Abstract
Objective
To explore cancer-related posttraumatic stress (PTS) reactions in siblings of children with cancer including prevalence, common symptoms, comorbidity with anxiety and depression, and gender and age-related patterns.
Method
A total of 125 children (63 females) between the ages of 8 and 17 (M = 12.4; SD = 2.9 years) with a brother or sister with cancer, diagnosed 4 to 38 months prior to the study (M = 1.3 years; SD = 6.7 months), completed the Child PTSD Symptom Scale (CPSS), Revised Children's Manifest Anxiety Scale, and Child Depression Inventory-Short Form.
Results
Over half of the sample (60%) scored in the moderate to severe range for PTS and 22% fulfilled full criteria for PTSD based upon CPSS responses. Nearly 75% reported “Feeling upset when you think about or hear about the cancer,” and “Trying not to think about, talk about, or have feelings about the cancer.” Over 60% reported arousal symptoms. PTS symptoms reportedly interfered with functioning for 75% of the sample and co-occurred with anxiety and depressive symptoms. Gender and age-related patterns were not found.
Conclusions
Siblings of children with cancer experience cancer-related PTS reactions and greater attention should be paid to ameliorating their cancer-related distress with empirically-based treatments.
Keywords: Childhood cancer, siblings, family, posttraumatic stress, adjustment
Since publication of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 1994), medical events such as severe injuries and life threatening illnesses have been recognized as potentially traumatic events. In the DSM-IV, potentially traumatic events are defined as events in which individuals were exposed to real or perceived threats to life or physical integrity and responded with intense fear, horror, or helplessness. People both directly (i.e., the medical patient) and indirectly (i.e., witnesses, family members) exposed to such events are identified as susceptible to traumatic reactions. While early research on the psychosocial adjustment of people with life threatening chronic illnesses focused on constructs such as depression and anxiety (e.g., Eiser, Hill & Vance, 2000), this evolution in the diagnostic criteria for Posttraumatic Stress Disorder (PTSD) spurred research into the traumatic nature of medical illnesses (e.g., Kazak et al, 2006).
Among pediatric illnesses, childhood cancer is perhaps the most frequently studied as a potential traumatic event. In fact, childhood cancer-related traumatic stress was explored in the DSM-IV field trials that led to the change in the PTSD criteria discussed above (Pelcovitz et. al., 1996; 1998). When diagnosed with cancer, children and their family members may perceive the diagnosis as a threat to life and various aspects of cancer treatment (e.g., lumbar punctures, needles, chemotherapy, radiation, surgery) can be interpreted as “assaults on physical integrity” as defined by the DSM-IV. In the DSM-IV field trials, 23 adolescent cancer survivors (aged 13 to 20) off treatment or in the maintenance phase of cancer treatment (Range: 0-11 years post-treatment; M = 3.3 years) and their mothers were evaluated for PTSD using structured clinical interviews. One-third of the survivors (35%) and half of their mothers (54%) reported symptoms consistent with PTSD at some point since the cancer diagnosis with 17% of survivors and 25% of their mothers experiencing cancer-related PTSD at the time of assessment. These rates were significantly greater than the rates reported in the control group, a community sample of families with healthy children.
More recent and larger trials have found much lower rates of PTSD in adolescent childhood cancer survivors. Rates of current and past cancer-related PTSD derived from structured clinical interviews have been reported at 5 and 8%, respectively (Kazak, Alderfer, Rourke et al., 2004) and across studies using self-report questionnaires, 12 to 25% fall into the clinical range for posttraumatic stress (PTS) symptoms (Barakat et al., 1997; Butler, Rizzi & Handwerger, 1996; Kazak, Alderfer, Rourke et al., 2004; Stuber, Christakis, Houskamp & Kazak, 1996). Overall, rates of PTSD for children with cancer have been found to be no different than that seen in the general population of children (Barakat et al., 1997; Phipps, Jurberg & Long, 2009).
Parents of children with cancer, however, do seem to have elevated rates of cancer-related PTSD. Studies using structured clinical interviews have found 27 to 30% of mothers and 12% of fathers of childhood cancer survivors qualify for a diagnosis of PTSD at some point in time since their child's diagnosis with 14 to 20% of mothers and 10% of fathers qualifying for a diagnosis at the time of data collection (Kazak, Alderfer, Rourke et. al. 2004; Goldenberg Libov, Nevid, Pelcovitz, & Carmony, 2002). As Kazak and colleagues noted, this rate of lifetime occurrence is similar to the rate reported in the general population of adults experiencing a traumatic event (i.e., 20% for females, 8% for males) and is roughly equivalent to rates reported by adults exposed to violent crimes or tragic deaths (Breslau, 2001). Studies using self-report forms document that 15-44% of mothers and fathers of children with cancer report clinical levels of posttraumatic stress (Barakat et al., 1997; Brown, Madan-Swain & Lambert, 2003; Kazak, Alderfer, Rourke et al., 2004; Landolt, Vollrath, Ribi, Gnehm, & Sennhauser, 2003; Lindahl Norberg, Lindblad, & Boman, 2005; Poder, Ljungman & von Essen, 2008).
As illustrated above, much of the previous research on posttraumatic stress associated with childhood cancer has focused upon patients and their parents. Siblings have typically been excluded. Siblings within these families have a unique experience of childhood cancer that can be highly distressing and potentially traumatic. They may witness their brother or sister in pain, looking severely ill, and/or losing weight and hair. They may be separated from the diagnosed child for extended periods, fear that he or she will die, and not understand the disease and treatment process. During cancer treatment, siblings may also lose some level of support from their parents as parental attention shifts to the sick child and treatment demands may remove parents from the home. Plus, regular routines may be disrupted as the family reorganizes to accommodate the cancer and its treatment and siblings may be placed in the care of extended family members or friends (Nolbris, Enskar, & Hellstrom, 2007; Prchal & Landolt, 2012; Wilkins & Woodgate, 2005). All of these changes can result in feelings of fear, helplessness, jealousy, isolation, and uncertainty in siblings of children with cancer (Alderfer et al., 2010).
