Abstract
Background
Anal cancer is one of the most common cancers affecting human immunodeficiency virus (HIV)-infected male patients. Currently, there is no consensus on post-treatment surveillance of HIV-infected men who have sex with men (MSM) who have been treated for high-grade intraepithelial neoplasia (HGAIN), the likely precursor to anal cancer.
Objective
To assess the cost-effectiveness of a range of strategies for anal cancer surveillance in HIV-infected MSM previously treated for HGAIN.
Methods
We developed a Markov model to project quality-adjusted life expectancy (QALE), lifetime costs, and the incremental cost-effectiveness ratios (ICER) of five strategies using high resolution anoscopy (HRA) and/or anal cytology testing after treatment.
Results
Performing HRA alone at 6- and 12-month visits was associated with a cost-effectiveness ratio of $4,446 per QALY gained. In comparison, combined HRA and anal cytology at both visits provided the greater health benefit at a cost of $ 17,373 per QALY gained. Our results were robust over a number of scenarios and assumptions, including patients’ level of immunosuppression. Results were most sensitive to test characteristics and cost, and progression rates of normal to HGAIN and HGAIN to cancer.
Conclusions
Our results suggest that combined HRA and anal cytology at 6 and 12 months may be a cost-effective surveillance strategy following treatment of HGAIN in HIV-infected MSM.
Keywords: HIV/AIDS, HPV, men who have sex with men, treatment, cost-effectiveness, anal cancer
Introduction
The incidence of anal cancer has increased during the era of highly active antiretroviral therapy (HAART), while in contrast, other human immunodeficiency virus (HIV)-related malignancies have become less common. 1–3 HIV-infected men who have sex with men (MSM) are at higher risk for developing anal cancer than all other populations. The incidence of anal cancer in this particular group is over 80 times higher than in HIV-uninfected individuals. 4–7 Nearly half of HIV-infected individuals living in the United States (U.S.) are MSM, and establishing cost-effective protocols for the prevention of anal cancer should be an important component in the care of HIV-infected patients who are living longer during the HAART era. 8
Screening HIV-infected MSM with annual anal cytology has been shown to be cost-effective, with an incremental cost-effectiveness ratio compared to no screening of $16,600 per quality-adjusted life year (QALY) saved, which is similar to other accepted screening tests such as colon cancer screening. 9 High resolution anoscopy (HRA) is a technique used to detect high-grade anal intraepithelial neoplasia (HGAIN)10,11 which is the likely precursor to anal cancer. Once identified by HRA, high-grade lesions can be treated with office-based ablation or intraoperative ablation. Algorithms for follow-up evaluation after treatment of HGAIN have been proposed 12, but there is currently no consensus on how to best manage this high-risk population post-treatment. Assessing the value of alternative management strategies would inform practice guidelines.
Our objective was to evaluate the cost-effectiveness of alternative follow-up strategies after treatment of HGAIN in HIV-infected MSM. We developed a decision-analytic model to synthesize the epidemiological, clinical, and economic data on recurrent anal disease, and estimated the clinical benefits, costs and cost-effectiveness of alternative management strategies.
Materials and Methods
Model Overview
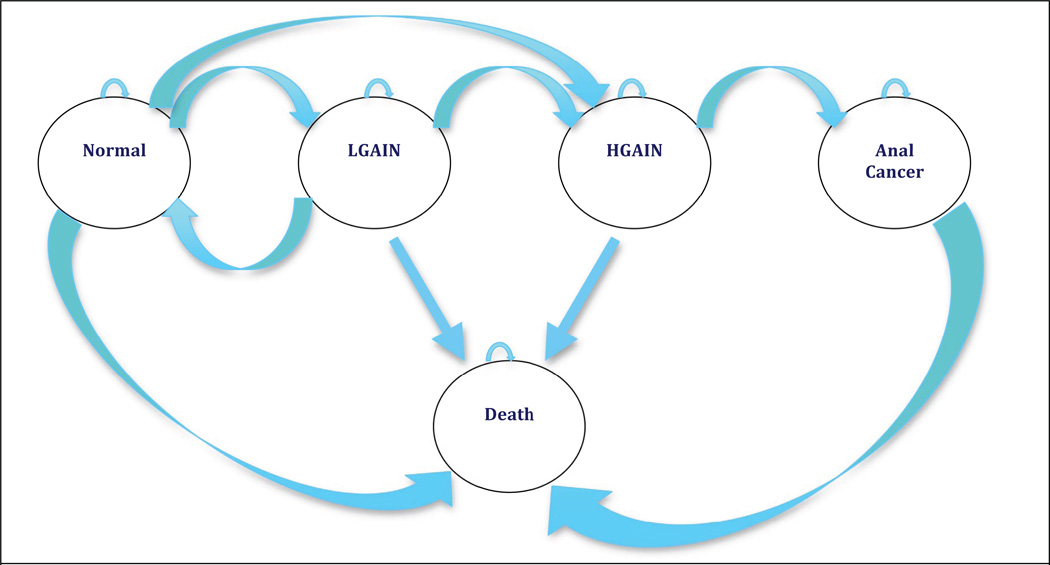
We developed a state-transition Markov model using TreeAge Pro 2009 (TreeAge, Williamstown, MA) to estimate the health and economic outcomes of surveillance strategies for MSM following treatment of HGAIN. HIV-infected MSM start in the Markov model health states defined by HPV-associated anal disease and HIV status (Figure 1), including normal (no disease), low-grade anal intraepithelial neoplasia (LGAIN), high-grade anal intraepithelial neoplasia (HGAIN), anal cancer and death. We simulated a cohort of 30-year-old HIV-infected MSM after treatment for HGAIN, which includes anal intraepithelial neoplasia (AIN) 2 or 3. Initial surveillance and monitoring for AIN occurred in 6-month cycles. Participants progressed through the different health states based on follow-up results after treatment for HGAIN. The model simultaneously simulated the natural history of HPV and HIV diseases and used transition probabilities from the literature to move participants through health states over time. 9,10,14 We assumed that disease regression from HGAIN was only possible after treatment. For the base case, we assumed that patients had a CD4 count greater than 500 cells/mm3 but we used sensitivity analyses to account for improved CD4 count after HAART initiation at a CD4 count less than 500 cells/mm3.
