Abstract
OBJECTIVE
The relation of breakfast intake frequency to metabolic health is not well studied. The aim of this study was to examine breakfast intake frequency with incidence of metabolic conditions.
RESEARCH DESIGN AND METHODS
We performed an analysis of 3,598 participants from the community-based Coronary Artery Risk Development in Young Adults (CARDIA) study who were free of diabetes in the year 7 examination when breakfast and dietary habits were assessed (1992–1993) and participated in at least one of the five subsequent follow-up examinations over 18 years.
RESULTS
Relative to those with infrequent breakfast consumption (0–3 days/week), participants who reported eating breakfast daily gained 1.9 kg less weight over 18 years (P = 0.001). In a Cox regression analysis, there was a stepwise decrease in risk across conditions in frequent breakfast consumers (4–6 days/week) and daily consumers. The results for incidence of abdominal obesity, obesity, metabolic syndrome, and hypertension remained significant after adjustment for baseline measures of adiposity (waist circumference or BMI) in daily breakfast consumers. Hazard ratios (HRs) and 95% CIs for daily breakfast consumption were as follows: abdominal obesity HR 0.78 (95% CI 0.66–0.91), obesity 0.80 (0.67–0.96), metabolic syndrome 0.82 (0.69–0.98), and hypertension 0.84 (0.72–0.99). For type 2 diabetes, the corresponding estimate was 0.81 (0.63–1.05), with a significant stepwise inverse association in black men and white men and women but no association in black women. There was no evidence of differential results for high versus low overall dietary quality.
CONCLUSIONS
Daily breakfast intake is strongly associated with reduced risk of a spectrum of metabolic conditions.
There is a historical precedent for breakfast intake being linked with health. The earliest documented claims were from fledgling ready-to-eat cereal companies in the 1800s and from a pork producer in the 1920s touting physician recommendations to eat a hearty breakfast of bacon and eggs (1,2). Midway through the 1900s, small studies finding potential health benefits of breakfast began appearing in the scientific literature (3–5). In the time since, investigation on a number of aspects related to breakfast intake and health has occurred with a range of study designs generally demonstrating that both the timing (breaking of a fasting state) and content of breakfast may be important for health, especially metabolic health, via interrelated mechanisms involving metabolism and appetite (6). On the basis of the existing data, the 2010 U.S. dietary guidelines were the first to include a specific recommendation for breakfast intake (7).
Several studies provide prospective evidence directly linking either the behavior of eating breakfast or consumption of typical breakfast foods with lower risk of weight gain/obesity, metabolic syndrome, hypertension, and type 2 diabetes (8–14). An important interpretative consideration is that breakfast intake frequency has generally been dichotomized into an all-or-none proposition, although consistent evidence across cultures and populations suggests there is a range of breakfast intake frequencies (8,15,16).
Therefore, we examined the association of a range of breakfast intake frequencies with risk of an array of incident metabolic outcomes over 18 years in the Coronary Artery Risk Development in Young Adults (CARDIA) study, a multicenter, population-based, prospective study of cardiovascular risk evolution in young black and white adult men and women in the U.S. We hypothesized that breakfast eating would show a graded inverse relationship with incident metabolic conditions, partially explained by quality of the overall diet.
RESEARCH DESIGN AND METHODS
Study and data collection
The CARDIA study is a multicenter, longitudinal investigation of the evolution of ischemic heart disease risk starting in young adulthood (17). The study began in 1985–1986 with 5,115 black and white adults 18–30 years of age from four metropolitan areas (Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA). Study participants were sampled to obtain roughly equal numbers of blacks (51.5%) and whites (48.5%), men (45.5%) and women (54.5%), 18–24 years of age (44.9%) and 25–30 years of age (55.1%), and with a high school education or less (39.7%) and with more than a high school education (60.3%). Participants were contacted by telephone every year and examined in person at baseline and 2, 5, 7, 10, 15, 20, and 25 years after baseline. A majority of the group was examined at each of the follow-up examinations (91, 86, 81, 79, 74, 72, and 72% of survivors, respectively). At each clinical examination, participants were asked to present fasting in the morning. Tobacco use, strenuous physical activity, and intake of caffeine, food, and alcohol were proscribed. The examinations followed standardized protocols harmonized over time and included measurements of blood pressure (BP), anthropometrics, and phlebotomy and structured questionnaires on sociodemographics, medical and family history, psychosocial characteristics, and diet, among others. The CARDIA study was approved by the institutional review board of each participating institution, and signed informed consent was obtained at each examination.
