Abstract
Objectives. We estimated the prevalence and incidence of gender identity disorder (GID) diagnoses among veterans in the Veterans Health Administration (VHA) health care system and examined suicide risk among veterans with a GID diagnosis.
Methods. We examined VHA electronic medical records from 2000 through 2011 for 2 official ICD-9 diagnosis codes that indicate transgender status. We generated annual period prevalence estimates and calculated incidence using the prevalence of GID at 2000 as the baseline year. We cross-referenced GID cases with available data (2009–2011) of suicide-related events among all VHA users to examine suicide risk.
Results. GID prevalence in the VHA is higher (22.9/100 000 persons) than are previous estimates of GID in the general US population (4.3/100 000 persons). The rate of suicide-related events among GID-diagnosed VHA veterans was more than 20 times higher than were rates for the general VHA population.
Conclusions. The prevalence of GID diagnosis nearly doubled over 10 years among VHA veterans. Research is needed to examine suicide risk among transgender veterans and how their VHA utilization may be enhanced by new VA initiatives on transgender care.
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) defines gender identity disorder (GID) as having deeply rooted feelings of persistent discomfort with one’s current biological gender and having the desire to be of the opposite gender to the extent that “the disturbance causes clinically significant distress or impairment in … important areas of functioning.”1(p260)
Although the diagnosis is relatively rare, persons diagnosed with GID constitute a subpopulation of people who experience numerous disparities in physical and mental health as well as health care access.2 Although a precise estimate of GID occurrence among the general population is unknown, one theoretical framework (i.e., flight into hypermasculinity) posits that GID may be overrepresented in the military and among veterans,3 and there is support for this hypothesis in community-based samples of transgender persons in which high prevalence of military service is observed.4 Furthermore, there is evidence of elevated risk for suicidal behavior among transgender populations.5–10 However, prevalence of GID and suicide-related events (e.g., suicide planning, suicide attempt) have yet to be examined among veterans who have received Veterans Health Administration (VHA) services. We have addressed this unmet need.
GENDER IDENTITY DISORDER TERMINOLOGY
Although there are multiple ways that a person diagnosed with GID may self-identify, the 2 common terms used in the literature for this self-identification are transgender and transsexual. Transgender is a term with broader scope; it typically encompasses individuals who self-identify as being or living outside socially constructed gender roles of masculinity and femininity. Transsexual is often used to conceptualize a subset of transgender persons who usually desire to undergo physical changes to their bodies, potentially including cross-gender hormone treatments and gender reassignment surgery.11
Because the data for our analysis did not permit an assessment of self-identified transgender or transsexual status, we have used the terms GID, transgender, and transsexual interchangeably, and our review of the literature includes findings of studies with GID, transgender, and transsexual samples. Although these populations share many qualities, we duly note that persons with GID constitute only a portion of transgender and transsexual communities. Thus, our focus on persons diagnosed with GID (i.e., a clinical subpopulation) should not be misinterpreted to represent either transgender or transsexual populations at large.