Figure 1. Markov Model Overview.
The model is composed of 5 health states. Each health states incorporates the natural history of anal disease (normal, low-grade intraepithelial neoplasia (LGAIN), high-grade intraepithelial neoplasia (HGAIN), anal cancer, and death), and the natural history of HIV with CD4 count greater than 500 cells/mm3.
We evaluated five surveillance strategies in HIV-infected MSM who had previously been treated for AIN 2 or 3: (1) HRA at 6 months followed by anal cytology at 12 months, (2) HRA at 6 months followed by HRA at 12 months, (3) combined HRA and anal cytology at 6 months followed by anal cytology at 12 months, (4) combined HRA and anal cytology at 6 months followed by HRA at 12 months, (5) combined HRA and anal cytology at 6 months followed by combined HRA and anal cytology at 12 months. All abnormal anal cytology tests were confirmed with HRA evaluation. Supplemental Digital Content Figure 1 depicts the follow-up algorithm for patients with HGAIN.
Health outcomes, expressed as quality-adjusted life years (QALYs), and costs associated with alternative surveillance strategies were projected for a cohort of 30-year old HIV-infected MSM over the lifetime. Strategies were compared using the incremental cost-effectiveness ratio (ICER), which is defined as the additional cost of a specific strategy divided by the additional clinical benefit, compared to the next less costly strategy. Strategies that were less effective and more costly than an alternate strategy (i.e., strongly dominated) and strategies with a higher incremental cost-effectiveness ratio than a more effective alternative strategy (i.e., weakly dominated) were eliminated from the calculations. Although there is no stringent cost-effectiveness threshold below which an intervention would be considered good value for money, a common benchmark in the U.S. includes $100,000/QALY gained. The analysis was conducted from the societal perspective, including costs irrespective of payor. As recommended for economic evaluations in the U.S., future costs and health benefits were discounted at an annual rate of 3%. 13 Costs were expressed in 2011 U.S. dollars. We performed a series of deterministic sensitivity analyses to identify parameters with the greatest impact on cost-effectiveness. Based on the results, we included important parameters in a probabilistic sensitivity analysis in which we defined key parameter values as distributions and used second-order Monte Carlo Simulation to perform 1000 cohort simulations.
Clinical Data
Table 1 summarizes model input values assumed in the base case analysis. 9–11,14, 16–22,35 Data obtained from the literature included information on background mortality rate; natural history of HPV and HIV diseases; operating characteristics of screening and diagnostic tests; effectiveness of treatment for HGAIN; mortality rate from anal cancer; costs associated with screening, diagnosis, and treatment of HGAIN and anal cancer and HIV treatment cost.
Table 1.
Selected model input parameters
| Variable | CD4 >500 cells/ mm3 | Sources |
|---|---|---|
| Progression ratea | ||
| Normal to low-grade | 0.0457 (0.0140‒0.1146) | 10, 14 |
| Normal to high-grade | 0.0417 (0.0118- 0.1086) | 10, 14 |
| Low-grade to high-grade | 0.2109 (0.1794‒0.3710) | 10, 14 |
| High-grade to cancer | 0.0253 (0.0039‒0.0836) | 9 |
| Regression ratea | ||
| Low-grade to normal | 0.0806 (0.0383‒0.1661) | 10, 14 |
| High-grade to normal | 0 | 10, 14 |
| Testing Characteristics | ||
| Anal cytology, % | ||
| Sensitivity | 81 (42‒98) | 16,17 |
| Specificity | 63 (32–81) | |
| HRA, % | ||
| Sensitivity | 95 (85‒99) | 9,11,17 |
| Specificity | 91 (85–100) | |
| Screening Cost, $ | ||
| Anal cytology, including performing the test |
60 (46‒71) | 21,35 |
| Work-up and treatment Cost, $ | ||
| AIN diagnosis (HRA and biopsy) | 314 (177‒334) | 21 |
| Treatment of detected HGAIN | 419 (271‒449) | 21 |
| Invasive anal cancer | 37,276 ( 18,080‒72,345) | 21 |
| HIV monthly care, $ | 390 ( 292‒488) | 22 |
| Health state utility weights | ||
| HIV | 0.94 (0.9‒0.98) | 20 |
| HGAIN (multiplier) | 0.98 (0.95‒0.99) | 18 |
| Anal SCC | 0.58 (0.5‒0.7) | 18,19 |
HGAIN: high grade intraepithelial lesion; HIV: human immunodeficiency virus; MSM : men who have sex with men ; AIN: anal intra-epithelial neoplasia; HRA: high resolution anoscopy
six-month cycle length.
