Abstract
OBJECTIVE
To investigate whether diabetes affects perioperative complications or mortality and to gauge its impact on medical expenditures for noncardiac surgeries.
RESEARCH DESIGN AND METHODS
With the use of reimbursement claims from the Taiwan National Health Insurance system, we performed a population-based cohort study of patients with and without diabetes undergoing noncardiac surgeries. Outcomes of postoperative complications, mortality, hospital stay, and medical expenditures were compared between patients with and without diabetes.
RESULTS
Diabetes increased 30-day postoperative mortality (odds ratio 1.84 [95% CI 1.46–2.32]), particularly among patients with type 1 diabetes or uncontrolled diabetes and patients with preoperative diabetes-related comorbidities, such as eye involvement, peripheral circulatory disorders, ketoacidosis, renal manifestations, and coma. Compared with nondiabetic control patients, coexisting medical conditions, such as renal dialysis (5.17 [3.68–7.28]), liver cirrhosis (3.59 [2.19–5.88]), stroke (2.87 [1.95–4.22]), mental disorders (2.35 [1.71–3.24]), ischemic heart disease (2.08 [1.45–2.99]), chronic obstructive pulmonary disease (1.96 [1.29–2.97]), and hyperlipidemia (1.94 [1.01–3.76]) were associated with mortality for patients with diabetes undergoing noncardiac surgery. Patients with diabetes faced a higher risk of postoperative acute renal failure (3.59 [2.88–4.48]) and acute myocardial infarction (3.65 [2.43–5.49]). Furthermore, diabetes was associated with prolonged hospital stay (2.30 [2.16–2.44]) and increased medical expenditures (1.32 [1.25–1.40]).
CONCLUSIONS
Diabetes increases postoperative 30-day mortality, complications, and medical expenditures in patients undergoing in-hospital noncardiac surgeries.
Diabetes is a common chronic disease that causes widespread disability and death, with a global prevalence of 2.8% in 2000 and an estimated prevalence of 4.4% in 2030 (1). In the U.S., the national burden of diabetes was estimated to be $245 billion in 2012 (2). The epidemiology, pathogenesis, prevention, and treatment of diabetes have been well established over the past 2 centuries (3).
Diabetes is an independent determinant of increased risk of perioperative complications and mortality in cardiovascular surgeries (4,5), yet how extensively diabetes affects postoperative mortality and complications in noncardiac surgeries has not been determined. Some studies indicated that survival outcomes and perioperative complications in noncardiac surgeries do not differ between patients with and without diabetes (6,7), whereas other research showed conflicting data about whether diabetes increased perioperative complications, mortality, hospital stay, and health care expenditures (8–16).
Previous studies were limited by several factors, including a focus on a single type of noncardiac surgery (6,8,10,12,14), small sample size (6,7,9,13), inappropriate selection of nondiabetes control subjects (6–16), inadequate adjustment for potential confounders (7,9–12,15), and reporting of a single outcome after surgery (10,16). It remains unclear whether coexisting medical conditions, types of diabetes, glycemic control, and diabetes-related comorbidities affect postoperative outcomes in patients with diabetes.
This study used Taiwan National Health Insurance Program reimbursement claims to investigate postoperative complications, 30-day mortality, length of hospital stay, and medical expenditures after adjustment by propensity score-matched pair method in patients with diabetes undergoing noncardiac surgeries. We also investigated the impact of coexisting medical conditions and diabetes-related comorbidities on postoperative 30-day mortality among patients with diabetes.
RESEARCH DESIGN AND METHODS
Data sources
Research data were obtained from reimbursement claims of the Taiwan National Health Insurance Program, which was implemented in March 1995 and covers >99% of the 22.6 million Taiwan residents. The National Health Research Institutes established the National Health Insurance Research Database that records all beneficiaries’ medical services, including inpatient and outpatient demographics, primary and secondary diagnoses, procedures, prescriptions, and medical expenditures, for public research interest. The validity of this database has been favorably evaluated, and research articles based on it have been accepted in prominent scientific journals worldwide (8,17–20).
Ethical approval
Insurance reimbursement claims from the National Health Insurance Research Database are available for public access. To protect personal privacy, the electronic database with patient identifications was decoded and scrambled for further research access. Although informed consent was not required because of this privacy protection, the study was evaluated and approved by the National Health Research Institutes (8,17–20).
Study population
We examined medical claims and identified 14,855 patients ≥20 years of age with preoperative diabetes from 1,499,745 patients who underwent major inpatient noncardiac surgeries between 2008 and 2010 in Taiwan. These surgeries required general, epidural, or spinal anesthesia and hospitalization for >1 day. Previous studies (8,17,19,20) considered patients with diabetes as those who had made two visits for outpatient care for diabetes. To identify patients with diabetes more strictly and avoid those with minor or borderline diabetes, the present study required at least one hospital admission (attributable to diabetes or related complications) and one visit for outpatient medical services for a principal diagnosis of diabetes within the 24-month preoperative period. We matched each surgical patient with diabetes with a randomly selected surgical patient without diabetes by sex, age, type of noncardiac surgery, type of anesthesia, coexisting medical conditions, operation in teaching hospital or not, and low income or not and conducted the analysis with a propensity score-matched pair procedure.