Currently, the most common treatments for GID are combinations of psychotherapy, cross-gender hormone therapy, living full time in the cross-gender role, electrolysis, voice therapy, and surgical procedures.12–14
PREVALENCE OF GENDER IDENTITY DISORDER
Precise estimates of the number of persons with GID are difficult to make, as not every person with GID is able to access care from a health care provider who is knowledgeable in this diagnosis.5,15,16 Moreover, many studies of GID use records of gender reassignment surgeries as a proxy census (i.e., counting only transsexuals with severe forms of GID),17 which likely produces underestimates of GID prevalence, as only a small fraction of GID-diagnosed individuals undergoes gender reassignment surgeries.18
The DSM-IV estimates that 1 in 30 000 natal males and 1 in 100 000 natal females have GID among the US population; however, these figures are based on older, limited data.1 More recent research, from other countries, reports that GID may be more common,19 ranging from approximately 1 in 13 000 natal males and 1 in 34 000 females in Belgium20 to 1 in 11 000 natal males and 1 in 20 000 natal females in the Netherlands.21 Although more precise estimates of population prevalence are unavailable, trends across studies suggest that GID is more common among natal males than among natal females,19 with a prevalence ratio of 3 natal males with GID to every 1 natal female with GID.17
SUICIDE RISK DISPARITIES
Research on GID-diagnosed, transgender, and transsexual populations is sparse, and no national-level health surveillance survey currently collects information that can be used to reliably identify these populations. The literature suggests that people diagnosed with GID may experience a significantly elevated risk for suicide. For example, a study of more than 300 transgender persons in Virginia documented that 65% had lifetime suicidal ideation.6 Similarly, a study of 70 US military veterans, most self-referred for a gender evaluation, found that 61% reported lifetime suicidal ideation.7 These estimates are much higher than the estimated 8.4% prevalence of lifetime suicidal ideation among the general adult US population.22 Elevated suicidal ideation has similarly been found among other samples of transgender persons in the United States.5,8–10
Research also suggests that attempted suicide is disproportionately higher among transgender populations. In a needs assessment of nearly 200 transgender persons in Philadelphia, Pennsylvania, nearly one third (30.1%) reported at least 1 lifetime suicide attempt.5 Clements-Nolle et al. also noted that roughly a third (32.2%) in their sample of more than 500 transgender respondents reported a lifetime suicide attempt.23 Other studies report a lifetime suicide attempt prevalence ranging from 18% to 41%.6,24–27 By comparison, less than 3% of the general US population report a lifetime suicide attempt.22
Relative to data about suicide ideation and attempt, information about suicide among persons with GID is perhaps the most limited, with the only known estimates derived from surveillance in the Netherlands. In a retrospective study of more than 1400 transsexual outpatients from that country’s largest clinic providing transsexual health care, van Kesteren et al. noted substantially higher death by suicide among transsexual patients than among the age- and gender-corresponding general Dutch population rates (standardized mortality ratio [SMR] = 9.29; 95% CI = 4.94, 15.88).28 In a recent follow-up study of outpatients from the same clinic in July 1997, the authors still found elevated rates of death from suicide, although they were not as pronounced as in their earlier findings (SMR = 5.70; 95% CI = 4.93, 6.54).29 More recent studies among transsexual persons in Sweden report a similar elevated risk of suicide.30 To our knowledge, no empirical investigation has examined similar rates of suicide mortality among US populations of persons with GID or who identify as either transgender or transsexual.
GENDER IDENTITY DISORDER AND VETERANS
There is a theoretical basis, informed by clinical case analysis, for the suggestion that the prevalence of GID may be disproportionately higher among persons with military service histories than among the general population. Based on a case series, Brown developed a flight into hypermasculinity theory, asserting that young men with GID may enlist in the military at critical periods in their psychosocial development to “become real men” or to purge their inner gender conflict through the strict rigor and focus on overtly masculine activities (e.g., weaponry training, physical training, combat).3
Supplementing Brown’s theoretical framework is the fact that more than 95% of the VHA system’s patients are male31; GID is suspected to occur with more frequency among natal males.1 In a community-based sample of 141 transgender individuals, Shipherd et al. found that veteran status was endorsed at 3 times what is observed in the general population, and VHA use was elevated among transgender veterans (16.3% in the past 6 months) relative to general rates of VHA use (annual 6.2%–15.8%).4 Furthermore, in June 2011, the VHA issued a new directive outlining health care for transgender and intersex veterans, which may have increased the willingness of transgender veterans to seek VHA care.
Thus, we first sought to document the prevalence of official diagnoses of GID within the VHA health care system. Second, because of evidence of greater risk for suicide attempt among transgender populations, we also examined suicide-related events among VHA-utilizing veterans with a diagnosis of GID.
