Abstract
Purpose
Commonly used terms such as “supportive care,” “best supportive care,” “palliative care,” and “hospice care” were rarely and inconsistently defined in the palliative oncology literature. We conducted a systematic review of the literature to further identify concepts and definitions for these terms.
Methods
We searched MEDLINE, PsycInfo, EMBASE, and CINAHL for published peer-reviewed articles from 1948 to 2011 that conceptualized, defined, or examined these terms. Two researchers independently reviewed each citation for inclusion and then extracted the concepts/definitions when available. Dictionaries/textbooks were also searched.
Results
Nine of 32 “SC/BSC,” 25 of 182 “PC,” and 12 of 42 “HC” articles focused on providing a conceptual framework/definition. Common concepts for all three terms were symptom control and quality-of-life for patients with life-limiting illness. “SC” focused more on patients on active treatment compared to other categories (9/9 vs. 8/37) and less often involved interdisciplinary care (4/9 vs. 31/37). In contrast, “HC” focused more on volunteers (6/12 vs. 6/34), bereavement care (9/12 vs. 7/34), and community care (9/12 vs. 6/34). Both “PC” and “SC/BSC” were applicable earlier in the disease trajectory (16/34 vs. 0/9). We found 13, 24, and 17 different definitions for “SC/BSC,” “PC,” and “HC,” respectively. “SC/BSC” was the most variably defined, ranging from symptom management during cancer therapy to survivorship care. Dictionaries/textbooks showed similar findings.
Conclusion
We identified defining concepts for “SC/BSC,” “PC,” and “HC” and developed a preliminary conceptual framework unifying these terms along the continuum of care to help build consensus toward standardized definitions.
Keywords: Supportive care, Best supportive care, Palliative care, Hospice care, Definitions, Concepts, Terminology
Introduction
The modern hospice movement has its origins in the work of Dr. Cicely Sanders in the 1960s and has since evolved from a philosophy of care to a professional discipline with expertise in symptom management, psychosocial and spiritual care, communication, decision making, caregiver support, and end-of-life care [10, 25, 26]. Dr. Baulfor Mount coined the term “palliative care” around 1975 to describe his hospice program in Canada, and it has since gained acceptance worldwide [33]. Over the past few decades, numerous other terms have been used to describe this ever evolving entity, including “care of the dying,” “terminal care,” “end-of-life care,” “continuing care,” “total care,” “holistic care,” “comprehensive care,” “comfort care,” “pain and symptom management,” and “quality-of-life care” [9, 17, 22, 33]. More recently “supportive care” and “best supportive care” have gained popularity [15, 21, 24]. Some opinion leaders have called these terms euphemisms [9, 14, 17], and others have argued for the need for standardized definitions [35, 42, 61].
Previous studies have shown that “palliative care” is confusing to clinicians and patients alike [8, 34, 50]. The National Institute of Health State of Science Conference Statement on Improving End-of-Life Care stated that “there has been a lack of definitional clarify related to several concepts and terms” [4]. The lack of definitions for key terms represents a barrier to clinical communication and research. To learn more about the state of definition, we recently sampled journal articles in 2004 and 2009 and determined the frequency of commonly used terms in the palliative oncology literature, the proportion of articles that provided definitions for each term, and how each term was defined [35]. We found that “palliative care” and “hospice care” were commonly used in the published palliative oncology literature and were variably defined with multiple definitions [35]. In contrast, “supportive care” and “best supportive care” were less frequently used, and no clear definitions were found for these terms. However, that study was limited only to articles published in two different 6-month periods, and thus did not provide a full picture of the definitions and concepts available.
A better understanding of the key concepts and defining features for “supportive care,” “best supportive care,” “palliative care,” and “hospice care” could provide a common ground for clinical and research communication and pave the way for standardization. The objective of this study is to examine the published literature, medical dictionaries, and textbooks for concepts and definitions for “supportive care,” “best supportive care,” “palliative care,” and “hospice care.”
Methods
Literature search
The Institutional Review Board at MD Anderson Cancer Center provided approval to proceed without the need for full committee review. Between February 21, 2011 and April 18, 2011, our clinical librarian searched all the citations on Ovid MEDLINE PubMed, Ovid PsycInfo, Ovid EMBASE, and EBSCO CINAHL from 1948 to 2011. Our search strategy consisted of Medical Subject Headings (MESH) and text word or text phrase for “palliative care/medicine,” “supportive care,” “best supportive care,” and “hospice care,” plus one of the following terms including “defin$,” “understanding,” “conceptualization,” “terminology,” and “nomenclature,” Original studies, reviews, systematic reviews, guidelines, editorials, commentaries, and letters were included. Non-English articles, dissertations, and conference abstracts were excluded. Duplicates were removed. We did not include definitions from the internet and/or various organizations because a vast majority of these were already included in the peer-reviewed manuscripts above, and we have recently reported these definitions in a related study [35]. Articles on palliative/supportive/hospice care that did not specifically define or conceptualize the terms were excluded from this analysis (e.g., articles on specialized palliative care interventions).
After the initial librarian search, two palliative care specialists independently reviewed the title and abstract of each citation for inclusion. Publications were included if one of their objectives was to provide a definition or conceptualization for the term of interest. Any disagreements were discussed and a consensus reached.
The search for articles examining one term often uncovered papers that discussed the concepts for multiple terms. For instance, “palliative care” and “hospice care” were often discussed together. For this reason, articles that were not identified in the initial search but found to be highly relevant were also included as additional articles of interest. For completeness, we also included an article on “best supportive care” that was recently published outside of the date range specified in our search strategy [15].
Upon identification of relevant articles, we retrieved the full manuscript, examined each study in detail and captured the key concepts involved. We elected to extract defining concepts using the entire manuscript as a unit instead of individual definitions to allow us to obtain a more complete perspective. This process was undertaken independently by two investigators, both with training in palliative care research (D.H. and M.D.). The inter-rater agreement for all variables was high (kappa00.82–1.0). We also extracted any definitions cited and/or provided by the authors. We combined the reporting for “supportive care” and “best supportive care” because three of nine articles defining these two terms used them interchangeably [15, 17, 18].
Dictionary and textbook search
We also searched for definitions related to “palliative care/medicine,” “supportive care,” “best supportive care,” and “hospice care” in six print dictionaries and four online medical dictionaries. The print dictionaries were selected from a list of 26 based on their year of publication and authoritative publishers, and included McGraw-Hill Allied Medical Dictionary (2008), Dorland's Illustrated Medical Dictionary (2007), Black's Medical Dictionary (2010), Mosby's Medical Dictionary (2009), Stedman's Medical Dictionary (2006), and Taber's Cyclopedic Medical Dictionary (2009).
The Google search engine was used to identify four online medical dictionaries based on criteria outlined by A Guide for Evaluating Health Web Sites provided by the National Network of Libraries of Medicine (http://nnlm.gov/outreac/consumer/evalsite.html). These included MediLexicon (2011), Medical Dictionary (WebMD, 2011), MedlinePlus Medical Dictionary (2011), and The Free Dictionary: Medical Dictionary (2011).
We identified five commonly used palliative medicine textbooks (Oxford Textbook of Palliative Medicine, 4th edition, Textbook of Palliative Medicine, 1st edition, Principles and Practice of Palliative Care and Supportive Oncology, 3rd edition, Palliative Medicine, 1st edition, and Principles and Practice of Supportive Oncology 1st edition), and searched for definitions for the terms of interest.
Statistical analysis
We summarized the concepts and definitions using frequencies and percentages.
Results
Literature search
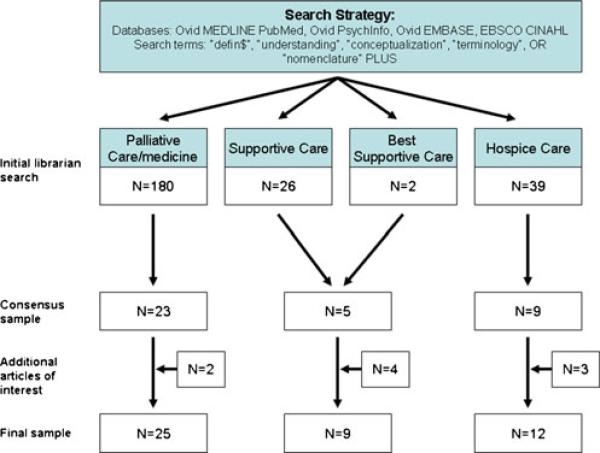
The literature search flowchart is shown in Fig. 1.
Fig. 1.
Search strategy for articles that defined “palliative care,” “supportive care,” “best supportive care,” and “hospice care”
Concepts and definitions for “supportive care” and “best supportive care”
Nine articles focused on the concepts of “supportive care” and “best supportive care,” including one systematic review, three editorials, three review articles, and two letters to the editor (Table 1). A majority of articles (N=7/9) acknowledged confusion in how these terms were used in the literature.
Table 1.