The following assumptions were made for the base case: (1) all positive anal cytology tests were subsequently evaluated by HRA; (2) screening coverage with anal cytology was assumed to be 100%; (3) all detected HGAIN and anal cancer cases were treated; (4) all lesions were treated with outpatient ablation and did not require intraoperative surgical intervention; (5) HAART was initiated at CD4 cell count < 500 cells/mm3; (6) recurrent HGAIN was assumed to have a natural history similar to anal dysplasia prior to treatment.
Natural history of anal dysplasia
Information on the rate of disease recurrence as well as disease progression and regression were obtained from the literature.9,10,14 As the natural history of anal disease in patients who had been treated was not available, we used available data on untreated patients.10,14 Transition probabilities accounted for the impact of HPV disease. Transition from HGAIN to anal cancer has not been well-documented in clinical studies, therefore,we utilized an estimate from a published study that used cancer incidence data to calibrate this parameter. 9 Five-year survival from anal cancer of 61.8% reported by the Surveillance, Epidemiology and End Results (SEER) program of the National Cancer Institute15 was used to reflect excess mortality due to disease.
Test Characteristics
Estimates of diagnostic tests operating characteristics were obtained from the literature.9,16–17 Data from the largest prospective study on HIV-infected MSM were used to estimate the sensitivity (81%) and specificity (63%) of anal cytology testing.16, 17 HRA test characteristics were derived from a longitudinal study of anal squamous intraepithelial lesions, with 95% sensitivity and 91% specificity. 9, 11, 17
Health-Related Quality of Life
Health outcomes were expressed in QALYs to capture mortality and morbidity associated with a particular health state. We used previously reported health utility weights for HGAIN. 18,19 We used published health state preferences for gastrointestinal cancer (0.58) as a proxy for anal cancer quality weights. HIV-related quality of life was a function of CD4 count and was informed by the literature.20 Joint health state preferences for HPV- and HIV-related disease were estimated using standard multiplicative assumptions. A utility multiplier of 0.98 was applied to patients with HGAIN.18
Cost
Costs included direct medical costs which incorporated cost of screening and diagnostic tests, as well as cost for HGAIN treatment. Cost estimates were obtained from the 2011 Medicare fee schedule.21 Cost of monthly HIV care included inpatient care and outpatient care, and were informed by the literature. 22 In sensitivity analyses we included the cost of HAART initiation as we assumed that antiretroviral therapy was initiated at CD4 count below 500. All costs were updated to 2011 U.S. dollars using the medical care component of the Consumer Price Index.23
Results
Base case
For 30-year-old HIV-infected MSM with prior HGAIN treatment, surveillance with HRA at 6 months and anal cytology at 12 months (HRA 6 / anal cytology 12) led to a life expectancy of 40.03 years and a discounted QALE of 21.48 QALYs at a lifetime discounted cost of $61,536 (Table 2.) Compared to HRA 6/anal cytology 12, HRA at 6 months and 12 months (HRA 6/HRA12) was associated with an incremental life expectancy gain of 0.1716, a discounted QALE gain of 0.0723 QALY at an incremental cost of $322, corresponding to an incremental cost-effectiveness ratio of $4,446/QALY gained. Combined HRA and cytology at 6 months, coupled with either HRA or cytology at 12 months, was associated with higher lifetime costs, but lower life expectancies than HRA at 6 and 12 months, and were therefore dominated. Compared to HRA6/HRA12, combined anal cytology and HRA at 6 and 12 months was associated with an incremental life expectancy gain of 0.2762 year, and a quality-adjusted life expectancy gain of 0.1061, a discounted lifetime cost of $63,701, corresponding to an incremental cost-effectiveness ratio of $17,373/QALY gained.
Table 2.
Cost-effectiveness of alternative surveillance strategies after treatment of HGAIN in HIV-infected MSM
| Strategy | Discounted cost (2011 $US ) |
Undiscounted Life expectancy (years) |
Discounted quality- adjusted life expectancy (years) |
Incremental cost- effectiveness ratio ($/QALY) |
|---|---|---|---|---|
| CD4 count > 500 cells/ mm3 | ||||
| HRA at 6 months / cytology at 12 months |
61,536 | 40.0329 | 21.4784 | --- |
| HRA at 6 months / HRA at 12 months | 61,857 | 40.2044 | 21.5507 | 4,446 |
| Combined HRA+ cytology at 6 months/ HRA at 12 months |
62,552 | 40.1380 | 21.5251 | Dominated |
| Combined HRA+ cytology at 6 months/ cytology at 12 months |
62,556 | 40.1416 | 21.5293 | Dominated |
| Combined HRA+ cytology at 6 months/ HRA+ cytology at 12 months |
63,701 | 40.4807 | 21.6568 | 17,373 |
HGAIN:high grade intraepithelial lesion; HIV: human immunodeficiency virus; MSM: men who have sex with men; QALY:quality-adjusted life year; HRA:high resolution anoscopy
Sensitivity analysis
Deterministic Sensitivity Analysis
The cost-effectiveness of post-treatment surveillance was most sensitive to estimates of test characteristics, cost and disease progression rate. Although a strategy combining HRA and anal cytology at both visits was affected by disease progression rate from normal to HGAIN and from HGAIN to cancer, the incremental cost-effectiveness ratio remained stably below a threshold of $100,000/QALY.