During each clinic exam, blood was drawn from an antecubital vein, and after serum separation, aliquots were stored at −70°C until shipped on dry ice to a central laboratory. Procedures followed in the collection and storage of plasma samples, laboratory quality-control procedures, and methodology for analysis of plasma triglycerides, HDL cholesterol, LDL cholesterol, and total cholesterol are described elsewhere (18). Serum glucose was measured at year 0 using the hexokinase ultraviolet method by American Bio-Science Laboratories (Van Nuys, CA) and at subsequent examinations using hexokinase coupled to glucose-6-phosphate dehydrogenase by Linco Research (St. Louis, MO).
BP was measured three times at 1-min intervals. At the baseline through year 15 follow-up exams, BP was measured using the Hawksley (Lancing, Sussex, U.K.) random-zero sphygmomanometer; the first and fifth phase Korotkoff sounds were recorded (17). At the year 20 and 25 exams, BP was measured with an automated sphygmomanometer (Omron HEM907XL oscillometer; Omron, Schaumburg, IL). The protocol specified the appropriate cuff size (small, medium, large, or extra-large) based on the upper arm circumference, which was measured by the BP technician at the midpoint between the acromion and the olecranon. Omron values were recalibrated to corresponding random zero values based on a study of both measurement techniques in 903 participants at year 20, as estimated random zero systolic value = 3.74 + 0.96 × Omron systolic value, and estimated random zero diastolic value = 1.30 + 0.97 × Omron diastolic value (19).
Anthropometry (height, weight, and waist circumference) was measured at each exam. Body weight was measured to the nearest 0.2 kg using a calibrated balance beam scale in participants wearing light clothing. Height (without shoes) was measured to the nearest 0.5 cm using a vertical ruler and waist circumference to the nearest 0.5 cm at the minimal abdominal girth (20). BMI was computed as weight in kilograms divided by squared height in meters.
Diet was assessed at years 0, 7, and 20 by using an interviewer-administered CARDIA diet history questionnaire (21). Interviewers asked open-ended questions about dietary consumption in the past month within 100 food categories that referenced 1,609 separate food items. Additionally, visits per week to fast food restaurants were queried at each examination, and frequency of breakfast, lunch, dinner, and morning, afternoon, and evening snacks (days/week) was queried at years 7 and 20. An a priori dietary quality score based on overall dietary intake was included as a covariate (16). In brief, 46 food groups considered beneficial or adverse with respect to health effects were categorized by increasing consumption level with scores of 0–4 (for 20 food groups considered beneficial), 4–0 (for 13 food groups considered adverse), or 0 (for 13 food groups considered neutral). The a priori dietary quality score was the sum of category scores, with a theoretical maximum of 132. Based on prior findings, it was assumed that a higher a priori dietary pattern score indicated better diet quality (22–24). The CARDIA diet history has been shown to be a valid and reliable instrument. Nutrient and energy estimates had larger variability among blacks than among whites (21,25). For other covariates, standard questionnaires were used to obtain self-reported demographic and behavioral information. Sex, race, date of birth, education, and cigarette smoking were ascertained by a structured interview or self-administered questionnaire at each examination. A physical activity score was derived from the CARDIA physical activity history, which is a simplified version of the Minnesota Leisure Time Physical Activity Questionnaire (26).