Conceptual elements for “best/supportive care,” “palliative care,” and “hospice care”
| Articles on “supportive care” and “best supportive care” |
Study type | Country | Discipline | Symptom control and quality of life |
Interprofessional care |
Volunteer involvement |
Caregiver care |
Bereavement | Patients on active treatment or trials |
Patients with advanced, noncurable disease |
Patients with curable disease |
Community- based program |
Inpatient program |
Term described as confusing |
Term describe as euphemistic |
Term associated with fear |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Page. Can Oncol Nurs J 1994 [47] | Editorial | Canada | Nursing | x | x | x | x | x | x | x | ||||||
| MacDonald N. Cancer Prev Control 1998 [39] | Letter to editor | Canada | Medicine | x | x | x | x | x | ||||||||
| O'Neill. J Pediatr Oncol Nurs 2000 [46] | Editorial | US | Nursing | x | x | x | x | |||||||||
| Cullen M. Lancet Oncol 2001 [20] | Review | UK | Medicine | x | x | x | x | |||||||||
| Zafar et al. J Clin Oncol 2008 [61] | Letter to editor | US | Medicine | x | x | x | x | |||||||||
| Cherny et al. Cancer 2009 [17] | Editorial | Israel | Medicine | x | x | x | x | x | x | x | x | |||||
| Cherny et al. J Clin Oncol 2009 27:32 [18] | Systematic review | Israel | Medicine | x | x | x | x | x | x | |||||||
| Ritchie et al. Curr Hematol Malig Rep 2010 [52] | Review | US | Medicine | x | x | x | x | x | ||||||||
| Cherny. Semin Oncol 2011 [15] | Review | Israel | Medicine | x | x | x | x | x | x | x | x | |||||
| Articles on “Palliative Care/Medicine” | ||||||||||||||||
| Doyle. Palliat Med 1993 [22] | Editorial | UK | Medicine | x | x | x | x | x | ||||||||
| Sutherland et al. Health Trends 1993 [56] | Review | UK | Health administrator | x | x | x | x | x | ||||||||
| Allen et al. The Pharmaceutical Journal 1995 [5] | Review | UK | Pharmacy | x | x | x | x | x | x | x | ||||||
| Finlay et al. BMJ 1995 [27] | Letter to editor | UK | Medicine | x | x | x | x | x | ||||||||
| Post et al. Bioethics Forum 1997 [51] | Review | US | Nursing, Law | x | x | x | x | x | ||||||||
| Goodlin. Hospital Practice 1997 [32] | Editorial | US | Medicine | x | x | x | x | x | ||||||||
| Billings. J Palliat Med 1998 [9] | Review | US | Medicine | x | x | x | x | x | x | x | ||||||
| Browde. South Afr Med J 2001 [13] | Review | South Africa | Medicine | x | x | x | x | x | ||||||||
| J Pharmacol Care Pain Symp Control 2001 [1] | Review | US | Organization | x | x | x | x | x | ||||||||
| Lipman. J Pharmacol Care Pain Symp Control 2001 [38] | Editorial | US | Pharmacy | x | x | x | ||||||||||
| Lamers. J Pain Palliat Care Pharm 2002 [37] | Review | US | Medicine | x | x | x | x | |||||||||
| J Hosp Palliat Nurs 2003 [3] | Review | US | Organization | x | x | x | x | |||||||||
| Doyle. Palliat Med 2003 [23] | Editorial | UK | Medicine | x | x | x | x | |||||||||
| Van Kleffens et al. Eur J Cancer Care 2004 [58] | Qualitative study | Netherlands | Philosophy | x | x | x | x | x | x | |||||||
| Meghani et al. J Adv Nurs 2004 [43] | Concept analysis | US | Nursing | x | x | x | x | x | x | x | x | x | ||||
| O'Connor. Int J Palliat Nurs 2005 [45] | Discourse analysis | Australia | Nursing | x | x | x | x | x | x | x | ||||||
| Mularski. Crit Care Med 2006 [44] | Review | US | Medicine | x | x | x | x | x | x | x | x | x | x | |||
| Martin. The Consultant Pharmacist 2006 [41] | Review | US | Pharmacy | x | x | x | x | x | x | x | x | |||||
| Ventafaridda. Palliat Med 2006 [59] | Editorial | Italy | Medicine | x | x | x | x | x | ||||||||
| Hanks. Palliat Med 2008 [33] | Editorial | UK | Medicine | x | x | x | x | x | x | x | x | x | x | |||
| Bekelman et al. Int J Cardiol 2008 [7] | Review | US | Medicine | x | x | x | x | x | x | x | ||||||
| Pastrana et al. Palliat Med 2008 [48] | Discourse analysis | Germany | Medicine | x | x | x | x | x | x | x | x | x | x | x | x | |
| Cherny et al. Cancer 2009 [17] | Editorial | Israel | Medicine | x | x | x | x | x | x | x | x | x | ||||
| Batchelor. Rehab Nurs 2010 [6] | Review | US | Nursing | x | x | x | x | x | x | x | x | x | ||||
| Pautex et al. JAGS 2010 [49] | Letter to editor | Switzerland | Medicine | x | x | x | x | x | x | |||||||
| Articles on “Hospice Care” | ||||||||||||||||
| Tehan. Hosp Forum 1980 [57] | Review | US | Medicine | x | x | x | x | x | x | x | x | |||||
| Sutherland et al. Health Trends 1993 [56] | Review | UK | Health administrator | x | x | x | x | x | x | x | ||||||
| McCann. J Palliat Care 1988 [42] | Review | US | Health administrator | x | x | x | x | x | x | x | x | x | ||||
| Mann et al. Am J Hosp Palliat Care 1997 [40] | Editorial | US | Nursing | x | x | x | x | |||||||||
| Billings. J Palliat Med 1998 [9] | Review | US | Medicine | x | x | x | x | x | x | x | x | x | ||||
| Chamberlain. Am J Hosp Palliat Care 2001 [14] | Editorial | US | Medicine | x | x | x | x | x | x | x | ||||||
| Lipman. J Pharmacol Care Pain Symp Control 2001 [38] | Editorial | US | Pharmacy | x | x | x | x | x | x | |||||||
| Jennings et al. Hastings Center Report 2003 [36] | Review | US | Political science | x | x | x | x | x | x | x | x | x | ||||
| Lamers. J Pain Palliat Care Pharm 2002 [37] | Review | US | Medicine | x | x | x | x | x | x | x | x | |||||
| Gazelle. NEJM 2007 [31] | Editorial | US | Medicine | x | x | x | x | x | x | x | ||||||
| Batchelor. Rehab Nurs 2010 [6] | Review | US | Nursing | x | x | x | x | x | x | x | ||||||
| Bosma et al. Pall Med 2010 [12] | Systematic review | Canada | Social work | x | x | x | x | x | x | x |
Among the three of nine articles focusing on “supportive care,” two described it as an all encompassing service providing care from diagnosis to bereavement and another defined it as symptom management during antineoplastic therapies. Six of the nine articles examined the term “best supportive care.” This term was discussed in the context of randomized controlled trials in five of six articles, of which four suggested that the descriptive word “best” requires justification and standardization, and four considered it to be equivalent to “palliative care.” The remaining “best supportive care” article defined it as “treatment with antibiotics, transfusions of blood and blood products, hydroxyurea, and hematopoietic growth factors” for patients with acute leukemia.
All nine articles discussed the role of “supportive care” and “best supportive care” for controlling symptoms and improving quality of life. The target population ranged from patients on cancer treatment (N=9/9) to cancer survivors (N=3/9). Volunteers (N=0/9) and bereavement services (N=1/9) were not usually discussed. Compared to “hospice care” and “palliative care,” “supportive care” focused more on patients receiving treatment and interdisciplinary care was less often described (Table 2).
Table 2.
A comparison of the conceptual elements among “best/supportive care,” “palliative care,” and “hospice care”
| Concepts | Best/supportive care,aN=9 (%) | Palliative care, N=25 (%) | Hospice care, N=12 (%) |
|---|---|---|---|
| Symptom control and quality of life | 9 (100) | 24 (96) | 12 (100) |
| Interprofessional care | 4 (44) | 20 (80) | 11 (92) |
| Volunteer involvement | 0 (0) | 6 (24) | 6 (50) |
| Caregiver care | 5 (56) | 22 (88) | 11 (92) |
| Bereavement care | 1 (11) | 6 (24) | 9 (75) |
| Patients on treatment/trials | 9 (100) | 8 (32) | 0 (0) |
| Patients with advanced, noncurable disease | 9 (100) | 25 (100) | 12 (100) |
| Patients with curable disease | 4 (44) | 12 (48) | 0 (0) |
| Community-based program | 0 (0) | 6 (24) | 9 (75) |
| Inpatient program | 0 (0) | 10 (40) | 6 (50) |
| Term described as confusing | 7 (78) | 11 (44) | 5 (42) |
| Term described as euphemistic | 2 (22) | 8 (32) | 2 (17) |
| Term associated with fear | 1 (11) | 4 (16) | 5 (42) |
Articles for “supportive care” and “best supportive care” were analyzed together
From the bibliographic databases, we identified 13 unique definitions for “supportive care” and “best supportive care” (Table 3). We found one entry for “supportive care” in our dictionary search and another in our textbook search (Table 4). No definitions were available for “best supportive care” in medical dictionaries and textbooks (Table 5).
Table 3.
Definitions for “best/supportive care,“ “palliative care,” and “hospice care”
| Articles on “supportive care” and “best supportive care” | Study type | Definition(s) proposed or information discussed | Citation source |
|---|---|---|---|
| Page. What is supportive care? Can Oncol Nurs J 1994 [47] | Editorial | Definition of supportive care “the provision of the necessary services for those living with or affected by cancer to meet their informational, emotional, spiritual, social or physical need during their diagnostic treatment or follow-up phases encompassing issues of health promotion and prevention, survivorship, palliation and bereavement....In other words, supportive care is anything one does for the patient that is not aimed directly at curing his disease but rather is focused at helping the patient and family get through the illness in the best possible condition. Clearly this type of help would need to be broad in scope and as varied as the individuals requiring it” | Toronto-Bayview Regional Cancer Centre, 1992 |
| MacDonald N. Best supportive care. Cancer Prev Control 1998 [39] | Letter to editor | Definition of Best Supportive Care “this group of patients would be managed by committed family physicians, well supported by the consultative services of a palliative care group and regional oncology program. Symptoms would be assessed in a comprehensive and systematic fashion; supportive care would be recognized as an exercise in prevention, with early application of symptom control measures, and the patients would be assured a high degree of follow-up and attention to detail” | Not available |
| O'Neill. What is Supportive Care and why is it important? J Pediatr Oncol Nurs 2000 [46] | Editorial | Definition of supportive care “a term that describes the side effects that are caused by chemotherapy and radiation. These side effects may be both physical and psychological in nature. Supportive care includes, but is not limited to, the treatment of emesis, nausea, depression, alopecia, oral complications, fatigue, and myelosuppression. These side effects adversely affect the patient's quality of life and may interfere with ultimate treatment success if the symptoms require significant chemotherapy dose reduction” | Not available |
| Cullen M. Best supportive care has had its day. Lancet Oncol 2001 [20] | Review | Definition of best supportive care “palliative radiotherapy as required for SVCO, hemoptysis, painful osseous metastases, brain metastases, or bronchial obstruction. Antibiotics were used to control infections. Corticosteroids were used to treat hypercalcaemia or increased intracranial pressure” | Rapp et al. JCO 1988 |
| Definition of best supportive care “as any palliative treatment excluding chemotherapy” | Anderson et al. Br J Cancer 2000 | ||
| Definition of Best Supportive Care “the standard management and treatment for breathlessness available to patients within each centre” | Bredin et al. BMJ 1999 | ||
| Zafar et al. Defining Best Supportive Care. J Clin Oncol 2008 [61] | Letter to editor | Definition of best supportive care “The best palliative care per investigator excluding antineoplastic agents” | Van Cutsem et al. J Clin Oncol 2007 |
| Definition of best supportive care “Treatment administered with the intent to maximize quality of life without a specific antineoplastic regimen,” which included “antibiotics, analgesics, antiemetics, thoracentesis, pleurodesis, blood transfusions, nutritional support, and focal external-beam radiation for control of pain, cough, dyspnea, or hemoptysis” | Jassem et al. J Clin Oncol 2008 | ||
| Definition of best supportive care “analgesics, antibiotics, blood transfusions, corticosteroids, antiemetics, antidiarrheals, or vitamins” | Rao et al. J Clin Oncol 2004 | ||
| Cherny et al. Stigma associated with “Palliative Care” Cancer 2009 [17] | Editorial | Definition of supportive care “A treatment approach to reduce side effects from chemotherapy and other primary treatments in cancer” to an all encompassing purview that incorporates all aspects of toxicity minimization, palliative care, and survivorship” | Not available |
| Cherny et al. Improving the methodologic and ethical validity of best supportive care studies in oncology: lessons from a systematic review. J Clin Oncol 2009 [18] | Systematic review | Definition of supportive care “supportive care, which included palliative radiation, psychosocial support, analgesics, and nutritional support” | Ganz et al. Cancer 1988 |
| Definition of best supportive care “The best palliative care per investigator excluding antineoplastic agents” | Van Cutsem et al. J Clin Oncol 2007 | ||
| Definition of palliative care “Palliative care, including RT (radiotherapy), antibiotics, cough suppressants, analgesics, and so on, was given to all patients without restriction according to the standard practice of the collaborating centers” | Cullen et al. J Clin Oncol 1999 | ||
| Ritchie et al. Levels of care: defining best supportive care in elderly patients with acute myeloid leukemia. Curr Hematol Malig Rep 2010 [52] | Review | Definition of best supportive care “Treatment with antibiotics, transfusions of blood and blood products, hydroxyurea, and hematopoietic growth factors. It is assumed that all patients with AML receive BSC in conjunction with their leukemia treatment...” | Not available |