Impact of disease progression rate and cost
When the estimate of the rate of disease progression from normal to HGAIN was decreased over a plausible range, the incremental cost-effectiveness ratio of combined anal cytology and HRA at 6 and 12 months increased from $17,373/ QALY gained to $ 46,133 /QALY gained. When the rate of disease progression was increased over a plausible range the incremental cost-effectiveness ratio decreased from $ 17,373/ QALY gained to $6,298/QALY gained. The sensitivity of diagnostic tests also had an impact on the cost-effectiveness of surveillance strategies. When decreasing the sensitivity of HRA to 85% the combined strategy of HRA with cytology became more attractive compared to a strategy of HRA alone, yielding a shift from $17,373 to $8,160/QALY gained. Furthermore, variations in HGAIN treatment effectiveness also impacted the cost-effectiveness ratio, which nonetheless remained below the $100,000/QALY threshold. Increasing the discount rate from 3% to 10% shifted the cost-effectiveness ratio from $17,373 to $33,460/QALY gained since the gains in health benefit are generally downstream from the costs. Costs of treating HGAIN and anal cancer had little impact on the cost-effectiveness of results.
Probabilistic Sensitivity Analysis
We performed 1000 simulations in which the input values for disease progression, test characteristics, cost of diagnostic tests, treatment efficacy and cost, and quality weights were varied simultaneously. We found that combined HRA and anal cytology at 6 and 12-month visits was the optimal strategy in 91% of simulations, HRA 6/ HRA 12 was optimal in 8%, while other strategies were optimal in less than 1% of simulations (Supplemental Digital Content Figure 2.)
Impact of CD4 count response to HAART
We performed a sensitivity analysis to account for an increase in CD4 count following HAART initiation. The following two CD4 count strata were considered: stratum A included CD4 count < 200 cells/ mm3 and stratum B represented CD4 count between 200 and 500 cells/ mm3. We used the approach that follows for our analysis. Information on disease progression was obtained from the literature. 10,14 Transition probabilities accounted for the combined impact of HPV and HIV disease, with more rapid disease progression at lower CD4 counts. We used information from a large observational cohort study to estimate CD4 count response to HAART initiation. 24 Those in stratum A (CD4 count < 200 cells/ mm3) reached 500 cells/ mm3 in approximately five years, while those in stratum B (200 and 500 cells/ mm3) required approximately 1.5 years. We observed that irrespective of variations in CD4 count, combined HRA and cytology performed at 6 and 12 months remained the most cost-effective strategy. ICERs were $ 15,354 / QALY and $13,556/ QALY gained for stratum A and B, respectively. Ratios remained below the threshold of $100,000/ QALY (Supplemental Digital Content Table 1 and 2, and Supplemental Digital Content 1)
Discussion
There is no consensus on the best subsequent management of HIV-infected MSM who have been treated for HGAIN. The results of this analysis suggest that repeated HRA is an effective and cost-effective surveillance modality. Surveillance strategies that included HRA at the 6- and 12-month visits, with or without anal cytology testing, were more effective than using HRA only for confirmatory testing of abnormal anal cytology testing. Our analysis revealed that both strategies (HRA 6/ HRA 12 and combined HRA/cytology at both visits) were cost-effective; however, the combined strategy extended life expectancy and quality-adjusted life expectancy while remaining below the commonly-cited threshold of $100,000/ QALY gained. HIV providers and guideline panels can use these results in the deliberations to improve outcomes after HIV-infected MSM are diagnosed and treated with HPV-associated disease.
The cost-effectiveness ratio remained robustly below a commonly-cited threshold of $100,000 per QALY over a wide range of sensitivity analyses. Our results were most influenced by test characteristics and cost, and progression rate of normal to HGAIN and HGAIN to cancer, suggesting that further studies of HPV expression in MSM in the HAART era are warranted, given trends toward earlier initiation of treatment and longer survival. In addition, probabilistic sensitivity analysis incorporating uncertainty in parameters included in the model revealed that combined HRA and anal cytology at 6 and 12-months was the optimal strategy in 91% of simulations.