A recent systematic review of the literature regarding the psychosocial adjustment of siblings of children with cancer concluded that these children and adolescents are at risk for adjustment difficulties (Alderfer et al., 2010). In this review, while mean levels of anxiety and depression were not found to be elevated for siblings of children with cancer, there was evidence to suggest that their distress can be conceptualized within a posttraumatic stress framework. While research is scant, across studies 29-38% of siblings of children with cancer report moderate to severe PTS symptoms. In the largest empirical study to date (N = 78; Alderfer, Labay & Kazak, 2003) of siblings (aged 10 to 20) of adolescent cancer survivors (1 to 12 years post-treatment, M = 5.3 years), almost one third had moderate to severe PTS reactions; a rate greater than that found in a comparison sample of children attending well-patient physician visits. Similarly, Packman et al. (1997) found one third of siblings (aged 6 to 18) of children who had undergone bone marrow transplantation (BMT; 3 months to 7 years previously, M = 3.2 years) reported moderate or greater levels of PTS. Half of these siblings were bone marrow donors; however, PTS rates in donors vs. non-donors did not differ. Finally, research conducted at a summer camp for siblings of children with cancer revealed that more than one third (38%) of the camp participants (aged 6 to 17) reported cancer-related PTS reactions (Packman et al., 2004; time since diagnosis was not specified). There is also evidence suggesting that female siblings are more likely to experience cancer-related PTS than males (i.e., Alderfer et al., 2003), however age-related differences have not been consistently documented (Alderfer et al., 2010).
These findings suggest that a trauma framework may be useful for understanding the cancer-related distress of siblings of children with cancer. However, these studies have limitations including broad ranges in time since treatment and select samples (e.g., camp attendees). Further, they do not provide a detailed account of the symptoms experienced by these children, nor do they guide clinicians as to which siblings may be most likely to experience reactions.
The purpose of the current study is to provide a more detailed examination of cancer-related traumatic stress in siblings of children with cancer. To provide a more homogeneous sample in terms of time since diagnosis and the current relevance of cancer, the sample was limited to siblings of children diagnosed with cancer within the past 2 years, or beyond the 2-year mark, but still on treatment. It was believed that this sample may experience an even greater rate of cancer-related traumatic stress symptoms than siblings with brothers or sisters further from diagnosis, similar to patterns documented among adolescent cancer survivors and their parents (e.g., Phipps, Long, Hudson, & Rai, 2005). To fill some current gaps in the literature we posed the following questions: a) Do siblings perceive cancer as a potentially traumatic experience?; b) What PTS symptoms do siblings experience and with what frequency?; c) Do PTS symptoms interfere with functioning and if so, what types of functioning?; d) Are PTS reactions comorbid with anxiety and depression?; and e) Do these PTS reactions vary based on age and sex?
Method
Participants
A total of 126 families of children with cancer (170 siblings) participated, representing 75% of eligible families (N = 167) approached for participation. Within families, all healthy siblings between the ages of 8 and 18 were permitted to participate, but one child's data was randomly selected from each family for inclusion in these analyses. One sibling was an outlier in terms of time since diagnosis (48 months post-diagnosis) and was excluded from analyses. The resulting 125 siblings were between the ages of 8 and 17 (M = 12.4; SD = 2.9 yrs.), half (50%, n = 63) were female and 83% indicated they were Caucasian, with 10% African American, 5% Hispanic, 1% Asian American and 1% identifying themselves as bi-racial, consistent with the racial/ethnic composition of our cancer center. At the time of assessment, 4.7 to 38 months had elapsed since the cancer diagnosis (M = 1.3 yrs; SD = 6.7 months). Cancer diagnoses included solid tumors (37%), leukemias (30%), lymphomas (16%), brain tumors (14%), and other diagnoses (3%). Approximately one fifth of the families (21%) reported annual incomes below $50,000, 43% between $50,000 and $100,000 and 36% above $100,000.
Procedure
This study was approved by our institution's Committee for the Protection of Human Subjects. The Tumor Registry of our large eastern pediatric Cancer Center was used to identify potentially eligible families. Eligible families had: a) a child with cancer currently on treatment (with no limit in time since diagnosis) or off treatment but within two years of diagnosis; b) a healthy sibling between the ages of 8 and 18; and, c) fluency in English. Siblings were defined as full biological brothers or sisters, half-siblings, step-siblings, and adopted siblings living within the same household. Letters describing the project were sent to 715 potentially eligible families and trained research assistants followed up with phone calls to assess eligibility and invite participation. The families were told that this was a study of the experience of siblings of children with cancer, their cancer-related beliefs, and adjustment. A total of 484 families did not meet eligibility criteria and an additional 63 could not be reached by phone for screening. For eligible, interested families, data collection home visits were scheduled. During these visits, informed consent and child assent were obtained and the siblings completed the measures in the order presented below. Most participating siblings completed questionnaires independently, however, research assistants did read items aloud to a few of the younger participants as they followed along with the questions and recorded their responses.
Measures
Child PTSD Symptom Scale (CPSS; Foa et al., 2001)
This 26-item self-report measure for children aged 8 to 18 parallels the diagnostic criteria for PTSD included in the DSM-IV. To ensure siblings responded related to their brother or sister's cancer, the following phrase was added to the instructions, “When/Since your brother or sister was diagnosed with cancer: …” Also, two items were added to the form (i.e. “Did you think that his or her life was in danger?” and “Did you feel intense fear, horror, or helplessness?”) to ensure that criterion A2 of the DSM-IV criteria for PTSD was assessed. On this measure, symptom items are rated on a 4-point scale (0 = “not at all” to 3 = “5 or more times a week”). A total symptom severity score is calculated (range = 0 to 51) with higher scores indicating greater PTS symptom severity. In our sample, coefficient alpha for the symptom scale was good at .89. Moderate to severe PTS is indicated by a cut-score of 11 or greater as recommended by the authors (Foa et al., 2001) based upon sensitivity (95%) and specificity (96%) for predicting cases of PTSD determined by the Child Post-Traumatic Stress Disorder Reaction Index. Respondents also indicate on the CPSS whether or not the rated problems have interfered with their functioning in the past month in each of seven specified domains (i.e., chores, relationships with friends, prayers, fun activities, schoolwork, relationships with family, and general happiness). The specific items reported on the CPSS were also used to determine which participants had a constellation of symptoms consistent with DSM-IV criteria for PTSD.