| Cherny. Best supportive care: a euphemism for no care or a standard of good care? Semin Oncol 2011 [15] | Review | Standards for best supportive care “1. Adequate staff training for primary level providers of supportive and palliative care including oncologist and oncology nurses to ensure appropriate knowledge skills and attitudes in supportive and palliative care | World Health Organization 1990 |
| 2. Interdisciplinary care with a minimum team of physician, nurse, and social worker | |||
| 3.Care coordinated to minimize the burden on patient, their caregiver(s), and family | |||
| 4. Routine patient evaluation using validated tools to evaluate the prevalence and severity of physical and psychological symptoms and the adequacy of social supports | |||
| 5.Treatment of physical symptoms, including pain, with evidence-based approaches and validated care pathways | |||
| 6.Patient monitoring for the adequacy of relief, and adjustment of treatment strategies as necessary | |||
| 7.Access to specialist palliative or pain management care for patients and situations that exceed the capabilities of the primary level care providers | |||
| 8.Meticulous management of the adverse effects of treatment | |||
| 9.Availability of psychological and spiritual care for patients and their family members | |||
| 10.Ongoing care planning based on ongoing assessment, determined by goals set with patient and family, and with consideration of the changing benefit/burden of any treatment strategy” | |||
| Articles on “palliative care/medicine” | Study type | Definition(s) proposed or Information discussed | Citation source |
| Doyle. Palliative medicine—a time for definition? Palliat Med 1993 [22] | Editorial | Definition of palliative medicine “The study and management of patients with active, progressive, far-advanced disease for whom the prognosis is limited and the focus of care is the quality of life” | Not available |
| Sutherland et al. Definitions in paediatric palliative care. Health Trends 1993 [56] | Review | Definition of palliative care “care which is provided when curative treatment is not possible or not appropriate, and which personalizes the care of the whole child and family, focusing on the relief of physical, emotional, social and spiritual distress and aiming for the best possible quality of life” | Not available |
| Allen et al. What is palliative care? The Pharmaceutical Journal 1995 [5] | Review | Definition of palliative care “the active total care of patients whose disease no longer responds to curative treatment and for whom the goal must be the best quality of life for them and their families....It includes the control of pain and other distressing symptoms, and integrates both the psychological and spiritual aspects of care. Palliative care does not cause an early death but provides a support system which aims to allow patients to die with dignity, peacefully and free of pain. It also helps patients and their families to come to terms with death” | World Health Organization 1990 |
| Finlay et al. Definitions in palliative care. BMJ 1995 [27] | Letter to editor | Definition of specialist palliative care “Specialist palliative care is delivered by clinicians who have specialist accredited training. Specialist palliative care teams are multidisciplinary and relate to both general and hospital practice, being available to provide advice and support that bridges the divide between home and hospital and to provide hospice care. They cooperate with others rather than take over from them. Specialist palliative care has a duty to carry out research and, through effective education, to disseminate widely the lessons learnt. It must be available to support those giving care with a palliative approach” | Not available |
| Post et al. Palliative Care: a bioethical definition, principles and clinical guidelines. Bioethics Forum 1997 [51] | Review | Definition of palliative care “active intervention, which has as its goal the achievement of maximum comfort and function of the total patient. While palliation can and should always be an integral part of the entire spectrum of patient care, it stands alone as the care for the patient who has been diagnosed with an irreversibly deteriorating or terminal condition and for whom curative treatment is no longer the goal of care” | Consensus workgroup |
| Goodlin. What is palliative care. Hospital Practice 1997 [32] | Editorial | Definition of palliative care “care that | World Health Organization 1990 |
| • “affirms life and regards dying as a normal process | |||
| • neither hastens nor postpones death | |||
| • provides relief from pain and other distressing symptoms | |||
| • integrates the psychological and spiritual aspects of patient care | |||
| • offers a support system to help patients live as actively as possible until death and | |||
| • offers a support system to help the family cope during the patient's illness and in their own bereavement” | |||
| Billings. What is palliative care? J Palliat Med 1998 [9] | Review | Definition of palliative care “The active total care of patients whose disease is not responsive to curative treatment... Control of pain, of other symptoms, and of psychological, social, and spiritual problems is paramount. The goal of palliative care is achievement of the best possible quality of life for patients and their families. Many aspects of palliative care are also applicable earlier in the course of illness, in conjunction with anticancer treatment” | World Health Organization 1990 |
| Definition of palliative care “The study and management of patients with active, progressive, far-advanced disease for whom the prognosis is limited and the focus of care is the quality of life” | The Oxford Textbook of Palliative Medicine 1993 | ||
| Definition of palliative care “Palliative care is comprehensive, interdisciplinary care, focusing primarily on promoting quality of life for patients living with a terminal illness and for their families. Key elements for helping the patient and family live as well as possible in the face of life-threatening illness include assuring physical comfort, psychosocial and spiritual support, and provision of coordinated services across various sites of care” | Not available | ||
| Browde. Expanding the definition of palliative medicine and integrating it into the mainstream. South Afr Med J 2001 [13] | Review | Definition of palliative medicine “The active comprehensive care of the physical, emotional, psychosocial and spiritual suffering of the patient and the family with the aim of relieving suffering for those for whom cure is no longer possible” | World Health Organization 1990 |
| Definition of palliative medicine “The active comprehensive care of the physical, emotional, psycho-social and spiritual needs of the patient and the family with the aim of relieving suffering. It starts at the moment of diagnosis of any illness and continues for the duration of the illness. If and when the illness becomes incurable, then palliative care will play the major or the total role’” | Palliative Medicine Institute | ||
| defining palliative care. J Pharmacol Care Pain Symp Control 2001 [1] | Review | Definition of palliative care “Palliative care is the comprehensive management of a patient's physical, psychological, social, spiritual and existential needs. It can be part of the treatment of any person with a serious or life-threatening medical condition for which a patient-centered approach, pain and symptom control, family involvement and compassionate care are needed. Palliative care affirms life and regards dying as a natural process that is profoundly personal experience for the individual and the family. Palliative care neither hastens nor postpones death, but rather seeks to relieve suffering and provide comfort, control symptoms and restore functional capacity while remaining sensitive to personal, cultural and religious values, beliefs and practices” | Not available |
| Lipman. Defining hospice and palliative care. J Pharmacol Care Pain Symp Control 2001 [38] | Editorial | Definition of palliative care “Palliative care has been defined by the World Health Organization (WHO) as ‘the active total care of patients whose disease is not responsive to curative treatment.’ WHO notes that control of pain, of other symptom, and of psychological, social and spiritual problems is paramount. The goal of palliative care is achievement of the best quality of life for patients and their families.” | World Health Organization 1990 |
| Lamers. Defining hospice and palliative care: some further thoughts J Pain Palliat Care Pharm 2002 [37] | Review | Definition of palliative care “An approach focusing on relief of pain and other symptoms to the exclusion of curative therapies in persons with life-limiting illness” | World Health Organization 1990 |
| Definition of palliative care “The comprehensive management of the physical, psychological, social, spiritual and existential needs of patients. It is especially suited to the care of people with incurable, progressive illnesses” | Last Acts Task Force | ||
| Definition of palliative care “...treatment that enhances comfort and improves the quality of the patient's life. No specific therapy is excluded from consideration” | The National Hospice and Palliative Care Organization 1993 | ||
| Definition of palliative care “an equivalent (or euphemism) for hospice, used by Mount to name the hospital unit and comprehensive program in the Royal Victoria Hospital, Montreal, Quebec” | Not available | ||
| Definition of palliative medicine “a recognized medical specialty in the United Kingdom, Canada and some other countries that focuses on symptom relief for persons with advanced illness” | Not available | ||
| Definition of palliative medicine “the study and management of patients with active, progressive, far-advanced disease for whom the prognosis is limited and the focus of care is the quality of life” | The Oxford Textbook of Palliative Medicine 1998 | ||
| American Academy of Hospice and Palliative Medicine introduces new definitions. J Hosp Palliat Nurs 2003 [3] | Review | Definition of Palliative Medicine “The specialty of Palliative Medicine is the study and treatment of patients living with life-threatening or severe advanced illness expected to progress toward dying and where care is particularly focused on alleviating suffering and promoting quality of life. Major components are pain and symptom management, information sharing, advance are planning, and coordination of care, including psychosocial and spiritual support for patients and their families” | American Association for Hospice and Palliative Medicine 2003 |
| Definition of palliative care “Palliative Care is comprehensive, specialized care provided by an interdisciplinary team to patients and families living with a life-threatening or severe advanced illness expected to progress toward dying and where care is particularly focused on alleviating suffering and promoting quality of life. Major concerns are pain and symptom management, information sharing and advanced care planning, psychosocial and spiritual support, and coordination of care” | American Association for Hospice and Palliative Medicine 2003 | ||
| Doyle. Palliat Med 2003 [23] | Editorial | Definition of palliative care “the earlier palliative care starts the better” | World Health Organization 2002 |
| Van Kleffens et al. Clarifying the term ‘palliative’ in clinical oncology. Eur J Cancer Care 2004 [58] | Qualitative study (30 patients, 16 physicians) | Definition of palliative care “Palliative care is an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” | World Health Organization 2002 |
| Meghani et al. A concept analysis of palliative care in the United States. J Adv Nurs 2004 [43] | Concept analysis | Definition of palliative care “that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” | World Health Organization 2002 |
| Definition of palliative care “Comprehensive, specialized care provided by an interdisciplinary team to patients and families living with a life-threatening or severe advanced illness expected to progress toward dying and where care is particularly focused on alleviating suffering and promoting quality of life. Major concerns are pain and symptom management, information sharing and advance care planning, psychosocial and spiritual support, and coordination of care” | American Association for Hospice and Palliative Medicine 2003 | ||
| Definition of palliative care “Palliative care is appropriate for any patient and/or family living with, or at risk of developing a life-threatening illness due to any diagnosis, with any prognosis, regardless of age, at any time they have unmet expectations and/or needs, and are prepared to accept care....It may complement and enhance disease-modifying therapy, or it may become the total focus of care” | Center to Advance Palliative Care | ||
| O'Connor. Mission statements: an example of exclusive language in palliative care? Int J Palliat Nurs 2005 [45] | Discourse analysis | Examined 38 mission statements from various palliative care services in Australia. Key themes included: values of the service, patients, family, care, life-limiting illness, teamwork, quality of life | Not applicable |