METHODS
The VHA is the single largest integrated system for health care in the United States, annually serving more than 8 million veterans.32 Because the VHA has a national system of standardized electronic medical records,33 we employed a review of both inpatient and outpatient electronic patient treatment files from fiscal year (FY)2000 through FY2011. We specified inclusion criteria for a GID case as being a patient with an ICD-9 diagnosis code of either 302.85 (gender identity disorder in adolescents or adults; i.e., GID) or 302.6 (gender identity disorder not otherwise specified; i.e., GID-NOS) recorded during any inpatient stay or outpatient encounter or visit. We counted a patient with a GID diagnosis only once, and the first notation of the GID diagnosis in the patient treatment files indicated the FY in which said patient would be counted. We generated period prevalence estimates for each FY by dividing the number of unique GID diagnoses in that FY by the total number of patients seen in that calendar year. FYs start October 1 and end September 30. For example, FY2011 started October 1, 2010, and ended September 30, 2011.
Although there is prevalence of GID diagnoses beginning in FY2000, the VHA patient data were not obtainable for FY2000 or FY2001; thus, we could not calculate any period prevalence or incidence proportions of GID diagnoses for those years. Beginning in FY2002, we calculated incidence estimates using the prevalence of GID at FY2000 as the baseline for assessing new, unique cases of GID. An additional conservative assumption in annual incidence calculations was omitting the cumulative extant cases of GID from the population at risk (i.e., the denominator) for each year, which assumes that a patient diagnosed with GID stayed in VHA care throughout the observed period and thus needed to be removed from the denominator of people at risk. For example, we subtracted the total new GID cases documented in both FY2000 and FY2001 from the FY2002 denominator for calculation of the most conservative FY2002 incidence.
It is important to note that although the vast majority of VHA users are veterans, the cohort of VHA users also includes some nonveterans (i.e., veterans’ family members). We reviewed inpatient and outpatient files for the unique cases of GID for variables specifically identifying that person as a nonveteran. Overall, the numbers of nonveteran VHA users with GID was extremely small in each year, ranging from a low of zero in FY2005 through FY2007 to a high of 5 in FY2000. Because of the small number of nonveteran cases, we kept all identified cases.
We examined past year suicide-related event prevalence by cross-referencing all GID cases with the VHA’s Suicide Prevention Application Network (SPAN) database. SPAN is a database of information about suicide-related behaviors reported by the national network of suicide prevention coordinators situated in every VHA medical center and large outpatient facility. We did not include suicide deaths among the outcomes. Suicide-related events include suicide-related behaviors recorded by the suicide prevention coordinators (e.g., interrupted suicide attempts, gestures with a firearm, suicide plans). Because the suicide prevention coordinators focus on behaviors, suicidal ideation is not a recorded outcome in SPAN. Furthermore, although SPAN does contain data on suicide deaths, the local reporting of deaths (i.e., from coroners or medical examiners) is not mandatory and is not considered complete. Thus all outcomes from SPAN used only nonfatal events.
We cross-referenced GID cases from available years of data from SPAN (i.e., FY2009–2011) for at least 1 suicide-related event noted in each year; we counted persons with multiple events in 1 year only once. To generate prevalence of suicide events, we divided the number of GID cases with at least 1 report of a suicide-related event for each year by the cumulative data of GID diagnoses in that particular year.
RESULTS
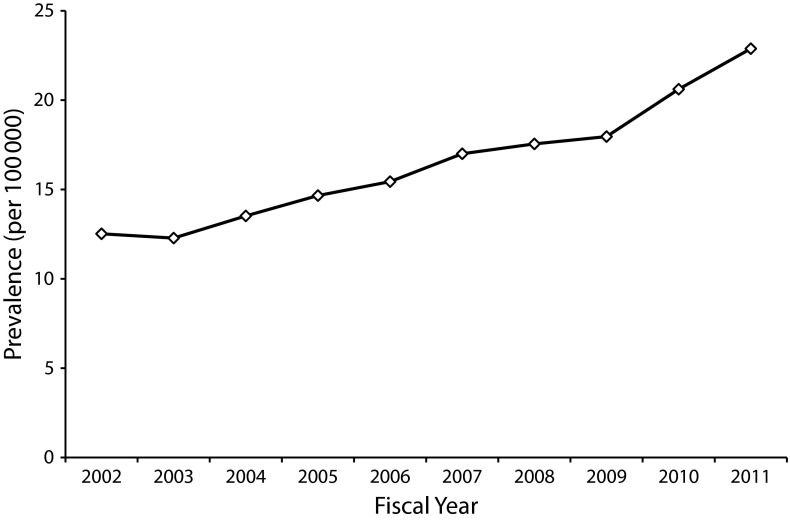
Across the analytic period of FY2000–FY2011, 3177 unique persons had at least 1 diagnosis of GID in their files. Prevalence calculations suggest an increasing trend of GID in the VHA (Figure 1). Although we could not calculate estimates for FY2000–FY2001 because of a lack of data on the VHA cohort of patients, beginning with FY2002 data, we noted a baseline prevalence of 12.52 per 100 000.