Revised Children's Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1985)
This standardized self-report measure assesses anxiety for children and adolescents from 6 to 19 years of age. Participants read 37 items that describe how people think or feel and indicate which are true for them. The number of “yes” responses on the 28 items comprising the Total Anxiety scale are counted and converted to an age and gender-based T-score (M = 50, SD = 10), with higher scores indicating higher levels of anxiety. The clinical range is defined as T-scores ≥ 70. Internal consistency using a Kuder-Richardson 20 coefficient for dichotomous data was .87 in our study.
Children's Depression Inventory- Short Form (CDI-Short Form; Kovacs, 1992)
This 10-item self-report inventory assesses behavioral and cognitive symptoms of depression. Responses to items indicate levels of symptomatology: 0 = absence of the symptom, 1 = mild or probable presence, 2= definite presence. Raw scores are converted to T-scores, with higher scores indicating increasingly severe depressive symptoms. The clinical range is defined as T-scores ≥ 70. The alpha reliability coefficient was .78 in our sample.
Statistical Approach
To gauge whether childhood cancer is perceived as traumatic for siblings, the percentage of the sample fulfilling individual and full symptom criteria for PTSD as defined in the DSM-IV (and listed in Table 1) per their responses on the CPSS were calculated; that is, at least one symptom of re-experiencing (Criterion B), three symptoms of avoidance (Criterion C) and two symptoms of arousal (Criterion D) reported as occurring at least “about once per week” over the course of at least one month (Criterion E) and interfering with functioning (Criterion F). We also calculated the percentage fulfilling all of the above criteria plus criterion A2 (i.e., perceived threat to the life of the child with cancer and intense fear, horror or helplessness). The percentage of siblings with moderate to severe PTS (i.e., CPSS score > 11) was also calculated.
Table 1. Percentage (n) of the Total Sample, and Female and Male Subgroups, Meeting DSM-IV PTSD Criteria.
| PTSD Criterion | Total Sample (N = 125) | Females (n = 63) | Males (n = 62) |
|---|---|---|---|
| A. Threat of death (to child with cancer) and feelings of intense fear, horror, or helplessness | 42% (52) | 44% (28) | 39% (24) |
| B. At least 1 re-experiencing symptom | 90% (112) | 91% (57) | 89% (55) |
| C. At least 3 avoidance symptoms | 56% (70) | 51% (32) | 61% (38) |
| D. At least 2 arousal symptoms | 82% (102) | 86% (54) | 77% (48) |
| E. Symptoms lasting for 1 month or more | 68% (83) | 71% (45) | 64% (38) |
| F. Symptoms interfere with functioning | 72% (90) | 67% (42) | 77% (48) |
| Full PTSD Criteria | 22% (28) | 29% (18) | 16% (10) |
To characterize PTS reactions, the percentage of siblings reporting each symptom at each level of frequency was calculated, graphed, and summarized. The percentages of our sample indicating that PTS symptoms interfered with functioning in each of the areas of functioning listed on the CPSS were also calculated.
To examine comorbidity with anxiety and depression, three methods were used. First, siblings fulfilling criteria or meeting the cut-off for moderate to severe PTS were compared to their counterparts on anxiety and depression scores using independent group t-tests. Second, correlations were calculated between PTS scores and anxiety and depression scores. Third, Pearson Chi-square was used to explore overlap in the distribution of siblings falling into the clinical ranges for anxiety, depression, and PTS/PTSD.
Gender differences in the percentage of siblings fulfilling criteria for PTSD were evaluated with Pearson Chi-square and gender differences in PTS scores were evaluated with independent samples t-tests. To examine age differences, ages were compared between siblings fulfilling criteria for PTSD or scoring above the PTS cut-score to siblings who did not via independent t-tests and age was correlated with PTS scores using Pearson correlations. To account for multiple t-test and Chi-square analyses, our criterion for statistical significance was set at .01.
Results
Is Childhood Cancer a Potentially Traumatic Event for Siblings?
One third of our sample (34%, n = 42) met symptom criteria for PTSD at the time of the study based upon their CPSS responses. When requiring report of perceived life threat and feelings of intense fear, horror, or helplessness, just over one fifth (22%; n = 28) of the siblings met full criteria for PTSD (see Table 1). Three fourths of our sample (77%; n = 96) reported they thought their brother or sister's life was in danger when hearing the cancer diagnosis or at some point since that time. Nearly half (48%; n = 59) indicated that they felt intense fear, horror, or helplessness related to the cancer. A full sixty percent of our sample reported moderate to severe posttraumatic stress reactions (n = 75). PTS total scores ranged from 0 – 40, (out of 51 possible points) with the mean level of PTS falling above the cut-score for moderate PTS (M = 14.3, SD = 9.4; cut-score = 11). Four siblings (3%) reported no PTS symptoms in the past month.
Which PTS Symptoms do Siblings Experience?
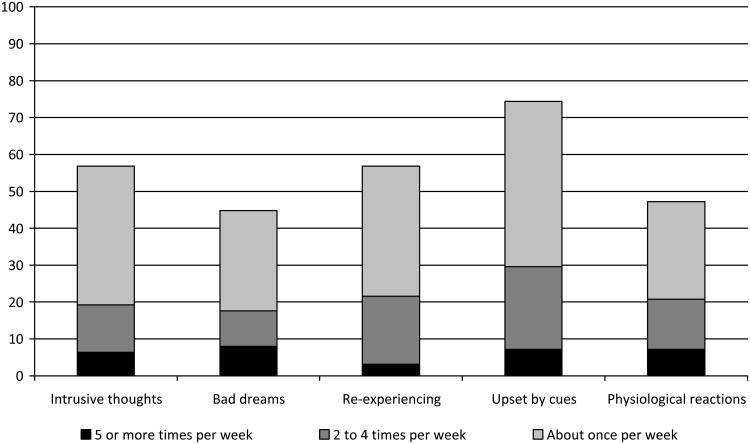
A total of 90% (n = 112) of our sample reported at least one symptom of re-experiencing, meeting criterion B for PTSD. As depicted in Figure 1, the most common re-experiencing symptom was “Feeling upset when you think about or hear about the cancer (for example, feeling scared, angry, sad, guilty, etc.)” with three fourths of our sample (74%, n = 93) indicating that they experienced this symptom more than “about once per week” in the past month and thirty percent (n = 37) indicating that they experienced it two or more times per week.