Assessment of outcomes
Year 7 (1992–1993) serves as the baseline for this study. Incident outcomes were identified at exam years 10–25. Obesity was defined as BMI ≥30 kg/m2 and abdominal obesity as waist circumference >88 cm for women or >102 cm for men. Hypertension was defined as systolic BP ≥140 mmHg, diastolic BP ≥90 mmHg, or self-reported use of antihypertensive medication. The metabolic syndrome was defined using the National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP) III criteria (27) as the presence of three or more of the following five conditions: 1) abdominal obesity, 2) fasting triglycerides ≥150 mg/dL, 3) HDL cholesterol <40 mg/dL in men and <50 mg/dL in women, 4) BP ≥130 mmHg systolic or ≥85 mmHg diastolic or use of antihypertensive medications, and 5) fasting glucose ≥100 mg/dL or use of diabetes medications. Incidence of type 2 diabetes was defined as use of diabetes medication (assessed at every visit), a fasting blood glucose level of ≥6.99 mmol/L (126 mg/dL) (measured at years 10–25), 2 h postchallenge glucose ≥11.1 mmol/L (200 mg/dL) (performed at the year 10, 20, and 25 exams), and/or an HbA1c ≥6.5% (48 mmol/mol) (assessed at the year 20 and 25 visits).
Statistical analysis
From the total sample of 5,115, we excluded 1,029 who did not participate in the year 7 clinical exam, a further 171 who did not participate in any clinical exam in years 10–25, 60 with diabetes at year 7, 215 without dietary data or with reported energy intakes not in the range of 800–8,000 kcal/day for men and 600–6,000 kcal/day for women, and 42 missing other data (alcohol, smoking, or physical activity) for an analytic sample of 3,598. For analyses on outcomes other than type 2 diabetes, participants prevalent with the condition at year 7 were also excluded and total n is provided in tables.
Breakfast intake frequency categories were created that allowed for logical cut points with a sufficient number of subjects. Baseline (year 7) characteristics were calculated across breakfast intake frequency categories reported at this exam. Multivariable least squares–adjusted means from general linear models (SAS Proc GLM) were used to estimate weight gain in kilograms and increase in waist circumference in centimeters by breakfast intake frequency categories. The models adjust for age, study center, race, sex, education (years), cigarette smoking (current, former, or never), physical activity (units/week), alcohol consumption (mL/day), fast food restaurant use (visits/week), overall dietary quality score, frequency of lunch/dinner and morning/afternoon/evening snacks (days/week), total energy intake (kcal), and weight or waist circumference and height at year 7, respectively. All participants were free of diabetes at each time point in the analysis of weight and waist circumference changes.
Proportional hazards (Cox) regression (SAS Proc PHREG) was used to examine the association between breakfast intake frequency categories and incidence of metabolic conditions. We estimated the hazard ratio (HR) and corresponding 95% CI. Time to event was calculated from the date of the baseline examination (year 7) to the date of the first follow-up examination meeting the criteria for the incident outcome (cases) or to the date of the last CARDIA examination for each participant without the incident outcome (censored). A tiered modeling approach was applied for all outcomes. The main model included age (years), study center, race, sex, education (years), cigarette smoking (current, former, or never), physical activity (units/week), alcohol consumption (mL/day), fast food restaurant use (visits/week), dietary quality score, frequency of lunch/dinner and morning/afternoon/evening snacks (days/week), and total energy intake (kcal). Depending on the outcome, either waist circumference (cm) or BMI (kg/m2) from year 7 was included in a second model, and, for hypertension, a third model further adjusted for systolic BP at year 7 in analyses examining potential mediators. There was no evidence that proportional hazards assumptions were violated for any of the outcomes as indicated by the lack of significant interaction between the breakfast intake frequency variable and time in the models. Tests for trend were performed by assigning the median value of intake frequency to the category and entering this as a continuous ordinal variable into the models. Effect modification of the associations was considered by level of the dietary quality index, BMI, race, and sex. All analyses were conducted with SAS statistical software version 9.2 (SAS Institute, Cary, NC).
