Abstract
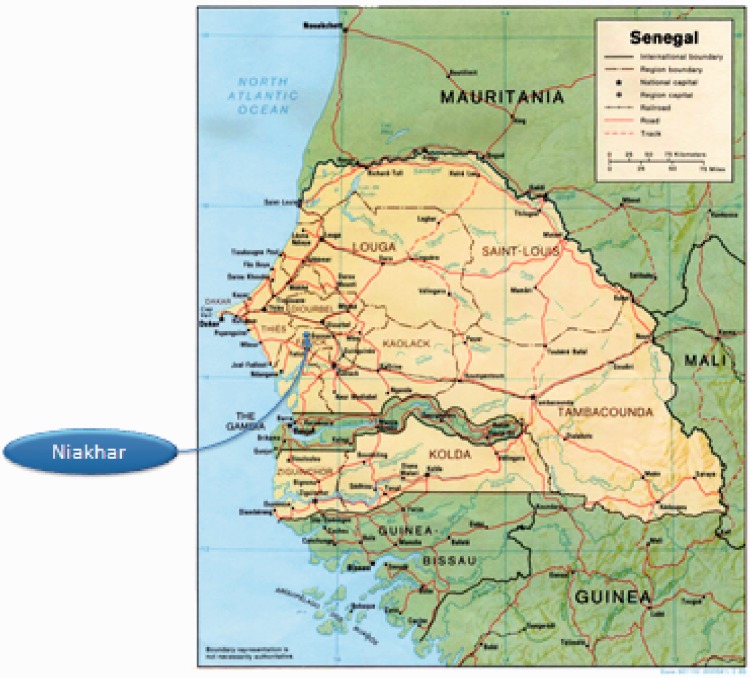
The Health and Demographic Surveillance System (HDSS) in Niakhar, a rural area of Senegal, is located 135 km east of Dakar. The HDSS was established in 1962 by the Institut de Recherche pour le Développement (IRD) of Senegal to face the shortcomings of the civil registration system and provide demographic indicators.
Some 65 villages in the Niakhar area were followed annually by the HDSS from 1962–1969. The study zone was reduced to 8 villages from 1969–1983, and from then on the HDSS was extended to include 22 other villages, covering a total of 30 villages for a population estimated at 43 000 in January 2012. Thus, 8 villages in the Niakhar area have been under demographic surveillance for almost 50 years and 30 villages for 30 years.
Vital events, migrations, marital changes, pregnancies, and immunizations are routinely recorded every 4 months. The HDSS data base also includes epidemiological, economic, and environmental information obtained from specific surveys. Data were collected through annual rounds from 1962 to 1987. The rounds became weekly from 1987–1997, followed by routine visits conducted every 3 months between 1997 and 2007 and every 4 months since then. The data collected in the HDSS are not open to access, but can be fairly shared under conditions of collaboration and endowment.
Why was the HDSS set up?
In the mid-twentieth century very few studies dealt with African populations. In the era before the independence of Senegal in 1960, and that of other African countries, demographic statistics were based on census and vital-registration data for European populations living in Africa. Data relative to African populations were based only on civil-registration systems in cities and parish-register data in rural areas. In Senegal, the first national demographic survey was conducted in 1960–1961 as part of the World Fertility Surveys. To face the important limitations of retrospective data and meet the data requirements of the first Economic and Social Plan for 1961–1964, some researchers suggested a follow-up system based on repeated surveys of 50 000 individuals in a rural area of Senegal. After 3 years of follow-up, researchers concluded that the previous surveys underestimated about 13% of births and 40% of infant mortality.1
The collection of demographic data was begun by Pierre Cantrelle in December 1962.2 The rationale for setting up the HDSS was to demonstrate the capacity to record reliable demographic and epidemiological data in rural areas of Africa.
At the time, the Sine-Saloum region was a populous area in Senegal. Two areas were selected to study contrasting demographic patterns. The Niakhar area, with a higher population density, was homogenous in terms of cultural, social, and economic patterns. The Paos-Koto area, less inhabited, included different ethnic groups. Some 65 villages were surveyed in Niakhar and 135 villages were surveyed in Paos-Koto. In 1969, budget cuts led to a reduction of the number of villages, to only 8 villages in Niakhar, in what was designated the ‘Ngayokhem area’, and 30 villages in Paos-Koto, designated the ‘Ndemen area’, continued to be followed. In 1982, a research team headed by Michel Garenne focused on demographic, epidemiological, and anthropological factors affecting child mortality.3 A study was conducted from 1983–1986 to better understand the relationship between nutritional status and mortality.3 To meet the needs of this study, the Ndemen area was abandoned in 1983 and the Ngayokhem area was expanded to include 30 villages, becoming the current Niakhar Health and Demographic Surveillance System (Niakhar HDSS) (Table 1). For the period 1962–1982, the available data came from the Ngayokhem area (8 villages), and beginning in 1983 from the Niakhar area (30 villages, including the Ngayokhem area).
Table 1.
Main stages of the Niakhar HDSS
| Observation period | Location | Number of villages | Population |
|---|---|---|---|
| December 1962 – February 1969 | Niakhar | 65 | 35 187 |
| Paos-Koto | 135 | 18 988 | |
| March 1969 – February 1983 | Ngayokhem | 8 | 4300 |
| Ndemen | 30 | 6000 | |
| March 1983 – Present | Niakhar | 30 | 23 000 (1983) |
| 43 000 (2012) |
Where is the HDSS area?
The study zone of the Niakhar HDSS is located at 14.5°N Latitude and 16.5°W Longitude in the department of Fatick (Sine-Saloum), 135 km east of Dakar, Senegal. The Niakhar study zone covers 203 km2 and is located in the continental Sahelian-Sudanese climatic zone. For 30 years the region in the study zone has suffered from drought. The average annual rainfall decreased from 800 mm in the 1950s to 500 mm in the 1980s. Increasing amounts of precipitation have been observed since the mid-2000s, with an average annual rainfall of 600 mm between 2005 and 2010.
Who is covered by the HDSS and how often have they been followed up?
In 2012, the HDSS in the Niakhar area covered a population of about 43 664 with a population density of about 214 per km2 residing in 30 villages of varying size. Although the area is rural, the three largest villages can be considered as semi-urbanised and include health facilities, a weekly market, daily buses to Dakar, and several shops. The Sereer ethnic group account for 96.7% of the population. The other ethnic groups present in the area are the Wolof (1.0%), Toucouleur (1.0%), and Laobe (0.5%), as well as the Peuhl, Moorish, Soce, and Diola (0.8%). The main religious groups in this area are Muslim (77.3%) and Christian (19.6%). Only 2.6% of the area population report practising animism, although it is deeply rooted in family traditions. The dominant language used is Sereer, but many people speak Wolof. Millet and groundnut are respectively the main staple and cash crops. Peasants also rear livestock. The agricultural crisis in Sahel and the demographic pressure have led to the development of new activities, such as meat production, and to temporary rural–urban migrations. The education level is very low: 50% of men and 75% of women between the ages of 15 and 24 years had no school-based education in 2000. The residential unit in the study area is the compound, which is composed of one or several households together with some members of the extended patrilineal family. The traditional houses are huts, which tend to be replaced by houses of modern construction made of concrete and corrugated iron. The availability of bore holes and drinking fountains has increased over the past several decades, and in 2003, 60% of households had access to tap water (inside or outside the house). The use of latrines is more recent: only 22% of households had access to sanitation in 2003. There is no electricity apart from that in three villages (Diohine, Toucar, and Ngayokhem), where it has been available since the early 2000s. Paved roads are 15 to 30 km away from the villages, but several daily bus or taxi services to Dakar are offered.
Individual characteristics (sex, age, ethnic group, religion, marital status) are collected for each resident in the study area. A resident is defined as a person who usually lives in the household. Migrations into and out of the study area are recorded after 6 months of presence or absence in the area. The exceptions to this general rule concern persons who migrate because of temporary work, who are considered residents if they come back to their village for at least 1 month per year. Absent workers with a family (wife and children) that lives in the village and absent students who are reported as family members are also considered residents.
What has been measured and how have the Niakhar HDSS databases been constructed?
The Niakhar HDSS collects, as basic data for each resident: individual, household, and compound identifying information; identification of the resident’s mother and father; relationship of the individual to the head of household; and the individual’s spousal relationship. From 1983, the HDSS routinely monitored deaths, pregnancies, births, miscarriages, stillbirths, weanings, migrations, changes of marital status, immunizations, and cases of measles and whooping cough among residents of the study area. Verbal autopsies (VAs) have been conducted after all deaths except for those that occurred between 1999 and 2004, during which period only the deaths of residents aged 0–55 years were investigated. The Niakhar HDSS also registers visitors as well as the demographic events related to them in cases of in-migration. Data about household characteristics (living conditions, domestic equipment, etc.) were collected in 1998 and 2003, and about community equipment (schools, boreholes, etc.) in 2003. Economic and environmental data will be collected in 2013. Table 3 presents further details on the data items collected. The interviewers for the Niakhar HDSS collect data with tablet-type personal computers carrying the most recently updated data base linked to a user-friendly interface indicating the household members of interviewees and the questionnaire to be completed. Daily updates of data are recorded on an external hard drive, and weekly synchronizations are scheduled during each round of data collection, which helps to update the HDSS data base and ascertain the consistency of data (i.e. residential relocations within the study area and marriages). Applications are written in Visual Basic.Net (Microsoft, Redmond, WA, USA) and the database is managed with Microsoft Access.
Table 2.
Projects of the Niakhar HDSS during the 5 past years
| Project title | Year | Partners |
|---|---|---|
| Clinical trials and medical research projects | ||
| Large-scale implementation of intermittent preventive treatment in children delivered through health services with community participation in the Sahel | 2008–2011 | Gates Foundation–IRD |
| Assessment of rapid diagnostic test, compliance and pharmacovigilance of artesunate plus amodiaquine malaria treatment in two areas in Senegal (Mlomp, Niakhar) | 2009 | PNLP–Global Fund–IRD |
| Assessment of the effectiveness of seasonal trivalent influenza vaccine among children in Senegal | 2009–2011 | CDC–PATH–IRD |
| Pilot study on the epidemiology of meningococcal carriage in countries of the African meningitis belt | 2010 | LSHTM–Wellcome Trust–IRD |
| Malaria in school-age children: epidemiological risk, disease burden and strategies for control | 2011–2012 | LSHTM–Wellcome Trust–IRD |
| The impact of meningococcal conjugate vaccination on pharyngeal carriage of serogroup A meningococci and on transmission of the infection | 2011–2012 | LSHTM–Wellcome Trust–IRD |
| Evaluation of the antibody persistence in African subjects up to five years after immunization with MenAfrivac, a meningococcal conjugate vaccine | 2011–2012 | PATH–IRD |
| Influenza surveillance to describe the epidemiology of influenza in tropical developing Africa and assess the long-term duration of vaccine protection | 2011–2013 | CDC–PATH–IRD |
| Assessment of the immunogenicity and safety of an MF-59 triva lent influenza vaccine and an unadjuvanted trivalent influenza vaccine among children in Senegal | 2012–2013 | CDC–PATH–IRD |
| Social sciences research projects | ||
| The Niakhar social networks and health project | 2012–2015 | NIH–University of Maryland–IRD |
| Validation of census and survey data used to estimate adult mortality in sub-Saharan Africa | 2012–2013 | INED-Columbia University- IRD-NIH-ANR |
| Household economic indicators (e.g. housing characteristics, household properties, access to water and electricity) | 2013 | IRD |
| Community equipment (drillings, wells, schools, places of worship, health-care facilities) | 2013 | IRD |
| Ecological surveillance (pluviometry, water quality, tree parks, biodiversity) | 2013–2014 | IRD |
Abbreviations: CDC, U.S. Centers for Disease Control and Prevention; IRD, France, Institut de Recherche pour le Developpement; PNLP, Senegal, Programme National de Lutte contre le Paludisme; PATH, international nonprofit organization; LSHTM, G.B. London School of Hygiene and Tropical Medicine; NIH, U.S. National Institutes for Health; ANR, France, Agence Nationale de la Recherche; INED, France, Institut National d'Etude Demographique.
Table 4.
Demographic characteristics of the Niakhar HDSS
| Characteristics | 1963–67a | 1968–72a | 1973–77a | 1984–88b | 1989–93b | 1994–98b | 1999–03b | 2004–08b | 2009–11b |
|---|---|---|---|---|---|---|---|---|---|
| Total population | 4455 | 4663 | 4667 | 23 824 | 25 743 | 28 412 | 30 863 | 35 582 | 40 687 |
| Male:female ratio per 100 | 93.2 | 93.3 | 91.0 | 95.6 | 97.5 | 98.6 | 98.4 | 98.1 | 98.5 |
| Population density per km2 | 101 | 106 | 106 | 117 | 127 | 140 | 152 | 175 | 13 |
| Population growth per 100 | 0.91 | 0.21 | 0.91 | 1.57 | 1.65 | 1.94 | 2.13 | 3.44 | 3.47 |
| Crude birth rate per 1000 | 46.8 | 48.4 | 49.5 | 50.4 | 46.0 | 41.8 | 41.9 | 41.1 | 40.1 |
| Crude death rate per 1000 | 36.7 | 33.6 | 30.6 | 23.2 | 16.4 | 16.8 | 14.2 | 9.5 | 6.2 |
| Crude in-migration rate per 1000 | 40.8 | 31.0 | 26.5 | 37.1 | 37.6 | 37.3 | 29.0 | 26.0 | 23.4 |
| Crude out-migration rate per 1000 | 51.3 | 45.4 | 57.1 | 49.0 | 51.0 | 43.4 | 35.5 | 23.6 | 23.1 |
| Total fertility rate (children per woman) | 6.9 | 6.9 | 6.8 | 7.9 | 7.7 | 7.0 | 6.9 | 6.7 | 6.4 |
| Neonatal Mortality per 1000 live births | 22.2 | 26.9 | 38.7 | 56.9 | 37.8 | 30.1 | 23.9 | 11.6 | 7.9 |
| Early neonatal mortality per 1000 live births | 29.4 | 23.4 | 18.5 | 17.6 | 9.3 | 6.1 | |||
| Infant Mortality per 1000 live births | 223 | 214 | 182 | 122.5 | 86.1 | 79.2 | 72.3 | 31.9 | 31.2 |
| Child Mortality per 1000 | 340 | 342 | 291 | 182.2 | 122.2 | 132.3 | 113.6 | 53.3 | 46.4 |
| Under-five mortality per 1000 live births | 485 | 480 | 421 | 282.4 | 198.8 | 201.0 | 177.7 | 83.5 | 76.2 |
| Male life expectancy at birth | 28.9 | 30.2 | 31.4 | 45.5 | 52.2 | 47.5 | 56.7 | 62.3 | 68.2 |
| Female life expectancy at birth | 30.4 | 30.4 | 36.3 | 49.0 | 55.6 | 52.6 | 60.8 | 66.1 | 69.1 |
aEight villages (Ngayokhem area).
bThirty villages (Niakhar area).
Table 3.
Information collected by the Niakhar HDSS
| Level | Date | |
|---|---|---|
| Village Public facilities (GIS) | ||
| Health centres, schools, bore holes, drinking fountains and wells, roads and trails, electricity | 2003 | |
| Household Head Facilities | ||
| Name of household head | Every 4 months | |
| Household domestic and farm properties | 1998 and 2003 | |
| Housing characteristics | ||
| Individual | ||
| Birth | Date of birth, place of birth, name, child characteristics (sex, ethnic group, religion), information on mother and father | Every 4 months |
| Pregnancy | Date of registration, date and place of delivery, pregnancy outcome | Every 4 months |
| Death | Date and cause of death | Every 4 months |
| Out-migration | Date, place, and purpose of out-migration | |
| In-migration | Identifying information (date of birth, sex, identification of mother, identification of father, previous household and village, relationship to the head of household, spousal relationship), date, place and purpose of in-migration, maternal history (women), activity, education, religion, marital status | Every 4 months |
| Immunization | All vaccinations of children under 15 years of age | Every 4 months |
| Measles | All cases of measles in children under 5 years of age | Every 4 months |
| Whooping cough | All cases of pertussis in children under 5 years of age | Every 4 months |
| Weaning | Date of weaning | |
Key findings and publications
During its first period of study, from 1965–1982, the Niakhar HDSS contributed to confirming the efficacy of longitudinal data for providing reliable indicators of demographic characteristics. Pierre Cantrelle’s work showed the atypical age pattern of mortality between the ages of 0 and 5 years, with a high risk of mortality in children 6–36 months old.4 Measles-related mortality was also measured, and the efficacy of the measles vaccine was demonstrated.5 Cantrelle documented the popular knowledge about measles in Africa and explored the relationships between mortality and fertility and the effect of nutritional status on mortality.6
Nutrition
A study conducted in 1983 and 1984 of the nutritional status and mortality of 5000 children aged 6–59 months concluded that treating severe malnutrition is apparently as important for reducing mortality as is preventing mild to moderate malnutrition.3,7
The results of a follow-up study of feeding practices and anthropometric measurements of children found no evidence for recommending the introduction of complementary foods at 4–5 months of age rather than at 6 months in the poor rural setting covered by the HDSS.8,9
Measles and pertussis vaccine trials
The clinical efficacy of measles vaccines was investigated in the Niakhar HDSS from 1987–1990. Three measles vaccines were tested: a standard Schwarz vaccine, a high-titer Edmonston–Zagreb vaccine, and a high-titer Schwarz vaccine. The two high-titer vaccines were given to children at 5 months of age, and the standard Schwarz vaccine at 10 months of age. In the randomized trial of the vaccines, the efficacy of the high-titer vaccines was lower than that of the standard vaccine.10,11 The epidemiology of measles was investigated in the Niakhar HDSS from 1983–1990. Studies showed that immunization against measles may directly help to reduce mortality by reducing the incidence of measles and indirectly help to reduce mortality through increases in the age at which infection occurs, by reducing the severity of infection for immunized children, and by changing transmission patterns in a way that reduces the severity of measles.12 Other findings were that as coverage with measles vaccination increases, the circulation of wild measles will decrease, and that the titer of vaccine-induced antibody to measles is less likely to be increased. Consequently, new epidemics of measles, albeit of milder form, may occur in areas of vaccination and that this should be recognized in campaigns to eradicate measles.13 An increased ratio of female-to-male mortality after the administration of high-titre measles vaccine appears to be due to a change in vaccination sequence rather than to the high-titre vaccine itself.14
Another randomized double-blind trial, comparing a diphtheria–tetanus–acellular pertussis vaccine (DTaP) with a whole-cell vaccine (DTwP), was conducted from 1987–1997.15,16 The results of this study showed that the safer DTaP vaccine may prove a valuable substitute for whole-cell vaccines when used in a schedule that includes a booster dose,17 and that pertussis vaccination is effective in reducing the severity of that disease.18
Malaria
Epidemiological studies of malaria began in 1988 when the spread of chloroquine resistance was first documented in Dakar and monitored in Niakhar and other areas of Senegal.19 The emergence of resistance to choloroquine in Niakhar in 1992 was followed by a rapid increase in the proportion of chloroquine-resistant malaria infections, from 10% in 1993 to 44% in 1996.19,20 Malaria-related mortality among children increased by a factor of 2.5 from 1992–1995 and 1988–1991,21 and then continued to increase until 2000 before declining dramatically between 2001 and 2012 in relation to changes in malaria treatment policies and the deployment in 2008 of insecticide-treated nets.22 Other studies investigated trends in consultations for episodes of malarial fever between 1992 and 2004 in three health-care facilities of the Niakhar area,23,24 and relationships between rainfall and trends in malaria-related mortality.20 Patterns of transmission of malaria in three different sites in the Niakhar area were also investigated.21
A randomized, placebo-controlled, double-blind trial of the effect of intermittent preventive treatment on morbidity from malaria, conducted in 2002–2003, showed that such treatment could be highly effective in preventing malaria among children under 5 years of age living in areas of seasonal malaria infection.22 The study demonstrated that monthly administration of one dose of sulfadoxine–pyrimethamine plus three doses of amodiaquine (SP+3AQ) is a highly effective regimen for seasonal intermittent preventive treatment (IPT) for malaria. The use of this regimen would minimize the spread of drug resistance and allow artemisinin to be reserved for the treatment of acute clinical malaria.23 These findings were followed in 2011 by a WHO international guideline introducing this new treatment for use in national policies, and it continues to be included in the National Malaria Control Program of Senegal.
Field research in malaria-related health-care behaviour has been conducted in the social sciences. A survey conducted in 2001 showed that the care of children with malaria is fundamentally a collective process that favours home-based care, hinders good compliance with treatments, and increases delays to presentation to a health-care facility.24 Several studies25,26 have highlighted the role of biomedical centres and sensitisation campaigns in promoting positive changes in malaria-related behaviour. A survey conducted in 2004 emphasized the importance of information and communication between care-givers and health-centre staff members at the time of the consultation and medicinal treatment for malaria in improving the use of drugs for treating the disease and thus preventing the emergence of rapid drug resistance to it.27
Meningitis
A clinical trial designed to evaluate a new conjugate vaccine (PsA-TT) for preventing infection by Neisseria meningitidis of serogroup A (MenA) was conducted in the Niakhar HDSS in 2007. It showed that the meningococcal A conjugate (PsA-TT) vaccine elicited a stronger antibody response to the group A antigen than did the quadrivalent polysaccharide reference vaccine (PsACWY).28 These results contributed to an international recommendation for the use of this vaccine and its introduction in December 2010 in all 25 countries of the ‘meningitis belt’.
Human immunodeficiency virus and sexually transmitted diseases
The epidemiology of infection with human immunodeficiency virus (HIV) was investigated by the HDSS in 1991 by monitoring pregnant women, patients with a persistent cough, and patients at health centres who had sexually transmitted diseases (STDs). The seroprevalence rate of HIV was 0.2% among women and 1.3% among men.29 Another study, conducted in 1996, concluded that mobility appears to be a key factor for the spread of HIV because population movement facilitates dissemination of the virus and also because mobile persons have high-risk behaviours in relation to its transmission.30
Emerging diseases
As malaria recedes, more cases of fever remain unexplained, justifying the development of programs to detect other infectious diseases. Every year, more than 11 million people in sub-Saharan Africa die (UNICEF. Monitoring and statistics. Available at: http://www.unicef.org/statistics. Accessed 14 October 2012) with the causes for the majority of deaths largely unknown. These uninvestigated deaths are generally attributed to infectious diseases.
A project to investigate the aetiology of ambulatory non-malarial infections in Senegal was initiated in 2010. Blood samples were collected from febrile patients seen in rural health centres in the Niakhar study area and were analysed in the laboratory with the polymerase chain reaction (PCR) assay and other molecular methods. Overall, the spectrum of bacterial pathogens causing fevers in Niakhar did not differ from that in other areas of Senegal. Bacterial deoxyribonucleic acid (DNA) was found in blood samples in about 25% of cases of acute unexplained fevers. The overall incidences of tick-borne relapsing fever caused by Borrelia crocidurae and of fever caused by Rickettsia felis were even higher than the incidence of infection with malaria parasites in the studied group. Among 321 blood samples, the DNA of R. felis was found in as many as 17.8% (unpublished data), and the index case, with an unusual clinical picture, was reported from Niakhar.31 A high incidence of Borrelia-induced relapsing fever (15.6%, 50/321) was observed mainly during the dry season. The overall incidence of Tropheryma whipplei was 1.9% (6/321). Several cases of bartonellosis (including trench fever) and Q fever were also diagnosed.
The study in which these findings were made identified hyperendemic diseases caused by R. felis and B. crocidurae, and endemic diseases caused by T. whipplei, Bartonella spp. and Coxiella burnetii (Q fever) in Niakhar.
Social and cultural aspects
A number of multidisciplinary studies in the social sciences, conducted between 1965 and 1985, have provided a full description of the Sereer agricultural system and warned of growing land pressure and environmental risks in the HDSS area.32 These studies have also uncovered the social and economic changes resulting from family adaptation to and resilience in the face of these factors.33–41
Sexuality, fertility and contraception
The fertility level in the Niakhar study area remains very high, at 6.4 births per woman in 2009–2011.42 This high fertility level can be explained mainly by the family and agricultural organisation in the area. However, changes in the environment, demographic pressure, and migrations also have direct and indirect effects on fertility.43
Findings in studies done in the HDSS area in the 1990s indicated that among newer generations, males tend to have sexual relationships earlier than they formerly did.44 Changes in couple formation and increases in premarital births have been documented.45–47 The consequences of premarital births for mothers48 and for children have been discussed.49 The prevalence of contraceptive measures in 1998 was very low, with just 1.5% of women using modern methods.50
Mortality and causes of death
Demographic surveillance has shown a long-term-decline in childhood mortality in the HDSS study area. Large-scale immunizations have largely contributed to the decrease and change in the age-related mortality pattern.51 Inadequate treatment for chloroquine-resistant malaria and a meningitis outbreak during the 1990s have interrupted the continuous decline in child mortality. The direct and indirect effects of new malaria-control policies, introduced in 2003 and completed in 2006–2008, are possible contributors to the recent dramatic decrease in child mortality.52
Verbal autopsy (VA) has provided useful information about the structure of the causes of mortality. Analyses of VA data have shown that apart from disease outbreaks, malaria was a leading cause of death for 1- to 9-year–old children, and that diarrhoea, acute respiratory infections, or fever of unknown origin was responsible for as many as 50% of deaths among children under 5 years of age.53
Demographic indicators
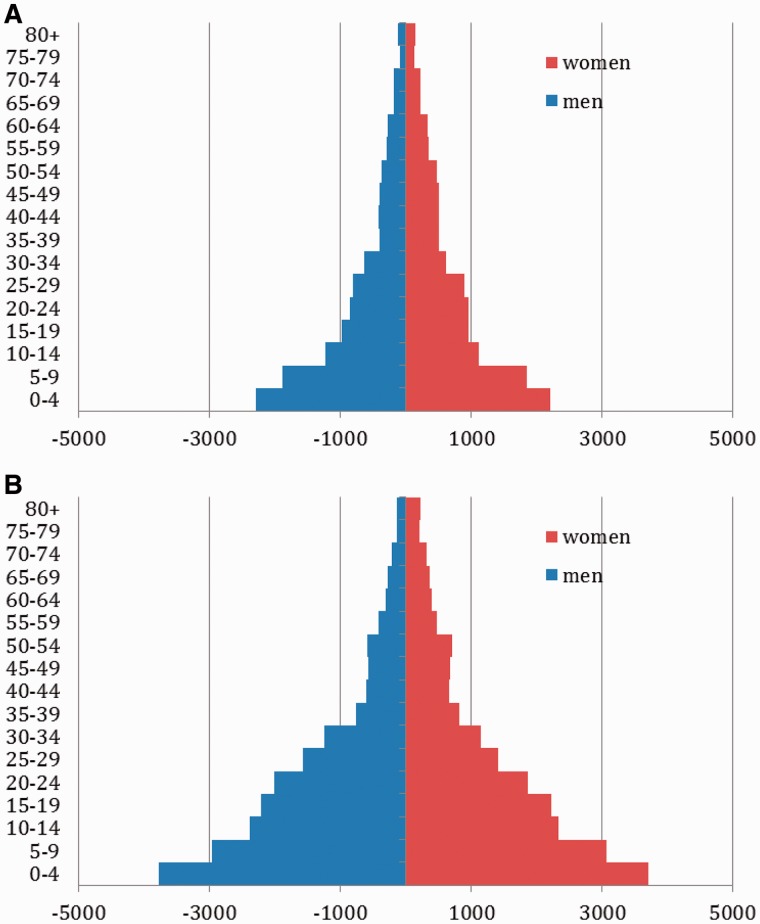
For the overall period in which the HDSS has conducted studies, demographic analyses show a population halfway through the demographic transition: mortality has decreased dramatically and fertility has remained very high, leading to an increase in population growth rates.
The structure of the population pyramid in the Niakhar HDSS area indicates a traditional demographic regime with a wide base indicating a high birth rate (Figure 2).
Figure 1.
Location of the Niakhar HDSS area
Figure 2.
Population pyramid of Niakhar HDSS (A) in 1985 and (B) in 2010 (resident on January 1 of the year)
Future analysis plans
The Niakhar HDSS plans to keep on providing data and long-term indicators of demographic trends in the Niakhar area in mortality (child, adult, and maternal); fertility (intensity, pace, non-marital, fostered children); migration (circular, temporary, out and in-migration); and marriage (marital patterns, divorce, and polygyny). It will also continue to follow up on malaria-, meningitis-, and influenza-related morbidity. The retrospective analysis of emerging pathogens (registered cases of rickettsiosis, relapsing fevers, bartonelloses, Q fever, and T. whipplei infection) may reveal important issues in the epidemiology of these diseases. The HDSS is also further exploring the economic and agricultural dynamics and family adaptations in relation to environment and climate change in the Niakhar area. A new research project will investigate the social network in the area and how it affects health-related behaviours from 2012–2015,54,55 and another project will seek to measure adult mortality. We also plan to further explore ethical issues.56–58
Strengths and weaknesses
A major scientific strength of the Niakhar HDSS is its long-term follow-up of findings, which provides a historical perspective on demographic and economic changes in the Niakhar area. The accumulation of research results during the period since its inception has provided a valuable source information for a multidisciplinary approach to issues in individual, social, and cultural development. The system’s long-term follow-up permits longitudinal analysis and causal interpretations.
The main weakness of the Niakhar HDSS is its overall cost. It is difficult to secure autonomous funding for the routine data collection done by the system. Research projects and particularly clinical trials therefore contribute importantly to this funding.
Data sharing and collaboration
The data collected by the Niakhar HDSS are not open to access, but can be fairly shared under conditions of collaboration and endowment. Collaborative research projects are encouraged. Enquiries and queries can be submitted to the first author at Valerie.Delaunay@ird.fr.
Funding
The work is currently supported primarily by Institut de Recherche pour le Développement. Current projects are supported by Gates Foundation, Global Fund, PATH, Wellcome Trust, National Institute for Health (1R03HD071117-01 and R01GM096999) and Agence Nationale de la Recherche (ANR-GUI-AAP-004).
Acknowledgements
We greatly thank people of Niakhar study area villages for their kindness and patience with all fieldworkers and research staff they are used to welcome. We acknowledge the great work of the numerous field, engineer and research staff that have followed during this five decades and have all contributed to the current Niakhar Health and Demographic Surveillance System.
Conflict of interest: None declared.
KEY MESSAGES.
The Niakhar HDSS is among the world’s oldest demographic surveillance systems.
Research results from the Niakhar HDSS have contributed to the development of relevant policies for measles, pertussis, and meningitis or to vaccine strategies for these diseases or both.
Recent clinical trials in the Niakhar HDSS have influenced the WHO international guidelines for introducing a new treatment for malaria into national policies.
References
- 1.Nadot R. Etat de la recherche démographique an Afrique Noire francophone et à Madagascar. Population. 1968;23:547–50. [Google Scholar]
- 2.Garenne M, Cantrelle P. Three decades of research on population and health: the ORSTOM experience in rural Senegal, 1962–1991. In: Das Goupta M, Aaby P, Garenne P, Pison G, editors. Prospective Community Studies in Developing Countries. Oxford: Clarendon Press; 1997. [Google Scholar]
- 3.Garenne M, Maire B, Fontaine O, Dieng K, Briend A. Risques de décès associés à différents états nutritionnels chez l'enfant d'âge préscolaire. CEPED. 2000:246. [Google Scholar]
- 4.Cantrelle P. International Population Conference. Accra, Ghana: IUSSP; 1974. Is there a standard pattern of African mortality? [Google Scholar]
- 5.Rey M, Baylet R, Mar ID, Cantrelle P. Vaccination contre la rougeole en milieu coutumier sénégalais par le vaccin vivant atténué. In: Edmonston B, editor. Archives of Virology. Vol. 16. 1965. pp. 260–67. [PubMed] [Google Scholar]
- 6.Cantrelle P. Fécondité, allaitement et mortalité infantile: différences inter-ethniques dans une même région: Saloum (Sénégal) Population. 1980;3:623–8. [Google Scholar]
- 7.Garenne M, Maire B, Fontaine O, Briend A. Distributions of mortality risk attributable to low nutritional status in Niakhar, Senegal. J Nutr. 2006;136:2893–900. doi: 10.1093/jn/136.11.2893. [DOI] [PubMed] [Google Scholar]
- 8.Simondon K, Simondon F. Infant feeding and nutritional status: the dilemma of mothers in rural Senegal. Eur J Clin Nutr. 1995;49:179–88. [PubMed] [Google Scholar]
- 9.Simondon K, Simondon F. Age at introduction of complementary food and physical growth from 2 to 9 months in rural Senegal. Eur J Clin Nutr. 1997;51:703–7. doi: 10.1038/sj.ejcn.1600470. [DOI] [PubMed] [Google Scholar]
- 10.Garenne M, Leroy O, Beau JP, Sene I. Efficacy of measles vaccines after controlling for exposure. Am J Epidemiol. 1993;138:182–95. doi: 10.1093/oxfordjournals.aje.a116844. [DOI] [PubMed] [Google Scholar]
- 11.Samb B, Aaby P, Whittle H, Seck A, Simondon F. Protective efficacy of high-titre measles vaccines administered from the age of five months: a community study in rural Senegal. Trans R Soc Tropic Med Hyg. 1993;87:697–701. doi: 10.1016/0035-9203(93)90301-6. [DOI] [PubMed] [Google Scholar]
- 12.Samb B, Aaby P, Whittle H, Seck A, Simondon F. Decline in measles case fatality ratio after the introduction of measles immunization in rural Senegal. Am J Epidemiol. 1997;145:51–7. doi: 10.1093/oxfordjournals.aje.a009031. [DOI] [PubMed] [Google Scholar]
- 13.Whittle H, Aaby P, Samb B, Jensen H, Bennett J, Simondon F. Effect of subclinical infection on maintaining immunity against measles in vaccinated children in West Africa. Lancet. 1999;353:98–102. doi: 10.1016/S0140-6736(98)02364-2. [DOI] [PubMed] [Google Scholar]
- 14.Aaby P, Jensen H, Samb B, et al. Differences in female-male mortality after high-titre measles vaccine and association with subsequent vaccination with diphtheria-tetanus-pertussis and inactivated poliovirus: reanalysis of West African studies. Lancet. 2003;361:2183–88. doi: 10.1016/S0140-6736(03)13771-3. [DOI] [PubMed] [Google Scholar]
- 15.Simondon F, Yam A, Gagnepain J, Wassilak S, Danve B, Cadoz M. Comparative safety and immunogenicity of an acellular versus whole-cell pertussis component of diphtheria-tetanus-pertussis vaccines in Senegalese infants. Eur J Clin Microbiol Infect Dis. 1996;15:927–32. doi: 10.1007/BF01690510. [DOI] [PubMed] [Google Scholar]
- 16.Preziosi MP, Ndiaye M, Coll-Seck A, Simondon F. The Senegal pertussis trial: safety and surveillance of adverse reactions. Dev Biol Stand. 1997;89:91–7. [PubMed] [Google Scholar]
- 17.Simondon F, Préziosi M-P, Yam A, et al. A randomized double-blind trial comparing a two-component acellular to a whole-cell pertussis vaccine in Senegal. Vaccine. 1997;15: 1606–12. doi: 10.1016/s0264-410x(97)00100-x. [DOI] [PubMed] [Google Scholar]
- 18.Preziosi MP, Halloran ME. Effects of pertussis vaccination on disease: vaccine efficacy in reducing clinical severity. Clin Infect Dis. 2003;37:772–79. doi: 10.1086/377270. [DOI] [PubMed] [Google Scholar]
- 19.Sokhna C, Molez J, Ndiaye P, Sané B, Trape J. Tests in vivo de chimiosensibilité de plasmodium falciparum à la chloroquine au Sénégal: évolution de la résistance et estimation de l'éfficacité thérapeutique. Bull Soc Pathol Exotique. 1997;90:83–89. [PubMed] [Google Scholar]
- 20.Ndiaye O, Le Hesran J-Y, Etard J-F, et al. Variations climatiques et mortalité attribuée au paludisme dans la zone de Niakhar, Sénégal, de 1984 à 1996. Cahiers Santé. 2001;11:25–33. [PubMed] [Google Scholar]
- 21.Robert V, Dieng H, Lochouarn L, et al. Transmission of malaria around Niakhar, Senegal. Trop Med Int Health. 1998;3:667–77. doi: 10.1046/j.1365-3156.1998.00288.x. [DOI] [PubMed] [Google Scholar]
- 22.Cisse B, Sokhna C, Boulanger D, et al. Seasonal intermittent preventive treatment with artesunate and sulfadoxine-pyrimethamine for prevention of malaria in Senegalese children: a randomised, placebo-controlled, double-blind trial. Lancet. 2006;367:659–67. doi: 10.1016/S0140-6736(06)68264-0. [DOI] [PubMed] [Google Scholar]
- 23.Sokhna C, Cissé B, Ba E, et al. A trial of efficacy, safety and impact on drug resistance of four potential drug regimens for seasonal intermittent preventive treatment for malaria in Senegalese children. PLoS One. 2008;3:e1471. doi: 10.1371/journal.pone.0001471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franckel A, Lalou R. Health-seeking behaviour for childhood malaria: household dynamics in rural Senegal. J Biosoc Sci. 2009;41:1–19. doi: 10.1017/S0021932008002885. [DOI] [PubMed] [Google Scholar]
- 25.Franckel A, Arcens F, Lalou R. Village context and health-seeking behaviour in the Fatick region of Senegal. Population. 2008;63:531–53. [Google Scholar]
- 26.Baxerres C, Le Hesran J-Y. Quelles ressources familiales financent la santé des enfants? Les difficultés du recours aux soins pour traiter le paludisme en milieu rural sénégalais. Tiers Monde. 2010;202:149–65. [Google Scholar]
- 27.Souares A, Lalou R, Sene I, Sow D, Le Hesran J. Factors related to compliance to anti-malarial drug combination: example of amodiaquine/sulphadoxine-pyrimethamine among children in rural Senegal. Malaria J. 2009;8:1–8. doi: 10.1186/1475-2875-8-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sow S, Brown J, Diallo A, et al. Immunogenicity and safety of a meningococcal a conjugate vaccine in Africans. N Engl J Med. 2011;364:2293–304. doi: 10.1056/NEJMoa1003812. [DOI] [PubMed] [Google Scholar]
- 29.Lemardeley P, Diallo A, Guèye-Ndiaye A, Becker C, Mboup S, Rey J-L. Evaluation en 1991 des risques de MST et d'infections par VIH en zone rurale sénégalaise. Cahiers Santé. 1995;5:43–46. [PubMed] [Google Scholar]
- 30.Lagarde E, Schim van der Loeff M, Enel C, et al. Mobility and the spread of human immunodeficiency virus into rural areas of West Africa. Int J Epidemiol. 2003;32:744–52. doi: 10.1093/ije/dyg111. [DOI] [PubMed] [Google Scholar]
- 31.Mediannikov O, Fenollar F, Bassene H, et al. Description of “Yaaf” the vesicular fever caused by acute Rickettsia felis infection in Senegal. J Infect. 2013;66:536–40. doi: 10.1016/j.jinf.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Lericollais A, editor. Paysans Sereer. Dynamiques Agraires et Mobilités au Sénégal. Paris: IRD Editions; 1999. [Google Scholar]
- 33.Fall AS. Une réponse à la crise de l'agriculture. La migration des Sereer du Siin (Sénégal) Sociétés-Espace-Temps. 1991;1:138–49. [Google Scholar]
- 34.Becker C, Mbodj M, Sarr I. La dynamique du peuplement sereer. Les Sereer du Sine. In: Lericollais A, editor. Paysans Sereer Dynamiques Agraires et Mobilités au Sénégal. Paris: IRD Editions; 1999. [Google Scholar]
- 35.Guigou B, Lericollais A. Crise de l'agriculture et marginalisation économique des femmes sereer Siin (Sénégal) Sociétés, Espaces, Temps. 1992;1:45–64. [Google Scholar]
- 36.Lombard J. Les fondements de l'économie locale. Les marchés ruraux du Sine. In: Lericollais A, editor. Paysans Sereer Dynamiques Agraires et Mobilités au Sénégal. Paris: IRD Editions; 1999. [Google Scholar]
- 37.Delpeuch B, Gastellu JM, editors. Maintenance Sociale et Changement Economique au Sénégal. II : Pratique du Travail et Rééquilibres Sociaux en Milieu Serer. Paris: ORSTOM; 1974. [Google Scholar]
- 38.Dupire M, Lericollais A, Delpech B, Gastellu J-M. Résidence, tenure foncière, alliance dans une société bilinéaire (serer du Sine et du Baol, Sénégal) Cahiers d'Etudes Africaines. 1975;55:417–52. [Google Scholar]
- 39.Lombard J. Riz des Villes, Mil des Champs en Pays Serers—Sénégal: Centre d'Etudes de Géographie Tropicale. 1993 [Google Scholar]
- 40.Mondain N, LeGrand T, Delaunay V. L'évolution de la polygamie en milieu rural sénégalais: institution en crise ou en mutation? Cahiers Québécois de Démographie. 2004;33:273–308. [Google Scholar]
- 41.Adjamagbo A, Delaunay V, Lévi P, Ndiaye O. Comment les ménages d'une zone rurale du Sénégal gèrent-ils leurs ressources? Etudes Rurales. 2006;177:71–90. [Google Scholar]
- 42.Biuatti A. Analyse de la Fécondité à Partir des Données du SSD de Niakhar, Sénégal par la Méthode d'Analyse Statistique des Biographies. Marseille: Aix-Marseille Université; 2012. [Google Scholar]
- 43.Delaunay V, Adjamagbo A, Lalou R. Questionner la transition de la fécondité en milieu rural africain : les apports d’une démarche longitudinale et institutionnelle. Cahiers Québécois de Démographie. 2006;35:27–50. [Google Scholar]
- 44.Delaunay V, Enel C, Lagarde E, et al. Sexualité des Adolescents: Tendances Récentes en Milieu Rural Sénégalais. Paris: CEPED; 2001. [Google Scholar]
- 45.Mondain N, Delaunay V. Life before marriage. Changes in couple formation and premarital pregnancies among the sereer sin in Senegal. Working Paper Series of Harvard Center for Population and Development Studies. 2003;13:1–32. [Google Scholar]
- 46.Delaunay V. Sexualité et fécondité des adolescents: évolutions récentes en milieu rural sénégalais. In: Gendreau F, Poupard M, editors. Les Transitions Démographiques des Pays du Sud. Rabat (MA), Paris: Estem; 2001. [Google Scholar]
- 47.Delaunay V. L'entrée en Vie Féconde. Expression Démographique des Mutations Socio-Economiques d'un Milieu Rural Sénégalais. Paris (FR): CEPED; 1994. [Google Scholar]
- 48.Mondain N, Delaunay V, Adjamagbo A. Maternité et mariage en milieu rural sénégalais: quel avenir pour les mères célibataires? In: Gourbin C, editor. Santé de la reproduction au Nord et au Sud De la connaissance à l'action. Louvain-la-Neuve: Presse Universitaire de Louvain; 2009. [Google Scholar]
- 49.Adjamagbo A, Delaunay V, Mondain N. Maternité prénuptiale en milieu rural Sénégalais. Quelles conséquences pour les enfants? In: Marcoux R, Dion J, editors. Mémoires et Démographie: Regards Croisés au Sud et au Nord. Presses de l’Université Laval; 2009. [Google Scholar]
- 50.Ndiaye CAT, Delaunay V, Adjamagbo A. Connaissance et utilisation des méthodes contraceptives en milieu rural Sereer au Sénégal. Santé: Cahiers d'Etudes et de Recherches Francophones (FR) 2003;13:31–7. [PubMed] [Google Scholar]
- 51.Delaunay V, Etard J-F, Préziosi M-P, Marra A, Simondon F. Decline of infant and child mortality rates in rural Senegal over a 37-year period (1963–1999) Int J Epidemiol. 2001;30:1286–93. doi: 10.1093/ije/30.6.1286. [DOI] [PubMed] [Google Scholar]
- 52.Trape JF, Sauvage C, Ndiaye O, et al. New malaria-control policies and child mortality in Senegal: reaching Millennium Development Goal 4. J Infect Dis. 2012;205:672–9. doi: 10.1093/infdis/jir805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Etard J-F, Le Hesran J-Y, Diallo A, Diallo J-P, Ndiaye J-L, Delaunay V. Childhood mortality and probable causes of death using verbal autopsy in Niakhar, Senegal; 1989–2000. Int J Epidemiol. 2004;33:1286–92. doi: 10.1093/ije/dyh259. [DOI] [PubMed] [Google Scholar]
- 54.Sandberg J, Rytina S, Delaunay V, Marra A. Social learning about levels of perinatal and infant mortality in Niakhar, Senegal. Social Networks. 2012;34:264–74. doi: 10.1016/j.socnet.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sandberg J, Delaunay V, Diallo A, Rytina S. Interpersonal Influence on Beliefs and Behaviours Concerning Childbirth Location in Rural Senegal: Evidence From the Niakhar Social Networks Pilot Survey. Los Angeles: Population Association of America; 2012. [Google Scholar]
- 56.Préziosi M-P, Yam A, Wassilak SGF, Simondon F. Individual versus community informed consent. In: session EaRMb (ed). Multilateral Initiative on Malaria, African Malaria Conference, 1999; Durban, South Africa, 1999. [Google Scholar]
- 57.Mondain N, Bologo E. L'intentionnalité du chercheur dans les pratiques de production de connaissances : les enjeux soulevés par la construction des données en démographie et santé en Afrique. Cahiers de Recherche Sociologique. 2009;48:175–203. [Google Scholar]
- 58.Bologo E, Mondain N. Questions éthiques et restitution dans les systèmes de surveillance démographique en Afrique. In: Mondain N, Bologo E, editors. La Recherche en Contexte de Vulnérabilité Engagement du Chercheur et Enjeux Ethiques. Paris: L'Harmattan; 2012. [Google Scholar]