Figure 1.
Percentages of sample reporting each symptom within PTSD Criterion B (Re-Experiencing) by frequency of occurrence.
Over half of our sample (56%, n = 70) reported three or more symptoms of avoidance meeting criterion C for PTSD. As illustrated in Figure 2, “Trying not to think about, talk about, or have feelings about the cancer,” was most frequently reported. Seventy percent (n = 88) of our sample reported experiencing this symptom more than “about once per week” and 40% (n = 50) indicated that they experienced it two or more times per week in the past month.
Figure 2.
Percentages of sample reporting each symptom within PTSD Criterion C (Avoidance) by frequency of occurrence.
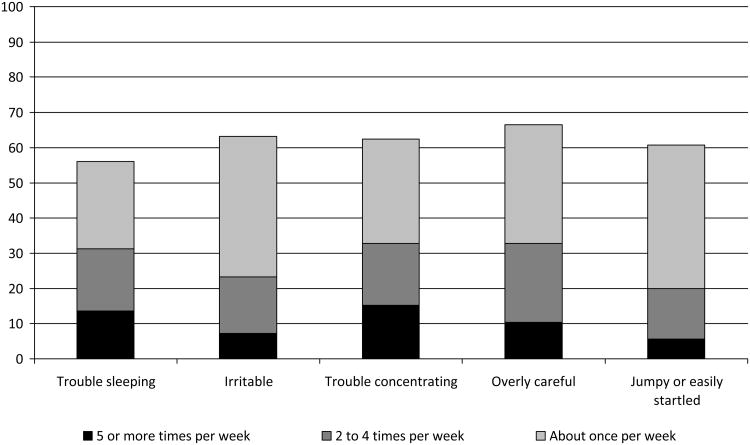
A total of 82% (n = 102) of our sample met criterion D for PTSD, reporting at least two symptoms of arousal. Two-thirds of our sample reported “Being overly careful, for example, checking to see who and what is around” (66%; n = 83), “Feeling irritable or having fits of anger” (63%, n = 79), “Having trouble concentrating” (62%, n = 78), and “Being jumpy or easily startled” (61%, n = 76) at a rate of “about once per week.” One third of the sample reported having trouble concentrating (33%, n = 41), being overly careful (33%, n = 41), and having trouble falling or staying asleep (31%, n = 39) at least twice a week during the past month.
Do PTS Symptoms Interfere with Functioning?
Nearly three fourths (74%, n = 90) of siblings with at least one symptom of PTS (n = 121) indicated that symptoms interfered with their functioning in at least one domain listed on the CPSS. Almost half (47%; n = 57) indicated that PTS symptoms interfered with their general happiness, and 36-42% indicated that PTS interfered with other areas of functioning including: fun and hobbies (42%; n = 51), school (41%; n = 50), chores or duties at home (37%; n = 45); friendships (37%; n = 45); and family relationships (36%; n = 43).
Are Anxiety and Depression related to PTS reactions?
T-tests demonstrated that siblings meeting full criteria for PTSD had higher self-reported anxiety (Ms [SDs] = 58.2 [11.5] vs. 48.1 [9.7]; t [123] = 4.7, p < .001) and depression (Ms [SDs] = 54.1 [11.0] vs. 46.5 [7.5]; t [123] = 4.2, p < .001) than siblings who did not meet criteria. Similarly, siblings above the cut-score for moderate to severe PTS had higher self-reported anxiety (Ms [SDs] = 55.1 [9.6] vs. 43.2 [8.8]; t [123] = 7.0, p < .001) and depression (Ms [SDs] = 51.2 [9.8] vs. 43.8 [5.1]; t [123] = 4.9, p < .001) than siblings who did not exceed the cut-off. Cancer-related PTS and anxiety scores were correlated at .69 (p < .001) and cancer-related PTS and depression scores were correlated at .59 (p < .001).
Consistent with previous literature, only 5% of our sample (n = 6) fell into the clinical range for self-reported anxiety (RCMAS: T-scores ranged from 18 – 87; M = 50.4, SD = 10.9; raw scores ranged from 0 - 27; M = 11.1, SD = 6.2) and only 3% (n = 4) fell into the clinical range for self-reported depression (CDI: T-scores ranged from 39 – 90; M = 48.2, SD = 9.0; raw scores ranged from 0 - 15; M = 2.7, SD = 2.9). However, of the six siblings in the clinical range for self-reported anxiety, five (83%) also met criteria for PTSD (χ2 [N=125] = 7.1, p < .01). Of the four siblings who fell into the clinical range for self-reported depression, two (50%) met full criteria for PTSD (χ2 [N=125] = 0.2, p = .18). One sibling's responses fell into the clinical range for both anxiety and depression and this individual also fulfilled criteria for PTSD.
Gender and Age Differences in PTS Reactions
Although nearly twice as many girls (29%) than boys (16%) fulfilled full criteria for PTSD, the distribution of cases was not significantly related to gender (χ2 [N = 125] = 2.8, p = .10). This pattern held true for each of the PTSD symptom criteria (χ2s [Ns = 125] < 1.4, ps > .23); the percentages are included in Table 1. Exactly the same percentage of girls and boys exceeded the clinical cut-off for PTS (30%). T-tests comparing girls (M = 14.7; SD = 10.1) and boys (M = 13.9; SD = 8.7) on PTS scores also revealed no significant differences (t[123] = .47, p = .64).
Siblings fulfilling criteria for PTSD did not differ in age (M = 13.5 years, SD = 2.7) from siblings who did not fulfill full criteria (M = 12.1 years, SD = 2.8; t[123] = 2.28, p = .02). Age differences were also not evident for the individual PTSD criteria (ts [123] < 1.88, ps > .06) except for criterion E (i.e., experiencing symptoms for at least one month); siblings experiencing symptoms for a month or more were older than siblings who did not (Ms [SDs] = 13.0 [2.9] vs. 11.2 [2.4]; t [120] = 3.4, p < .005). There was no apparent age difference between siblings scoring above versus below the cut-score for moderate to severe PTS (Ms [SDs] = 12.7 [2.9] vs. 12.0 [2.7]; t [123] = 1.2, p = .23) and age was not correlated with PTS scores (r = .03, p = .71).