Previous studies have shown that annual screening of HIV-infected MSM is cost-effective9; however, there are no published studies on the cost-effectiveness of alternative surveillance strategies after treatment for HGAIN. In the early HAART era, Goldie et al. showed that annual screening with anal cytology was cost-effective with a ratio of $ 16,600 per QALY saved.9 A more recent analysis by Lam et al. concluded that direct use of HRA was the most cost-effective strategy to screen for HGAIN in HIV-infected MSM.25 These two analyses were performed from a U.S. perspective; in contrast, Karnon et al. found that screening high-risk MSM for anal cancer in the United Kingdom (UK) was not cost-effective.18 This discrepancy was likely observed given the lower rates of anal cancer in the UK compared to that in the U.S. The reasons for differences in incidence warrant further exploration. Our results were in line with other HIV-related interventions such as genotypic resistance testing prior to antiretroviral therapy initiation or prophylaxis for Pneumocystis Jiroveci pneumonia. ICERs adjusted for inflation were $35,067 per QALY gained and $29,043 per QALY gained, respectively.
There are several limitations to our study. The natural history of anal dysplasia with or without treatment has not been well-defined. Furthermore, the efficacy of secondary prevention for anal cancer has yet to be proven in a large randomized controlled trial.27 While uncertainty remains about the ability of secondary screening to prevent future anal cancers, clinical reality dictates that providers select an immediate course of action when caring for patients with a history of anal dysplasia. Our analysis uses decision analytic methods to provide a rational approach to making decisions about management despite imperfect information. We used the best available data about disease progression and treatment efficacy, and performed multiple sensitivity analyses to explore the impact of uncertainty on our results. While future data could shed new light on the conclusions of this analysis, no such data are immediately forthcoming and decisions must be made today on the best surveillance strategy for patients with a history of anal dysplasia. Our results provide clinicians and guideline panels with information on which to formulate decisions. Our analyses showed that our findings are stable over a wide range of assumptions, including variations in the rates of progression from normal to HGAIN or HGAIN to cancer. Our estimates could be further refined if better estimates of the long-term outcomes of treating HGAIN in an outpatient setting were available. Furthermore, our findings may not be generalizable to a population with severe disease that could not be managed in an outpatient setting, or to other high risk groups for anal cancer such as women with a history of high-grade cervical lesions. Furthermore, utility values used to generate QALYs were based on gastrointestinal cancers and were not specific to anal cancer. These inputs might impact the clinical benefits observed in our analysis.
In conclusion, our analysis suggests that combined HRA and anal cytology at 6 and 12-month visits may be a cost-effective follow-up strategy for HIV-infected MSM who have been treated for HGAIN. Our hope is that these findings contribute to the informed discussions on how to improve outcomes for HIV-infected MSM who are living longer during the HAART era. Future studies are needed on the acceptability of HGAIN treatment among patients and health care providers.
Supplementary Material
Supplemental Digital Content Figure 2. Result of probabilistic sensitivity analysis.HRA+ cytology 6/ HRA+ cytology 12= combined HRA and anal cytology at 6 months followed by combined HRA and anal cytology at 12 months; HRA 6/ HRA 12= HRA at 6 months followed by HRA at 12 months; HRA 6/ Cytology 12= HRA at 6 months followed by anal cytology at 12 months; HRA +cytology 6 / cytology 12= combined HRA and anal cytology at 6 months followed by anal cytology at 12 months; HRA+ cytology 6/ HRA 12= combined HRA and anal cytology at 6 months followed by HRA at 12 months. We performed 1000 simulations in which parameter input values were varied simultaneously. Combined HRA and anal cytology at 6 and 12-month visits was the optimal strategy in 91% of simulations, HRA 6/ HRA 12 was optimal in 8%, while other strategies were optimal in less than 1% of simulations.
Table 3.
Sensitivity Analysis
| Incremental Cost-effectiveness Ratio, $ per Quality-Adjusted Life Year Saved |
||
|---|---|---|
| Variable | HRA then HRA | HRA+ Cytology then HRA+ Cytology |
| Base Case | 4,446 | 17,373 |
| Progression rate | ||
| Normal to LGAIN | ||
| 0.014 | 5,291 | 11,636 |
| 0.1146 | 3,819 | 17,817 |
| Normal to HGAIN | ||
| 0.0118 | 4,485 | 46,133 |
| 0.1086 | 4,202 | 6,298 |
| LGAIN to HGAIN | ||
| 0.1794 | 4,622 | 18,165 |
| 0.3710 | 3,899 | 14,154 |
| HGAIN to anal cancer | ||
| 0.0039 | 9,428 | 71,139 |
| 0.0836 | 2,730 | 7,305 |
|
Anal Cancer mortality rate |
||
| 0.05127 | 4,478 | 18,693 |
| 0.1892 | 4,426 | 16,550 |
| HRA Sensitivity | ||
| 0.85 | 3,823 | 8,160 |
| HRA Specificity | ||
| 0.85 | 5,551 | 18,481 |
| Treatment Effectiveness | ||
| 0.63 | 4,405 | 17,639 |
| 0.75 | 4,525 | 16,927 |
| Cost of anal cytology test | ||
| 46 | 5,092 | 15,675 |
| 71 | 3,939 | 18,707 |
| Cost of HGAIN ablation | ||
| 271 | 4,200 | 16,996 |
| 449 | 4,496 | 17,449 |
|
Cost of Anal Cancer treatment |
||
| 18,080 | 4,899 | 17,959 |
| 72,345 | 3,620 | 16,301 |
| Discount rate, % | ||
| 0 | 4,046 | 13,020 |
| 5 | 4,751 | 21,200 |
| 10 | 5,569 | 33,460 |
|
Baseline CD4 count between 200 and 500 cells/ mm3 |
¶ | 13,556 |
|
Baseline CD4 count < 200 cells/ mm3 |
¶ | 15,354 |
LGAIN: low-grade anal intra-epithelial neoplasia; HGAIN: high grade intraepithelial lesion; HRA: high resolution anoscopy.