RESULTS
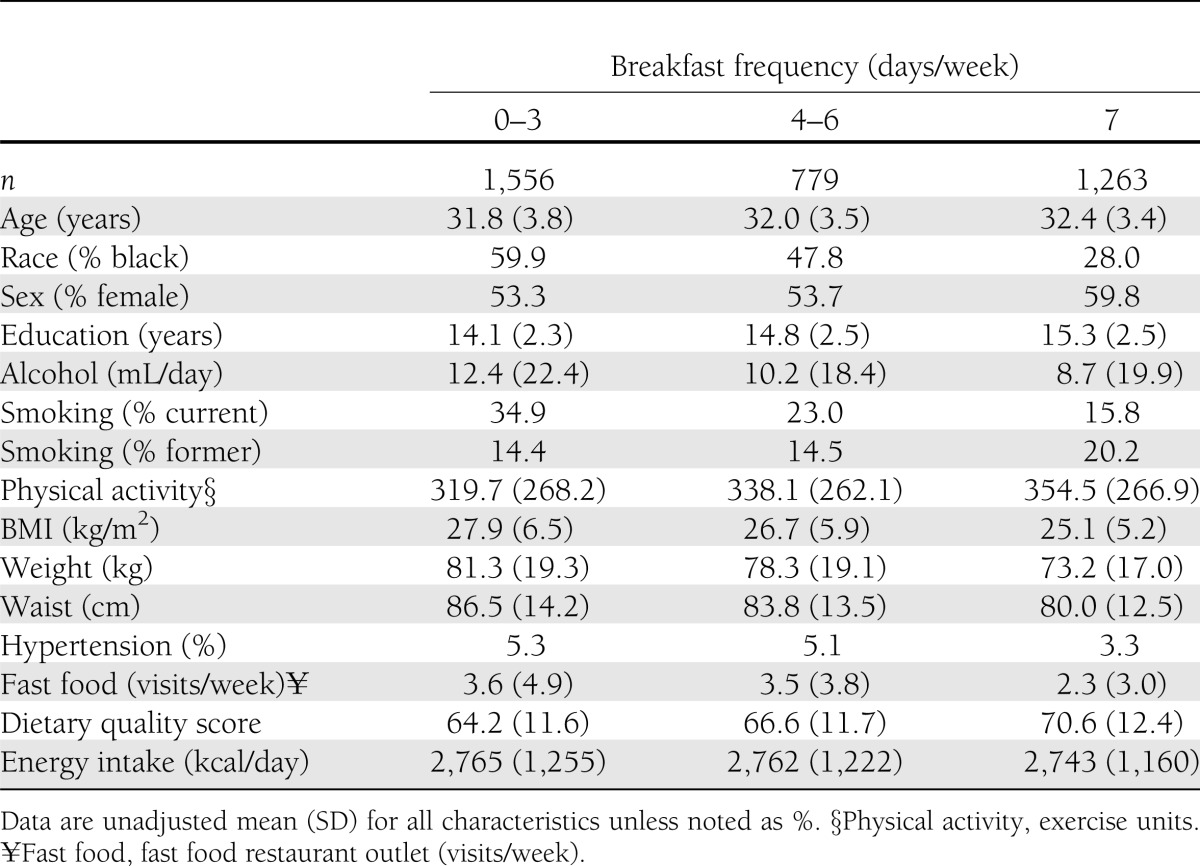
Based upon the year 7 data, 43.2% of participants reported infrequent breakfast intake (0–3 days/week), 21.7% reported eating breakfast frequently (4–6 days/week), and 35.1% of participants reported eating breakfast daily (7 days/week) (Table 1). With higher levels of breakfast intake, a greater proportion of participants were white and female and were on average more educated, consumed less alcohol, did not currently smoke, were more physically active, had a lower BMI, visited fast food restaurants less frequently, and had a higher dietary quality score.
Table 1.
Participant characteristics according to breakfast frequency (days per week): CARDIA year 7, 1992–1993
Over 18 years of follow-up, there was a significant mean weight gain in all participants free of diabetes throughout the study; yet, frequent (4–6 days/week) and daily breakfast consumers gained less weight relative to non- or infrequent breakfast consumers (Supplementary Fig. 1A and B). Specifically, participants reporting daily breakfast intake gained 1.91 kg less than those reporting infrequent intake (0–3 days/week) (P = 0.001) over 18 years after full adjustment for demographic, lifestyle, dietary habits, and baseline weight. A similar trend was observed for waist circumference.