Measures and definition
We identified income status by defining low-income patients as those qualifying for waived medical copayment because this status is verified by the Taiwan Bureau of National Health Insurance. Also recorded were whether the surgery was performed in a teaching hospital and the types of noncardiac surgery and anesthesia. We used the ICD-9-CM to define preoperative medical diseases and postoperative complications. Preoperative diabetes (code 250) was defined as the major exposure. Coexisting medical conditions were determined from medical claims for the 24-month preoperative period and included hypertension (codes 401–405), mental disorders (290–319), ischemic heart disease (410–414), chronic obstructive pulmonary disease (COPD) (490–496), stroke (430–438), hyperlipidemia (272.0, 272.1, and 272.2), liver cirrhosis (571), or renal dialysis. In-hospital 30-day mortality after the index surgery was considered the study’s primary outcome. Six major surgical postoperative complications were analyzed as secondary outcomes, including septicemia (codes 038 and 998.5), pneumonia (480–486), stroke (430–438), acute renal failure (584), deep wound infection (958.3), and acute myocardial infarction (410) after the index surgery (21,22). To investigate the impact of uncontrolled or poorly controlled diabetes on 30-day postoperative mortality, we identified patients with uncontrolled diabetes according to ICD-9-CM definitions (codes 250.02, 250.03, 250.12, 250.13, 250.22, 250.23, 250.32, 250.33, 250.42, 250.43, 250.52, 250.53, 250.62, 250.63, 250.72, 250.73, 250.82, 250.83, 250.92, and 250.93). Also considered as potential diabetes-related contributors to 30-day postoperative mortality were type 1 or type 2 diabetes and diabetes-related comorbidities, including ketoacidosis (code 250.1), coma (250.2 and 250.3), renal manifestations (250.4), eye involvement (250.5), and peripheral circulatory disorders (250.7). Prolonged length of hospital stay and stay in the intensive care unit (ICU); in-hospital medical expenditures, including claims for prescription/medications, physician fees, ward fees, laboratory examinations, and radiologic images; medical treatments; surgical procedures; and postoperative care were also considered secondary outcomes. These outcomes were compared between patients with and without preoperative diabetes.
Statistical analysis
To reduce confounding errors (23–29), we used a propensity score-matched pair procedure to adjust for sex, age, types of surgery and anesthesia, operation in a teaching hospital or not, low-income status, and coexisting medical conditions between surgical patients with and without diabetes. Adjusted odds ratios (ORs) with 95% CIs for 30-day postoperative complications and mortality between patients with and without diabetes were analyzed with multivariate logistic regression by controlling for sex, age, low-income status, operation in a teaching hospital or not, preoperative coexisting medical conditions, and types of surgery and anesthesia. To assess the impact of diabetes severity on 30-day postoperative mortality, multivariate logistic regression was used to control for potential confounders, including ketoacidosis, coma, renal manifestations, eye involvement, peripheral circulatory disorders, type 1 and type 2 diabetes, and uncontrolled diabetes. The multivariate logistic regression analyses were also applied to investigate 30-day postoperative mortality associated with coexisting hypertension, mental disorders, ischemic heart disease, COPD, stroke, hyperlipidemia, liver cirrhosis, and renal dialysis. SAS version 9.1 (SAS Institute Inc., Cary, NC) statistical software was used for data analyses; two-sided P < 0.05 indicated significant differences between groups.
RESULTS
Table 1 shows the demographic characteristics of patients with and without diabetes who underwent noncardiac surgery. After propensity score matching, the absolute difference between surgical patients with and without diabetes was insignificant. Compared with nondiabetic control patients (Table 2), patients with diabetes showed higher risks of postoperative complications, including septicemia (OR 2.76 [95% CI 2.50–3.04]), pneumonia (1.88 [1.65–2.14]), stroke (1.70 [1.49–1.94]), acute renal failure (3.59 [2.88–4.48]), deep wound infection (1.33 [1.04–1.70]), acute myocardial infarction (3.65 [2.43–5.49]), and overall complications (2.42 [2.26–2.60]). Preoperative diabetes was associated with a significant increase in 30-day postoperative mortality (1.84 [1.46–2.32]). Prolonged length of hospital stay, stay in the ICU, and increased medical expenditures were all significantly associated with preoperative diabetes, with ORs of 2.30 (2.16–2.44), 1.67 (1.59–1.76), and 1.32 (1.25–1.40), respectively. Compared with surgical patients without diabetes, patients with diabetes were more likely to have significantly higher postoperative mortality with type 1 diabetes (1.99 [1.24–3.21]) and diabetes-related comorbidities, such as eye involvement (2.11 [1.58–2.80]), peripheral circulatory disorders (2.13 [1.51–3.02]), ketoacidosis (2.21 [1.27–3.84]), renal manifestations (2.46 [1.89–3.21]), and coma (2.81 [1.86–4.22]) (Table 3). Patients with uncontrolled diabetes faced a higher risk of postoperative mortality than did those without diabetes (2.18 [1.71–2.79]).
Table 1.
Characteristics of patients with and without diabetes undergoing noncardiac surgery
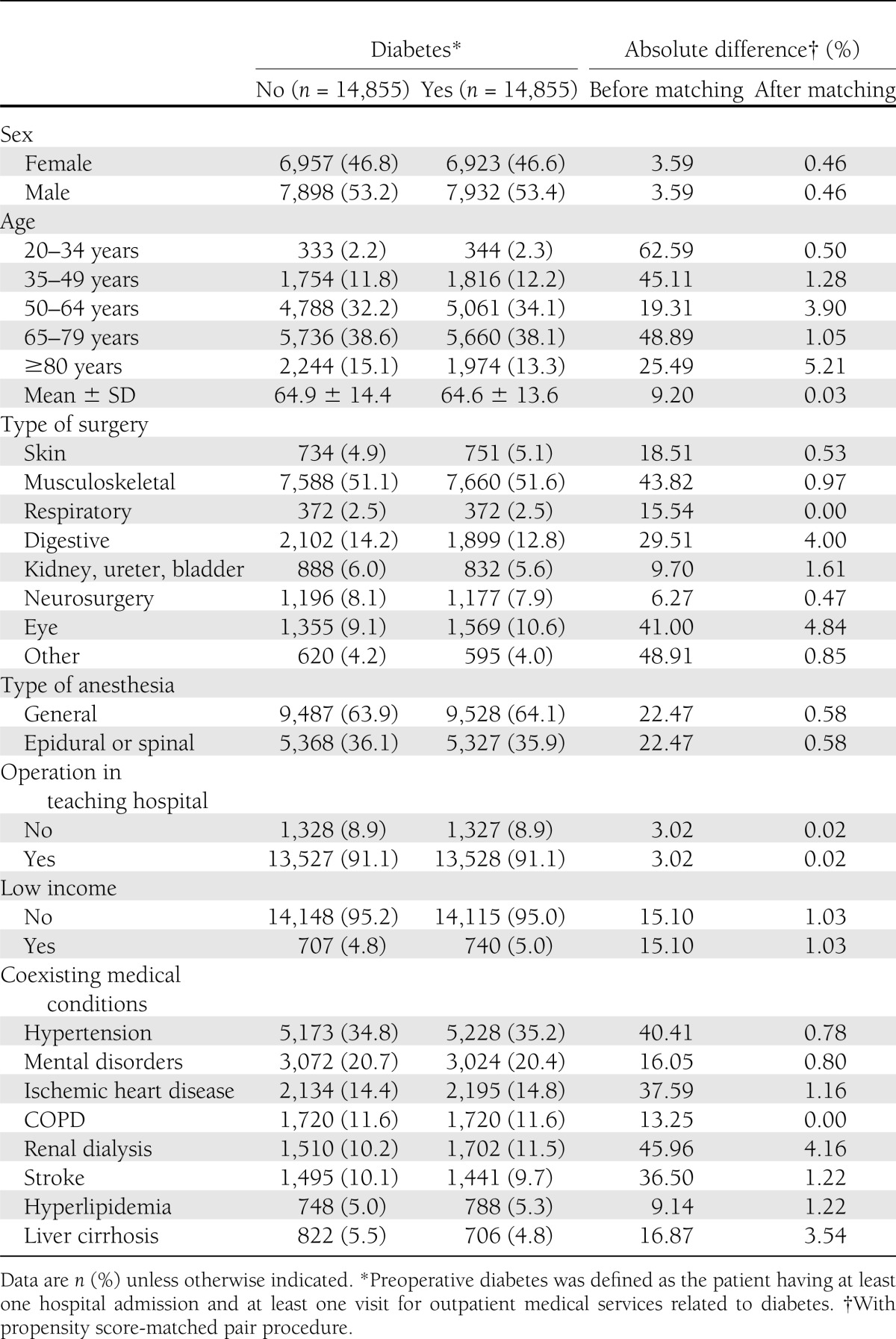
Table 2.
Risk of postoperative complications associated with diabetes in the multiple logistic regression models*
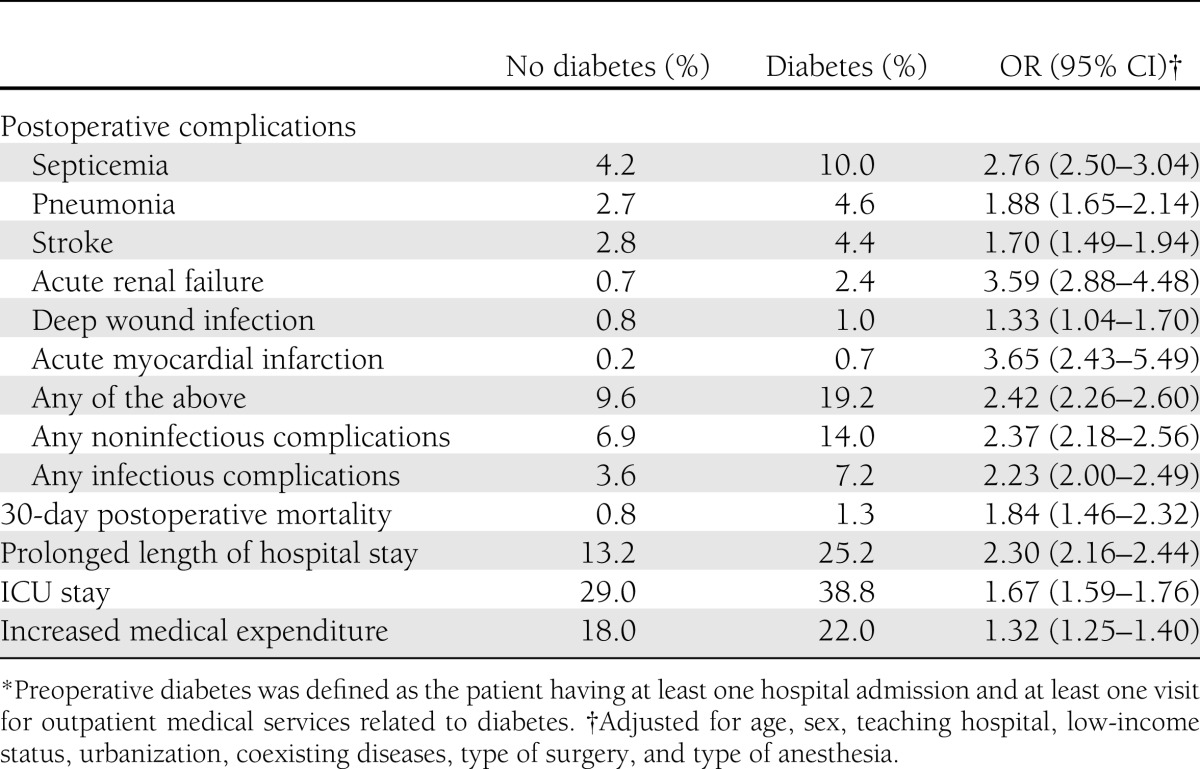
Table 3.
Preoperative diabetes-related comorbidities in association with 30-day postoperative mortality in the multiple logistic regression models*
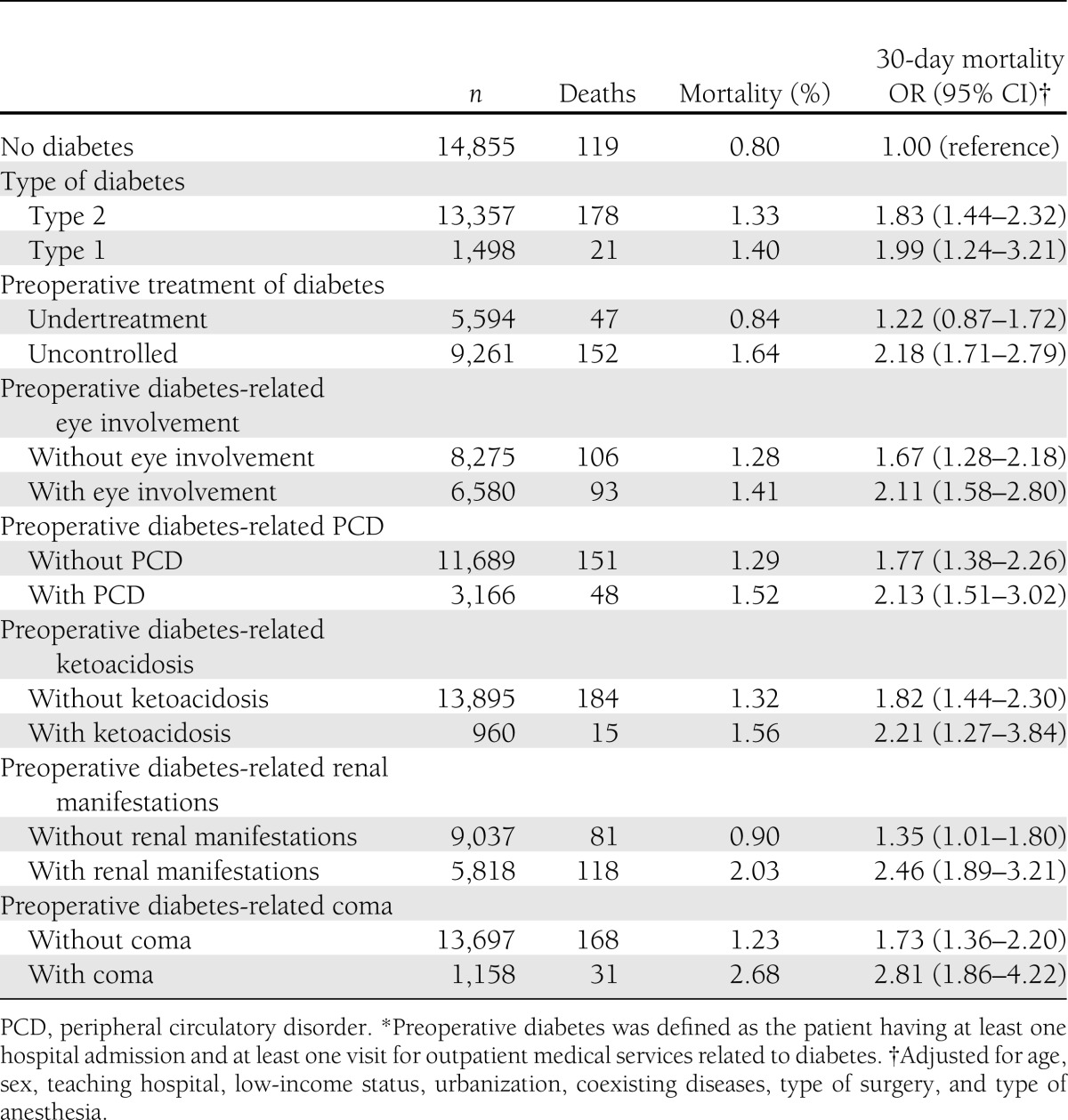
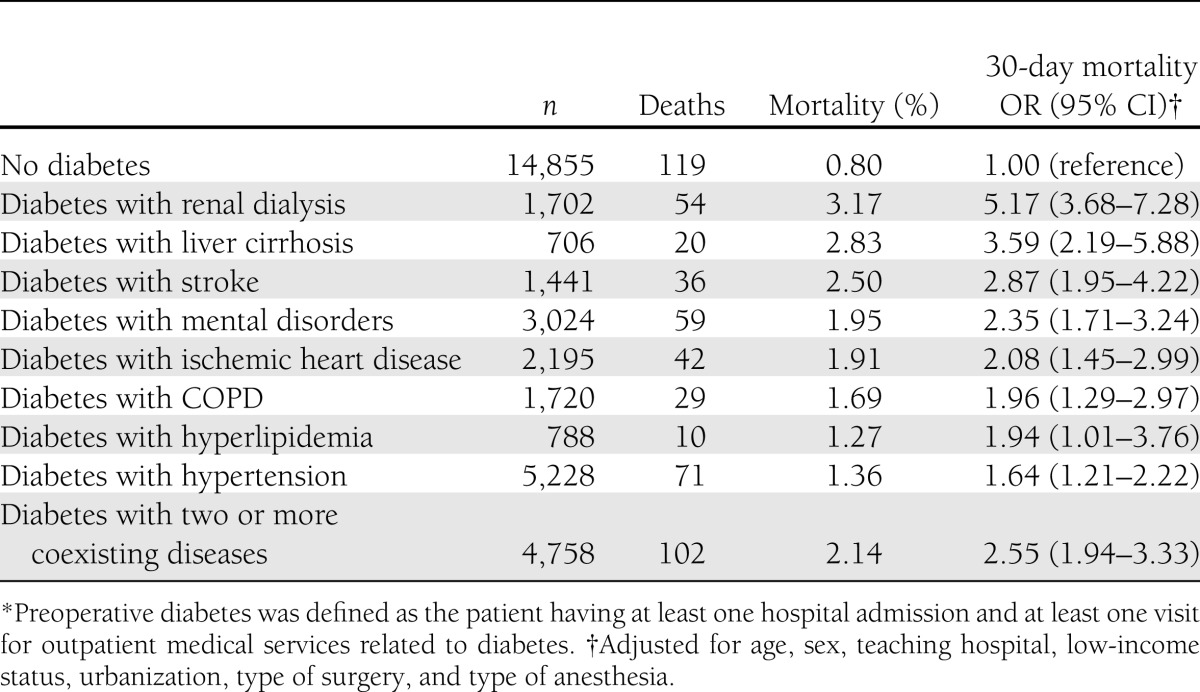
Table 4 shows the impact of coexisting medical conditions on 30-day postoperative mortality in patients with diabetes. Renal dialysis (OR 5.17 [95% CI 3.68–7.28]), liver cirrhosis (3.59 [2.19–5.88]), stroke (2.87 [1.95–4.22]), mental disorders (2.35 [1.71–3.24]), ischemic heart disease (2.08 [1.45–2.99]), COPD (1.96 [1.29–2.97]), and hyperlipidemia (1.94 [1.01–3.76]) increase the risk of postoperative mortality for patients with diabetes compared with control patients. Patients with diabetes and more than two coexisting medical conditions were more likely to have higher postoperative mortality than those without diabetes (2.55 [1.94–3.33]).
Table 4.
The joint effects of coexisting medical conditions on 30-day postoperative mortality in patients with diabetes*
CONCLUSIONS
To our knowledge this is the first nationwide, population-based, propensity score-matched study to demonstrate that diabetes increases postoperative complications, particularly for acute myocardial infarction and renal failure, in patients with diabetes undergoing noncardiac surgeries. Diabetes also increased length of hospital stay, medical expenditures, and 30-day postoperative mortality. Patients with diabetes and related comorbidities, type 1 diabetes, uncontrolled diabetes, and coexisting medical conditions were all more vulnerable to 30-day postoperative mortality than were control patients without diabetes.
Most previous studies adjusted for age, sex, socioeconomic covariates, and hospital characteristics but did not consider the factors of preoperative diabetes-related comorbidities associated with postoperative mortality (9–12). Coexisting medical conditions, such as mental disorder, liver cirrhosis, and renal dialysis, have been deemed independent determinants in perioperative complications and mortality (8,17,19,20,24–26). By using a propensity score-matched pair model to reduce influences from these confounders, we have validated that diabetes is an important independent determinant for perioperative adverse events in patients undergoing noncardiac surgeries.
Whether diabetes is an independent determinant of increased short-term (30-day) postoperative complications in noncardiac surgery was unclear (6–11). The present study indicates that diabetes predisposes patients to infectious and noninfectious postoperative complications. The findings are the first in our knowledge to indicate that diabetes increases the risk of acute renal failure in patients undergoing noncardiac surgeries (8–11) and are similar to those of a recent epidemiological, longitudinal follow-up investigation that suggested a 2.5-fold risk of acute renal failure for patients with diabetes (30). Hyperglycemia-associated endothelial dysfunction (31), impaired wound healing (32), postoperative sepsis (33), and cerebral ischemia (34) in combination with superimposed surgical stress in noncardiac surgeries could substantially contribute to the increased risk of postoperative complications. In addition, the prolonged length of hospital and ICU stays resulting from the increased risk of postoperative complications might consequently elevate hospital expenditures. However, this assumption should be validated in future prospective randomized trials.
Although Cook et al. (10) reported similar findings in patients with diabetes undergoing cervical fusion, they relied only on administrative ICD-9-CM coding to define uncontrolled diabetes and did not consider coexisting medical conditions as potential confounders in their analysis. The current study identified uncontrolled diabetes on the basis of ICD-9-CM coding. In addition, to reduce confounding from such coexisting medical conditions as hypertension, mental disorders, ischemic heart disease, COPD, renal dialysis, stroke, hyperlipidemia, and liver cirrhosis (24–29,33), we adjusted for these covariates in the propensity score-matched models and then controlled for these factors through multivariate logistic regression. We found that uncontrolled diabetes and diabetes-related comorbidities increase postoperative 30-day mortality after various noncardiac surgeries, and these findings were similar to those in cardiac surgeries (13). However, whether intensive glycemic control in the noncardiac surgery postoperative period could reduce the risk of short-term mortality still needs to be elucidated.
In this study, type 1 diabetes had a greater influence on postoperative 30-day mortality than type 2 diabetes; this comparison is unprecedented. Cook et al. (10) reported that type 1 diabetes was associated with a higher mortality rate than type 2 diabetes in patients who underwent cervical fusion. Patients with type 1 diabetes mostly started from their younger stage when compared with those with type 2 diabetes (35). Expected longer exposure to the hyperglycemic environment predisposing to the occurrence of more severe macro- and microangiopathy-related complications could partially account for the present results. However, this hypothesis needs to be tested in future studies.
Previous studies indicated that diabetic patients with coexisting mental disorders were at increased long-term mortality compared with those without; this finding could be partially attributed to poor diabetes control in those with coexisting mental disorders (36). History of liver cirrhosis, renal dialysis, ischemic heart disease, stroke, COPD, or hypertension per se was proven to be independently associated with higher risks of postoperative mortality in noncardiac surgeries (24–29). However, whether a greater impact on postoperative short-term mortality exists in patients with diabetes and these comorbid conditions is still unresolved. The present study provides evidence that coexisting liver cirrhosis or renal dialysis in combination with diabetes has a much higher impact on postoperative 30-day mortality than diabetes only. With these results, medical resources should be appropriately allocated to patients with diabetes and coexisting medical conditions when they undergo noncardiac surgeries.
This study had several limitations. First, records from reimbursement claims for postoperative complications, comorbidities, and coexisting medical conditions might be underreported in clinical practice. However, these data should be distributed equally between both groups without causing bias in the results. This study focused on 30-day postoperative short-term mortality, which is less likely to be underreported. Second, severity of diabetes was defined by the registered diagnosis codes, not by laboratory data, such as fasting glucose level. Third, detailed information on sociodemographic factors, dietary habits, and lifestyles was not available in the National Health Insurance Research Database for this study to validate the association of these factors with postoperative adverse outcomes (8,17–20). Fourth, to strictly identify patients with diabetes, we enrolled only those who experienced hospitalization and outpatient care for diabetes within 24 months before the index surgery. Therefore, data interpretation should be made carefully; the findings from this study might only be suitable for patients with significant diabetes. Although the surgical patients without diabetes were those who had no medical visits with an ICD-9-CM code (250) for diabetes within 24 months before the index surgery, some mild or borderline diabetes may have existed in this group. In this way, the influence of diabetes on postoperative outcomes may be underestimated.
In conclusion, we precisely describe that diabetes is an important independent risk factor in increased postoperative complications, 30-day mortality, length of hospital stay, and medical expenditures in patients undergoing noncardiac surgeries. Uncontrolled diabetes, coexisting medical conditions, and diabetes-related comorbidities all contribute to increased postoperative 30-day mortality. This study provides a comprehensive perioperative assessment and enhances the understanding of the complex issues of care for patients with diabetes who undergo noncardiac surgery.
Acknowledgments
This study is based in part on data obtained from the National Health Insurance Research Database provided by the Bureau of National Health Insurance of the Taiwan Department of Health and managed by the National Health Research Institutes.
No potential conflicts of interest relevant to this article were reported.
The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, the Taiwan Department of Health, or the National Health Research Institutes.
C.-C.Y. interpreted the results, drafted the manuscript, and reviewed and edited the manuscript. C.-C.L. created the concept and design, performed the statistical analysis, interpreted the results, drafted the manuscript, and reviewed and edited the manuscript. Y.-C.C., L.-B.J., H.-R.Y., C.-C.S., and T.-L.C. participated in the study design, interpreted the results, and revised the manuscript. T.-L.C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–1053 [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polonsky KS. The past 200 years in diabetes. N Engl J Med 2012;367:1332–1340 [DOI] [PubMed] [Google Scholar]
- 4.Herlitz J, Wognsen GB, Emanuelsson H, et al. Mortality and morbidity in diabetic and nondiabetic patients during a 2-year period after coronary artery bypass grafting. Diabetes Care 1996;19:698–703 [DOI] [PubMed] [Google Scholar]
- 5.McAlister FA, Man J, Bistritz L, Amad H, Tandon P. Diabetes and coronary artery bypass surgery: an examination of perioperative glycemic control and outcomes. Diabetes Care 2003;26:1518–1524 [DOI] [PubMed] [Google Scholar]
- 6.Poon RT, Fan ST, Wong J. Does diabetes mellitus influence the perioperative outcome or long term prognosis after resection of hepatocellular carcinoma? Am J Gastroenterol 2002;97:1480–1488 [DOI] [PubMed] [Google Scholar]
- 7.Hjortrup A, Sørensen C, Dyremose E, Hjortsø NC, Kehlet H. Influence of diabetes mellitus on operative risk. Br J Surg 1985;72:783–785 [DOI] [PubMed] [Google Scholar]
- 8.Yeh CC, Hsieh CH, Liao CC, Su LT, Wang YC, Li TC. Diabetes mellitus and cerebrovascular disease as independent determinants for increased hospital costs and length of stay in open appendectomy in comparison with laparoscopic appendectomy: a nationwide cohort study. Am Surg 2012;78:329–334 [PubMed] [Google Scholar]
- 9.Juul AB, Wetterslev J, Kofoed-Enevoldsen A. Long-term postoperative mortality in diabetic patients undergoing major non-cardiac surgery. Eur J Anaesthesiol 2004;21:523–529 [DOI] [PubMed] [Google Scholar]
- 10.Cook C, Tackett S, Shah A, et al. Diabetes and perioperative outcomes following cervical fusion in patients with myelopathy. Spine 2008;33:E254–E260 [DOI] [PubMed] [Google Scholar]
- 11.Bower WF, Jin L, Underwood MJ, et al. Overt diabetes mellitus adversely affects surgical outcomes of noncardiovascular patients. Surgery 2010;147:670–675 [DOI] [PubMed] [Google Scholar]
- 12.Marchant MH, Jr, Viens NA, Cook C, Vail TP, Bolognesi MP. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am 2009;91:1621–1629 [DOI] [PubMed] [Google Scholar]
- 13.Sato H, Carvalho G, Sato T, Lattermann R, Matsukawa T, Schricker T. The association of preoperative glycemic control, intraoperative insulin sensitivity, and outcomes after cardiac surgery. J Clin Endocrinol Metab 2010;95:4338–4344 [DOI] [PubMed] [Google Scholar]
- 14.Malmstedt J, Leander K, Wahlberg E, Karlström L, Alfredsson L, Swedenborg J. Outcome after leg bypass surgery for critical limb ischemia is poor in patients with diabetes: a population-based cohort study. Diabetes Care 2008;31:887–892 [DOI] [PubMed] [Google Scholar]
- 15.Frisch A, Chandra P, Smiley D, et al. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care 2010;33:1783–1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wukich DK, McMillen RL, Lowery NJ, Frykberg RG. Surgical site infections after foot and ankle surgery: a comparison of patients with and without diabetes. Diabetes Care 2011;34:2211–2213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yeh CC, Wu SC, Liao CC, Su LT, Hsieh CH, Li TC. Laparoscopic appendectomy for acute appendicitis is more favorable for patients with comorbidities, the elderly, and those with complicated appendicitis: a nationwide population-based study. Surg Endosc 2011;25:2932–2942 [DOI] [PubMed] [Google Scholar]
- 18.Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf 2011;20:236–242 [DOI] [PubMed] [Google Scholar]
- 19.Chang CC, Hu CJ, Lam F, Chang H, Liao CC, Chen TL. Postoperative adverse outcomes in surgical patients with epilepsy: a population-based study. Epilepsia 2012;53:987–994 [DOI] [PubMed] [Google Scholar]
- 20.Liao CC, Chiu WT, Yeh CC, Chang HC, Chen TL. Risk and outcomes for traumatic brain injury in patients with mental disorders. J Neurol Neurosurg Psychiatry 2012;83:1186–1192 [DOI] [PubMed] [Google Scholar]
- 21.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med 2009;361:1368–1375 [DOI] [PubMed] [Google Scholar]
- 22.Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ, Participants in the VA National Surgical Quality Improvement Program Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 2005;242:326–341; discussion 341–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health 1995;85:949–956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kao HK, Chang KP, Ching WC, Tsao CK, Cheng MH, Wei FC. Postoperative morbidity and mortality of head and neck cancers in patients with liver cirrhosis undergoing surgical resection followed by microsurgical free tissue transfer. Ann Surg Oncol 2010;17:536–543 [DOI] [PubMed] [Google Scholar]
- 25.Chen CC, Hsu PW, Lee ST, et al. Brain surgery in patients with liver cirrhosis. J Neurosurg 2012;117:348–353 [DOI] [PubMed] [Google Scholar]
- 26.Drolet S, Maclean AR, Myers RP, Shaheen AA, Dixon E, Donald Buie W. Morbidity and mortality following colorectal surgery in patients with end-stage renal failure: a population-based study. Dis Colon Rectum 2010;53:1508–1516 [DOI] [PubMed] [Google Scholar]
- 27.Sabaté S, Mases A, Guilera N, et al. ANESCARDIOCAT Group Incidence and predictors of major perioperative adverse cardiac and cerebrovascular events in non-cardiac surgery. Br J Anaesth 2011;107:879–890 [DOI] [PubMed] [Google Scholar]
- 28.Belmont PJ, Jr, Davey S, Orr JD, Ochoa LM, Bader JO, Schoenfeld AJ. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg 2011;213:370–378 [DOI] [PubMed] [Google Scholar]
- 29.Mashour GA, Shanks AM, Kheterpal S. Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology 2011;114:1289–1296 [DOI] [PubMed] [Google Scholar]
- 30.Girman CJ, Kou TD, Brodovicz K, et al. Risk of acute renal failure in patients with type 2 diabetes mellitus. Diabet Med 2012;29:614–621 [DOI] [PubMed] [Google Scholar]
- 31.Hempel A, Maasch C, Heintze U, et al. High glucose concentrations increase endothelial cell permeability via activation of protein kinase C alpha. Circ Res 1997;81:363–371 [DOI] [PubMed] [Google Scholar]
- 32.Brem H, Tomic-Canic M. Cellular and molecular basis of wound healing in diabetes. J Clin Invest 2007;117:1219–1222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rayfield EJ, Ault MJ, Keusch GT, Brothers MJ, Nechemias C, Smith H. Infection and diabetes: the case for glucose control. Am J Med 1982;72:439–450 [DOI] [PubMed] [Google Scholar]
- 34.Pulsinelli WA, Levy DE, Sigsbee B, Scherer P, Plum F. Increased damage after ischemic stroke in patients with hyperglycemia with or without established diabetes mellitus. Am J Med 1983;74:540–544 [DOI] [PubMed] [Google Scholar]
- 35.Duncan GE. Prevalence of diabetes and impaired fasting glucose levels among US adolescents: National Health and Nutrition Examination Survey, 1999-2002. Arch Pediatr Adolesc Med 2006;160:523–528 [DOI] [PubMed] [Google Scholar]
- 36.Frayne SM, Halanych JH, Miller DR, et al. Disparities in diabetes care: impact of mental illness. Arch Intern Med 2005;165:2631–2638 [DOI] [PubMed] [Google Scholar]