Discussion
The findings of this study add to the literature regarding the adjustment of siblings of children with cancer by demonstrating noteworthy levels of cancer-related traumatic stress. More than half (60%) of the siblings in our sample reported experiencing moderate to severe levels of PTS with nearly one quarter (22%) fulfilling strict full criteria for PTSD. These numbers highlight the need for attention to the adjustment of siblings of children with cancer and the development of interventions to address their cancer-related distress.
These rates of moderate to severe PTS are higher than rates reported in previous studies of siblings of children with cancer (Alderfer et al., 2003, Packman et al., 1997; 2004), probably because the siblings in our sample had a brother or sister still on treatment (up to 38 months post-diagnosis) or off-treatment but within 2 years of diagnosis. Previous work used samples farther from the time of diagnosis. Research with both adolescents with cancer and their parents has demonstrated cross-sectionally that those closer to the time of diagnosis report more PTS symptoms than those farther from diagnosis (e.g., Phipps, Long, Hudson & Rai, 2005). In a study of parents of children with cancer still on treatment, 68% of mothers and 57% of fathers reported moderate to severe PTS reactions on a self-report questionnaire (Kazak, Boeving, Alderfer, Hwang & Reilly, 2005); these rates are quite similar to the rate we found for siblings in our sample. Studies of “cases” of PTSD drawn from self-report questionnaires of parents of children with cancer still on treatment have been reported to be 13% (Jurbergs, Long, Ticona & Phipps, 2009); 22-28% (Poder et al., 2008); 23% (Lindahl Norberg, Lindblad, & Bowman, 2005) and 44% (Landolt et al., 2003). Weighted by the number of subjects in these samples, the average rate is 28%; again, this rate is similar to the rate in our sample.
Previous studies have not examined whether and what percentage of siblings fulfills criteria for cancer-related PTSD. Self-report questionnaires are not ideal for this purpose and typically overestimate the incidence of PTSD compared to structured clinical interviews (e.g., Griffin, Uhlmansiek, Resick, & Mechanic, 2004) in part because questionnaires typically only focus upon the presence or absence of PTS symptoms, not perceptions of the potentially traumatic event, the duration of symptoms, or whether the symptoms interfere with functioning. We added two questions to the CPSS to ensure that we assessed all aspects of DSM-IV PTSD criteria and found that 22% of our sample met criteria in the past month. In the general population, it is estimated that 6% of youth will meet criteria for PTSD at some point in time by the age of 18 (Pfefferbaum, 1997); our rates of PTSD seem elevated in comparison to these norms.
The most commonly reported cancer-related PTS symptoms were “Feeling upset when you think about or hear about the cancer (for example, feeling scared, angry, sad, guilty, etc.)” and “Trying not to think about, talk about, or have feelings about the cancer.” Symptoms of arousal were also frequently and quite consistently reported with 56-66% of the sample indicating irritability, problems sleeping and concentrating, and being overly careful and jumpy or easily startled. Given the high rates of cancer-related PTS and the specific content of the most frequently reported symptoms, plus the fact that part of our sample were families of children still on cancer treatment, it is important to note that in these symptoms may reflect normative responses (e.g., feeling upset) and attempts to cope (e.g., avoidance) with the extreme stressor that is childhood cancer. General conceptualizations of traumatic stress are moving toward the interpretation of such symptoms as part of an adaptive process (e.g., Kassam-Adams, 2006; Noll & Kupst, 2007), even though they may be distressing. Indeed, the distress associated with PTS may communicate to others in one's social network that support is needed to adapt to the stressor. Furthermore, intrusive thoughts may reflect ongoing cognitive processing of the event, avoidance may allow for a break from reminders of the event and allow resumption of other necessary tasks, and increased physiological arousal may prime an individual to quickly recognize and respond to additional threats. It is only when these symptoms are persistent and cause clinically significant distress or impairment in social, occupational, or other important areas of functioning, that they represent a true disorder.
Nearly three fourths of siblings in our sample reporting PTS symptoms indicated that they interfered with functioning in at least one domain of their lives. Furthermore, participants reported declines in functioning without displaying a full constellation of PTSD symptoms. While we believe that the siblings in our study answered this question about whether or not their PTS symptoms interfered with their functioning honestly, in hindsight, we wonder if indeed this question assesses true impairment in functioning as outlined by DSM-IV criteria. A more objective assessment of the siblings' functioning, using multi-informant reports from parents, peers or teachers may have been more useful. Still, our data demonstrate that most siblings perceived that cancer-related symptoms of PTS got in the way of their day-to-day lives.
Our study also revealed that cancer-related posttraumatic stress reactions are accompanied by symptoms of general anxiety and depression, which is consistent with the broader PTSD literature (e.g., Copeland, Keeler, Angold & Costello, 2007). While clinically significant levels of anxiety and depression were rare in our sample, nearly all of the children falling into the clinical range for anxiety also met full criteria for cancer-related PTSD. The overlap between clinically significant levels of depressive symptoms and cancer-related PTSD, however, was not statistically significant. This pattern of findings is consistent with the DSM-IV grouping of PTSD among anxiety disorders.
We did not find a significant relationship between gender and PTS/PTSD. This finding was surprising given past studies suggest females are more likely to experience traumatic stress reactions in response to a range of traumatic events (e.g., Breslau, 2009) including childhood cancer in a brother or sister (Alderfer et al., 2003). Similarly, despite our wide age range (8-17), we did not uncover consistent age-related differences in PTS reactions. These findings suggest that gender and age might not be adequate markers of subgroups of siblings at greater risk for PTS reactions. In an effort to identify siblings at greatest risk for cancer-related PTS, further research is needed to examine other potential predictors such as individual temperament (e.g, Phipps, Jurberg, & Long, 2009) or family factors such communication patterns, problem solving abilities, or affective tone (e.g., Alderfer, Navsaria, & Kazak, 2009).