| Mularski. Defining and measuring quality palliative and end-of-life care in the intensive care unit. Crit Care Med 2006 [44] | Review | Definition of palliative care “an approach that improves the quality of life...of patients and their families... [for] problems associated with life-threatening illness...through the prevention and relief of suffering by...early identification, ...assessment, and...treatment of pain and other problems, physical, psychosocial and spiritual’” | World Health Organization 2005 |
| Definition of palliative care “palliative care is medical treatment that aims to relieve suffering and improve quality of life simultaneously with all other appropriate treatment for patients with advanced illness, and their families” | Center to Advance Palliative Care: Definition of Palliative Care 2005 | ||
| Martin. Understanding palliative care. The Consultant Pharmacist 2006 [41] | Review | Definition of palliative care “the active total care of patients whose disease is not responsive to curative treatment... WHO suggests ‘active total care’ includes optimal pain control as well as control of other distressing symptoms such as nausea, dyspnea, and insomnia, while simultaneously addressing the patient's psychological, social, and spiritual needs” | World Health Organization 1990 |
| Standards for palliative care; also included National Consensus Project key elements of palliative care, including | National Consensus Project 2004 | ||
| “Structure and processes of care | |||
| Physical aspects of care | |||
| Psychological and psychiatric aspects of care | |||
| Social aspects of care | |||
| Spiritual, religious, and existential aspects of care | |||
| Cultural aspects of care | |||
| Care in the imminently dying patient | |||
| Ethical and legal aspects of care” | |||
| Ventafaridda. According to the 2002 WHO definition of Palliative Care. Palliat Med 2006 [59] | Editorial | Definition of palliative care “Palliative care is multidisciplinary and its approach is focused both on the patient and their family. It encompasses the care of the patient and family during the progression to incurable illness, the advanced stages of disease and the last hours of life. It is based on the integration of medical and other holistic treatments” | World Health Organization 2002 |
| Hanks. Palliative care: careless use of language undermines our identity. Palliat Med 2008 [33] | Editorial | Definition of palliative care “The term ‘palliative care’ implies a personalized form of health care. It extends the health care professional's mandate beyond the biomedical model to the wider horizon necessary if one is to attend to suffering as well as the biology of disease, caring as well as curing, quality of life as well as quantity of life. The patient and family or significant others are taken together as a unit of care in assessment of needs related to illness. The aim of palliative care is to support optimal quality of life and to foster healing—that is a shift in response towards an experience of integrity and wholeness on the continuum of the quality of life” | ABC of palliative care 2006 |
| Bekelman et al. Defining the role of palliative care in older adults with heart failure. Int J Cardiol 2008 [7] | Review | Definition of palliative care “Palliative care is ‘patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs and facilitating patient autonomy’” | National Quality Forum. A national framework and preferred practices for palliative and hospice care quality 2007 |
| Pastrana et al. A matter of definition—key elements identified in a discourse analysis of definitions of palliative care. Palliat Med 2008 [48] | Discourse analysis | A total of 37 English and 26 German definitions were identified and analyzed. No specific definition included in the text | Not applicable |
| The authors found that palliative care was defined in three ways: as function, as structure or as philosophy of care and organization. They also identified four main categories in discussing definition of palliative care: target groups, structure, tasks and expertise | |||
| Cherny et al. Stigma associated with “Palliative Care” Cancer 2009 [17] | Editorial | Definition of Palliative Care “Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” | World Health Organization 2007 |
| Definition of palliative care “the integration into cancer care of therapies to address the multiple issues that cause suffering for patients and their families and have an impact on the quality of their lives. Palliative cancer care aims to give patients and their families the capacity to realize their full potential, when their cancer is curable as well as when the end of life is near” | Ferris et al. J Clin Oncol 2009 | ||
| Batchelor. Palliative or hospice care? Understanding the similarities and differences. Rehab Nurs 2010 [6] | Review | Definition of Palliative Care “An approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problem, physical, psychosocial and spiritual” | World Health Organization 2002 |
| Definition of palliative care “Palliative care extends the principles of hospice care to a broader population that could benefit from receiving this type of care earlier in their illness or disease process. No specific therapy is excluded from consideration. An individual's needs must be continually assessed and treatment options should be explored and evaluated in the context of the individual's values and symptoms. Palliative care, ideally, would segue into hospice care as the illness progresses” | The National Hospice and Palliative Care Organization 2003 | ||
| Pautex et al. A Common definition of geriatric palliative medicine. JAGS 2010 [49] | Letter to editor | Definition of geriatric palliative medicine “GPM (Geriatric palliative medicine) is the medical care and management of older patients with health-related problems and progressive, advanced disease for which the prognosis is limited and the focus of care is quality of life” | Consensus workgroup |
| Articles on “hospice care” | Study type | Definition(s) proposed or Information discussed | Citation Source |
| Tehan. Hosp Forum. Standards for hospice address definition and quality concerns. 1980 [57] | Review | Standards of hospice care “The National Hospice Organization, in addition to dealing with these concerns, has recognized two potentially major problems for this burgeoning movement—the need for a formal definition of “hospice” and the maintenance of quality. The NHO has developed standards that will serve both to define a hospice program and to function as a basis for an eventual accreditation and licensure system | National Hospice Organization Standards Document |
| 1. Appropriate therapy is the goal of hospice care | |||
| 2. Palliative care is the most appropriate form of care when cure is no longer possible | |||
| 3. The goal of palliative care is the prevention of distress from chronic signs and symptoms | |||
| 4. Admission to a hospice program of care is dependent on patient and family needs and their expressed request for care | |||
| 5. Hospice care consists of a blending of professional and nonprofessional services | |||
| 6. Hospice care considers all aspects of the lives of patients and their families as valid areas of therapeutic concern. | |||
| 7. Hospice care is respectful of all patient and family belief systems, and will employ resources to meet the personal philosophic, moral, and religious needs of patients and their families | |||
| 8. Hospice care provides continuity of care | |||
| 9. A hospice care program considers the patient and the family together as the unit of care | |||
| 10. The patient's family is considered to be a central part of the hospice care team | |||
| 11. Hospice care programs seek to identify, coordinate, and supervise persons who can give care to patients who do not have a family member available to take on the responsibility of giving care | |||
| 12.Hospice care for the family continues into the bereavement period | |||
| 13.Hospice care is available 24 h a day, 7 days a week | |||
| 14. Hospice care is provided by an interdisciplinary team | |||
| 15. Hospice programs will have structured and informal means of providing support to staff | |||
| 16. Hospice programs will be in compliance with the Standards of the National Hospice Organization and the applicable laws and regulations governing the organization and delivery of care to patients and families | |||
| 17. The services of the hospice program are coordinated under a center administration | |||
| 18. The optimal control of distressful symptoms is an essential part of a hospice care program requiring medical, nursing, and other services of the interdisciplinary team | |||
| 19. The hospice care team will have: | |||
| a. a medical director on staff | |||
| b. physician on staff | |||
| c. a working relationship with the patient's physician | |||
| 20. Based on patient's needs and preferences as determining factors in the setting and location for care, a hospice program provides in-patient care and care in the home setting | |||
| 21. Education, training, and evaluation of hospice services is an ongoing activity of a hospice care program | |||
| 22. Accurate and current records are kept on all patients” | |||
| Sutherland et al. Definitions in paediatric palliative care. Health Trends 1993 [56] | Review | Definition of hospice care “Sister Frances Dominica emphasized that for children ‘hospice” retains its original meaning as a ‘place of rest and refreshment on a journey representing a whole philosophy of care rather than a physical facility | Dominica. Br J Hosp Med 1987 |
| Definition of Hospice Care “This philosophy is founded on the belief that children and their families should be offered help to achieve the best quality of life—physical, emotional and spiritual—through a child's lifetime and to help the bereave live on after the child's death. It is a philosophy, which can be translated into community-based care, by paediatric community nursing teams, without necessarily having the back-up of a hospice building. It may be helpful to separate ‘hospice’ from ‘hospice care’—using ‘hospice’ to denote a facility and ‘hospice care’ to refer to care provided in a hospice or other special building, or in the family home and community” | Not available | ||
| Definition of Hospice Care “flexible, individualized, supportive care, including palliative care when appropriate, provided in a hospice or elsewhere, which aims to achieve the best quality of life for the child and family and continues into bereavement for as long as necessary” | Not available | ||
| McCann. Hospice Care in the United States: The Struggle for definition and survival. J Palliat Care 1988 [42] | Review | Definition of Hospice Care “Although hospices differ in organizational structure and the employee status of those delivering care. These basic principles are as follows: | Not available |
| • The patient and the family are the unit of care | |||
| • Medicine, nursing, social work, spiritual, and bereavement services are available to patients and families in the inpatient and home settings | |||
| • The objectives of care are the management of physical and psychosocial symptoms | |||
| • Hospice services are available 24 h a day, 7 days a week | |||
| Care is available in both the home care and inpatient settings” | |||
| Definition of Hospice Care “Hospice in 1982 represented a beginning, an effort to make interdisciplinary team services available to any terminal patient in any setting. Hospice care in 1986 represented a service provided primarily in the home to patients whose care givers can manage their care 24 h a day, seven days a week, with intermittent visits from the hospice staff and some hourly relief from volunteers” | Not available | ||
| Mann et al. Hospice and/or Palliative Care? Am J Hosp Palliat Care 1997 [40] | Editorial | Definition of Hospice Care “Hospice care has to be understood as not only providing excellent pain control and symptom management but also for providing psychological and spiritual support.” | Not available |
| Billings. What is Palliative Care? J Palliat Med 1998 [9] | Review | Definition of hospice care “Hospice has come to mean primarily a governmentally regulated organization or program for dying persons and their families, typically focusing on home care, and limited to patients with: | Field et al. Institute of Medicine. Approaching Death: Improving care at the end of life. 1997 |
| 1. An expected prognosis of 6 months or less | |||
| 2. A focus on comfort measures—this is sometimes (but not always) defined by hospice programs as a desire to forego a variety of “aggressive” and often expensive management approaches (usually including cardiopulmonary resuscitation, blood product replacement, and some forms of radiotherapy, surgery, chemotherapy, and acute care hospitalization), at least insofar as these treatment modalities are being used in an attempt to cure or prolong life rather than to palliative symptoms | |||
| 3. A general preference for care at home (except where inpatient hospice is available and specifically sought) | |||
| 4. A willingness to sign a form acknowledging that they want to enter a hospice program and focus on comfort care | |||