Across all metabolic outcomes, there was a stepwise decrease in crude incidence rate, and the incidence rate was nearly halved in daily breakfast consumers relative to those who were infrequent breakfast consumers (0–3 days/week) (Table 2). These graded associations were evident in the main Cox regression model adjusting for demographics, lifestyle covariates, and dietary habits. Relative to infrequent intake of breakfast, frequent breakfast intake (4–6 days/week) and daily breakfast intake were each significantly associated with a decreased risk of abdominal obesity, obesity, metabolic syndrome, hypertension, and type 2 diabetes in a ranked manner. After adjustment for baseline measures of adiposity (waist circumference [cm] or BMI [kg/m2]), the associations were attenuated but a significant inverse association persisted between daily breakfast intake and abdominal obesity, obesity, metabolic syndrome, and hypertension.
Table 2.
HR and 95% CI of metabolic outcomes according to breakfast frequency: CARDIA years 7–25 (1992–1993 to 2010–2011)
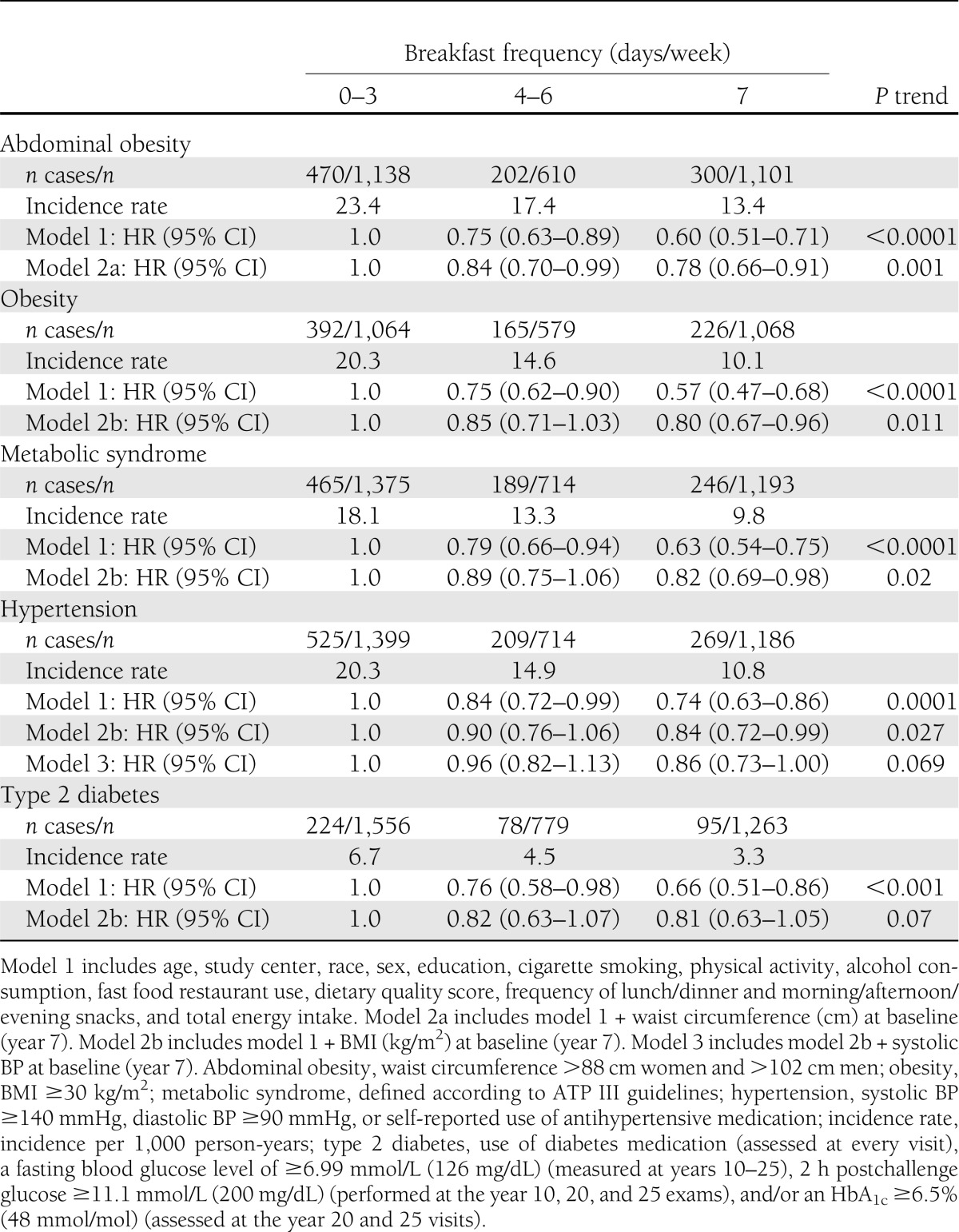
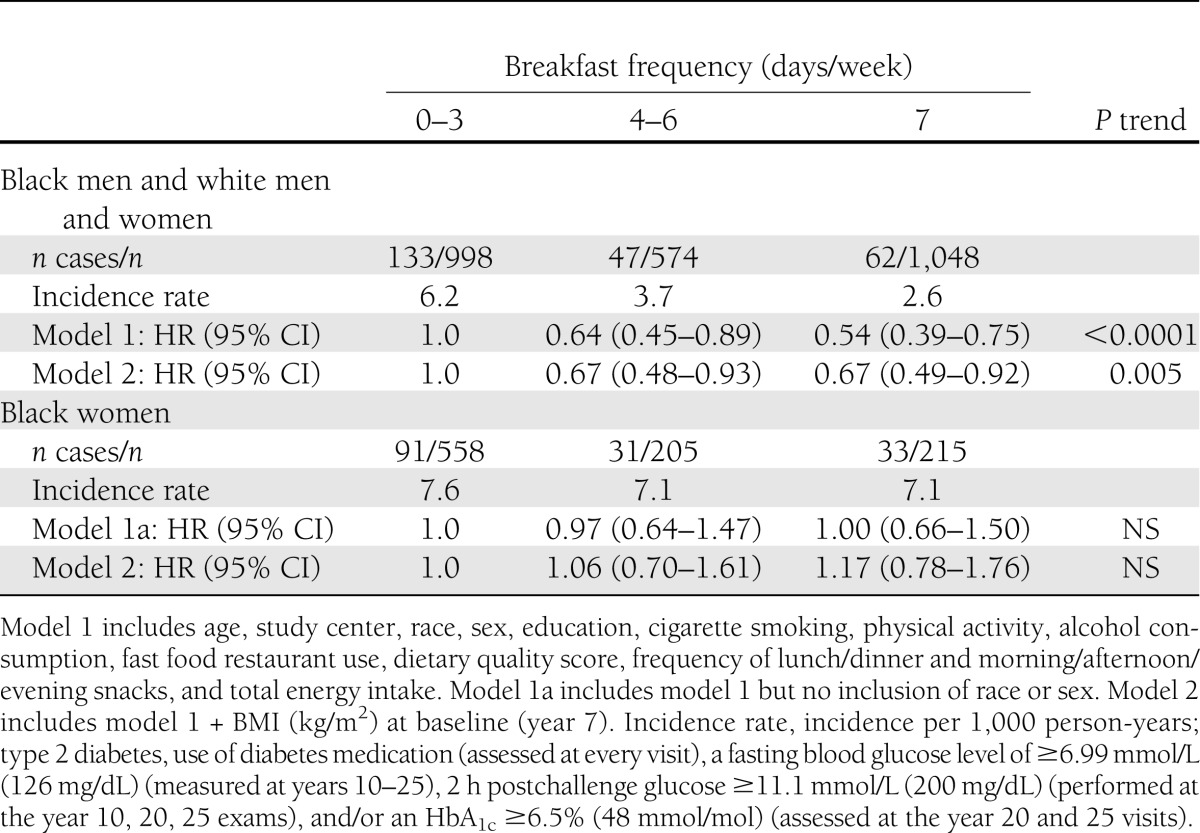
The estimates for incident type 2 diabetes were mediated upon adjustment for BMI in the whole-population HR and 95% CI for frequent breakfast intake (HR 0.82 [95% CI 0.63–1.07]) and daily intake (0.81 [0.63–1.05]). However, there was evidence that the results for type 2 diabetes differed in black women from those for the rest of the study sample (Table 3). In black women, breakfast intake frequency was not associated with incident type 2 diabetes, whereas the results were consistent and strongly inversely associated in black men and white men and women even after adjustment for BMI. Black women had the highest rate of incident diabetes in the cohort and greatest mean level of BMI in year 7 (29.0 kg/m2) relative to the rest of the study population (black men, 27.0 kg/m2; white men, 26.0 kg/m2; white women, 24.9 kg/m2). Adjustment for hypertensive status and medication did not materially alter the results for incident type 2 diabetes.
