Abstract
OBJECTIVE
The optimal screening regimen for gestational diabetes mellitus (GDM) remains controversial. Risk factors used in selective screening guidelines vary. Given that universal screening is not currently adopted in our European population, we aimed to evaluate which selective screening strategies were most applicable.
RESEARCH DESIGN AND METHODS
Between 2007 and 2009, 5,500 women were universally screened for GDM, and a GDM prevalence of 12.4% using International Association of Diabetes in Pregnancy Study Groups (IADPSG) criteria was established. We retrospectively applied selective screening guidelines to this cohort.
RESULTS
When we applied National Institute for Health and Clinical Excellence (NICE), Irish, and American Diabetes Association (ADA) guidelines, 54% (2,576), 58% (2,801), and 76% (3,656) of women, respectively, had at least one risk factor for GDM and would have undergone testing. However, when NICE, Irish, and ADA guidelines were applied, 20% (120), 16% (101), and 5% (31) of women, respectively, had no risk factor and would have gone undiagnosed. Using a BMI ≥30 kg/m2 for screening has a specificity of 81% with moderate sensitivity at 48%. Reducing the BMI to ≥25 kg/m2 (ADA) increases the sensitivity to 80% with a specificity of 44%. Women with no risk factors diagnosed with GDM on universal screening had more adverse pregnancy outcomes than those with normal glucose tolerance.
CONCLUSIONS
This analysis provides a strong argument for universal screening. However, if selective screening were adopted, the ADA guidelines would result in the highest rate of diagnosis and the lowest number of missed cases.
The World Health Organization (WHO) defines gestational diabetes mellitus (GDM) as any degree of glucose intolerance with onset or first recognition during pregnancy (1). GDM results in higher maternal and neonatal morbidities in the short- and long-term. GDM is common, and prevalence is increasing due to the increase in overweight and obesity in the background population. In Ireland it complicates ∼12% (2) of pregnancies.
Diagnosis of GDM and subsequent treatment decreases morbidities for the mother and baby in the index pregnancy. Diagnosis of GDM also highlights an at-risk population that can be targeted for primary prevention of type 2 diabetes. The optimal screening regimen for GDM remains controversial, with conflicting recommendations for universal and selective screening among various expert groups. Currently, the American Diabetes Association (ADA), the U.S. Preventive Services Task Force (USPSTF), the National Institute for Health and Clinical Excellence (NICE), and the 2010 Irish guidelines recommend risk factor–based screening. The Australasian Diabetes in Pregnancy society recommends universal screening (3). With studies from North America (4) showing that ∼90% of women have at least one risk factor for GDM, there is a strong argument for universal screening. However, a lack of randomized-controlled trials addressing this issue means there is insufficient evidence to definitely determine whether a universal approach to screening should be the gold standard of care. Also, the population of North America is phenotypically different from that of Europe, so evidence-based recommendations from North American studies may not be directly applicable to a European population.
The Atlantic Diabetes in Pregnancy (ATLANTIC DIP) network is a research collaboration among five antenatal centers along the Irish Atlantic seaboard. The aim of this clinical network is to provide optimal, evidence-based care for women before, during, and after pregnancy. Between 2007 and 2009, universal screening for GDM was offered. Given that universal screening is not currently adopted or supported financially at a national level, we aimed to analyze which selective screening modalities and single risk factors had the highest sensitivity and specificity for diagnosing GDM. An additional objective was to calculate the proportion of women with GDM who would be missed if selective screening methods were adopted. Finally, there is a suggestion that women with GDM who carry no risk factors for the condition, who are only detected as part of universal screening, have a “milder” form of glucose intolerance and that their pregnancy outcomes may be similar to those of the background population. As such, this study analyzed pregnancy outcomes of these “low-risk” GDM women and compared them with the outcomes in women with normal glucose tolerance (NGT).
RESEARCH DESIGN AND METHODS
Design and study population
This was a retrospective study designed to analyze the relative merits of various screening techniques and single risk factors for GDM, in terms of diagnostic accuracy (sensitivity and specificity), as part of the ATLANTIC DIP research program.
Universal screening was offered to all pregnant women in five antenatal centers from 2007 to 2009. Screening occurred at 24–28 weeks’ gestation using a 75-g 2-h oral glucose tolerance test, and International Association of Diabetes in Pregnancy Study Groups (IADPSG) criteria were applied for diagnosis. This involved having one or more of fasting plasma glucose ≥5.1 mmol/L/92 mg/dL, 1-h postglucose load ≥10 mmol/L/180 mg/dL, or 2-h postglucose load ≥8.5 mmol/L/153 mg/dL.
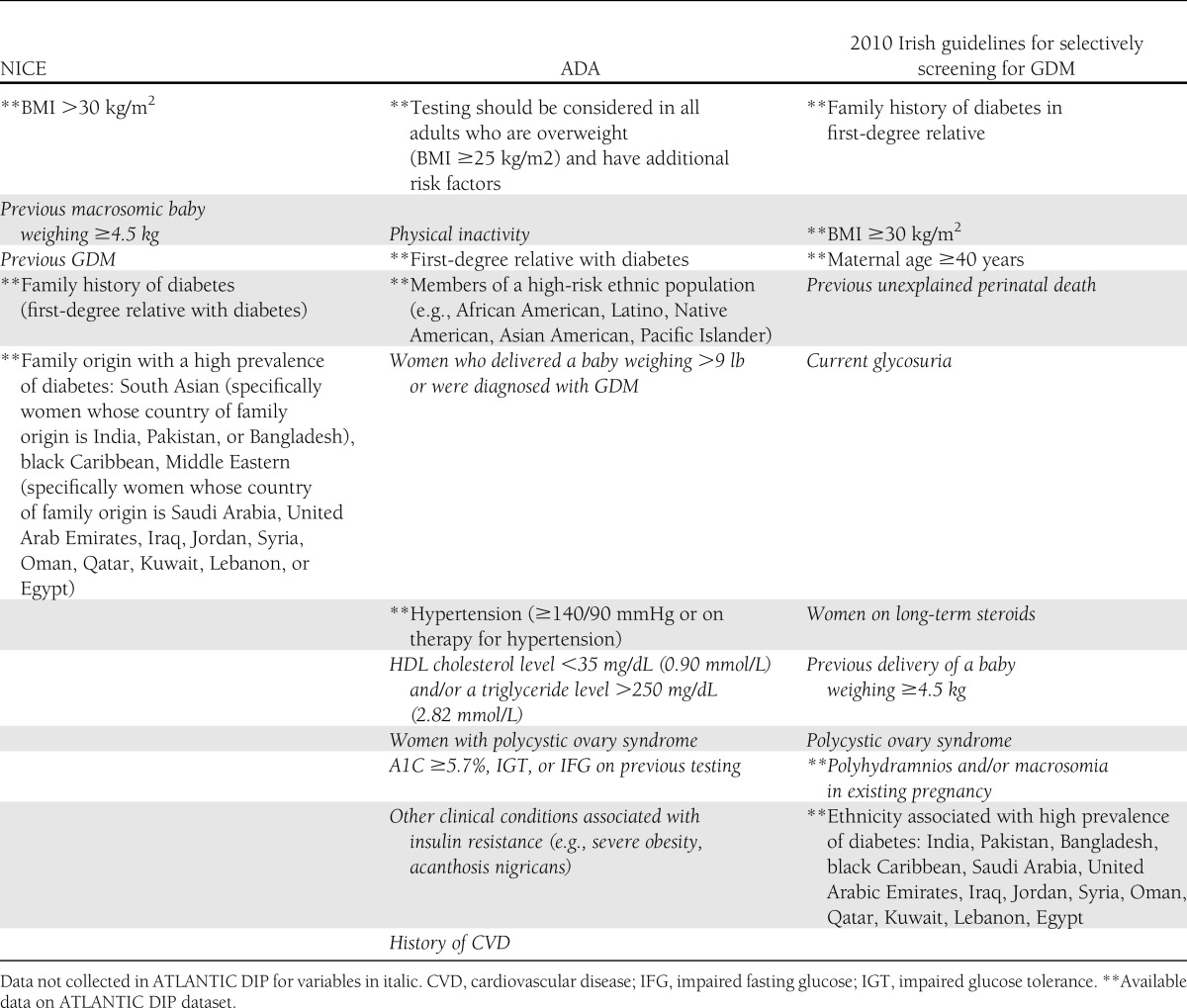
At the first obstetric visit, 12,487 pregnant women were offered screening and 9,365 (75%) consented. Of those who consented, 5,500 (44%) presented for testing. Baseline characteristics of age, ethnicity, parity, family history of diabetes in first-degree relatives, BMI, and blood pressure were recorded. Data were collected and stored in an electronic database (DIAMOND). If GDM was diagnosed, women received combined antenatal/diabetes care according to local guidelines. Once pregnancy was completed, data on maternal (pre-eclamptic toxemia, pregnancy-induced hypertension, mode of delivery) and infant (weight, size for gestational age, Apgar scores, hypoglycemia, jaundice, respiratory distress syndrome) were collected. The screening regimens chosen for analysis were universal screening and selective screening based on the ADA, NICE, and 2010 Irish national GDM guidelines (Table 1).
Table 1.
Comparison of guidelines for screening for GDM
Statistical analyses
PASW 19 and statspages.org software were used for statistical analysis. The χ2 test was used to find the proportion of GDM between the stratified groups of age and BMI. Sensitivity, specificity, and 95% CIs were calculated for each risk factor, including the stratified groups for age and BMI. Descriptive statistics were used to identify the number of GDM women with zero risk factors and with more than one risk factor. Classification tree analysis was used to assess the age and BMI at which the risk of GDM was significantly increased.
RESULTS
At the first obstetric visit, 12,487 pregnant women were offered universal screening and 9,365 (75%) consented. Of those who consented, 5,500 (44%) presented for testing. The prevalence of GDM was 12.4% (n = 681). Most women (93%) were Caucasian, with a mean age of 32 ± 5.3 years and a mean BMI of 26.9 ± 5.1 kg/m2. The characteristics of women with GDM in the presence and absence of risk factors for GDM are reported in Table 2.
Table 2.
Maternal characteristics
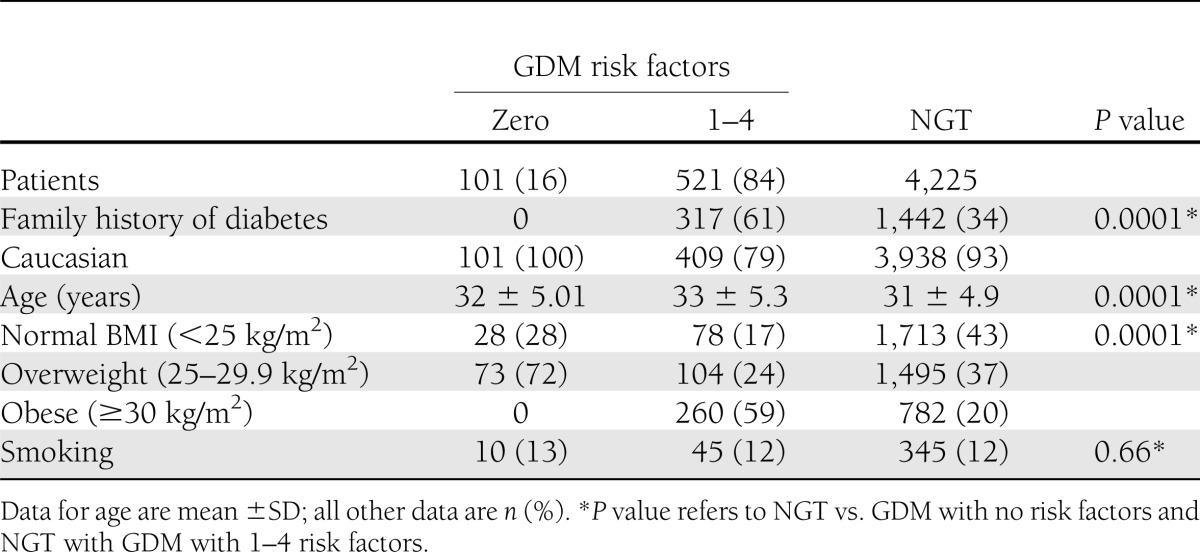
All women received medical nutritional therapy and advice on exercise. In addition, 31% of women required insulin to reach their glucose goals, comprising 10% of women with no risk factors and 21% of women with risk factors.