The findings of this study need to be considered within the context of its limitations. First, this study was framed as a study of siblings of children with cancer and we specifically asked participants to focus on their experience with cancer when responding to the traumatic stress measure. Research demonstrates that focusing individuals on a specific aspect of their life through either study framing or the order of questions may impact findings (e.g., Smith, Schwarz, Roberts & Ubel, 2006; Strack, Martin & Schwarz, 1996). The results that we obtained in our study reflect the responses of siblings of children with cancer when they are thinking about cancer and their role as a sibling of a child with cancer. These factors may not be salient to siblings of children with cancer most of the time, suggesting the possibility that their responses may not reflect their overall general level of functioning. Further research using a broader framework, not restricted to adjustment in the context of cancer, and research into the general salience of cancer in the lives of these siblings would be informative.
A second limitation of the study is that all of the measures used were questionnaires. The gold standard for assessing PTSD is a structured clinical interview administered by a trained clinician. Individuals completing a questionnaire may not interpret questions consistent with the nature of the clinical criterion it is designed to assess. That said, we did choose a self-report questionnaire with strong psychometric properties and ensured that we assessed all aspects of the DSM-IV PTSD criteria by adding two items. Furthermore, in addition to exploring rates of cancer-related PTSD we used the well-established cut score on the CPSS to calculate and report upon the percentage of our sample scoring in the moderate to severe range for PTS.
Third, although our sample was relatively homogenous compared to past sibling studies, we still had heterogeneity in our sample in regard to treatment status. Some of the siblings in our sample had brothers or sisters still on treatment while others' brothers or sisters had already completed treatment. This heterogeneity raises two issues. First, on a conceptual level, measuring posttraumatic stress symptoms while related stressors are ongoing may appear questionable. However, this practice is common (e.g., Jurbergs et al., 2009; Kazak et al., 2005; Phipps et al., 2005; Poder et al., 2008) and acceptable within the DSM-IV PTSD framework as long as 30 days has passed since the initiation of the potentially traumatic event. This approach is justified in that symptoms emerge during ongoing traumatic events and uncovering such symptoms early may allow for intervention and prevention of prolonged, chronic reactions (Kazak et al., 2006).
In addition, our methods did not allow for comparisons between the traumatic stress reactions of siblings of children with cancer on versus off-treatment, as we did not assess or record whether the child with cancer was on or off-treatment if the family was within 2 years of diagnosis. We also did not assess medical status (e.g., active disease, remission, relapse, recurrence), severity of illness/prognosis, frequency of clinic visits or hospitalizations, or treatment intensity. Future research is needed to determine if these factors relate to cancer-related PTS reactions of siblings of children with cancer. Identifying such moderators and/or predictors of posttraumatic stress reactions may help efforts to conduct appropriate screening, channel scarce psychosocial resources, and develop specific cancer-related traumatic stress interventions.
Lastly, we appreciate that there is a range of responses to potentially traumatic events including resilience and growth (e.g., Barakat, Alderfer & Kazak, 2006; Bonanno & Mancini, 2010; Currier, Hermes & Phipps, 2009); however, we did not assess these responses in the current study. Qualitative studies of siblings of children with cancer reveal themes of increased empathy, compassion, maturity and growth (see Alderfer et al, 2008 for a review; Kamibeppu et al., 2011) and studies of posttraumatic growth and benefit finding among siblings of children with cancer are needed.
In conclusion, many siblings of children with cancer experience cancer-related distress that can be conceptualized within a posttraumatic stress framework. Educational information should be provided to families of children with cancer, educators and others who may interact with siblings of children with cancer so that they become aware that cancer can greatly impact healthy siblings within the family, help identify siblings experiencing cancer-related traumatic stress symptoms, and suggest further evaluation and treatment. Future research is needed to assess cancer-related PTS reactions in siblings over time. Such research could isolate factors capable of distinguishing subgroups of siblings experiencing normative, temporary PTS reactions that are part of an adaptive process from those siblings who experience unremitting symptoms that substantially interfere with functioning. Siblings at greatest risk may include those with a previous exposure to trauma and high levels of anxiety (Copeland et al., 2007; Ozono et al., 2007). Further exploration of characteristics such as temperament, disease-related factors such as duration and intensity of cancer treatment, and ecological factors related to the family, hospital, peer, and school systems may assist in identifying risk and protective factors for these siblings.
For children with cancer-related PTSD empirically-based treatment is needed. Trauma-focused cognitive behavioral therapy is a well-established intervention for children and adolescents with PTSD with evidence of long-term success (see Silverman et al., 2008 for a review); however this therapy has not been empirically evaluated for siblings within the context of childhood cancer. Because childhood cancer is a family-level stressor, family-based multi-systemic interventions may be particularly useful in this population (e.g., Walsh, 2007) and empirical evidence is emerging for such models (e.g., Kazak, Alderfer, Streisand et al., 2004). While there is limited evidence to support the use of psychotropic medication in children with PTSD, in children with persistent symptoms or co-morbid anxiety and depression, medication may be useful (Cohen, Mannarino, Perel, & Staron, 2007; Donnelly, 2003).
Even for siblings without PTSD, support services are warranted. This may be particularly difficult given the economic realities present in most cancer centers and the fact that siblings may not regularly interface with the medical and psychosocial care teams at the hospital. However, screening of siblings should be an element of family-based pediatric cancer care with referrals to the community as needed (Alderfer & Noll, 2006). Activating support services for siblings within their existing social networks, such as school-based counselors may be helpful (Alderfer & Hodges, 2010). Furthermore, siblings can draw support from community-based organizations such as SuperSibs!, a national non-profit foundation designed to honor, support and recognize siblings of children with cancer (www.supersibs.org).
Figure 3.
Percentages of sample reporting each symptom within PTSD Criterion D (Arousal) by frequency of occurrence.
Acknowledgments
This work was supported by grants from the National Institutes of Health [CA110926] and the American Cancer Society [MRSG 05-213] awarded to MAA; we acknowledge these agencies for their support. We also thank the families who participated and the “SIBS-C research team” including Stephanie Poulos-Hopkins and Camille Daniels. Specific thanks for input regarding this paper go to the members of the Writers' Seminar of The CHOP/PENN Mentored Psychosocial Research Curriculum, supported by a K05 (CA128805) awarded to Anne E. Kazak, Ph.D. Preliminary results of this work were presented at the 2007 Annual Convention of the American Psychosocial Association and 2008 National Child Health Psychology Conference.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its council of Editors disclaim any responsibility or liabilities for errors or emissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/fsh
Contributor Information
Lynne M. Kaplan, The Children's Hospital of Philadelphia
K. Julia Kaal, The Children's Hospital of Philadelphia.
Lauren Bradley, The Children's Hospital of Philadelphia.