FIGURE 1—
Prevalence of GID diagnoses by fiscal year: United States, 2000–2011.
Note. GID = gender identity disorder.
The prevalence of GID among VHA users has nearly doubled over the 10-year period we examined, whereas the incidence has been relatively stable (Table 1). Beginning in FY2000, new cases have been identified in the VHA at an average rate of 246 cases per year, whereas some previously identified veterans with GID continue to use VHA care, resulting in a near doubling of the prevalence of GID diagnoses in the VHA. All 3 past year prevalence estimates of suicide-related events, ranging from 4000 per 100 000 to 5000 per 100 000, were much higher than are any currently available general population metric of past year suicidal behavior (Table 2).
TABLE 1—
Prevalence and Incidence of GID Diagnoses by Fiscal Year: United States, 2000–2011
| Fiscal Year | Total New GID Diagnoses, No. | Total GID Diagnoses, No. | Total VHA Patients, No. | Period Prevalencea | Incidencea |
| 2000 | 472b | 472 | … | … | … |
| 2001 | 261 | 475 | … | … | … |
| 2002 | 283 | 569 | 4 544 353 | 12.52 | 6.23 |
| 2003 | 228 | 590 | 4 805 421 | 12.28 | 4.74 |
| 2004 | 235 | 673 | 4 977 772 | 13.52 | 4.72 |
| 2005 | 214 | 747 | 5 094 425 | 14.66 | 4.20 |
| 2006 | 196 | 801 | 5 188 825 | 15.44 | 3.78 |
| 2007 | 209 | 889 | 5 230 122 | 17.00 | 4.00 |
| 2008 | 203 | 930 | 5 299 645 | 17.55 | 3.83 |
| 2009 | 230 | 979 | 5 448 058 | 17.96 | 4.22 |
| 2010 | 285 | 1162 | 5 638 263 | 20.61 | 5.06 |
| 2011 | 361 | 1326 | 5 795 165 | 22.88 | 6.23 |
Note. GID = gender identity disorder; VHA = Veterans Health Administration. Prevalence = total GID diagnoses/total VHA patients; incidence = total new GID diagnoses/total VHA patients in previous years’ diagnoses.
Per 100 000 patients.
Used as baseline although formal diagnosis may have occurred before fiscal year 2000.
TABLE 2—
Suicide-Related Event Prevalence Among GID-Diagnosed Veterans by Fiscal Year: United States, 2000–2011
| Fiscal Year | GID Patients With ≥ 1 Suicide-Related Events | Total GID Patients | Period Prevalence of Suicide-Related Eventsa |
| 2009 | 40 | 979 | 4085.80 |
| 2010 | 49 | 1162 | 4216.87 |
| 2011 | 68 | 1326 | 5128.21 |
Note. GID = gender identity disorder.
Per 100 000 patients.
DISCUSSION
To our knowledge this is the largest study of a transgender population to date in the United States, and our findings indicate a much higher prevalence of GID among VHA veterans than what has been reported previously in the literature,19 lending support to Brown’s flight into hypermasculinity theory within military populations. Specifically, in FY2011, 22.9 per 100 000 VHA users had a diagnosis of GID, which is more than 5 times the DSM-IV prevalence estimate of GID in the general US population (4.3/100 000 persons). The results showed a relatively stable annual incident rate of 246 new diagnoses of GID, contributing to an increasing prevalence of VHA veterans with GID.