= HRA then HRA used as baseline as other strategies were dominated.
Acknowledgments
The authors thank Erika D’agata, M.D., M.P.H. who provided guidance and critical review of the manuscript. Support for this study came from the Harvard Medical School Center for Excellence in Minority Health and Health Disparities (Health Disparities Post Graduate Fellowship funded by Health Resources and Services Administration, Bureau of Health Professions grant).
Role of Funding Sources:
Agencies funding this study have no role in the collection, analysis or interpretation of data.
Source of Funding:
L.A.P. has received honoraria from Merck as a member of the speakers’ bureau. K.H.M. received research support from Merck, Bristol-Myers Squibb and Gilead.
S.A.A. was supported by the Harvard Medical School Center for Excellence in Minority Health and Health Disparities (Health Disparities Post Graduate Fellowship funded by Health Resources and Services Administration, Bureau of Health Professions grant.) J.J.K. is supported in part by the National Cancer Institute (1R01CA160744-01A1) and BPL is supported in part by the National Institute of Drug Abuse (R01 DA031059.)
Footnotes
Conflicts of Interest
For the remaining authors no conflicts of interest were declared.
Author Disclosure Statement
L.A.P. has received honoraria from Merck as a member of the speakers’ bureau. K.H.M. received research support from Merck, Bristol-Myers Squibb and Gilead.
Contributor Information
Sabrina A. Assoumou, Instructor in Medicine, Boston University School of Medicine, Boston Medical Center, One Boston Medical Center Place, Boston, MA 02118, P: 617-414-2896, F:617-638-8070, sabrina.assoumou@bmc.org.
Kenneth H. Mayer, Infectious Disease Attending and Director of HIV Prevention Research, Beth Israel Deaconess Medical Center, Visiting Professor of Medicine, Harvard Medical School, Medical Research Director and Co-Chair, The Fenway Institute, Fenway Health, 1340 Boylston Street, 8th floor, Boston, Mass 02215, P: 617-927-6087, F: 617-267-0764, mayer@fenwayhealth.org
Lori Panther, Associate Medical Director for Clinical Research, The Fenway Institute, Division of Infectious Disease, Beth Israel Deaconess Medical Center, 1340 Boylston Street, Boston, MA USA 02215, P: 617-927-6056, F: 617-632-7626, lpanther@bidmc.harvard.edu.
Benjamin P. Linas, Assistant Professor of Medicine, Boston University School of Medicine, Assistant Professor of Epidemiology, Boston University School of Public Health, Boston Medical Center, 850 Harrison Ave., Dowling - 3N room 3205, Boston, MA 02118, P: 617-414-5238, F: 617-414-706, Benjamin.Linas@bmc.org.
Jane J. Kim, Assistant Professor of Heath Decision Science, Department of Health Policy and Management, Harvard School of Public Health, 718 Huntington Avenue, Boston, MA 02115, P: (617) 432-0095, Jkim@hsph.harvard.edu.
References
- 1.Chiao EY, Krown SE, Stier EA, et al. A population-based analysis of temporal trends in the incidence of squamous anal canal cancer in relation to the HIV epidemic. J Acquir Immune Defic Syndr. 2005 Dec 1;40(4):451–455. doi: 10.1097/01.qai.0000159669.80207.12. [DOI] [PubMed] [Google Scholar]
- 2.Long JL, Engels EA, Moore RD, et al. Incidence and outcomes of malignancy in the HAART era in an urban cohort of HIV-infected individuals. AIDS. 2008 Feb 19;22(4):489–496. doi: 10.1097/QAD.0b013e3282f47082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piketty C, Selinger-Leneman H, Grabar S, et al. Marked increase in the incidence of invasive anal cancer among HIV-infected patients despite treatment with combination antiretroviral therapy. AIDS. 2008;22:1203–1211. doi: 10.1097/QAD.0b013e3283023f78. [DOI] [PubMed] [Google Scholar]
- 4.Ries LAG, Young JL, Keel GE, et al. SEER Survival Monograph: Cancer Survival Among Adults: U.S. SEER Program, 1988–2001, Patient and Tumor Characteristics. Bethesda, MD: Magaret M. Madeleine and Laura M. Newcomer. National Cancer Institute, SEER Program, NIH Pub. No. 07-6215; 2007. Chapter 5. [Google Scholar]
- 5.Ries LAG, Harkins D, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2003. Bethesda, MD: National Cancer Institute; 2006. http://seer.cancer.gov/csr/1975_2003/, based on November 2005 SEER data submission, posted to the SEER web site. [Google Scholar]