Melissa A. Alderfer, The Children's Hospital of Philadelphia and Perelman School of Medicine, University of Pennsylvania
References
- Alderfer MA, Hodges JA. Supporting siblings of children with cancer: A need for family-school partnerships. School Mental Health. 2010;2:72–81. doi: 10.1007/s12310-010-9027-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderfer MA, Labay L, Kazak A. Brief report: Does posttraumatic stress apply to siblings of childhood cancer survivors? Journal of Pediatric Psychology. 2003;28:281–286. doi: 10.1093/jpepsy/jsg016. [DOI] [PubMed] [Google Scholar]
- Alderfer MA, Long KA, Lown EA, Marsland AL, Ostrowski NL, Hock JM, Ewing LJ. Psychosocial adjustment of siblings of children with cancer: A systematic review. Psycho-oncology. 2010;19:789–805. doi: 10.1002/pon.1638. [DOI] [PubMed] [Google Scholar]
- Alderfer MA, Navsaria N, Kazak AE. Family functioning and posttraumatic stress disorder in adolescent survivors of childhood cancer. Journal of Family Psychology. 2009;23:717–725. doi: 10.1037/a0015996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderfer MA, Noll RB. Identifying and addressing the needs of siblings of children with cancer. Pediatric Blood & Cancer. 2006;47:537–538. doi: 10.1002/pbc.20691. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [DOI] [Google Scholar]
- Barakat LP, Alderfer MA, Kazak AE. Posttraumatic growth in adolescent survivors of cancer and their mothers and fathers. Journal of Pediatric Psychology. 2006;31:413–419. doi: 10.1093/jpepsy/jsj058. [DOI] [PubMed] [Google Scholar]
- Barakat LP, Kazak AE, Meadows AT, Casey R, Meeske K, Stuber ML. Families surviving childhood cancer: A comparison of posttraumatic stress symptoms with families of healthy children. Journal of Pediatric Psychology. 1997;22:843–859. doi: 10.1093/jpepsy/22.6.843. doi:10.1093/ jpepsy/22.6.843. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD. Beyond resilience and PTSD: Mapping the heterogeneity of responses to potential trauma. Psychological Trauma: Theory, Research, Practice, and Policy. 2010 Nov 8; doi: 10.1037/a0017829. Advance online publication. [DOI] [Google Scholar]
- Breslau N. The epidemiology of posttraumatic stress disorder: What is the extent of the problem? Journal of Clinical Psychiatry. 2001;62:16–22. [PubMed] [Google Scholar]
- Breslau M. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse. 2009;10:198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- Brown RT, Madan-Swain A, Lambert R. Posttraumatic stress symptoms in adolescent survivors of childhood cancer and their mothers. Journal of Traumatic Stress. 2003;16:309–318. doi: 10.1023/A:1024465415620. [DOI] [PubMed] [Google Scholar]
- Butler RW, Rizzi LP, Handwerger BA. Brief report: The assessment of Posttraumatic Stress Disorder in pediatric cancer patients and survivors. Journal of Pediatric Psychology. 1996;21:499–504. doi: 10.1093/jpepsy/21.4.499. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Perel JM, Staron V. A pilot randomized controlled trial of combined trauma-focused CBT and sertraline for childhood PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(7):811–819. doi: 10.1097/chi.0b013e3180547105. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;65(5):577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Currier JM, Hermes S, Phipps S. Children's responses to serious illness: Perceptions of benefit and burden in a pediatric cancer population. Journal of Pediatric Psychology. 2009;34:1129–1134. doi: 10.1093/jpepsy/jsp021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly CL. Pharmacologic treatment approaches for children and adolescents with posttraumatic stress disorder. Child and Adolescent Psychiatric Clinics of North America. 2003;12(2):251–269. doi: 10.1016/S1056-4993(02)00102-5. [DOI] [PubMed] [Google Scholar]
- Eiser C, Hill JJ, Vance YH. Examining the psychological consequences of surviving childhood cancer: Systematic review as a research method in pediatric psychology. Journal of Pediatric Psychology. 2000;25:449–460. doi: 10.1093/jpepsy/25.6.449. [DOI] [PubMed] [Google Scholar]
- Goldenberg Libov B, Nevid JS, Pelcovitz D, Carmony TM. Posttraumatic stress symptomatology in mothers of pediatric cancer survivors. Psychology and Health. 2002;17:501–511. doi: 10.1080/0887044022000004975. [DOI] [Google Scholar]
- Griffin MG, Uhlmansiek MH, Resick PA, Mechanic MB. Comparison of the posttraumatic stress disorder scale versus the clinician-administered posttraumatic stress disorder scale in domestic violence survivors. Journal of Traumatic Stress. 2004;17(6):497–503. doi: 10.1007/s10960-004-5798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurbergs N, Long A, Ticona L, Phipps S. Symptoms of posttraumatic stress in parents of children with cancer: Are they elevated relative to parents of healthy children? Journal of Pediatric Psychology. 2009;34:4–13. doi: 10.1093/jpepsy/jsm119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamibeppu K, Sato I, Honda M, Ozono S, Sakamoto N, Iwai T, Ishida Y. Mental health among young adult survivors of childhood cancer and their siblings including posttraumatic growth. Journal of Cancer Survivorship. 2010;4:303–312. doi: 10.1007/s11764-010-0124-z. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N. Introduction to the special issue: Posttraumatic stress related to pediatric illness and injury. Journal of Pediatric Psychology. 2006;31:337–342. doi: 10.1093/jpepsy/jsj052. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Alderfer MA, Rourke MT, Simms S, Streisand R, Grossman JR. Posttraumatic stress symptoms and Posttraumatic Stress Disorder in families of adolescent cancer survivors. Journal of Pediatric Psychology. 2004;29:211–219. doi: 10.1093/jpepsy/jsh022. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Alderfer MA, Streisand R, Simms S, Rourke M, Barakat L, Gallagher P, Cnaan A. Treatment of posttraumatic stress symptoms in adolescent survivors of childhood cancer and their families: A randomized clinical trial. Journal of Family Psychology. 2004;18:493–504. doi: 10.1037/0893-3200.18.3.493. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Boeving CA, Alderfer MA, Hwang WT, Reilly A. Posttraumatic stress symptoms (PTSS) during treatment in parents of children with cancer. Journal of Clinical Oncology. 2005;23:7405–7410. doi: 10.1200/JCO.2005.09.110. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Kassam-Adams N, Schneider A, Zelikovsky N, Alderfer MA, Rourke M. An integrative model of pediatric medical traumatic stress. Journal of Pediatric Psychology. 2006;31:343–349. doi: 10.1093/jpepsy/jsj054. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Vollrath M, Ribi K, Gnehm HE, Sennhauser FH. Incidence and associations of parental and child posttraumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry. 2003;44:1199–1207. doi: 10.1111/1469-7610.00201. [DOI] [PubMed] [Google Scholar]
- Lindahl Norberg A, Lindblad F, Boman KK. Parental traumatic stress during and after paediatric cancer treatment. Acta Oncologica. 2005;44:382–388. doi: 10.1080/02841860510029789. doi:10.1080/ 02841860510029789. [DOI] [PubMed] [Google Scholar]
- Nolbris M, Enskar K, Hellstrom A. Experience of siblings of children treated for cancer. European Journal of Oncology Nursing. 2007;22:227–233. doi: 10.1016/j.ejon.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Noll R, Kupst M. The psychological impact of pediatric cancer: Hardiness, the exception or the rule? Journal of Pediatric Psychology. 2007;32:1089–1098. doi: 10.1093/jpepsy/jsm049. [DOI] [PubMed] [Google Scholar]
- Ozono S, Saeki T, Mantani T, Ogata A, Okamura H, Yamawaki S. Factors related to post-traumatic stress in adolescent survivors of childhood cancer and their parents. Support Care Cancer. 2007;15:309–317. doi: 10.1007/s00520-006-0139-1. [DOI] [PubMed] [Google Scholar]
- Packman W, Crittenden M, Schaeffer E, Bongar B, Rieger Fischer J, Cowan M. Psychosocial consequences of bone marrow transplantation in donor and nondonor siblings. Journal of Developmental & Behavioral Pediatrics. 1997;18:244–253. doi: 10.1097/00004703-199708000-00004. [DOI] [PubMed] [Google Scholar]
- Packman W, Fine J, Chesterman B, VanZutphen K, Golan R, Amylon M. Camp Okizu: Preliminary investigation of a psychological intervention for siblings of pediatric cancer patients. Children's Health Care. 2004;33:201–215. doi: 10.1207/s15326888chc3303_3. [DOI] [Google Scholar]
- Pelcovitz D, Goldenberg B, Kaplan S, Weinblatt M, Mandel F, Meyers B, Vincinguerra V. Posttraumatic stress disorder in mothers of pediatric cancer survivors. Psychosomatics. 1996;37:116–126. doi: 10.1016/S0033-3182(96)71577-3. [DOI] [PubMed] [Google Scholar]
- Pelcovitz D, Goldenberg Libov B, Mandel F, Kaplan S, Weinblatt M, Septimus A. Posttraumatic stress disorder and family functioning in adolescent cancer. Journal of Traumatic Stress. 1998;11:205–221. doi: 10.1023/A:1024442802113. [DOI] [PubMed] [Google Scholar]
- Phipps S, Jurbergs N, Long A. Symptoms of post-traumatic stress in children with cancer: Does personality trump health status? Psycho-Oncology. 2009;18:992–1002. doi: 10.1002/pon.1496. doi:10.1002/ pon.v18:910.1002/pon.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps S, Long A, Hudson M, Rai SN. Symptoms of post-traumatic stress in children with cancer and their parents: Effects of informant and time from diagnosis. Pediatric Blood & Cancer. 2005;45:952–959. doi: 10.1002/pbc.20373. [DOI] [PubMed] [Google Scholar]
- Poder U, Ljungman G, von Essen L. Posttraumatic stress disorder among parents of children on cancer treatment: a longitudinal study. Psycho-Oncology. 2008;17:430–437. doi: 10.1002/pon.1263. [DOI] [PubMed] [Google Scholar]
- Prchal A, Landolt MA. How siblings of pediatric cancer patients experience the first time after diagnosis. Cancer Nursing. 2012;35:133–140. doi: 10.1097/NCC.0b013e31821e0c59. [DOI] [PubMed] [Google Scholar]
- Silverman W, Ortiz C, Viswesvaran C, Burns B, Kolko D, Putnam F, Amaya-Jackson L. Evidence-based psychosocial treatment for children and adolescents exposed to traumatic events. Journal of Clinical Child & Adolescent Psychology. 2008;37:156–83. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Smith DM, Schwarz N, Roberts TR, Ubel PA. Why are you calling me? How study introductions change response patterns. Quality of Life Research. 2006;15:621–630. doi: 10.1007/s11136-005-4529-5. [DOI] [PubMed] [Google Scholar]
- Strack F, Martin L, Schwarz N. Priming and communication: Social determinants of information use in judgments of life satisfaction. European Journal of Social Psychology. 1996;18:429–442. doi: 10.1002/ejsp.2420180505. [DOI] [Google Scholar]
- Stuber ML, Christakis DA, Houskamp B, Kazak AE. Posttrauma symptoms in childhood leukemia survivors and their parents. Psychosomatics. 1996;37:254–261. doi: 10.1016/S0033-3182(96)71564-5. [DOI] [PubMed] [Google Scholar]
- Walsh F. Traumatic loss and major disasters: Strengthening family and community resilience. Family Process. 2007;46:207–227. doi: 10.1111/j.1545-5300.2007.00205.x. [DOI] [PubMed] [Google Scholar]
- Wilkins K, Woodgate R. A review of qualitative research on the childhood cancer experience from the perspective of siblings: A need to give them a voice. Journal Pediatric Oncology Nursing. 2005;22:305–319. doi: 10.1177/1043454205278035. [DOI] [PubMed] [Google Scholar]