proxy-reported weight in the National Health Interview Survey, 1976–2002. Popul Health Metr. 2009;7:2. doi: 10.1186/1478-7954-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reither EN. Why Are Our Waistlines Expanding? Age-Period-Cohort Analyses of the Obesity Epidemic and a Critical Examination of Mass Preparation Theory [PhD dissertation] Madison, WI: Department of Sociology, University of Wisconsin–Madison; 2005. [Google Scholar]
- 27.Yang Y, Land K. Age-period-cohort analysis of repeated cross-section surveys: fixed or random effects? Sociol Methods Res. 2008;36(3):297–326. [Google Scholar]
- 28.Thiébaut ACM, Bénichou J. Choice of time-scale in Cox’s model analysis of epidemiologic cohort data: a simulation study. Stat Med. 2004;23(24):3803–3820. doi: 10.1002/sim.2098. [DOI] [PubMed] [Google Scholar]
- 29.Royston P, Lambert PC. Flexible Parametric Survival Analysis Using Stata: Beyond the Cox Model. College Station, TX: Stata Press; 2011. [Google Scholar]
- 30.Keyes KM, Utz RL, Robinson W, Li G. What is a cohort effect? Comparison of three statistical methods for modeling cohort effects in obesity prevalence in the United States, 1971–2006. Soc Sci Med. 2010;70(7):1100–1108. doi: 10.1016/j.socscimed.2009.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of Obesity in the United States, 2009–2010. Hyattsville, MD: National Center for Health Statistics; 2012. NCHS Data Brief No. 82. [Google Scholar]
- 32.Healthy People 2010 Final Review. Hyattsville, MD: National Center for Health Statistics; 2012. [Google Scholar]
- 33.Preston SH, Stokes A. Contribution of obesity to international differences in life expectancy. Am J Public Health. 2011;101(11):2137–2143. doi: 10.2105/AJPH.2011.300219. [DOI] [PMC free article] [PubMed] [Google Scholar]