- 6.Daling JR, Weiss NS, Hislop TG, et al. Sexual practices, sexually transmitted diseases, and the incidence of anal cancer. N Engl J Med. 1987;317:973–977. doi: 10.1056/NEJM198710153171601. [DOI] [PubMed] [Google Scholar]
- 7.Silverberg MJ, Lau B, Justice AC, Press N, Martin JN, Dubrow R, et al. the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of IeDEA. Risk of Anal Cancer in HIV-Infected and HIV-Uninfected Individuals in North America. Clin Infect Dis. 2012 Feb 13; doi: 10.1093/cid/cir1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. HIV prevalence estimates—US, 2006. MMWR. 2008;57(39):1073–1076. [PubMed] [Google Scholar]
- 9.Goldie SJ, Kuntz KM, Weinstein MC, et al. The clinical effectiveness and cost-effectiveness of screening for anal squamous intraepithelial lesions in homosexual and bisexual HIV-positive men. JAMA. 1999 May 19;281(19):1822–1829. doi: 10.1001/jama.281.19.1822. [DOI] [PubMed] [Google Scholar]
- 10.Palefsky JM, Holly EA, Ralston ML, et al. High incidence of anal high-grade squamous intra-epithelial lesions among HIV-positive and HIV-negative homosexual and bisexual men. AIDS. 1998 Mar 26;12(5):495–503. doi: 10.1097/00002030-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Jay N, Berry JM, Hogeboom CJ, et al. Colposcopic appearance of anal squamous intraepithelial lesions: relationship to histopathology. Dis Colon Rectum. 1997;40:919–928. doi: 10.1007/BF02051199. [DOI] [PubMed] [Google Scholar]
- 12.Chin-Hong PV, Palefsky JM. Natural history and clinical management of anal human papillomavirus disease in men and women infected with human immunodeficiency virus. Clin Infect Dis. 2002 Nov 1;35(9):1127–1134. doi: 10.1086/344057. [DOI] [PubMed] [Google Scholar]
- 13.Gold MR, Siegel JE, Russell LB, et al., editors. Cost-effectiveness in Health and Medicine. By New York: Oxford University Press; 1996. [Google Scholar]
- 14.Palefsky JM, Holly EA, Hogeboom CJ, et al. Virologic, immunologic, and clinical parameters in the incidence and progression of anal squamous intraepithelial lesions in HIV-positive and HIV-negative homosexual men. J Acquir Immune Defic Syndr Hum Retrovirol. 1998 Apr 1;17(4):314–319. doi: 10.1097/00042560-199804010-00004. [DOI] [PubMed] [Google Scholar]
- 15.National Cancer Institute. Surveillance, epidemiology, end results (SEER) cancer statistics review, 1975–2006. [Accessed June 3, 2011]; Available at: http://seer.cancer.gov/csr/1975_2006/results_merged/topic_survival.pdf.
- 16.Chiao EY, Giordano TP, Palefsky JM, et al. Screening HIV-infected individuals for anal cancer precursor lesions: a systematic review. Clin Infect Dis. 2006 Jul 15;43(2):223–233. doi: 10.1086/505219. Epub 2006 Jun 7. [DOI] [PubMed] [Google Scholar]
- 17.Palefsky JM, Holly EA, Ralston ML, et al. Anal cytological abnormalities and anal HPV infection in men with Centers for Disease Control group IV HIV disease. Genitourin Med. 1997 Jun;73(3):174–180. doi: 10.1136/sti.73.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karnon J, Jones R, Czoski-Murray C, et al. Cost-utility analysis of screening high-risk groups for anal cancer. J Public Health (Oxf) 2009 Mar;31(1):194. doi: 10.1093/pubmed/fdn045. 200Sep;30(3):293-304. Epub 2008 Jun 17. Erratum in: J Public Health (Oxf) [DOI] [PubMed] [Google Scholar]
- 19.Kim Jane J, Goldie Sue J. Health and economic implications of HPV vaccination in the United States. N Engl J Med. 2008 Aug 21;359(8):821–832. doi: 10.1056/NEJMsa0707052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freedberg KA, Scharfstein JA, Seage GR., 3rd The cost-effectiveness of preventing AIDS-related opportunistic infections. JAMA. 1998 Jan 14;279(2):130–136. doi: 10.1001/jama.279.2.130. Erratum in: JAMA 1999 Jun 2;281(21):1989. [DOI] [PubMed] [Google Scholar]
- 21.Medicare Physician Fee Schedule. [Accessed on October 5, 2012];Centers for Medicare and Medicaid Services. Available at http://www.cms.gov/apps/physician-fee-schedule/overview.asp.
- 22.Schackman BR, Gebo KA, Walensky RP, et al. The lifetime cost of current human immunodeficiency virus care in the United States. Med Care. 2006 Nov;44:990–997. doi: 10.1097/01.mlr.0000228021.89490.2a. [DOI] [PubMed] [Google Scholar]
- 23.Consumer Price Index-Medical Care Component. [Accessed on October 5, 2012];U.S. Department of Labor, Bureau of Labor and Statistics. Available at: www.bls.gov/cpi/cpid09av.pdf.