Table 3.
HR and 95% CI of type 2 diabetes according to breakfast frequency, stratified results: CARDIA years 7–25 (1992–1993 to 2010–2011)
There was no evidence that the results varied for any of the other outcomes by race, sex, or BMI at baseline. There was no evidence that adjustment for family history of type 2 diabetes or hypertension materially altered any of the results. The frequency of lunch, dinner, or snacks was not associated with any of the outcomes. Of note, we also examined the association between breakfast intake frequency and future dyslipidemia (low HDL cholesterol and elevated triglycerides per ATP III criteria). There was an inverse, but nonsignificant, association with greater breakfast intake (data not presented).
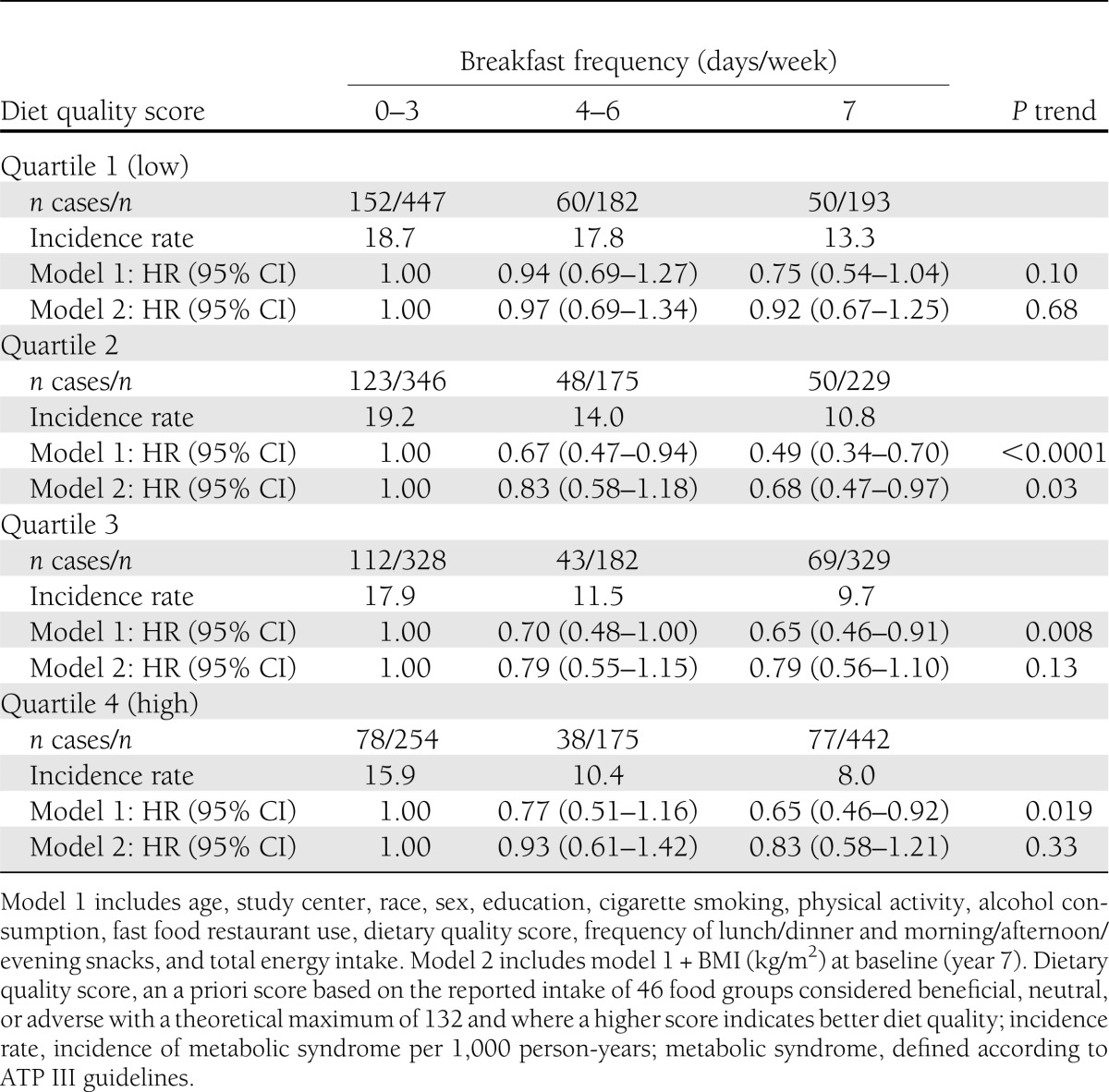
We hypothesized that the association between breakfast intake frequency and metabolic risk may vary by the quality of the overall dietary pattern, i.e., any association may be limited to those with higher relative diet quality. However, we found no evidence in formal tests for interaction or stratified analyses that the relationship between breakfast intake frequency and metabolic risk was differential by overall dietary quality. We present results from the analysis with metabolic syndrome (Table 4) as they are typical of findings for the outcomes examined. We ranked the dietary quality score into quartiles, with the lowest representing the poorest overall quality and the highest representing a theorized best overall dietary pattern. Across quartiles of dietary quality, there was a stepwise decrease in incidence rate of metabolic syndrome with greater breakfast intake frequency. The highest incident rates of metabolic syndrome were observed in infrequent breakfast consumers (0–3 days/week) in the bottom half of overall dietary quality, whereas