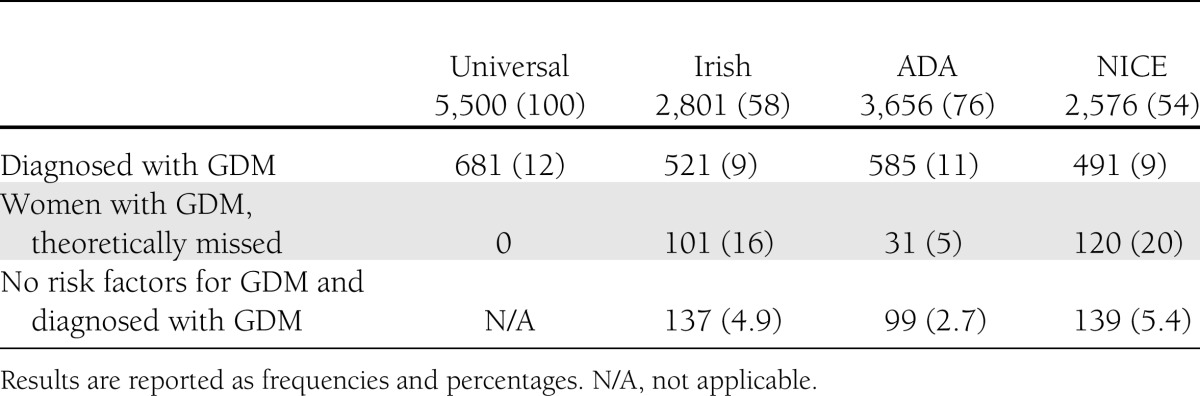
When the NICE guidelines were applied, 54% of women (n = 2,576) had at least one risk factor for GDM and would have undergone testing. Twenty percent of women (n = 120) with GDM on universal screening had no NICE risk factors and would have remained undiagnosed. Fifty-eight percent of women (n = 2,801) had at least one risk factor for GDM and would have undergone testing if the Irish guidelines were applied. Sixteen percent (n = 101) had no risk factors and would have remained undiagnosed. Seventy-six percent of women (n = 3,656) had at least one risk factor according to the ADA guidelines and would have undergone testing. Five percent of women (n = 31) identified with GDM by universal screening had no risk factors and would have remained undiagnosed. The prevalence of GDM among those with no risk factors was 2.7, 4.9, and 5.4% using ADA, Irish, and NICE guidelines, respectively (Table 3).
Table 3.
Numbers diagnosed with screening criteria
We analyzed whether using a combination of age and BMI only was effective in terms of diagnostic accuracy. Using a classification tree analysis, we found that women who had a low prevalence (<1%) of GDM were those aged <21 years with a BMI <25 kg/m2, so potentially, this group could be omitted from screening. This can be compared with a prevalence of 7.7% in women aged >21 years with a BMI ≥25 kg/m2. This would have prevented only 79 women from being unnecessarily tested.
Age (>40 years) is included as a risk factor in the Irish guidelines. When applied to our cohort it, equated to a high specificity (94%) for GDM; however, the sensitivity was very low, at 9%. If age was reduced to ≥30 years the sensitivity increased to 73%, with a specificity of 34%.
There is debate about which BMI cutoff should be considered as part of selective screening criteria. ADA recommends ≥25 kg/m2, NICE, >30 kg/m2, and the Irish guidelines, ≥30 kg/m2. In our cohort, a BMI ≥30 kg/m2 was specific (81%), with intermediate sensitivity (48%). Reducing the BMI cutoff to ≥25 kg/m2, as indicated in the ADA guidelines, increased the sensitivity to 80%, with a reduction of specificity to 44%.
Blood pressure of 140/90 mmHg has a very low sensitivity of 12%, although it is very specific (93%). Of the women screened, 47% stated they had a first-degree relative with diabetes, which had intermediate sensitivity of 47% and specificity of 70%. When ethnicity was assessed, a higher proportion of non-Caucasian women (28%) were identified as having GDM compared with their Caucasian counterparts (11%). It is highly specific (94%) but has a very low sensitivity (16%) given that the vast majority of our patients were Caucasian.
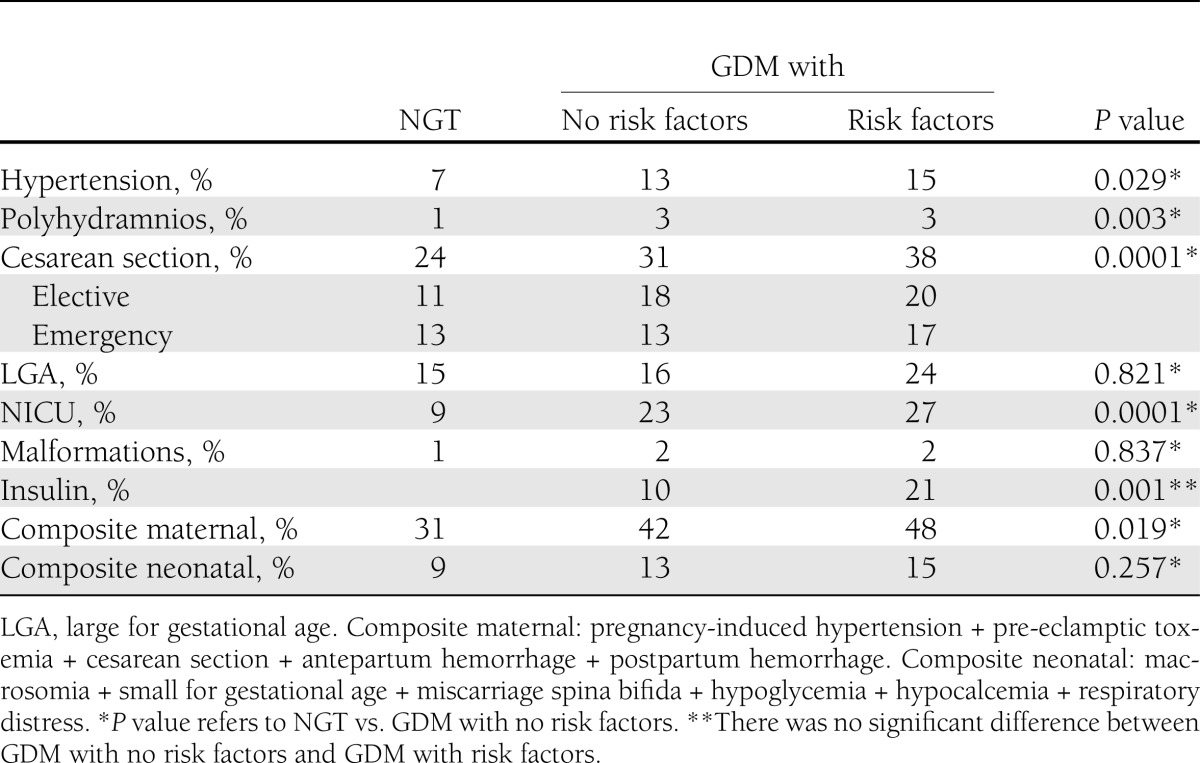
We examined pregnancy outcomes of women who had no risk factors but were diagnosed with GDM on universal screening, defined as the “low-risk” group of women with NGT (Table 4). This low-risk group was treated for GDM according to local protocol. These low-risk women with GDM had more hypertensive disorders in pregnancy (P = 0.029), higher rates of total cesarean section deliveries (P = 0.0001), and more polyhydramnios (P = 0.003). Infants had a nonsignificant increase in congenital malformations and significantly higher rates of admission to neonatal intensive care units (NICU; P = 0.0001), despite treatment. The miscarriage rates were similar between the two groups. We also compared outcomes in those with GDM who had no risk factors with those who had one or more risk factors. Maternal and neonatal morbidities (hypertensive disorders, previous miscarriages, caesarean section deliveries, admission to NICU, large for gestational age, and premature deliveries ≤36 weeks) were higher in those who had at least one risk factor for GDM (Table 4). Rates of stillbirths and congenital malformations were similar between the two groups.
Table 4.
Pregnancy outcomes among women with and without GDM diagnosed by IADPSG criteria
CONCLUSIONS
GDM is common, with a rising prevalence, and is associated with higher maternal and neonatal morbidity. It carries additional long-term health consequences for the mother and her offspring (4,5). Diagnosis and appropriate treatment of the condition is associated with a reduction in morbidity (6,7). Given the lack of symptoms associated with this condition and the evidence-base accruing from several studies (5,8–10), screening of asymptomatic patients is considered necessary. However, there is no consensus regarding which women should be screened and whether selective, risk factor–based screening or a universal screening approach should be adopted. Also, among those groups advocating selective screening, there is still considerable variability in the risk factors that are incorporated into a screening strategy. These uncertainties are based on a lack of randomized controlled trials indicating which approach is superior.
Our study aimed to apply the available screening strategies to our European, predominantly Caucasian population. We set out to analyze whether the current, most commonly adopted national and international selective screening practices are appropriate compared with universal screening using IADPSG criteria (11). Through unselected screening of all women and recording of risk factors, we were able to evaluate the usefulness of selective screening for the detection of GDM and assess how many women would have remained undiagnosed if selective screening rather than universal screening were applied. We have shown that selective screening misses a significant proportion of women and that outcomes in these pregnancies are worse compared with NGT pregnancies.
It is important to note that less than half (n = 5,500 [44%]) of those offered screening attended. We have found this to be related primarily to the woman’s geographical location relative to the screening site in addition to her socioeconomic status (12). We also found that those with risk factors for GDM were more likely to attend for screening, which is a potential confounder in the prevalence rates of GDM. Finally the 75-g oral glucose tolerance test was administered at an isolated appointment, which may have affected attendance rates, because the appropriate time for testing (i.e., 24–28 weeks) does not coincide with the national routine antenatal schedule.
Some have argued that universal screening will identify more women with GDM in a low-risk population and that these might have less clinical significance (13). Also, some of the trials showing improvements in morbidity outcomes used selective screening strategies, and as such, contained higher-risk populations or a high proportion of women of non-Caucasian ethnicity, which is different from our European population (5,14). Contrary to this theory of “low-risk” GDM, studies have shown similar poor outcomes among young, lean women with GDM (15,16). We addressed this by analyzing outcomes in this low-risk cohort with GDM and compared them with women with NGT as well as with women who had GDM and risk factors for the condition. Despite diagnosis and subsequent treatment, pregnancy outcomes were worse for the mother and baby in those with “low-risk” GDM compared with NGT women. The pregnancy outcomes in this group, however, were better than for those with GDM and risk factors. This suggests that although these women carried a lower risk than women with risk factors, they still had poorer outcomes compared with women with NGT.
We believe the higher rate of caesarean section and admission rates to the NICU in those with GDM and no risk factors compared those with NGT was partly due to local obstetric practice and the label of “GDM” rather than to clinical indication. This raises issues regarding appropriate management of these women and education of those involved in clinical care.
The current argument for screening lies in several large studies, including the Australian Carbohydrate Intolerance Study in pregnant women (ACHOIS) (10) trial and the study by Landon et al. (6), which showed that treating even mild levels of glucose intolerance resulted in a reduction in perinatal mortality and morbidity; as such, this is accepted to be indirect evidence of the role of screening. Of course, levels of glucose intolerance, whether mild or severe, cannot be known before actually performing glucose tolerance testing, and instead, risk factors for the condition are accepted as surrogate markers for potential dysglycemia. Cohorts such as the ACHOIS, however, comprised 25% of higher-risk ethnic minorities, and thus are not directly applicable to our population. The Hyperglycemia and Adverse Pregnancies Outcomes (HAPO) trial (5) also consisted of 52.7% non-Caucasian ethnicities. Our study by comparison is more applicable to a European population.
Screening also identifies women at high risk of developing diabetes in the future. As previously shown, 18% of this cohort continued to have prediabetes/diabetes in the postpartum period (17), and this has further risen to 30% at a median of 2.5 years after the index pregnancy (18). Of women who progressed to prediabetes/diabetes postpartum, 90% had risk factors for GDM. Prediabetes/diabetes in the first year postpartum appears to be reduced by breast-feeding, and thus, diagnosis and subsequent encouragement to breast-feed is important, although long-term data in this area are lacking.
There are also long-term consequences for the offspring related to fetal hyperinsulinism and β-cell hyperstimulation as well as changes in the hypothalamus (19). If GDM can be detected and treated in a timely fashion using an appropriate population-specific screening strategy, then hyperstimulation of the fetal pancreas may be avoided, with consequences downstream for the adult health of the infant. During the routine antenatal appointments at our five study centers, the following details were recorded: age, parity, obstetric history, family history of diabetes, BMI, ethnicity, and blood pressure. Details such as history of polycystic ovarian syndrome, signs of insulin resistance, lipid panel, physical inactivity, or previous steroid use are not routinely recorded. Our practice is representative of that at a national level, and thus, those variables may be of limited usefulness to a screening strategy. Also, applying selective screening is time-consuming during routine obstetric assessment and may in fact result in missing GDM in women who do have risk factors because of inadequate recording.
Because of the lack of international uniformity and financial constraints, we set out to assess the various selective screening guidelines. Our analysis suggests that the ADA guidelines would result in the highest diagnosis rate with the lowest number of women misclassified as not having GDM. If we are to adjust our current guidelines, we suggest including BMI ≥25 kg/m2 rather than the current recommendation of ≥30 kg/m2 because this alone will result in correctly diagnosing 80% of women with GDM. We have also shown that women aged <21 years who have a BMI <25 kg/m2 could potentially be excluded from screening because GDM prevalence is low in this subgroup. This would incur a cost-saving, but this cohort is small and comprises 2% of the entire group.
Acknowledgments
This study was funded by the Health Research Board, Ireland.
No potential conflicts of interest relevant to this article were reported.
G.E.A. performed the statistical analysis, wrote the research design and methods and results sections, and reviewed and edited the manuscript. L.A.O. wrote the introduction and the discussion sections and reviewed and edited the manuscript. F.D., principal investigator of the ATLANTIC DIP study, conceived the research question and reviewed and edited the manuscript. F.D. is the guarantor of this work and as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank all the participants who consented to take part in the ATLANTIC DIP study and the staff from the participating hospitals.
Parts of this study were presented in poster form at the 7th International DIP Symposium—Diabetes, Hypertension, Metabolic Syndrome & Pregnancy, Florence, Italy, 13–16 March 2013; at the 48th Annual Meeting of the European Association for the Study of Diabetes, Berlin, Germany, 1–5 October 2012; and at the 44th Annual Meeting of the Diabetic Pregnancy Study Group, Lille, France, 18–20 October 2012.
Footnotes
References
- 1.World Health Organization. Definition, Diagnosis, and Classification of Diabetes Mellitus and its Complications Geneva, World Health Org., 1999 (report)
- 2.O’Sullivan EP, Avalos G, O’Reilly M, Dennedy MC, Gaffney G, Dunne F, Atlantic DIP collaborators Atlantic Diabetes in Pregnancy (DIP): the prevalence and outcomes of gestational diabetes mellitus using new diagnostic criteria. Diabetologia 2011;54:1670–1675 [DOI] [PubMed] [Google Scholar]
- 3.Nankervis A, McIntyre HD, Moses R, et al. Australasian Diabetes In Pregnancy Society (ADIPS) Consensus Guidelines for the Testing and Diagnosis of Gestational Diabetes Mellitus in Australia [article online]. Available from http://www.adips.org Accessed 10 November 2012
- 4.Dodd JM, Crowther CA, Antoniou G, Baghurst P, Robinson JS. Screening for gestational diabetes: the effect of varying blood glucose definitions in the prediction of adverse maternal and infant health outcomes. Aust N Z J Obstet Gynaecol 2007;47:307–312 [DOI] [PubMed] [Google Scholar]
- 5.Metzger BE, Lowe LP, Dyer AR, et al. HAPO Study Cooperative Research Group Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008;358:1991–2002 [DOI] [PubMed] [Google Scholar]
- 6.Landon MB, Spong CY, Thom E, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 2009;361:1339–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alwan N, Tuffnell DJ, West J. Treatments for gestational diabetes. Cochrane Database Syst Rev 2009:CD003395. [DOI] [PMC free article] [PubMed]
- 8.Jensen DM, Korsholm L, Ovesen P, Beck-Nielsen H, Mølsted-Pedersen L, Damm P. Adverse pregnancy outcome in women with mild glucose intolerance: is there a clinically meaningful threshold value for glucose? Acta Obstet Gynecol Scand 2008;87:59–62 [DOI] [PubMed] [Google Scholar]
- 9.Ferrara A, Weiss NS, Hedderson MM, et al. Pregnancy plasma glucose levels exceeding the American Diabetes Association thresholds, but below the National Diabetes Data Group thresholds for gestational diabetes mellitus, are related to the risk of neonatal macrosomia, hypoglycaemia and hyperbilirubinaemia. Diabetologia 2007;50:298–306 [DOI] [PubMed] [Google Scholar]
- 10.Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS, Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 2005;352:2477–2486 [DOI] [PubMed] [Google Scholar]
- 11.International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Metzger BE, Gabbe SG, Persson B, et al. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010;33:676–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cullinan J, Gillespie P, Owens L, Dunne F, ATLANTIC DIP Collaborators Accessibility and screening uptake rates for gestational diabetes mellitus in Ireland. Health Place 2012;18:339–348 [DOI] [PubMed] [Google Scholar]
- 13.Naylor CD, Sermer M, Chen E, Farine D, Toronto Trihospital Gestational Diabetes Project Investigators Selective screening for gestational diabetes mellitus. N Engl J Med 1997;337:1591–1596 [DOI] [PubMed] [Google Scholar]
- 14.Langer O, Yogev Y, Most O, Xenakis EM. Gestational diabetes: the consequences of not treating. Am J Obstet Gynecol 2005;192:989–997 [DOI] [PubMed] [Google Scholar]
- 15.Moses RG, Moses J, Davis WS. Gestational diabetes: do lean young Caucasian women need to be tested? Diabetes Care 1998;21:1803–1806 [DOI] [PubMed] [Google Scholar]
- 16.Weeks JW, Major CA, de Veciana M, Morgan MA. Gestational diabetes: does the presence of risk factors influence perinatal outcome? Am J Obstet Gynecol 1994;171:1003–1007 [DOI] [PubMed] [Google Scholar]
- 17.O’Reilly MW, Avalos G, Dennedy MC, O’Sullivan EP, Dunne F. Atlantic DIP: high prevalence of abnormal glucose tolerance post partum is reduced by breast-feeding in women with prior gestational diabetes mellitus. Eur J Endocrinol 2011;165:953–959 [DOI] [PubMed] [Google Scholar]
- 18.Noctor E, Atlantic DIP. The prevalence of pre-diabetes/diabetes up to 5 years post partum in women with previous gestational diabetes along the Atlantic coast. In Abstracts of the European Association for the Study of Diabetes, 2012. Abstract 1077, S442 [Google Scholar]
- 19.Galjaard S, Devlieger R, Van Assche FA. Fetal growth and developmental programming. J Perinat Med 2013;41:101–105 [DOI] [PubMed] [Google Scholar]