- 24.Gras L, Kesselring AM, Griffin JT, et al. ATHENA, Netherlands National Observational Cohort Study.CD4 cell counts of 800 cells/mm3 or greater after 7 years of highly active antiretroviral therapy are feasible in most patients starting with 350 cells/mm3 or greater. J Acquir Immune Defic Syndr. 2007 Jun 1;45(2):183–192. doi: 10.1097/QAI.0b013e31804d685b. [DOI] [PubMed] [Google Scholar]
- 25.Lam JM, Hoch JS, Tinmouth J, et al. Cost-effectiveness of screening for anal precancers in HIV-positive men. AIDS. 2011 Mar 13;25(5):635–642. doi: 10.1097/QAD.0b013e3283434594. [DOI] [PubMed] [Google Scholar]
- 26.Hu D, Goldie SJ. The economic burden of noncervical human papillomavirus disease in the United States. Am J Obstet Gynecol. 2008;198:e1–e7. doi: 10.1016/j.ajog.2008.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sax PE, Islam R, Walensky RP, Losina E, Weinstein MC, Goldie SJ, Sadownik SN, Freedberg KA. Should resistance testing be performed fortreatment-naive HIV-infected patients? A cost-effectivenessanalysis Clin Infect Dis. 2005 Nov 1;41(9):1316–1323. doi: 10.1086/496984. [DOI] [PubMed] [Google Scholar]
- 28.Palefsky JM. Antiretroviral therapy and anal cancer: the good, thebad, and the unknown. Sex Transm Dis. 2012 Jul;39(7):501–503. doi: 10.1097/OLQ.0b013e31825f7921. [DOI] [PubMed] [Google Scholar]
- 28.Arias L. United States Life Tables. National Vital Statistics Reports. 2010 Jun 28;Vol. 58 No. 21. [PubMed] [Google Scholar]
- 29.Melnikow J, Kulasingam S, Slee C, et al. Surveillance after treatment for cervical intraepithelial neoplasia: outcomes, costs, and cost-effectiveness. Obstet Gynecol. 2010 Nov;116(5):1158–1170. doi: 10.1097/AOG.0b013e3181f88e72. [DOI] [PubMed] [Google Scholar]
- 30.Surawicz CM, Critchlow C, Sayer J, et al. High grade anal dysplasia in visually normal mucosa in homosexual men: seven cases. Am J Gastroenterol. 1995;90:1776–1778. [PubMed] [Google Scholar]
- 31.Nathan M, Hickey N, Mayuranathan L, Vowler SL, Singh N. Treatment of anal human papillomavirus-associated disease: a long term outcome study. Int J STD AIDS. 2008 Jul;19(7):445–449. doi: 10.1258/ijsa.2007.007290. [DOI] [PubMed] [Google Scholar]
- 32.Goldstone SE, Kawalek AZ, Huyett JW. Infrared coagulator: a useful tool for treating anal squamous intraepithelial lesions. Dis Colon Rectum. 2005 May;48(5):1042–1054. doi: 10.1007/s10350-004-0889-0. [DOI] [PubMed] [Google Scholar]
- 33.Cranston RD, Hirschowitz SL, Cortina G, Moe AA. A retrospective clinical study of the treatment of high-grade anal dysplasia by infrared coagulation in a population of HIV-positive men who have sex with men. Int J STD AIDS. 2008 Feb;19(2):118–120. doi: 10.1258/ijsa.2007.005665. [DOI] [PubMed] [Google Scholar]
- 34.Goldstone RN, Goldstone AB, Russ J, Goldstone SE. Long-term Follow-up of Infrared Coagulator Ablation of Anal High-Grade Dysplasia in Men Who Have Sex With Men. Dis Colon Rectum. 2011 Oct;54(10):1284–1292. doi: 10.1097/DCR.0b013e318227833e. [DOI] [PubMed] [Google Scholar]
- 35.Marks DK, Goldstone SE. Electrocautery Ablation of High-Grade Anal Squamous Intraepithelial Lesions in HIV-Negative and HIV-Positive Men who have sex with Men. J Acquir Immune Defic Syndr. 2011 Nov;:30. doi: 10.1097/QAI.0b013e3182437469. [DOI] [PubMed] [Google Scholar]
- 36.Center for Medicare Services. US Department of Health and Human Services. [Accessed October 5];2011 Clinical Diagnostic Laboratory Fee Schedule. 2012 Available at http://www.cms.gov/Medicare/Medicare-Fee-for-ServicePayment/ClinicalLabFeeSched/clinlab.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content Figure 2. Result of probabilistic sensitivity analysis.HRA+ cytology 6/ HRA+ cytology 12= combined HRA and anal cytology at 6 months followed by combined HRA and anal cytology at 12 months; HRA 6/ HRA 12= HRA at 6 months followed by HRA at 12 months; HRA 6/ Cytology 12= HRA at 6 months followed by anal cytology at 12 months; HRA +cytology 6 / cytology 12= combined HRA and anal cytology at 6 months followed by anal cytology at 12 months; HRA+ cytology 6/ HRA 12= combined HRA and anal cytology at 6 months followed by HRA at 12 months. We performed 1000 simulations in which parameter input values were varied simultaneously. Combined HRA and anal cytology at 6 and 12-month visits was the optimal strategy in 91% of simulations, HRA 6/ HRA 12 was optimal in 8%, while other strategies were optimal in less than 1% of simulations.