the lowest incident rates of metabolic syndrome were observed in the daily breakfast eaters in the top half of overall dietary quality. In the main stratified Cox regression model (model 1), there was a graded inverse association with incident metabolic syndrome with more frequent breakfast intake across overall dietary quality; however, the results were only suggestively significant in the lowest quartile of diet quality.
Table 4.
HR and 95% CI of metabolic syndrome according to breakfast frequency by overall dietary quality: CARDIA years 7–25 (1992–1993 to 2010–2011)
We also performed a sensitivity analysis with metabolic syndrome as the outcome exploring the statistical effect of adjustment for common breakfast foods in the study (timing of consumption was not asked). The whole grain breakfast cereal food group was the only breakfast-oriented food to materially alter the point estimates in model 2 with metabolic syndrome as the outcome (HR 0.86 [95% CI 0.72–1.02]) for daily breakfast relative to infrequent breakfast. The refined grain cereals, eggs, sausage/processed meats, fried potatoes, and donuts/pastries/cakes food groups did not materially alter the point estimates.
Of note, breakfast frequency at year 7 displayed an r = 0.46 (P < 0.0001) correlation with breakfast frequency at year 20. Accounting for the year 20 breakfast data significantly depleted the analytic sample (∼42–60% of sample depending on outcome) since any prospective examination between year 20 and 25 exams required data from year 7 and 20, no history of the respective metabolic condition at year 20, and attendance at the year 25 exam. In the sensitivity analyses accounting for the average breakfast intake over time in this subgroup (years 7 and 20), the results did not materially differ from the results presented using the year 7 data. