Abstract
Objective
Substantial physiological changes occur during pregnancy and lactation, making breast evaluation challenging in these patients. This article reviews the imaging challenges of the breast during pregnancy and lactation. The normal imaging appearance, imaging protocols and the imaging features of each commonly encountered benign and malignant entity with pathological correlation and supporting examples is described. An awareness of the imaging features of the breast during these physiological states and of various benign and malignant diseases that occur permits optimal management.
Conclusions
Evaluation of the pregnant and lactating patients who present with a breast problem is challenging. Although ultrasound may characterise the finding in many cases, mammography and even MRI may have a role in the management of these patients.
Teaching points
• To review physiological changes of the breast during pregnancy and lactation
• To review imaging protocols of the breast during pregnancy and lactation
• Discuss imaging findings with pathological correlation of benign and malignant diseases in pregnancy and lactation
• Discuss pathological correlation of imaging findings in pregnancy and lactation
Keywords: Breast, Disease, Lactating, Pregnancy, Ultrasound, MRI
Background
Pregnancy-associated breast cancer occurs with a frequency of one in 3,000–10,000 pregnancies, accounting for 1–3 % all breast cancers [1]. It is not infrequent for women to present to their physicians with a breast problem during pregnancy or within 1 year of delivery. Changes occurring in the breast during these physiological states make clinical and radiological evaluation of these patients challenging. Improving understanding of varied breast problems and their imaging appearance on multiple modalities is essential to ensure optimal management of these patients.
In the first and second trimester, there is proliferation and differentiation of the lobules, alveoli and lactiferous ducts, the alveolar epithelium becomes secretory. With rising serum prolactin during the third trimester, the milk-producing cells continue to differentiate and colostrum eventually fills the alveoli and milk ducts prior to delivery. These proliferative changes result in bilateral breast enlargement and increased overall density of the breast tissue on imaging. Following delivery, the lactogenic effect of prolactin results in a substantial increase in milk production. All of these physiological changes directly impact the imaging appearance of the breast on mammography, ultrasound and magnetic resonance imaging (MRI) thereby complicating evaluation of pregnant and/or lactating patients, presenting with a breast problem.
Imaging protocols and challenges
Radiological evaluation varies depending upon the age of the woman, her pregnancy and lactational status. Subsequent to a clinical history and thorough physical examination, patients are frequently imaged to determine whether there is an underlying abnormality to account for the patient’s symptoms. For pregnant and lactating women under the age of 30 years, ultrasound is the initial imaging test of choice given the lack of radiation exposure. Mammogram could be considered in these patients if ultrasound is negative or it reveals indeterminate, suspicious or no findings [2]. Lactating women over 30 years of age are typically imaged using both mammography and ultrasound. In an effort to reduce the overall breast density, lactating patients are encouraged to express milk immediately prior to imaging. In a pregnant patient, mammography should be performed, if ultrasound reveals a suspicious finding or if biopsy of a solid lesion reveals malignancy. A complete evaluation of a pregnant patient with a lump should not be delayed until after delivery, because of fear of radiation. Without shielding the abdomen, the dose to the fetus from a four-view mammogram is 0.4 mrad, much less than background, and with shielding, the risk is not significant and safe to the fetus [3]. Fetal malformations are known to occur at a dose exceeding 10 rads [3].
The National Comprehensive Cancer Network guidelines for clinical practice in pregnant patients with breast cancer or suspected to have breast cancer, states that “mammography of the breast with shielding can be safely done” [4, 5].
Normal imaging appearance of the breast in pregnancy and lactation
The imaging appearance on mammography, ultrasound and MRI is variable depending upon the duration of pregnancy and/or lactating state. An overall diffuse increase in breast density accompanied by breast enlargement is commonly seen on mammography (Fig. 1a, b). Given increased density of the breast the sensitivity of mammography is low (30 % for dense breast compared with 80 % for fatty breast), and cancer detection may be somewhat difficult [6]. Murphy et al. [7] evaluated patients with false-negative mammograms and symptomatic cancer, and found that 78 % of the mammographically occult lesions were in women with heterogeneously or extremely dense tissue. The imaging features of breast cancer on the mammogram are identical to those seen in non-pregnant women These are spiculated or irregular masses, pleomorphic linear branching or grouped microcalcifications, focal asymmetries and architectural distortion. Detection is sometimes difficult as the overlying dense tissue may obscure the findings.
Fig. 1.
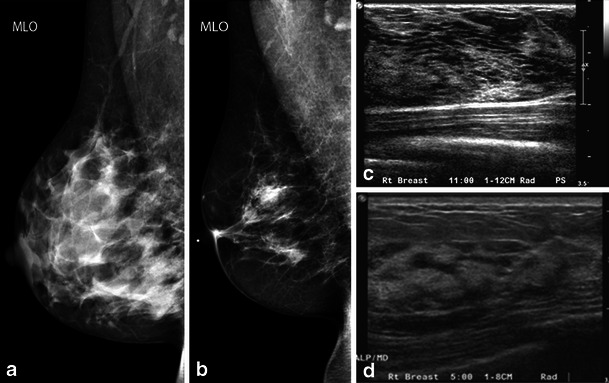
Normal pregnancy and lactational change: a 39-year-old woman, lactating for 3 months. a Note the larger breast size and increased density of parenchyma in spite of pumping prior to imaging on right MLO view compared with b, reduced density of parenchyma on mammogram performed prior to pregnancy. c Pregnancy change: a 38-year-old woman, 24 weeks pregnant presents with breast pain. Note diffuse hypoechogenicity due to enlargement of non-fatty fibroglandular components during pregnancy. d Increased echogenicity with ductal prominence, which is typical appearance of a lactating breast on grey-scale ultrasound
Ultrasound has a better sensitivity in pregnant and lactating patients, ranging from 86.7 to 100 % [8, 9]. On ultrasound, the breast predominantly appears diffusely hypoechoic during pregnancy due to enlargement of the non-fatty fibroglandular component (Fig. 1c), whereas during lactation there is diffuse hyperechogenicity with prominent ducts and vascularity during lactation [1] (Fig. 1d). Typical imaging findings for breast cancer on ultrasound are hypoechoic to isoechoic irregular mass with or without associated posterior shadowing; occasionally there may be posterior acoustic enhancement due to central necrotic components. Colour Doppler helps assess vascularity of the mass lesion.
There is a limited role for breast MRI during pregnancy as intravenous gadolinium crosses the placenta. The routine use of contrast-enhanced MRI in the evaluation of pregnant patients is not appropriate and is recommended only in situations where the risk–benefit ratio is clear [10]. Contrast enhanced MRI can be safely performed in lactating women. Background enhancement on MRI refers to normal enhancement in glandular tissue. The degree of background enhancement can influence sensitivity of MRI [11–13]. Lactating breast tissue has a uniformly long T2, resulting in diffuse high signal intensity on T2-weighted MR images. Normal lactating tissue shows rapid enhancement followed by an early plateau of enhancement, unlike normal non-lactating breast tissue, which shows mild and progressive enhancement [14] (Fig. 2). Breast cancers are visible during lactation owing to their lower signal intensity on T2-weighted images and more intense initial contrast enhancement with early washout compared with normal breast tissue [14] (Fig. 3), though some authors report an overlap of enhancement characteristics of invasive cancer with that of the lactating tissue, attributed to increased vascular permeability [15] (Fig. 4).
Fig. 2.
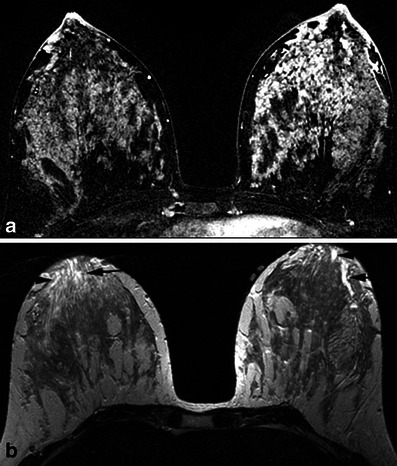
a Normal lactating tissue showing diffuse rapid enhancement on dynamic contrast enhanced MRI. b Note the bright ducts (black arrows) on T2- weighted images
Fig. 3.

a A 44-year-old woman, 10 months postpartum and lactating. Note the irregular spiculated mass (white arrows) showing low signal intensity on T2–weighted images and (b) intense enhancement (white arrows) on dynamic contrast enhanced mages. This was a biopsy proven invasive lobular carcinoma with lymphovascular invasion
Fig. 4.
a A 36-year-old woman, 12 months postpartum and lactating. Note the mass (white arrows) showing high signal intensity on T2–weighted images and (b) increased enhancement (white arrows) on dynamic contrast-enhanced images, compared with the rest of the breast tissue. This was a biopsy-proven grade 3, invasive ductal carcinoma
If breast MR is performed, the ACR practice guidelines recommend that it is safe for the mother to continue breast-feeding after receiving gadolinium. If the mother remains concerned about any potential ill effects, she should be given the opportunity to make an informed decision as to whether to continue or temporarily abstain from breast-feeding after receiving a gadolinium contrast medium. If the mother so desires, she may abstain from breast-feeding for 24 h with active expression and discarding of breast milk from both breasts during that period. In anticipation of this, she may wish to use a breast pump to obtain milk before the contrast study to feed the infant during the 24-h period following the examination [16].
Breast diseases in the pregnant and lactating patient
A wide variety of benign and malignant breast problems may be encountered in these patients. Due to physiological changes, the most commonly encountered problems are lactational change/lobular hyperplasia, lactational adenoma and lactational calcifications.
Benign entities include galactocele, fibroadenoma, obstructed milk duct, mastitis with or without abscess, hyperplastic intramammary and/or axillary lymph nodes, and granulomatous mastitis. Malignant diseases include pregnancy-associated breast cancer and metastatic disease.
Benign entities
Lactational changes/lobular hyperplasia and/or lactational adenoma
Variable ductal and lobular proliferation in the breast tissue during pregnancy results in lactational changes that are detectable on histopathology. When the lactational change presents as a palpable or radiographically visible mass, the benign finding is referred to as a lactational adenoma. It is the most common breast mass during pregnancy [17]. Usually during the third trimester it reduces in size or regresses spontaneously after delivery. It occasionally recurs with subsequent pregnancies. Lactational adenomas can mimic other benign breast tumours such as fibroadenomas, phyllodes tumour and circumscribed malignancies. Although these neoplasms are known to grow due to rising oestrogen levels associated with pregnancy, their aetiology is somewhat ambiguous as some suggest they represent a variant of fibroadenoma, tubular adenoma, lobular hyperplasia or arise de novo. The consensus is they are tubular adenomas with lactational changes [18]. Haemorrhage and infarction occur in approximately 5 % of cases [17]. These tumours commonly lack a capsule, which may explain the absence of a discernible margin. On histopathology, both lactational change and lactational adenoma show lobular expansion with numerous enlarged and dilated acini separated by connective tissue. On ultrasound, lactational change occasionally is visible as a homogeneous to heterogeneous mass (Fig. 5), whereas lactational adenoma most often reveals a homogeneous circumscribed oval mass with posterior acoustic enhancement and gentle lobulations (Fig. 6). In general the features are benign; however, the mass can mimic malignancy, showing irregular margins and posterior shadowing, warranting biopsy [19–21]. Mammography most often shows a circumscribed mass with no associated calcifications. Management varies between conservative follow-up imaging and/or biopsy, based on the imaging appearance. As the coexistence of lactating adenoma and malignancy has been reported [18, 20], close clinical follow-up in 3–6 months, even in a biopsy-proven case, is warranted.
Fig. 5.
Lactational change: a 31-year-old lactating woman, presenting with lump in the right breast. a Grey-scale ultrasound shows a partially circumscribed hypoechoic nodule with cystic areas, (b) with internal vascularity on power Doppler. c Pathology slide at high power (20×) shows lobular expansion containing increased numbers of acini, many of which are enlarged and dilated, consistent with lactational change
Fig. 6.
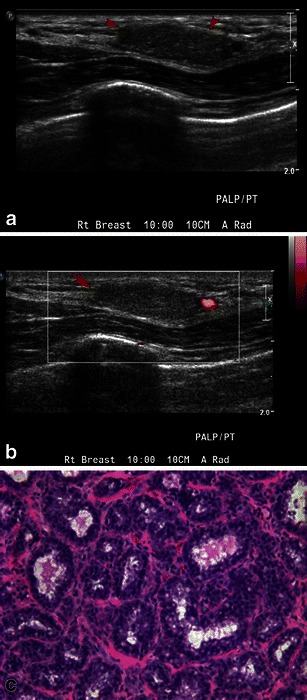
Lactating adenoma: a 38-year-old pregnant woman, presenting with a breast lump. a Grey-scale ultrasound image shows an isoechoic, circumscribed nodule. b Power Doppler image shows minimal peripheral vascularity. Biopsy was performed revealing lactating adenoma. c Higher-power image (20×) shows epithelial cell enlargement, cytoplasmic vacuolisation and a hobnail appearance with protrusion of cells into the acinar lumen
Lactational calcifications
Benign calcifications are sometimes seen in lactating patients undergoing imaging for a breast problem or for screening. In general, calcifications are not a common mammographic feature of lactational or post-lactational breast. On mammography, these are usually diffuse or regional, predominantly punctate calcifications, and could be bilateral or unilateral (Fig. 7). Rarely, the calcifications may be grouped, and in those cases, stereotactic biopsy may be indicated to exclude malignancy (Fig. 7). In a series of case reports, all cases had bilateral and diffuse distribution with focal groups, of which some had a linear branching pattern, some had a casting pattern [22] and some diffuse with regional distribution [23]. On histology, the calcifications are seen in both ducts and lobules. The small rounded microcalcifications in the lobular acini likely reflect the granular pattern as seen as focal groups, whereas larger calcifications in dilated ducts correspond to the casting pattern on mammography[22]. These are possibly related to milk stasis or apoptosis associated with lactation [24, 25].
Fig. 7.
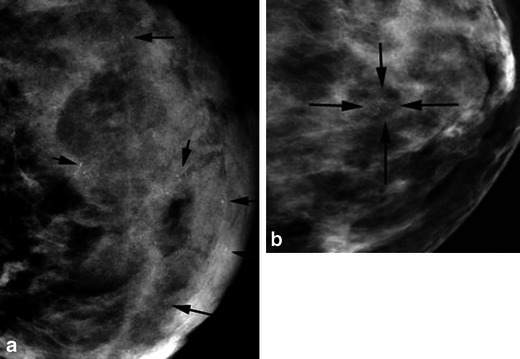
Lactational calcifications. a A 39-year-old lactating woman with an area of palpable concern in the right breast. A mammogram of the left breast, MLO view, shows incidental new diffuse microcalcifications (black arrows). Similar findings were also appreciated in the opposite breast. All of these calcifications represent lactational deposits. b A 38-year-old lactating woman presented with a right breast lump; incidental focal microcalcifications (black arrows) were seen in the left breast at 12:00, magnification view in CC and ML view (not shown here) showed a focal cluster of slightly pleomorphic calcifications. Stereotactic biopsy was performed, which revealed lactational calcifications
Enlargement of axillary breast tissue
The embryonic mammary ridge (milk line) extends from the axilla to the groin. Incomplete regression of this ridge during embryological formation gives rise to ectopic breast tissue.
Accessory breast tissue occurs in up to 0.2–6 % of the general population [26]. Ectopic breast tissue is subject to the same hormonal influences and risk of disease as eutopic breast tissue. During menses or pregnancy, hormonal stimulation can cause engorgement and discomfort. As a consequence, these patients typically complain of fullness and discomfort in this area. Ectopic breast tissue can undergo lactational change during pregnancy, and in the presence of a nipple-areolar complex it can give rise to lactation [26]. The axilla is the most common site in which accessory breast tissue can be found [27]. On mammography, ultrasound and MRI, accessory breast tissue has the imaging appearance of normal breast tissue. Primary carcinoma of ectopic breast tissue has been reported only in a small number of cases [27].
Obstructed milk duct
Patients typically present with a tender pea-size to wedge-shaped lump [28], which is related to mechanical obstruction secondary to a change in infant feeding pattern, or scarring from previous surgery, or infection [29]. This may be in the retroareolar region but can occur in any location in the breast. On ultrasound, the imaging appearance is variable, ranging from a discrete non-compressible mass or duct (Fig. 8) to a diffuse echogenic area with a hypoechoic rim. For recurrent blocked ducts, an obstructive lesion should be excluded. Ultrasound-guided aspiration is rarely performed as this is typically managed with warm compresses, massage and frequent milk expression. Direct aspiration could be performed for symptom relief and diagnosis. If symptoms do not resolve this may progress to mastitis [30].
Fig. 8.
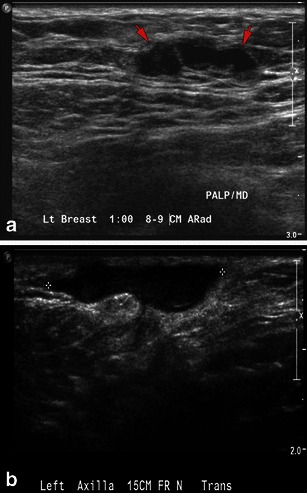
Blocked milk duct: a 35-year-old lactating woman with fluctuant non-tender breast mass. a Grey-scale ultrasound image reveals linear hypoechoic structure with no vascularity on power Doppler (not shown here). Findings were consistent with a blocked milk duct. b A 27-year-old lactating woman, presenting with tender mass in left axilla. Grey-scale ultrasound reveals a hypoechoic tubular lesion with no vascularity on power Doppler (not shown here). This was aspirated, for symptomatic relief to the patient, yielding milky fluid
Mastitis
WHO defines mastitis as an inflammatory condition of the breast which may or may not be accompanied by infection. It is most commonly seen during lactation with a reported incidence of 6.6–33 % [31]. Although various aetiologies likely exist (milk stasis, blocked ducts, engorgement or physical injury to the breast), one more common theory is that poor attachment of the infant to the breast leads to cracking of the nipple epithelium, creating a retrograde path for bacteria to enter the breast tissue [32]. Milk stasis provides a medium for bacterial growth. The most common causative organism of lactation-related mastitis and abscess is Staphylococcus aureus. Patients can present with breast pain, redness, and swelling and may have flu-like symptoms. Imaging on ultrasound may reveal skin thickening, areas of decreased parenchymal echogenecity or increased fat echogenecity, increased vascularity on colour Doppler and reactive or enlarged axillary nodes [33] (Fig. 9a). Because the organism is usually β-lactamase producing, penicillinase-resistant antibiotics should be used [33]. Treatment typically entails antibiotics and frequent breast feeding or breast emptying to limit milk stasis. Treating mastitis promptly prevents abscess formation. If the patient’s symptoms do not resolve within 2 weeks or are recurrent, mammography may be indicated to exclude an underlying malignancy.
Fig. 9.
a Mastitis: a 29-year-old lactating woman, presenting with breast pain and erythema. Ultrasound reveals skin thickening and no discrete abscess consistent with mastitis. Patient’s redness and pain resolved after treatment with antibiotics. b Breast abscess: a 39-year-old lactating woman with left breast erythema swelling and fever. Grey-scale ultrasound shows a multiloculated fluid collection with debris representing abscess. Aspiration yielded pus, and microbiology revealed MRSA
Breast abscess
Acute bacterial mastitis will either resolve with antibiotic therapy or evolve into an abscess if treatment is delayed or inadequate. Approximately 4.8–11 % of lactation-related mastitis is complicated by breast abscesses [33]. Infection is most commonly due to S. aureus (with increasing cases of methicillin-resistant S. aureus MRSA) and Streptococcus. The patient presents with fever, chills, tenderness and breast erythema. Imaging with ultrasound can confirm the diagnosis, provide a means to drain the collection to tailor antibiotic therapy and can be safely used for regular follow-up of abscess. Ultrasound is the modality of choice and typically reveals a complex hypoechoic cystic mass of varied shape, commonly multiloculated with indistinct margins, peripheral vascularity and posterior acoustic enhancement (Fig. 9b); however, there should be no vascularity within the fluid collection [34]. Mammography is performed only if unclear of diagnosis and may show signs such as mass, distortion, asymmetric density and skin thickening, which are not specific to cancer. Presence of suspicious calcifications is more specific for cancer [35]. Percutaneous drainage combined with antibiotic therapy provides effective treatment. In some cases multiples drainages are required [35–37]. Warm compresses and frequent breast feeding also help to shorten the duration of symptoms. The presence of mastitis and/or abscess poses no risk to the breast feeding infant. Cessation of breast-feeding is necessary only when treatment with an antibiotic contraindicated for the newborn is prescribed (e.g. tetracycline, ciprofloxacin or chloramphenicol) or if surgical drainage is performed [35]. Due to overlap of radiological findings in infection and inflammatory breast cancer, if there is clinical suspicion, strong family history or atypical course breast biopsy or skin punch biopsy should be considered.
Galactocele
It is the most common benign breast lesion in lactating women and can present in the third trimester, after delivery, or even after cessation of breast feeding. Galactoceles typically occur as a result of an obstructed duct leading to distension of proximal lobular segments. Patients most often present with a tender mass. The imaging appearance of galactocele is variable, depending on the amount of fat, protein and water content [38]. On mammography, a mass with a fat-fluid level on the lateral projection is a diagnostic sign in the appropriate clinical setting. (Fig. 10a), The presence of solid, mobile echogenic contents with distal acoustic shadowing in a fluid-filled cavity on ultrasound, is considered to be highly suggestive of a galactocele [39]. On ultrasound, most lesions appear benign with thin, well-circumscribed margins; the internal appearance may be homogeneous with low level echoes or heterogeneous, depending on its contents. It may appear multicystic or have a complex echotexture (Fig. 10b, c). The margins vary from well-defined to ill-defined, depending upon the amount of surrounding inflammation. Histopathology reveals cuboidal and flat epithelial-lined cysts often accompanied by inflammatory and/or necrotic debris (Fig. 10d). If asymptomatic, or if typical with a fat-fluid level, galactoceles can be managed conservatively.
Fig. 10.
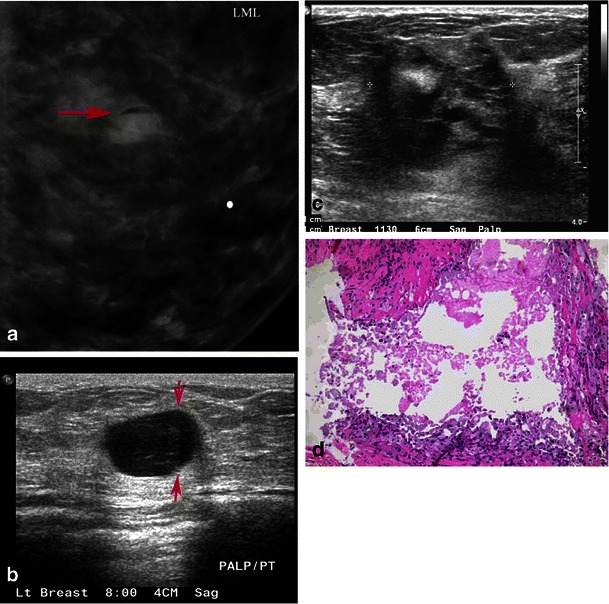
Galactocele: a 35-year-old lactating woman, presenting with a palpable lump. a Photographic magnification of left lateral mammogram shows a well-circumscribed lesion with a fat fluid level on the lateral projection. This is the classic appearance of galactocele. b Grey-scale ultrasound shows a cystic lesion which, on adjusting the gain, shows a fat/fluid level diagnostic of galactocele. c Another patient, a 38-year-old lactating woman, presenting with breast pain and palpable mass. Mammogram showed dense breast tissue with a partially obscured mass and skin thickening (not shown here). Grey-scale ultrasound image shows heterogeneous ill-defined mass, which was vascular on power Doppler. Biopsy was performed. d Microscopic high-power image (40×), revealing a ruptured galactocele with cyst contents leaking into the surrounding tissue, causing a lipogranulomatous inflammation and foamy histiocyte aggregation
Fibroadenoma
It is the most common benign breast tumour in young women. Women typically present with a firm mobile mass. These tumours are hormone sensitive; hence they often enlarge during pregnancy and/or lactation in response to elevated circulating hormones. If during pregnancy the fibroadenoma outgrows its blood supply, it may undergo infarction, in which case patients may present with a painful mass. On mammography, fibroadenomas appear well circumscribed, have a round or oval shape and may be smoothly lobulated (Fig. 11). Coarse popcorn-like calcifications may be seen if the tumour underwent infarction; otherwise, calcifications are quite rare as patients tend to be young in age. On ultrasound, the typical features of a fibroadenomas is round or oval shape, may show homogeneous internal echoes, well-circumscribed margins, pseudo-capsule, absence of posterior acoustic shadowing and normal adjacent breast tissue [40]. However, during pregnancy, the appearance can be somewhat atypical with cystic changes, increased vascularity and/or prominent ducts. The presence of atypical features such as microlobulations, irregular margins, heterogeneous echotexture, posterior acoustic shadowing and extensive hypoechogenicity, should lead to percutaneous core biopsy to confirm the diagnosis.
Fig. 11.

Fibroadenoma: a 22-year-old pregnant woman, presenting with a lump. a Grey-scale ultrasound shows a partially circumscribed macrolobulated nodule without internal vascularity. Core-needle biopsy was performed. b Microscopic low power (10×) reveals a fibroadenoma, illustrating benign proliferation of glands and stroma
Enlarged intramammary and/or axillary lymph nodes
Benign lymph nodes are usually bilateral multiple, have a lucent centre and a hilar notch [41]. Benign aetiologies include regional inflammatory process, infectious diseases, rheumatoid arthritis and malignant aetiologies include metastatic breast cancer and lymphoma [41]. During lactation, enlarged intramammary and/or axillary lymph nodes may be seen. The hyperplastic nodes are felt to be related to the bacterial seeding of the nipple by the infant during breast feeding. These nodes are typically seen in the upper outer quadrant of the breast and axilla. On mammography, normal nodes appear oval or bean-shaped with circumscribed sometimes lobulated margins and a radiolucent notch and abnormal nodes are dense [42]. When the lymph nodes are more than 33 mm, have ill-defined or spiculated margins, or contain intranodal microcalcifications they are strongly associated with malignancy [42]. On ultrasound, benign nodes demonstrate a hypoechoic rim with an echogenic hilum. Typically, hyperplastic nodes commonly demonstrate concentric cortical thickening, whereas asymmetric focal hypoechoic cortical lobulations or a completely hypoechoic node with loss of fatty hilum raises suspicion of malignancy and a fine-needle aspiration/core biopsy is recommended [43] (Fig. 12).
Fig. 12.
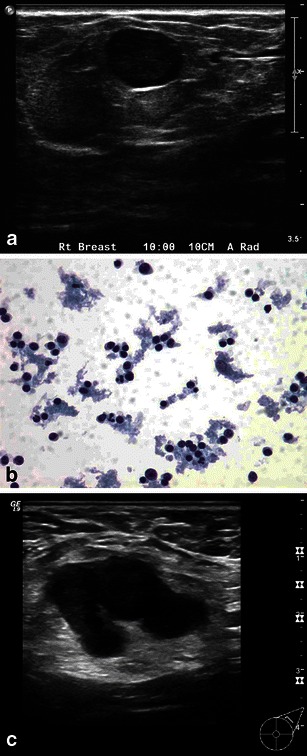
a Benign reactive lymph node: a 30-year-old pregnant woman, presenting with a palpable lump. Grey-scale ultrasound image shows well circumscribed hypoechoic nodule, with significant vascularity on power Doppler. b Fine-needle aspiration cytology reveals polymorphous population of lymphocytes and macrophages, all features of benign reactive lymph node. c Metastatic lymph node: a 39-year-old woman, 12 weeks pregnant, presenting with palpable axillary mass. The patient had a remote history of breast cancer treated with mastectomy. Gray-scale ultrasound showed an enlarged axillary node with abnormally thickened cortex. Core biopsy revealed metastatic breast cancer
Granulomatous mastitis
Granulomatous mastitis is a rare inflammatory disease of unknown aetiology that often mimics malignancy. It typically affects young women usually within 6 years of pregnancy. Patients may present with a distinct, firm, painful mass that tends to spare the subareolar regions [1]. Axillary lymphadenopathy and, rarely, sinus tracts may be encountered. Inflammatory factors are suggested as possible causes, although a recent study isolated Corynebacterium in 75 % of cases [44, 45]. Diagnosis is based on exclusion. Histology usually reveals non-caseating, granulomatous inflammatory reaction and diagnoses such as tuberculosis, other fungal infections, sarcoidosis, Wegener’s granulomatosis and granulomatous reactions found in association with carcinomas must be excluded. The imaging appearance can be variable and at times mimic malignancy. On mammography no abnormality may be detected or non-specific imaging findings such as a benign-appearing solitary or multiples mass, architectural distortion, focal asymmetry, spiculated mass and skin thickening may be seen. Dursun et al. [46] reported no calcifications in the 36 patients from their study. On ultrasound, solitary or multiple circumscribed heterogeneous hypoechoic masses with tubular configuration, diffuse abscess and fistula formation may be seen (Fig. 13). MRI is non-specific and may reveal enhancing mass or non-mass-like enhancement, though one study showed rim enhancement, and benign time–signal intensity curve in 22 of 34 patients [46]. Management is challenging, but usually entails a combination of steroids and wide surgical excision, particularly for resistant or recurrent disease [12]. Recurrence is not uncommon.
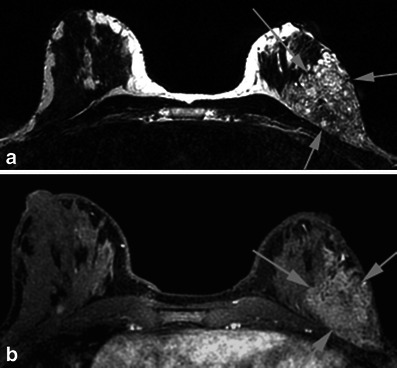
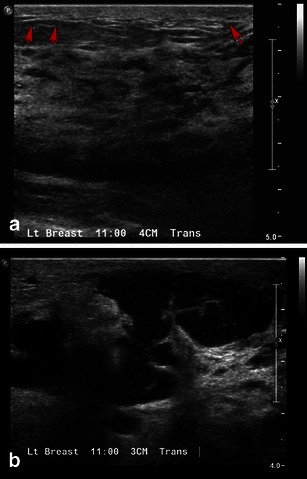
Fig. 13.
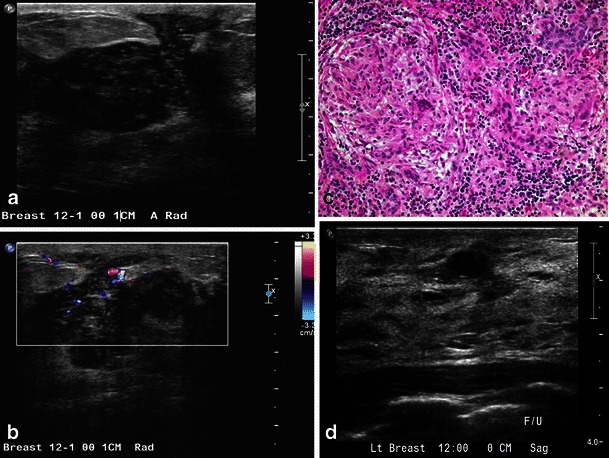
Granulomatous mastitis: a 30-year-old woman, postpartum, presenting with erythema, skin thickening and draining sinus. Grey-scale ultrasound image (a, b) showed irregular hypoechoic mass with peripheral vascularity. Biopsy was performed; high power image (40×) (c) showed non-necrotising granulomas, lymphocytes and plasma cells in the background. Special stains for fungus and mycobacterium were negative. Follow-up after conservative treatment and steroids were done. The follow-up ultrasound image (d) revealed significant improvement. Findings were consistent with granulomatous mastitis
Malignant entities
Pregnancy-Associated Breast Cancer (PABC)
Breast cancer diagnosed during pregnancy or within the first year after delivery is referred to as pregnancy-associated breast cancer. It accounts for 1–2 % of all newly diagnosed breast cancers each year and affects one out of every 3,000 live births. Typically presenting as a painless palpable lump, diagnosis is often delayed as physical examination of the pregnant and lactating breast is challenging. Overall, PABC is biologically aggressive with the majority of these tumours being oestrogen and progesterone receptor negative and Her2-neu receptor positive. The biological nature of these tumours consequently bodes a poorer prognosis. During pregnancy, ultrasound remains the optimal tool for imaging. However, if a suspicious finding is seen on the ultrasound in a pregnant patient, mammography should be performed. Imaging findings on both mammography and ultrasound of PABC is identical to cancer presenting in a non-pregnant or non-lactating woman. Ultrasound may reveal a circumscribed to spiculated hypoechoic to complex mass with irregular shape, posterior shadowing and non-parallel orientation (Fig. 14). Though cancers usually show posterior acoustic shadowing, in one study of 22 cases, posterior acoustic enhancement was seen in 12 of the 22 patients, likely reflecting the necrotic/cystic degeneration seen in these aggressive tumours [8]. Other associated findings include thickening of the Cooper’s ligaments, oedema, skin thickening and axillary lymphadenopathy. Mammography permits evaluation of microcalcifications, multifocality and multicentricity. Typically, a mass with or without associated pleomorphic calcifications is seen (Fig. 14). Secondary findings might include architectural distortion, nipple or skin retraction and lymphadenopathy. MRI is not typically done in pregnant patients, but can be safely performed in lactating patients. MRI is done for staging and to evaluate extent of disease. MRI may reveal a circumscribed to irregular mass with type II or type III enhancement kinetics. Other findings include non-mass-like enhancement and ductal enhancement [10].
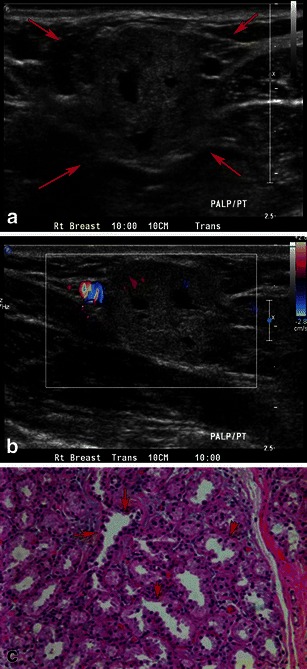
Fig. 14.
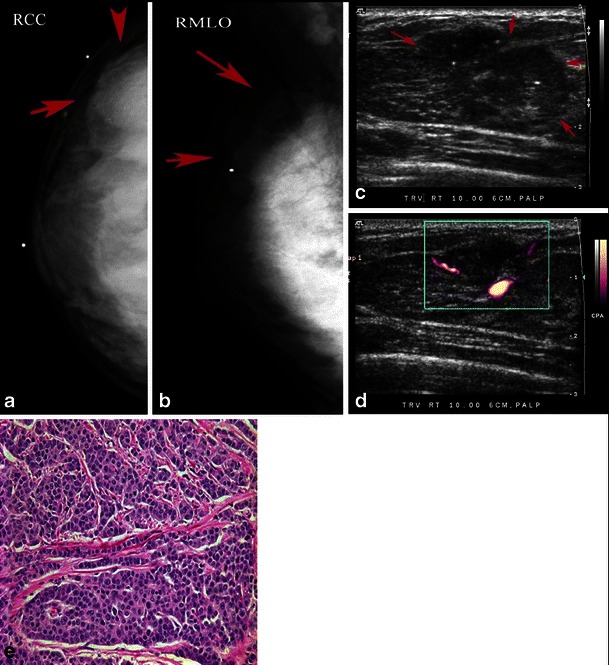
Pregnancy-associated breast cancer: a 36-year-old woman, 19 weeks pregnant, presenting with a palpable lump. Mammogram (a, b) reveals a dense partially circumscribed mass in the upper outer quadrant with associated microcalcifications. c Grey-scale ultrasound shows a hypoechoic ill-defined mass with hyperechoic foci of microcalcifications. d Power Doppler shows internal vascularity. e Microscopic high-power image (40×) shows grade 3 invasive ductal carcinoma with lack of tubule formation, pleomorphic nuclei and abundant mitotic figures
Metastatic disease
With a reported incidence of 1.7–6.6 %, metastasis to the breast most commonly occurs from the contralateral breast cancer, lymphoma/leukaemia, melanoma and lung carcinoma. Though, any tumour can metastasise to the breast, non-mammary metastatic lesions are rare. Imaging entails targeted ultrasound and diagnostic mammography. Most metastases appear as well-circumscribed masses which lack calcifications, although psammomatous calcifications may be seen if the primary is of ovarian or thyroid origin. Metastatic lesions are more likely multiple and bilateral and are often found in the subcutaneous fat, whereas primary breast cancers develop in glandular tissue. Percutaneous core biopsy permits diagnosis when clinically needed to guide management.
Conclusion
Substantial physiological changes during pregnancy and lactation make it challenging to evaluate patients presenting with a breast problem. Most findings in pregnant and lactating patients are benign. Ultrasound is the first-line imaging modality for all pregnant women and for lactating women less than 30 years of age. Mammography is indicated in lactating women over 30 years of age and in pregnant women with suspicious findings on the initial ultrasound or with a biopsy diagnosis of breast cancer. An awareness of the imaging features of the various benign and malignant diseases during these physiological states, permits optimal management.
References
- 1.Sabate JM, Clotet M, Torrubia S, et al. Radiologic evaluation of breast disorders related to pregnancy and lactation. Radiographics. 2007;27(Suppl 1):S101–S124. doi: 10.1148/rg.27si075505. [DOI] [PubMed] [Google Scholar]
- 2.Robbins J, Jeffries D, Roubidoux M, Helvie M (2011) Accuracy of diagnostic mammography and breast ultrasound during pregnancy and lactation. AJR Am J Roentgenol 196:716–722 [DOI] [PubMed]
- 3.Magno S, Terribile D, Franceschini G, et al. Early onset lactating adenoma and the role of breast MRI: a case report. J Med Case Rep. 2009;3:43. doi: 10.1186/1752-1947-3-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Comprehensive Cancer Network (2008) Clinical practice guidelines in oncology: breast cancer. In: National comprehensive cancer network, Vol. 2. NCCN, Fort Washington
- 5.National Comprehensive Cancer Network(2008) Clinical practice guidelines in oncology: breast cancer screening and diagnosis guidelines. In: National comprehensive cancer network, Vol. 1. NCCN, Fort Washington [DOI] [PubMed]
- 6.Mandelson MT, Oestreicher N, Porter PL, et al. Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst. 2000;92:1081–1087. doi: 10.1093/jnci/92.13.1081. [DOI] [PubMed] [Google Scholar]
- 7.Murphy IG, Dillon MF, Doherty AO, et al. Analysis of patients with false negative mammography and symptomatic breast carcinoma. J Surg Oncol. 2007;96:457–463. doi: 10.1002/jso.20801. [DOI] [PubMed] [Google Scholar]
- 8.Ahn BY, Kim HH, Moon WK, et al. Pregnancy- and lactation-associated breast cancer: mammographic and sonographic findings. J Ultrasound Med. 2003;22:491–497. doi: 10.7863/jum.2003.22.5.491. [DOI] [PubMed] [Google Scholar]
- 9.Liberman L, Giess CS, Dershaw DD, Deutch BM, Petrek JA. Imaging of pregnancy-associated breast cancer. Radiology. 1994;191:245–248. doi: 10.1148/radiology.191.1.8134581. [DOI] [PubMed] [Google Scholar]
- 10.Ayyappan AP, Kulkarni S, Crystal P. Pregnancy-associated breast cancer: spectrum of imaging appearances. Br J Radiol. 2010;83:529–534. doi: 10.1259/bjr/17982822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuhl C. The current status of breast MR imaging. Part I. Choice of technique, image interpretation, diagnostic accuracy, and transfer to clinical practice. Radiology. 2007;244:356–378. doi: 10.1148/radiol.2442051620. [DOI] [PubMed] [Google Scholar]
- 12.Ocal K, Dag A, Turkmenoglu O, Kara T, Seyit H, Konca K. Granulomatous mastitis: clinical, pathological features, and management. Breast J. 2010;16:176–182. doi: 10.1111/j.1524-4741.2009.00879.x. [DOI] [PubMed] [Google Scholar]
- 13.Cubuk R, Tasali N, Narin B, Keskiner F, Celik L, Guney S. Correlation between breast density in mammography and background enhancement in MR mammography. Radiol Med. 2010;115:434–441. doi: 10.1007/s11547-010-0513-4. [DOI] [PubMed] [Google Scholar]
- 14.Espinosa LA, Daniel BL, Vidarsson L, Zakhour M, Ikeda DM, Herfkens RJ. The lactating breast: contrast-enhanced MR imaging of normal tissue and cancer. Radiology. 2005;237:429–436. doi: 10.1148/radiol.2372040837. [DOI] [PubMed] [Google Scholar]
- 15.Talele AC, Slanetz PJ, Edmister WB, Yeh ED, Kopans DB. The lactating breast: MRI findings and literature review. Breast J. 2003;9:237–240. doi: 10.1046/j.1524-4741.2003.09322.x. [DOI] [PubMed] [Google Scholar]
- 16.American College of Radiology (2012) 79/ Administration of contrast media to breast-feeding mothers. In: ACR manual on contrast media—version 8. ACR, Reston
- 17.Baker TP, Lenert JT, Parker J, et al. Lactating adenoma: a diagnosis of exclusion. Breast J. 2001;7:354–357. doi: 10.1046/j.1524-4741.2001.20075.x. [DOI] [PubMed] [Google Scholar]
- 18.Saglam A, Can B. Coexistence of lactating adenoma and invasive ductal adenocarcinoma of the breast in a pregnant woman. J Clin Pathol. 2005;58:87–89. doi: 10.1136/jcp.2004.018275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sumkin JH, Perrone AM, Harris KM, Nath ME, Amortegui AJ, Weinstein BJ. Lactating adenoma: US features and literature review. Radiology. 1998;206:271–274. doi: 10.1148/radiology.206.1.9423682. [DOI] [PubMed] [Google Scholar]
- 20.Hertel BF, Zaloudek C, Kempson RL. Breast adenomas. Cancer. 1976;37:2891–2905. doi: 10.1002/1097-0142(197606)37:6<2891::AID-CNCR2820370647>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 21.Adeniran A, Al-Ahmadie H, Mahoney MC, Robinson-Smith TM. Granular cell tumor of the breast: a series of 17 cases and review of the literature. Breast J. 2004;10:528–531. doi: 10.1111/j.1075-122X.2004.21525.x. [DOI] [PubMed] [Google Scholar]
- 22.Mercado CL, Koenigsberg TC, Hamele-Bena D, Smith SJ. Calcifications associated with lactational changes of the breast: mammographic findings with histologic correlation. AJR Am J Roentgenol. 2002;179:685–689. doi: 10.2214/ajr.179.3.1790685. [DOI] [PubMed] [Google Scholar]
- 23.Stucker DT, Ikeda DM, Hartman AR, et al. New bilateral microcalcifications at mammography in a postlactational woman: case report. Radiology. 2000;217:247–250. doi: 10.1148/radiology.217.1.r00oc19247. [DOI] [PubMed] [Google Scholar]
- 24.Quarrie LH, Addey CV, Wilde CJ. Programmed cell death during mammary tissue involution induced by weaning, litter removal, and milk stasis. J Cell Physiol. 1996;168:559–569. doi: 10.1002/(SICI)1097-4652(199609)168:3<559::AID-JCP8>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 25.Marti A, Feng Z, Altermatt HJ, Jaggi R. Milk accumulation triggers apoptosis of mammary epithelial cells. Eur J Cell Biol. 1997;73:158–165. [PubMed] [Google Scholar]
- 26.Sanguinetti A, Ragusa M, Calzolari F, et al. Invasive ductal carcinoma arising in ectopic breast tissue of the axilla. Case report and review of the literature. G Chir. 2010;31:383–386. [PubMed] [Google Scholar]
- 27.Gutermuth J, Audring H, Voit C, Haas N. Primary carcinoma of ectopic axillary breast tissue. J Eur Acad Dermatol Venereol. 2006;20:217–221. doi: 10.1111/j.1468-3083.2005.01362.x. [DOI] [PubMed] [Google Scholar]
- 28.Geddes DT. Ultrasound imaging of the lactating breast: methodology and application. Int Breastfeed J. 2009;4:4. doi: 10.1186/1746-4358-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eglash A, Plane MB, Mundt M. History, physical and laboratory findings, and clinical outcomes of lactating women treated with antibiotics for chronic breast and/or nipple pain. J Hum Lact. 2006;22:429–433. doi: 10.1177/0890334406293431. [DOI] [PubMed] [Google Scholar]
- 30.Ferris-James DM, Iuanow E, Mehta TS, Shaheen RM, Slanetz PJ. Imaging approaches to diagnosis and management of common ductal abnormalities. Radiographics. 2012;32:1009–1030. doi: 10.1148/rg.324115150. [DOI] [PubMed] [Google Scholar]
- 31.Kvist LJ, Larsson BW, Hall-Lord ML, Steen A, Schalen C. The role of bacteria in lactational mastitis and some considerations of the use of antibiotic treatment. Int Breastfeed J. 2008;3:6. doi: 10.1186/1746-4358-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crepinsek MA, Crowe L, Michener K, Smart NA. Interventions for preventing mastitis after childbirth. Cochrane Database Syst Rev (Online) 2012;10:CD007239. doi: 10.1002/14651858.CD007239.pub3. [DOI] [PubMed] [Google Scholar]
- 33.Ulitzsch D, Nyman MK, Carlson RA. Breast abscess in lactating women: US-guided treatment. Radiology. 2004;232:904–909. doi: 10.1148/radiol.2323030582. [DOI] [PubMed] [Google Scholar]
- 34.Karstrup S, Solvig J, Nolsoe CP, et al. Acute puerperal breast abscesses: US-guided drainage. Radiology. 1993;188:807–809. doi: 10.1148/radiology.188.3.8351352. [DOI] [PubMed] [Google Scholar]
- 35.Trop I, Dugas A, David J, et al. Breast abscesses: evidence-based algorithms for diagnosis, management, and follow-up. Radiographics. 2011;31:1683–1699. doi: 10.1148/rg.316115521. [DOI] [PubMed] [Google Scholar]
- 36.Christensen AF, Al-Suliman N, Nielsen KR, et al. Ultrasound-guided drainage of breast abscesses: results in 151 patients. Br J Radiol. 2005;78:186–188. doi: 10.1259/bjr/26372381. [DOI] [PubMed] [Google Scholar]
- 37.Eryilmaz R, Sahin M, Hakan Tekelioglu M, Daldal E. Management of lactational breast abscesses. Breast. 2005;14:375–379. doi: 10.1016/j.breast.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 38.Sawhney S, Petkovska L, Ramadan S, Al-Muhtaseb S, Jain R, Sheikh M. Sonographic appearances of galactoceles. J Clin Ultrasound. 2002;30:18–22. doi: 10.1002/jcu.10038. [DOI] [PubMed] [Google Scholar]
- 39.Salvador R, Salvador M, Jimenez JA, Martinez M, Casas L. Galactocele of the breast: radiologic and ultrasonographic findings. Br J Radiol. 1990;63:140–142. doi: 10.1259/0007-1285-63-746-140. [DOI] [PubMed] [Google Scholar]
- 40.Skaane P, Engedal K. Analysis of sonographic features in the differentiation of fibroadenoma and invasive ductal carcinoma. AJR Am J Roentgenol. 1998;170:109–114. doi: 10.2214/ajr.170.1.9423610. [DOI] [PubMed] [Google Scholar]
- 41.Lee CH, Giurescu ME, Philpotts LE, Horvath LJ, Tocino I. Clinical importance of unilaterally enlarging lymph nodes on otherwise normal mammograms. Radiology. 1997;203:329–334. doi: 10.1148/radiology.203.2.9114083. [DOI] [PubMed] [Google Scholar]
- 42.Walsh R, Kornguth PJ, Soo MS, Bentley R, DeLong DM. Axillary lymph nodes: mammographic, pathologic, and clinical correlation. AJR Am J Roentgenol. 1997;168:33–38. doi: 10.2214/ajr.168.1.8976915. [DOI] [PubMed] [Google Scholar]
- 43.Bedi DG, Krishnamurthy R, Krishnamurthy S, et al. Cortical morphologic features of axillary lymph nodes as a predictor of metastasis in breast cancer: in vitro sonographic study. AJR Am J Roentgenol. 2008;191:646–652. doi: 10.2214/AJR.07.2460. [DOI] [PubMed] [Google Scholar]
- 44.Going JJ, Anderson TJ, Wilkinson S, Chetty U. Granulomatous lobular mastitis. J Clin Pathol. 1987;40:535–540. doi: 10.1136/jcp.40.5.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paviour S, Musaad S, Roberts S, et al. Corynebacterium species isolated from patients with mastitis. Clin Infect Dis. 2002;35:1434–1440. doi: 10.1086/344463. [DOI] [PubMed] [Google Scholar]
- 46.Dursun M, Yilmaz S, Yahyayev A, et al. Multimodality imaging features of idiopathic granulomatous mastitis: outcome of 12 years of experience. Radiol Med. 2012;117:529–538. doi: 10.1007/s11547-011-0733-2. [DOI] [PubMed] [Google Scholar]