| 5. Health insurance that covers hospice” | |||
| Chamberlain. What's in a name? Am J Hosp Palliat Care 2001 [14] | Editorial | No specific definition included in the text | Medicare Hospice Benefit |
| “Medical supplies and appliances including drugs and biological, provided as needed for the palliation and management of the terminal illness and related conditions” | |||
| “Radiation, chemotherapy, surgery, and other aggressive palliative measures have appropriate uses in hospice and palliative medicine, as long as the goal of therapy is symptom relief, and the benefits of treatment outweigh the burdens...all treatment options are explored and evaluated within the context of the patient's wishes and the goals of care” | American Academy of Hospice and Palliative Medicine 1999 | ||
| Lipman. Defining hospice and palliative care. J Pharmacol Care Pain Symp Control 2001 [38] | Editorial | Definition of Hospice Care “Hospice is a philosophy and program that delivers palliative care. Hospice care is provided by an interdisciplinary team that provides expert medical care, pain management, and emotional and spiritual support expressly tailored to the patient's wishes. Emotional and spiritual support also are extended to the family of the patient. In American hospice programs, care is usually provided in the patient's home or in a home-like setting operated by a hospice” | Not available |
| Jennings et al. What is hospice care? Hastings Center Report 2003 [36] | Review | Definition of Hospice Care “both a concept (that is, a philosophy and a paradigm of care) and an organizational form of health care delivery. Hospice services include professional nursing care, personal assistance with activities of daily living, various forms of rehabilitation therapy, dietary counseling, psychological and spiritual counseling for both patient and family, volunteer services, respite care, provision of medical drugs and devices necessary for palliative care, and family bereavement services following the patients death. Hospice care is provided by an interdisciplinary care team comprised of nurses, social workers, pastoral counselors, nursing assistants, and other health professionals under the management of a physician, who may be the patient's own primary care physician or may be affiliated directly with the hospice program” | Not available |
| Lamers. Defining hospice and palliative care: Some further thoughts J Pain Palliat Care Pharm 2002 [37] | Review | Definition of Hospice Care Initially a building in which dying persons receive care | Not available |
| Definition of Hospice Care Later a philosophy of improved care for dying persons; a program of care persons with lime-limiting illness; in French, Spain, and French Canada, a pejorative term (dysphemism) for an institution housing destitute persons | Not available | ||
| Definition of Hospice Care In the “United States, ‘hospice’ refers to a specific programmatic model for delivering palliative care. Hospice care, therefore, subsumes a subset of palliative care” | Byock et al. J Palliat Med 1998 | ||
| Definition of Hospice Care “The gold standard of palliative care” | Byock. 2001 | ||
| Definition of Hospice Care “in some parts of the United States (California), the word ‘hospice’ is also used by programs that do not provide the medical and nursing services requisite for Medicare certification” | Not available | ||
| Gazelle. Understanding hospice—an underutilized option for life's final chapter. NEJM 2007 [31] | Editorial | Concepts for Hospice Care “Medicare is the primary payer for hospice care in approximately 80 % of cases, with care most often provided in the patient's home... Under Medicare, most expenses related to the terminal diagnosis are paid in full, including all medication and equipment and all visits by hospice nurses and home health aides....Other hallmark hospice services include intensive emotional and spiritual counseling, 24-h crisis management, and bereavement support for at least 1 year after the patient's death... Hospice care can successfully address the critical end-of-life concerns that have been identified in numerous studies: dying with dignity, dying at home and without unnecessary pain, and reducing the burden placed on family caregivers” | Not available |
| Batchelor. Palliative or Hospice Care? Understanding the Similarities and Differences. Rehab Nurs 2010 [6] | Review | Definition of hospice care “an interdisciplinary approach to providing comprehensive care to those approaching the end of life. To quality for hospice services, a patient must be in the terminal phase of an illness with a life expectancy of 6 or fewer months as certified by two physicians (U.S. Department of Health and Human Services, 2001). Hospice care focuses on symptom management, which enables the patient to maintain dignity and quality of life. Hospice treats the person and family rather than the disease and affirms life, neither hastening nor prolonging death (NHPCO, 2008a)... Support and comfort care measures are employed so patients can live as fully and comfortably as possible” | National Hospice and Palliative Care Organization 2008 |
| Bosma et al. Cultural conceptualizations of hospice palliative care: more similarities than differences. Pall Med 2010 [12] | Systematic rview | A total of 15 studies on the cultural aspects of palliative care/hospice care and terminal care. No specific definition included in the text | NA |
| The authors found 3 major themes regarding palliative hospice care | |||
| 1. Hospice palliative care is holistic care | |||
| • Pain and symptom management | |||
| • Attending to unfinished business | |||
| • Spiritual and religious care | |||
| • Support to family, friends and professional care providers | |||
| • Quality of life and care choices | |||
| 2. Preferred qualities of health care providers | |||
| • Compassion, respect and kindness | |||
| • Speak clearly and listen carefully | |||
| • Don't talk about dying: focus on hope and optimism | |||
| • Knowledge ensures good care | |||
| 3. ‘Preempting burdens’ | |||
| • Put your affairs in order | |||
| • Families and friends need support |
Table 4.
Definitions for “palliative care,” “supportive care,” and “hospice care” from print and online dictionaries
| Print Dictionaries | Palliative care and palliative medicine | Supportive Care and Best Supportive Care | Hospice and hospice care |
|---|---|---|---|
| McGraw-Hill Allied Medical Dictionary (2008) | Palliative care. 1. Care based on the principles of hospice care, to enable persons with terminal diseases or conditions to receive assistance, therapy, comfort, and guidance before their illness progresses to the hospice stage. 2. Any care given to ease pain or distressing symptoms without treating the cause. | Supportive care. No entry | Hospice care. Physical, psychological, social, and spiritual care administered to dying patients and families |
| Palliative medicine. No entry | Best supportive care. No entry | Hospice. A facility that provides hospice care and care itself | |
| Dorland's Illustrated Medical Dictionary (2007) | Palliative care. No entry Palliative medicine. No entry |
Supportive Care. No entry Best supportive care. No entry |
Hospice care. No entry Hospice. A facility that provides palliative and supportive care for terminally ill patients and their families, either directly or on a consulting basis |
| Black's Medical Dictionary (2009) | Palliative care. The comprehensive care of patients and families facing terminal illness, focusing primarily on comfort and support. Such care includes: | Palliative medicine. No entry | Hospice care. No entry |
| –careful control of symptoms, especially PAIN –psychosocial and spiritual care –a personalised management plan centred on the patient's needs and wishes –care that takes into account the family's needs and that is carried into the bereavement period –provision of coordinated services in the home, hospital, day-care centre and other facilities used by the patient |
Best supportive care. No entry | Hospice. A hospital that cares only for the terminally ill and dying. The emphasis is on providing quality of life, and special care is taken in providing pain relief by whichever methods are deemed best suited to the person's needs. Hospice care in the UK has been greatly developed, generally funded by a combination of the NHS and charitable funds, with activities supported by voluntary workers | |
| Palliative medicine. No entry | |||
| Mosby's Medical Dictionary (2009) | Palliative care. No entry | Supportive care. No entry | Hospice care. No entry |
| Supportive medicine. No entry | Best supportive care. No entry | Hospice. A system of family centered care designed to assist the terminally ill person to be comfortable and to maintain quality of life through the phases of dying. Hospice care is a multidisciplinary and includes hoe visits, professional health care available on call, teaching and emotional support of the family, and physical care of the client. Some hospice programs provide care in a center, as well as in the home or in a nursing home. Hospice also offers bereavement counseling for the family | |
| Stedman's Medical Dictionary (2006) | Palliative care. No entry | Supportive care. No entry | Hospice care. No entry |
| Palliative medicine. No entry | Best supportive care. No entry | Hospice. An institution that provides a centralized program of palliative and supportive services to dying people and their families, in the form of physical, psychological, social and spiritual care; such services are provided by an interdisciplinary team of professionals and volunteers who are available in the home and in specialized inpatient settings | |
| Taber's Cyclopedic Medical Dictionary (2009) | Palliative care. No entry | Supportive care. No entry | Hospice care. No entry |
| Palliative medicine. No entry | Best supportive care. No entry | Hospice. An interdisciplinary program of palliative services that address the physical, spiritual, social, and economic needs of terminally ill patients and their families. This care may be provided in the home or a hospice center | |
| Online Dictionaries | Palliative care and palliative medicine | Supportive care and best supportive care | Hospice and hospice care |
| MediLexicon (2011) | Palliative care. No entry | Supportive care. No entry | Hospice care. No entry |
| Palliative medicine. No entry | Best supportive care. No entry | Hospice. 1. An institution that provides a centralized program of palliative and supportive services to dying people and their families, in the form of physical, psychological, social, and spiritual care; such services are provided by an interdisciplinary team of professionals and volunteers who are available in the home and in specialized inpatient settings. Source: Stedman's Medical Dictionary 28th Edition, Copyright© 2006 Lippincott | |
| Medical Dictionary (WebMD, 2011) | Palliative care. Syn. Palliative treatment. Treatment to alleviate symptoms without curing the disease | Supportive care. No entry | Hospice care. No entry |
| Palliative medicine. No entry | Best Supportive care. No entry | Hospice. 1. An institution that provides a centralized program of palliative and supportive services to dying people and their families, in the form of physical, psychological, social, and spiritual care; such services are provided by an interdisciplinary team of professionals and volunteers who are available in the home and in specialized inpatient settings. Source: Stedman's Medical Dictionary 28th Edition, Copyright© 2006 Lippincott | |
| MedlinePlus Medical Dictionary (2011) | Palliative care. No entry | Supportive care. No entry | Hospice care. No entry |
| Palliative medicine. No entry | Best supportive care. No entry | Hospice. A facility or program designed to provide a caring environment for meeting the physical and emotional needs of the terminally ill. Source: Merriam-Webster's Medical Dictionary, 2011 | |
| The Free Dictionary: Medical Dictionary (2009) | Palliative care. An approach to health care that is concerned primarily with attending to physical and emotional comfort rather than effecting a cure. Source: Jonas: Mosby's Dictionary of Complementary and Alternative Medicine | Supportive care. medical and other interventions that attempt to support and make comfortable rather than to cure. Source: Jonas: Mosby's Dictionary of Complementary and Alternative Medicine. (c) 2005, Elsevier. | Hospice care. No entry |
| Palliative medicine. No entry | Best supportive care. No entry | Hospice. A program or facility that provides palliative care and attends to the emotional, spiritual, social, and financial needs of terminally ill patients at a facility or at a patient's home. Source: The American Heritage Medical Dictionary, Copyright @ 2007, 2004, Houghton Mifflin. Hospice Care. No entry Hospice. A program under medical direction and nurse coordination that provides a variety of inpatient and home care for individuals who are terminally ill and their family members; provides calming and accommodating care that meets the special needs arising from the variety of stresses experienced during the final phases of illness, death, and grieving (e.g., emotional, physical, social, economic, and spiritual). Source: Mosby's Dental Dictionary, 2nd edition. © 2008 Elsevier, Inc. |
Table 5.
Definitions for “palliative care,” “supportive care,” and “hospice care” from various textbooks
| Textbooks | Palliative care and palliative medicine | Supportive care and best supportive care | Hospice and hospice care |
|---|---|---|---|
| Oxford Textbook of Palliative Medicine, 4th edition (2010) | Palliative Care. [WHO] an ‘approach which improves the quality of life of patients and their families facing life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychological, and spiritual’. (p. 58) [ESMO] care that aims to optimize the comfort, function, and social support of the patient and their family when cure is not possible (p. 111) | Supportive Care. [ESMO] Aims to optimize the comfort function, and social support of the patient and their family at all stages of the illness (p. 111) | Hospice care. No entry. A table describing various types of hospice care (routine home care, continuous home care, general inpatient care, inpatient respite care) can be found in p. 18 but it did not provide a definition for the specific term “hospice care” |
| Palliative Medicine. [Uncited definition #1] Physician discipline within the broad therapeutic model known as palliative care (p. 1586) | Best supportive care. No entry | Hospice. No entry | |
| Textbook of Palliative Medicine, 1st edition (2006) | Palliative Care. [EAPC,1998] 1. The active, total care of the patients hose disease is not responsive to curative treatment. Control of pain, or other symptoms, and of social, psychological and spiritual problems in paramount. 2. Interdisciplinary in its approach and encompasses the patient, the family and community in its scope. In a sense, palliative care is to offer the most basic concept of care- that is providing for the needs of the patient wherever he or she is cared for, either at home or in the hospital. 3. Affirms life and regards dying as a normal process; it neither hastens nor postpones death. It sets out to preserve the best possible quality of life until death. (p. 14) [African] 1. The active total care of patients whose disease is not responsive to curative treatment. 2. Control of pain and of other symptoms and of psychologic, social and spiritual problems is paramount. 3. The goal is achievement of the best possible quality of life for patients and their families. (p. 42) [WHO] an approach which improves quality of life of patients and their families facing life-threatening illness through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychological, and spiritual. (p. 69) [AIDS] patient- and family-centered care, which optimizes quality of life by active anticipation, prevention, and treatment of suffering. Respectful and trusting relationships are the foundation used by the interdisciplinary team throughout the continuum of illness to address physical, intellectual, emotional, social and spiritual needs and facilitate patient autonomy, access to information, and choice (p. 71) | Supportive care. No entry | Hospice care. No entry |
| Palliative Medicine. No entry | Best Supportive Care. No entry | Hospice. A model designed to provide care at the end of life (p. 271) | |
| Principles and Practice of Palliative Care and Supportive Oncology, 3rd edition (2007) | Palliative Care. [National Consensus Project] the goal of palliative care is to prevent and relieve suffering and to support the best possible quality of life for patients and their families, regardless of the stage of the disease or the need for other therapies. Palliative care is both a philosophy of care and an organized, highly structured system for delivering care. Palliative care expands traditional disease-model medical treatments to include the goals of enhancing quality of life for patients and family, optimizing function, helping with decision making and providing opportunities for personal growth. As such, it can be delivered concurrently with life-prolonging care or as the main focus of care. (p. 496) [WHO, 1990] Active total care of patients whose disease is not responsive to curative treatment... Control of pain, of other symptoms, and of psychological, social, and spiritual problems is paramount. The goal of palliative care is achievement of the best possible quality of life for patients and their families. Many aspects of palliative care are also applicable earlier in the course of the illness, in conjunction with anticancer treatment. (p. 490) [Oxford text book of palliative medicine, 1993] The study and management of patients with active, progressive, far-advanced disease for whom the prognosis is limited and the focus of care is the quality of life. (p. 490) [Uncited definition #1] An approach to management of terminal illness that focuses on symptom control and support rather than a cure or life prolongation (p. 490) [Uncited definition #2] Palliative care is s special service to help patients and their families live as well as possible in the face of a serious or life-threatening illness.(p 496) [Uncited definition #3] comprehensive medical care focused on relieving the suffering of patients facing serious or life-threatening illness and that of their families (p. 655) | Supportive care. No entry | Hospice care. No entry |
| Palliative Medicine. [Dr. Balfour Mount] medical discipline of hospice care (p. 501) The authors also stated that the ‘scope of palliative medicine remains an issue for debate, ranging from broad definition as “alleviation of symptoms,” “improving quality of life,” or treating patients “not responsive to curative treatment” or with “complex and serious illness” to extremely narrow notion of “care in the final months of life” or subspecialty of oncology’.(p489) | Best supportive care. No entry | Hospice. [Uncited definition #1] Best defined as most intensive, refined form of palliative care. Hospice is a philosophy of care that recognizes that the disease is not curable, that time is limited to months at best and that symptom control and quality of life are preeminent goals.(p500) [Uncited definition #2] a free standing unit where dying persons reside and receive care (p. 489) | |
| Palliative Medicine, 1st edition (2009) | Palliative Care. [Service organization perspectives] The comprehensive, active care of patients with advanced disease or serious illness and their families; it aims to improve quality of life based on patient and family needs, demands, and wishes and is practiced by a competent multidisciplinary team. (p. 23) [Uncited definition #1] refers to the comprehensive management of the physical, psychological, social, spiritual and existential needs of patients. It is especially suited to the care of people with incurable, progressive illness. (p. 35) | Supportive care. No entry | Hospice care. No entry |
| Palliative Medicine. Medical discipline of the broad therapeutic model known as palliative care (p. 119) | Best supportive care. No entry | Hospice. [Uncited definition #1] A concept of care, not a specific place; it is a philosophy rather than a building or service [Uncited definition #2] Holistic approach (physical, psychological, social, and spiritual) (p. 18). [1842, Lyon, France] place for the terminally ill (p. 19) Independent organization devoted to the care of patients and their families, based in the community, often in a specific, dedicated building (p. 26) | |
| Principles and Practice of Supportive Oncology 1st edition (1998) | Palliative Care [WHO] active total care of patients whose disease is not responsive to curative treatment (p. 845) | Supportive care. No entry | Hospice. [US] system that pays for the care of the dying. [Other parts of the world] a place for care of the indigent (p. 737) |
| Palliative Medicine. [Dr. Derek Doyle] the study and management of patients with active, progressive, far-advanced disease for whom the prognosis is limited and the focus of care is quality of life (p. 737) | Best supportive care. No entry | Hospice care. No entry |
Concepts and definitions for “palliative care” and “palliative medicine”
Our search revealed 25 articles on “palliative care/medicine” (Table 1). The authors were predominantly from the USA (N=11) and Europe (N=10) and represented multiple disciplines including medicine (N=14), nursing (N=4), pharmacy (N=3), and others (N=4).
Common concepts defining palliative care included quality of life and symptom control (N=24/25), interdisciplinary care (N=20/25), caregiver support (N=22/25), and patients with life-limiting advanced illness (N=25/25). Twelve of the 25 articles discussed the role of palliative care earlier in the disease trajectory (Table 1). Eleven of the 25 articles reported “palliative care” as confusing and 8 of 25 described the euphemistic use of terms in palliative care.
Among 4 terminology research original studies, 5 organization statements, 6 editorials commenting on definitional issues, and 10 articles explaining the role of palliative care, we found 24 unique definitions for palliative care/medicine (Table 2). Definitions cited included those from the World Health Organization, the American Association for Hospice and Palliative Medicine, the Center to Advanced Palliative Care, the National Consensus Project, the National Quality Forum, the National Hospice and Palliative Care Organization, the American Society of Clinical Oncology, the Palliative Medicine Institute, and two textbooks (the Oxford Textbook of Palliative Medicine, the ABCs of Palliative Care). The World Health Organization 1990 and 2002 criteria were cited most often in 14 of 25 articles (Table 3). The term “palliative medicine” was used interchangeably with “palliative care” (Table 3).
Our dictionary search revealed four definitions for “palliative care” and 0 for “palliative medicine” (Table 4). Palliative care textbooks provided a total of 15 definitions for “palliative care,” with four of five textbooks referring to the WHO definition (Table 5). “Palliative medicine” was defined in four of five textbooks.
Concepts and definitions for “hospice care”
The concept of “hospice care” was examined in five editorials, two organization statements, and five review articles (Table 1). Hospice care was mostly discussed in the context of the USA (N=10). Five of 12 articles found this term “confusing,” and 5 of 12 discussed fear associated with the use of this term.
The key concepts discussed in these articles were symptom management (N=12/12), interprofessional care (N=11/12), caregiver involvement (N=11/12), and bereavement services (N=9/12). Five of the 12 articles discussed the 6-month prognosis criterion for hospice admission (N=5/12) (Table 1). Nine of the 12 articles discussed hospice as predominantly community based, and 6 of 12 also described inpatient services. Compared to “supportive care” and “palliative care,” “hospice care” emphasized more on the role of volunteers, bereavement care, and community care (Table 2).
Overall, 17 definitions were available for “hospice care” from 12 articles (Table 3). All print and online dictionaries and textbooks provided a definition for “hospice,” describing it as a philosophy, a system, a program or a facility. (Tables 4 and 5).
Discussion
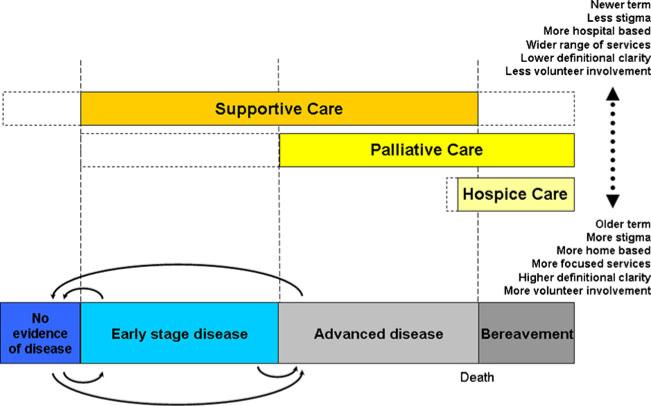
The use of the terms “best/supportive care,” “palliative care,” and “hospice care” have been of interest to many individuals, including Dr. Cicely Saunders [54]. In this systematic review, we examined empirical data from the literature and identified defining concepts for “best/supportive care,” “palliative care,” and “hospice care.” Our search revealed a wide range of definitions for these terms, with significant overlaps yet many distinguishing features. Based on our findings, we developed a preliminary conceptual framework unifying these terms along the continuum of care to help build consensus toward standardized definitions.
The term “supportive care” has been in existence for several decades [47] and is part of the name of the organization “Multinational Association of Supportive Care in Cancer” and its association journal Supportive Care in Cancer. “Supportive care” is also the name of multiple textbooks, such as Cancer Supportive Care and Supportive Care in Cancer Therapy.
Consistent with our previous study [35], we found that “supportive care” and “best supportive care” were used interchangeably at times, and both were variably defined with a wide spectrum of definitions. The scope of services under “supportive care” ranged from the use of hydroxyurea for patients with acute leukemia to survivorship care [17, 47, 52]. When Fitch et al. developed the Supportive Care framework in 1994, it was described as a comprehensive program to meet “patients’ physical, informational, emotional, psychological, social, spiritual, and practical needs during the prediagnostic, diagnostic, treatment and follow-up phases” [28–30]. This definition was consistent with other articles identified in our search [17, 47]. A questionnaire named the “Supportive Care Needs Survey” has been developed and subsequently validated to include five domains: physical and daily living, psychological needs, sexuality, patient care and support needs, and health system and information needs [11, 53, 55]. The “supportive care” population included patients on cancer treatment needing symptom support to those with life-limiting illness and their families. Almost half of the authors commented that “best supportive care” is essentially equivalent to “palliative care” [15, 18, 20, 39]. Recognizing the importance of definitional clarity for these two terms, a number of investigators have taken the initiative to develop consensus definitions through the Delphi process [15, 19].
In contrast to “supportive care,” “palliative care” was relatively more homogeneously defined. “palliative care” involves interdisciplinary care focusing on improving patients’ quality of life by addressing their physical, emotional, and spiritual needs, and on supporting their families. Our findings are consistent with those of a concept analysis study [43]. The WHO definition [2] captured the essential features of “Palliative care,” and was cited the most often. Although all definitions unanimously agreed that “Palliative care” serves patients with life-limiting illness, there has been some debate whether it involves patients with curable disease as well.
There appears to be general consensus on what constitutes “hospice care”—a predominantly community based program that provides interprofessional multidimensional care for patients with terminal illness (i.e., expected survival <6 months) and their families, working in conjunction with volunteers to provide services ranging from symptom management to bereavement care. “Hospice care” was considered to be under the spectrum of “palliative care” by several authors [9, 37].
By examining “supportive care,” “palliative care,” and “hospice care” together, we are able to highlight the significant similarities and differences among these terms. All three terms denote interprofessional care to optimize quality of life; however, the scope of service, patient population, and how each is perceived differ significantly (Fig. 2). Chronologically, “hospice care” is the earliest term. Understandably, it is more often defined in dictionaries compared to “supportive care,” which is a newer term with an evolving meaning. “Palliative care” is somewhere in between. “Hospice care” is limited to patients with terminal illness (i.e., prognosis 6 months or less in the USA), while “supportive care” is expanding its services to address the full range of issues from survivorship to bereavement. Finally, “hospice care” and to a certain extent “palliative care” are associated with a lot of stigma because of their association with death and dying. In contrast, “supportive care” is gaining popularity as the name for some “palliative care” programs because it is less likely to provoke anxiety [21, 24].
Fig. 2.
A conceptual framework toward understanding “supportive care,” “palliative care,” and “hospice care.” Based on our systematic review, the stage of disease was a key distinguishing factor among “best/supportive care,” “palliative care,” and “hospice care.” Thus, the different stages of disease are depicted at the bottom, with solid arrows showing that patients can shift from one stage to another. The patient population and scope of service for “supportive care,” “palliative care,” and “hospice care” is shown by the horizontal bars above. Under this model, “hospice care” is part of “palliative care,” which in turn, is part of “supportive care.” Importantly, the dashed boxes illustrate the evolving nature of these definitions to expand their scope of service. For instance, in addition to providing care to patients on treatment, some of the definitions of “supportive care” also included a more comprehensive description involving cancer survivors and the bereaved. Similarly, an increasing number of articles suggest that “palliative care” should start from the time of diagnosis. Other distinguishing features among the three terms are listed on the right hand side
Based on our review, we developed a preliminary conceptual framework (Fig. 2) aimed to highlight the overlapping yet unique function of each term. Under this model, “hospice care” is part of “palliative care,” which in turn is under the umbrella of “supportive care.” Our conceptual framework, which shares some similarities to a proposed model in the Oxford Textbook of Palliative Medicine [16], is developed independently based on findings from our literature review. It may help clinicians, researchers, and policy makers put the three terms in context of the existing literature, and ultimately formulate a consensus toward standardized definitions for these terms. Importantly, this model is an evolving one based on our finding that “supportive care,” “palliative care,” and “hospice care” are all actively expanding their services to reach patients earlier in the disease trajectory.
To our knowledge, this is the most comprehensive examination of these four commonly used terms. A number of investigators have conducted systematic reviews with a narrower focus. For instance, Cherny et al. [18] examined the meaning of “best supportive care” and “supportive care” in oncology clinical trials. Meghani [43] carried out a concept analysis of “palliative care” and “hospice,” although the number of studies in the final sample was not reported. Bosma et al. [12] also performed a systematic review of “hospice palliative care” limited to studies that focused on cultural conceptualizations. Importantly, our findings are consistent with these studies, and bring a new perspective by putting these terms in context of each other.
Our study has several limitations. First, our initial search strategy may not have captured all the articles relevant to our interest. This strategy was developed in conjunction with professional medical librarians to ensure a balance between sensitivity and specificity. We only examined the peer-reviewed literature focusing on conceptualizing/defining the terms of interest and did not specifically retrieve definitions from various organizations because a majority of them were already cited and discussed in the papers (Table 3). Second, we did not review the gray literature or conduct a hand search of abstracts. Third, our search was limited to the English language, and hence, cultural variations in definitions for these terms could not be examined. This could potentially limit the generalizability of our study findings on an international basis. Fourth, we did not conduct a construct or linguistic analysis. Future studies may benefit from more in-depth examination of the concepts identified in this study. Fifth, we did not specifically examine the meaning of each term by geographic region. Further studies are required to determine how these terms may be interpreted in various continents. Finally, our study did not examine new hybrid terms such as “supportive and palliative oncology,” “palliative and supportive services,” “psychosocial oncology,” and “hospice palliative care.”
Palliative care has evolved from a philosophy of care for the dying to an interprofessional discipline that addresses quality of life for patients and their families throughout the disease trajectory [60]. As this discipline matures, we urgently need consensus definitions to help standardize clinical care, research, and program development. The preliminary conceptual framework based on our systematic review may help clarify the relative meaning of these important terms and facilitate the synthesis of standardized definitions through consensus building among various international supportive, palliative, and hospice care organizations. Rather than trichotomizing patient care into three different services, this model supports the provision of patient care by a single discipline comprised of a team of healthcare professionals with expertise in symptom management, psychosocial care, spiritual support, caregiver care, communication, and complex decision-making skills and end-of-life care.
Acknowledgments
Dr. Hui is supported in part by an institutional startup grant #18075582. Dr. Bruera is supported in part by National Institutes of Health grants RO1NR010162-01A1, RO1CA122292-01, and RO1CA124481-01. Dr. Torres-Vigil is supported in part by a National Cancer Institute grant 1K01CA151785-01.This study is also supported by the MD Anderson Cancer Center Support Grant (CA 016672). The sponsors of the study had no role in study design, data collection, analysis, interpretation, or writing of the report.
Footnotes
Conflict of Interest
No relevant financial conflict of interest reported for all authors. D.H. has full control of all primary data, and the journal may review the data if requested.
Contributor Information
David Hui, Department of Palliative Care & Rehabilitation Medicine Unit 1414, University of Texas M.D. Anderson Cancer Center, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Maxine De La Cruz, Department of Palliative Care & Rehabilitation Medicine Unit 1414, University of Texas M.D. Anderson Cancer Center, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Masanori Mori, Department of Palliative Medicine, Seirei Hamamatsu General Hospital, Shizuoka, Japan.
Henrique A. Parsons, Department of Palliative Care & Rehabilitation Medicine Unit 1414, University of Texas M.D. Anderson Cancer Center, 1515 Holcombe Boulevard, Houston, TX 77030, USA
Jung Hye Kwon, Department of Palliative Care & Rehabilitation Medicine Unit 1414, University of Texas M.D. Anderson Cancer Center, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Isabel Torres-Vigil, Department of Palliative Care & Rehabilitation Medicine Unit 1414, University of Texas M.D. Anderson Cancer Center, 1515 Holcombe Boulevard, Houston, TX 77030, USA; Graduate College of Social Work, University of Houston, Houston, TX, USA.
Sun Hyun Kim, Department of Family Medicine, Myong Ji Hospital, Kwandong University, College of Medicine, Gyeonggi, South Korea.
Rony Dev, Department of Palliative Care & Rehabilitation Medicine Unit 1414, University of Texas M.D. Anderson Cancer Center, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
Ronald Hutchins, Research Medical Library, The University of Texas MD Anderson Cancer Center, Houston, TX, USA.
Christiana Liem, Research Medical Library, The University of Texas MD Anderson Cancer Center, Houston, TX, USA.
Duck-Hee Kang, The University of Texas Health Science Center at Houston School of Nursing, Houston, TX, USA.
Eduardo Bruera, Department of Palliative Care & Rehabilitation Medicine Unit 1414, University of Texas M.D. Anderson Cancer Center, 1515 Holcombe Boulevard, Houston, TX 77030, USA.
References
- 1.Defining palliative care: Moyers on dying J Pharmaceut Care Pain Symptom Control. 2001;9(2):63–67. [Google Scholar]
- 2.WHO . WHO definition of palliative care. World Health Organization; Geneva: 2002. [Google Scholar]
- 3.American Academy of Hospice and Palliative Medicine introduces new definitions J Hosp Palliat Nurs. 2003;5(2):71. [Google Scholar]
- 4.NIH state-of-the-science conference statement on improving end-of-life care NIH Consens State Sci Statements. 2004;21(3):1–26. [PubMed] [Google Scholar]
- 5.Allen M. (1) What is palliative care? Pharm J. 1995;254(6830):293–294. [Google Scholar]
- 6.Batchelor NH. Palliative or hospice care? Understanding the similarities and differences. Rehabil Nurs. 2010;35(2):60–64. doi: 10.1002/j.2048-7940.2010.tb00032.x. [DOI] [PubMed] [Google Scholar]
- 7.Bekelman DB, Hutt E, Masoudi FA, Kutner JS, Rumsfeld JS. Defining the role of palliative care in older adults with heart failure. Int J Cardiol. 2008;125(2):183–190. doi: 10.1016/j.ijcard.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Benini F, Fabris M, Pace DS, Verno V, Negro V, De Conno F, Orzalesi MM. Awareness, understanding and attitudes of Italians regarding palliative care. Ann Ist Super Sanita. 2011;47(3):253–259. doi: 10.4415/ANN_11_03_03. [DOI] [PubMed] [Google Scholar]
- 9.Billings JA. What is palliative care? J Palliat Med. 1998;1(1):73–81. doi: 10.1089/jpm.1998.1.73. [DOI] [PubMed] [Google Scholar]
- 10.Board IOMNCP . Improving palliative care for cancer. Institute of Medicine; Washington: 2001. [Google Scholar]
- 11.Bonevski B, Sanson-Fisher R, Girgis A, Burton L, Cook P, Boyes A. Evaluation of an instrument to assess the needs of patients with cancer. Support Care Rev Group Cancer. 2000;88(1):217–225. doi: 10.1002/(sici)1097-0142(20000101)88:1<217::aid-cncr29>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 12.Bosma H, Apland L, Kazanjian A. Cultural conceptualizations of hospice palliative care: more similarities than differences. Palliat Med. 2010;24(5):510–522. doi: 10.1177/0269216309351380. [DOI] [PubMed] [Google Scholar]
- 13.Browde S. Expanding the definition of palliative medicine and integrating it into the mainstream. S Afr Med J. 2001;91(9):732–733. [PubMed] [Google Scholar]
- 14.Chamberlain BH. What's in a name? Am J Hosp Palliat Care. 2001;18(6):367–369. doi: 10.1177/104990910101800602. [DOI] [PubMed] [Google Scholar]
- 15.Cherny N. Best supportive care: a euphemism for no care or a standard of good care? Semin Oncol. 2011;38(3):351–357. doi: 10.1053/j.seminoncol.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Cherny N, Catane R. Palliative medicine and modern cancer care. In: Hanks G, Cherny N, Christakis N, Fallai M, Kaasa S, Portenoy RK, editors. Oxford textbook of palliative medicine. Oxford University Press; New York: 2010. pp. 111–124. [Google Scholar]
- 17.Cherny NI. Stigma associated with “palliative care”: getting around it or getting over it. Cancer. 2009;115(9):1808–1812. doi: 10.1002/cncr.24212. [DOI] [PubMed] [Google Scholar]
- 18.Cherny NI, Abernethy AP, Strasser F, Sapir R, Currow D, Zafar SY. Improving the methodologic and ethical validity of best supportive care studies in oncology: lessons from a systematic review. J Clin Oncol. 2009;27:5476–5486. doi: 10.1200/JCO.2009.21.9592. [DOI] [PubMed] [Google Scholar]
- 19.Cramp F, Bennett M. Development of a generic working definition of ‘supportive care’. BMJ Support Palliat Care. 2012 doi: 10.1136/bmjspcare-2012-000222. http://spcare.bmj.com/content/early/2012/08/02/bmjspcare-2012-000222.full. [DOI] [PubMed]
- 20.Cullen M. ‘Best supportive care’ has had its day. Lancet Oncol. 2001;2(3):173–175. doi: 10.1016/S1470-2045(00)00260-6. [DOI] [PubMed] [Google Scholar]
- 21.Dalal S, Palla S, Hui D, Nguyen L, Chacko R, Li Z, Fadul N, Scott C, Thornton V, Coldman B, Amin Y, Bruera E. Association between a name change from palliative to supportive care and the timing of patient referrals at a comprehensive cancer center. Oncologist. 2011;16(1):105–111. doi: 10.1634/theoncologist.2010-0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doyle D. Palliative medicine—a time for definition? Palliat Med. 1993;7(4):253–255. doi: 10.1177/026921639300700401. [DOI] [PubMed] [Google Scholar]
- 23.Doyle D. Proposal for a new name as well as having the new WHO definition of palliative care. Palliat Med. 2003;17(1):9–10. doi: 10.1191/0269216303pm651ed. [DOI] [PubMed] [Google Scholar]
- 24.Fadul N, Elsayem A, Palmer JL, Del Fabbro E, Swint K, Li Z, Poulter V, Bruera E. Supportive versus palliative care: what's in a name?: a survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer. 2009;115(9):2013–2021. doi: 10.1002/cncr.24206. [DOI] [PubMed] [Google Scholar]
- 25.Fallon M, Smyth J. Terminology: the historical perspective, evolution and current usage—room for confusion? Eur J Cancer. 2008;44(8):1069–1071. doi: 10.1016/j.ejca.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 26.Ferris FD, Bruera E, Cherny N, Cummings C, Currow D, Dudgeon D, Janjan N, Strasser F, von Gunten CF, Von Roenn JH. Palliative cancer care a decade later: accomplishments, the need, next steps. J Clin Oncol. 2009;27(18):3052–3058. doi: 10.1200/JCO.2008.20.1558. [DOI] [PubMed] [Google Scholar]
- 27.Finlay IG, Jones RV. Definitions in palliative care. BMJ. 1995;311(7007):754. doi: 10.1136/bmj.311.7007.754a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fitch M. Providing supportive care for individuals living with cancer. Ontario Cancer Treatment and Research Foundation; Toronto: 1994. [Google Scholar]
- 29.Fitch M. Supportive care for cancer patients. Hosp Q. 2000;3(4):39–46. doi: 10.12927/hcq..16542. [DOI] [PubMed] [Google Scholar]
- 30.Fitch MI. Supportive care framework. Can Oncol Nurs J. 2008;18(1):6–24. doi: 10.5737/1181912x181614. [DOI] [PubMed] [Google Scholar]
- 31.Gazelle G. Understanding hospice—an underutilized option for life's final chapter. N Engl J Med. 2007;357(4):321–324. doi: 10.1056/NEJMp078067. [DOI] [PubMed] [Google Scholar]
- 32.Goodlin SJ. What is palliative care? Hosp Pract (Minneap) 1997;32(2):13–16. doi: 10.1080/21548331.1997.11443418. [DOI] [PubMed] [Google Scholar]
- 33.Hanks G. Palliative care: careless use of language undermines our identity. Palliat Med. 2008;22(2):109–110. doi: 10.1177/0269216308089301. [DOI] [PubMed] [Google Scholar]
- 34.Hanratty B, Hibbert D, Mair F, May C, Ward C, Corcoran G, Capewell S, Litva A. Doctors’ understanding of palliative care. Palliat Med. 2006;20(5):493–497. doi: 10.1191/0269216306pm1162oa. [DOI] [PubMed] [Google Scholar]
- 35.Hui D, Mori M, Parsons H, Li ZJ, Damani S, Evans A, Bruera E. The lack of standard definitions in the supportive and palliative oncology literature. J Pain Symptom Manag. 2012;43(3):582–592. doi: 10.1016/j.jpainsymman.2011.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jennings B. I. What is hospice care hastings cent. Rep Spec Suppl. 2003;33(2):S6–S12. [Google Scholar]
- 37.Lamers WM., Jr Defining hospice and palliative care: some further thoughts. J Pain Palliat Care Pharmacother. 2002;16(3):65–71. doi: 10.1080/j354v16n03_07. [DOI] [PubMed] [Google Scholar]
- 38.Lipman AG. Defining hospice and palliative care. J Pharmaceut Care Pain Symptom Contr. 2001;9(1):1–3. [Google Scholar]
- 39.MacDonald N. Best supportive care. Cancer Prev Control. 1998;2(4):191–192. [PubMed] [Google Scholar]
- 40.Mann SM, Welk TA. Hospice and/or palliative care? Am J Hosp Palliat Care. 1997;14(6):314–315. doi: 10.1177/104990919701400611. [DOI] [PubMed] [Google Scholar]
- 41.Martin CM. Understanding palliative care. Consult Pharm. 2006;21(9):698–713. doi: 10.4140/tcp.n.2006.698. [DOI] [PubMed] [Google Scholar]
- 42.McCann BA. Hospice care in the United States: the struggle for definition and survival. J Palliat Care. 1988;4(1–2):16–18. [PubMed] [Google Scholar]
- 43.Meghani SH. A concept analysis of palliative care in the United States. J Adv Nurs. 2004;46:152–161. doi: 10.1111/j.1365-2648.2003.02975.x. [DOI] [PubMed] [Google Scholar]
- 44.Mularski RA. Defining and measuring quality palliative and end-of-life care in the intensive care unit. Crit Care Med. 2006;34(11 Suppl):S309–S316. doi: 10.1097/01.CCM.0000241067.84361.46. [DOI] [PubMed] [Google Scholar]
- 45.O'Connor M. Mission statements: an example of exclusive language in palliative care? Int J Palliat Nurs. 2005;11(4):190–195. doi: 10.12968/ijpn.2005.11.4.18041. [DOI] [PubMed] [Google Scholar]
- 46.O'Neill JE. What is supportive care and why is it important? J Pediatr Oncol Nurs. 2000;17(3):133–134. doi: 10.1053/jpon.2000.8164. [DOI] [PubMed] [Google Scholar]
- 47.Page B. What is supportive care? Can Oncol Nurs J. 1994;4:62–63. [Google Scholar]
- 48.Pastrana T, Junger S, Ostgathe C, Elsner F, Radbruch L. A matter of definition—key elements identified in a discourse analysis of definitions of palliative care. Palliat Med. 2008;22(3):222–232. doi: 10.1177/0269216308089803. [DOI] [PubMed] [Google Scholar]
- 49.Pautex S, Curiale V, Pfisterer M, Rexach L, Ribbe M, Van Den Noortgate N. A common definition of geriatric palliative medicine. J Am Geriatr Soc. 2010;58(4):790–791. doi: 10.1111/j.1532-5415.2010.02791.x. [DOI] [PubMed] [Google Scholar]
- 50.Payne S, Sheldon F, Jarrett N, Large S, Smith P, Davis CL, Turner P, George S. Differences in understanding of specialist palliative care amongst service providers and commissioners in South London. Palliat Med. 2002;16(5):395–402. doi: 10.1191/0269216302pm572oa. [DOI] [PubMed] [Google Scholar]
- 51.Post LF, Dubler NN. Palliative care: a bioethical definition, principles, and clinical guidelines. Bioeth Forum. 1997;13(3):17–24. [PubMed] [Google Scholar]
- 52.Ritchie EK, Roboz GJ. Levels of care: defining best supportive care in elderly patients with acute myeloid leukemia. Curr Hematol Malig Rep. 2010;5(2):95–100. doi: 10.1007/s11899-010-0048-8. [DOI] [PubMed] [Google Scholar]
- 53.Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer. Support Care Review Group Cancer. 2000;88(1):226–237. doi: 10.1002/(sici)1097-0142(20000101)88:1<226::aid-cncr30>3.3.co;2-g. [DOI] [PubMed] [Google Scholar]
- 54.Saunders C. What's in a name? Palliat Med. 1987;1(1):57–61. [Google Scholar]
- 55.Schofield P, Gough K, Lotfi-Jam K, Aranda S. Validation of the Supportive Care Needs Survey-short form 34 with a simplified response format in men with prostate cancer. Psychooncology. 2012 doi: 10.1002/pon.2016. http://onlinelibrary.wiley.com/doi/10.1002/pon.2016/pdf. [DOI] [PubMed]
- 56.Sutherland R, Hearn J, Baum D, Elston S. Definitions in paediatric palliative care. Health Trends. 1993;25(4):148–150. [PubMed] [Google Scholar]
- 57.Tehan CB. Standards for hospice address definition and quality concerns. Hosp Forum. 1980;23(1):16–17. [PubMed] [Google Scholar]
- 58.van Kleffens T, Van Baarsen B, Hoekman K, Van Leeuwen E. Clarifying the term ‘palliative’ in clinical oncology. Eur J Cancer Care (Engl) 2004;13(3):263–271. doi: 10.1111/j.1365-2354.2004.00481.x. [DOI] [PubMed] [Google Scholar]
- 59.Ventafridda V. According to the 2002 WHO definition of palliative care. Palliat Med. 2006;20(3):159. doi: 10.1191/0269216306pm1152ed. [DOI] [PubMed] [Google Scholar]
- 60.von Gunten CF, Lupu D. Development of a medical subspecialty in palliative medicine: progress report. J Palliat Med. 2004;7(2):209–219. doi: 10.1089/109662104773709332. [DOI] [PubMed] [Google Scholar]
- 61.Zafar SY, Currow D, Abernethy AP. Defining best supportive care. J Clin Oncol. 2008;26(31):5139–5140. doi: 10.1200/JCO.2008.19.7491. [DOI] [PubMed] [Google Scholar]