Why the prevalence of GID among this veteran population is higher than is that in the general population is beyond the scope of our study; several areas of future research are needed to better qualify these results. For instance, the estimate of GID from the DSM is based on older studies and may not accurately reflect the current prevalence of GID. Furthermore, because GID is more prevalent among natal males than among natal females, the VHA may see a disproportionately high prevalence because the majority of its patients are males. Reports of GID diagnoses from other large health systems in the United States would aid in examining how results from patients enrolled in different health systems (e.g., 1 not solely composed of those eligible for VHA benefits) compare with our findings and thus help to better understand the current prevalence of GID.
On the basis of simple de-identified counts, it is unclear whether these veterans continued to seek care over time in the VHA once diagnosed. The existence of transgender veterans poses many additional questions, such as what types of care are most utilized among this population. Preliminary studies suggest that transgender veterans are likely to seek both medical and mental health care at VHA facilities.4 Utilization and quality of care are particularly salient questions since the VHA announced its first ever directive outlining health care provision to transgender and intersex veterans in June 2011, and there have been documented problems in accessing care for transgender persons.34 Consequently, there may be historical effects in the trends of GID diagnoses in the time before and after the issuance of the directive. In addition to utilization, future research is needed to examine other facets of health, including comorbidities and sources of mortality.
Suicide is a particular concern for this population. Results show that suicide-related events occur at significantly elevated rates among this population, which corroborates results from other transgender samples.8–10,26,27 Estimates for each year—ranging from 4000 per 100 000 to 5000 per 100 000—were well above any general population metric related to suicidal behavior. For example, general population data available from the Centers for Disease Control and Prevention Web-based Injury Statistics Query and Reporting System indicate a past year crude rate of self-harm injuries of 150.61 per 100 000 in the year 2010.35 Among VHA veterans in general, the rate of suicide-related events in FY2010 was approximately 202 per 100 000 patients,36 which makes the FY2010 rate among veterans with GID more than 20 times higher.
A recent World Health Organization multinational report of past-year suicidal behavior noted that approximately 2.0% of adults reported suicidal ideation, 0.6% reported suicide planning, and 0.3% reported a suicide attempt.37 By contrast, estimates of unique suicide-related events among veterans with GID using VHA care ranged from 4.1% to 5.1%. Although comparisons are illustrative and studies strive to measure similar overarching constructs of suicide risk, exact definitions and measures of suicidal behavior differ, making direct comparison impossible. Moreover, it is unclear whether transgender veterans may have higher or lower burden of suicide risk compared with their transgender nonveteran peers, as veterans may carry unique experiences that are associated with suicide risk, such as combat exposure and traumatic brain injury.38–40 Nor is it clear how this population of veterans with GID diagnoses compares with the larger population of transgender veterans who do not meet criteria for GID or GID-NOS.
The burden of suicide risk among this population clearly warrants more attention regarding etiology, prevention, and intervention. For example, high rates of early life trauma among transgender persons (e.g., childhood maltreatment, peer victimization)24,34,41,42 may contribute to the risk of suicide, but it is unclear how and whether trauma from military service interacts with previous trauma. In terms of prevention and because of the extremely high prevalence of suicide-related behavior among this sample of transgender veterans, more research is needed to examine whether suicide prevention campaigns and services are reaching or being utilized by this population.43–45
Limitations
Several limitations of this study must be noted. First, although we have reported a census sample of all GID diagnoses in VHA medical records from FY2000 through FY2011, the specialized nature of this subpopulation (i.e., clinically diagnosed veterans) limits generalizability.
Second, the study period was before the VHA’s June 2011 directive outlining health care for transgender veterans. Thus, the census of GID diagnoses may be an underestimate because transgender veterans may have felt uncomfortable seeking care from the VHA before the issuance of the directive. For instance, before the national directive a few localized VHA policies prevented access to specific types of care (i.e., cross-gender hormones) for veterans with GID, which may have resulted in veterans seeking care elsewhere.
Third, we were unable to assess for misclassification bias through potential mistaken diagnosis codes in the patient treatment files.
Fourth, we employed a definition of transgender status limited to clinical diagnoses, which may have missed persons without clinical diagnoses of GID who self-identify as transgender but may have included persons with GID who do not self-identify as transgender. Finally, although SPAN is currently the largest registry of suicide-related events in the United States, it may not capture all events and has operated only since 2008; thus, it is likely an underestimate of suicide risk for this population.
Conclusions
As research continues to develop, the VHA has taken steps to improve health care outcomes for transgender veterans since issuing the transgender health care directive.46 Activities included system-wide communications and development of resources about transgender health care and a series of national virtual meetings for VHA clinical staff on conducting evaluations for hormone therapy, prescribing cross-gender hormones, and providing an integrated care approach for transgender veterans. Plans are underway to produce a web-based continuing education program on transgender health care for new clinical staff and to establish formal clinical consultation services on culturally appropriate transgender care. These efforts are supported by recent joint commission guidelines that require accredited facilities to eliminate discriminatory policies and procedures and provide staff training on culturally and clinically appropriate care for lesbian, gay, bisexual, and transgender individuals.47
This report contributes to a small but growing body of literature about transgender health and is a first step in exploring the unique health needs of GID-diagnosed veterans within the VHA. Transgender persons experience many barriers in seeking and access to health care,4,5,34 but these issues have not been explored fully among transgender persons within the VHA, which is the nation’s largest integrated health care system.
Several questions remain about the transgender veteran population, the most pressing of which includes addressing the unusually high burden of suicidal behavior and finding ways of identifying transgender populations beyond the sole use of diagnosis codes. More nuanced future examinations could also contribute to a better understanding about subgroups within the transgender veteran population. The VHA has made recent progress by issuing a directive outlining clinical care guidelines for transgender veterans and providing training to staff, but there is still much to learn about this veteran population’s health care utilization and epidemiology of health issues.
Acknowledgments
This work was partially supported by the Department of Veterans Affairs VISN-2 Center of Excellence for Suicide Prevention and by a postdoctoral fellowship in an Institutional National Research Service Award from the National Institute of Mental Health (award 5T32MH02006112 to J. R. B.).
Note. The opinions expressed in this work are the authors’ and do not reflect those of the funding institutions, the US Department of Veterans Affairs, or the US Government.
Human Participant Protection
This project was approved by the institutional review board of the Veterans Affairs Medical Center-Syracuse, NY.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: 2000. [Google Scholar]
- 2.Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001;91(6):915–921. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown G. Transsexuals in the military: flight to hypermasculinity. Arch Sex Behav. 1988;17(6):527–537. doi: 10.1007/BF01542340. [DOI] [PubMed] [Google Scholar]
- 4.Shipherd JC, Mizock L, Maguen S, Green K. Male-to-female transgender veterans and VA health care utilization. Int J Sex Health. 2012;24(1):78–87. [Google Scholar]
- 5.Kenagy GP. Transgender health: findings from two needs assessment studies in Philadelphia. Health Soc Work. 2005;30(1):19–26. doi: 10.1093/hsw/30.1.19. [DOI] [PubMed] [Google Scholar]
- 6.Xavier J, Honnold JA, Bradford J. The Health, Health-Related Needs, and Lifecourse Experiences of Transgender Virginians. Richmond, VA: Virginia Department of Health; 2007. [Google Scholar]
- 7.McDuffie E, Brown G. 70 US veterans with gender identity disturbances: a descriptive study. Int J Transgenderism. 2010;12 1, 21–30. [Google Scholar]
- 8.Mathy R. Transgender identity and suicidality in a nonclinical sample: sexual orientation, psychiatric history, and compulsive behaviors. J Psychol Human Sex. 2002;14(4):47–65. [Google Scholar]
- 9.Xavier J, Bobbin M, Singer B, Budd E. A needs assessment of transgendered people of color living in Washington, DC. Int J Transgenderism. 2005;8(2–3):31–47. [Google Scholar]
- 10.Kenagy G, Bostwick W. Health and social service needs of transgender people in Chicago. Int J Transgenderism. 2005;8(2–3):57–66. [Google Scholar]
- 11.Lombardi EL. Enhancing transgender health care. Am J Public Health. 2001;91(6):869–872. doi: 10.2105/ajph.91.6.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levine SB, Brown GR, Coleman E et al. The standards of care for gender identity disorders. J Psychol Human Sex. 1999;11(2):1–34. [Google Scholar]
- 13.Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People, Version 7. Minneapolis, MN: World Professional Association for Transgender Health; 2011. [Google Scholar]
- 14.King RS, Brown GR, McCrea CR. Voice parameters that result in identification or misidentification of biological gender in male-to-female transgender veterans. Int J Transgenderism. 2012;13(3):117–130. [Google Scholar]
- 15.Sanchez NF, Sanchez JP, Danoff A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. Am J Public Health. 2009;99(4):713–719. doi: 10.2105/AJPH.2007.132035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sperber J, Landers S, Lawrence S. Access to health care for transgendered persons: results of a needs assessment in Boston. Int J Transgenderism. 2005;8(2–3):75–91. [Google Scholar]
- 17.Landén M, Wålinder J, Lundström B. Prevalence, incidence and sex ratio of transsexualism. Acta Psychiatr Scand. 1996;93(4):221–223. doi: 10.1111/j.1600-0447.1996.tb10638.x. [DOI] [PubMed] [Google Scholar]
- 18.Cohen-Kettenis PT, Gooren L. Transsexualism: a review of etiology, diagnosis and treatment. J Psychosom Res. 1999;46(4):315–333. doi: 10.1016/s0022-3999(98)00085-3. [DOI] [PubMed] [Google Scholar]
- 19.Zucker K, Lawrence A. Epidemiology of gender identity disorder: recommendations for the Standards of Care of the World Professional Association for Transgender Health. Int J Transgenderism. 2009;11(1):8–18. [Google Scholar]
- 20.De Cuypere G, van Hemellrijck M, Michel A et al. Prevalence and demography of transsexualism in Belgium. Eur Psychiatry. 2007;22(3):137–141. doi: 10.1016/j.eurpsy.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Bakker A, van Kesteren PJM, Gooren L, Bezemer P. The prevalence of transsexualism in the Netherlands. Acta Psychiatr Scand. 1993;87(4):237–238. doi: 10.1111/j.1600-0447.1993.tb03364.x. [DOI] [PubMed] [Google Scholar]
- 22.Baca-Garcia E, Perez-Rodriguez MM, Keyes KM et al. Suicidal ideation and suicide attempts in the United States: 1991–1992 and 2001–2002. Mol Psychiatry. 2010;15(3):250–259. doi: 10.1038/mp.2008.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: the influence of gender-based discrimination and victimization. J Homosex. 2006;51(3):53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- 24.Grossman AH, D’Augelli AR. Transgender youth and life-threatening behaviors. Suicide Life Threat Behav. 2007;37(5):527–537. doi: 10.1521/suli.2007.37.5.527. [DOI] [PubMed] [Google Scholar]
- 25.Maguen S, Shipherd JC. Suicide risk among transgender individuals. Psychol Sex. 2010;1(1):34–43. [Google Scholar]
- 26.Grant JM, Mottet LA, Tanis J, Herman JL, Harrison J, Keisling M. National Transgender Discrimination Survey Report on Health and Health Care. Washington, DC: National Center for Transgender Equality and the National Gay and Lesbian Task Force; 2010. [Google Scholar]
- 27.Terada S, Matsumoto Y, Sato T, Okabe N, Kishimoto Y, Uchitomi Y. Suicidal ideation among patients with gender identity disorder. Psychiatry Res. 2011;190(1):159–162. doi: 10.1016/j.psychres.2011.04.024. [DOI] [PubMed] [Google Scholar]
- 28.van Kesteren PJM, Asscheman H, Megens JAJ, Gooren L. Mortality and morbidity in transsexual subjects treated with cross-sex hormones. Clin Endocrinol (Oxf) 1997;47(3):337–342. doi: 10.1046/j.1365-2265.1997.2601068.x. [DOI] [PubMed] [Google Scholar]
- 29.Asscheman H, Giltay EJ, Megens JA, de Ronde W, van Trotsenburg MA, Gooren LJ. A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol. 2011;164(4):635–642. doi: 10.1530/EJE-10-1038. [DOI] [PubMed] [Google Scholar]
- 30.Dhejne C, Lichtenstein P, Boman M, Johansson ALV, Långström N, Landén M. Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS ONE. 2011;6(2):e16885. doi: 10.1371/journal.pone.0016885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frayne SM, Yano EM, Nguyen VQ et al. Gender disparities in Veterans Health Administration care. Med Care. 2008;46(5):549–553. doi: 10.1097/MLR.0b013e3181608115. [DOI] [PubMed] [Google Scholar]
- 32.US Department of Veterans Affairs. About VHA. 2011 Available at: http://www.va.gov/health/aboutVHA.asp#datasource. Accessed January 26, 2012. [Google Scholar]
- 33.Jha AK, DesRoches CM, Campbell EG et al. Use of electronic health records in US Hospitals. N Engl J Med. 2009;360(16):1628–1638. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 34.Shipherd JC, Green K, Abramovitz SM. Transgender clients: identifying and minimizing barriers to mental health treatment. J Gay Lesbian Ment Health. 2010;14(2):94–108. [Google Scholar]
- 35.Centers for Disease Control and Prevention. Injury prevention & control: data & statistics (WISQARS) 2011 Available at: http://www.cdc.gov/injury/wisqars/index.html. Accessed January 11, 2012. [Google Scholar]
- 36.US Department of Veterans Affairs. Fact Sheet: VA Suicide Prevention Program Facts About Veteran Suicide. Washington, DC: Office of Patient Care Services; Office of Mental Health Services; 2011. [Google Scholar]
- 37.Borges G, Nock MK, Haro Abad JM et al. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry. 2010;71(12):1617–1628. doi: 10.4088/JCP.08m04967blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kemp JE, Bossarte R. Suicide Data Report, 2012. Washington, DC: Department of Veterans Affairs; 2013. [Google Scholar]
- 39.Prigerson HG, Maciejewski PK, Rosenheck RA. Population attributable fractions of psychiatric disorders and behavioral outcomes associated with combat exposure among U.S. men. Am J Public Health. 2002;92(1):59–63. doi: 10.2105/ajph.92.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maguen S, Luxton DD, Skopp NA et al. Killing in combat, mental health symptoms, and suicidal ideation in Iraq war veterans. J Anxiety Disord. 2011;25(4):563–567. doi: 10.1016/j.janxdis.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Shipherd JC, Maguen S, Skidmore WC, Abramovitz SM. Potentially traumatic events in a transgender sample. Traumatology. 2011;17(2):56–67. [Google Scholar]
- 42.Drescher J, Byne W. Gender dysphoric/gender variant (GD/GV) children and adolescents: summarizing what we know and what we have yet to learn. J Homosex. 2012;59(3):501–510. doi: 10.1080/00918369.2012.653317. [DOI] [PubMed] [Google Scholar]
- 43.Katz IR, Kemp JE, Blow FC, McCarthy JF, Bossarte R. Changes in suicide rates and in mental health staffing in the Veterans Health Administration, 2005. Psychiatr Serv. 2013;64(7):620–625. doi: 10.1176/appi.ps.201200253. [DOI] [PubMed] [Google Scholar]
- 44.Kemp JE, Bossarte R. Surveillance of suicide and suicide attempts among veterans: address a national imperative. Am J Public Health. 2012;102(suppl 1):e4–e5. doi: 10.2105/AJPH.2012.300652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Katz I. Lessons learned from mental health enhancement and suicide prevention activities in the Veterans Health Administration. Am J Public Health. 2012;102(suppl 1):S14–S16. doi: 10.2105/AJPH.2011.300582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Blosnich JR, Bossarte RM, Silenzio VM. Suicidal ideation among sexual minority veterans: results from the 2005–2010 Massachusetts Behavioral Risk Factor Surveillance Survey. Am J Public Health. 2012;102(suppl 1):S44–S47. doi: 10.2105/AJPH.2011.300565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community: A Field Guide. Oak Brook, IL: The Joint Commission; 2011. [Google Scholar]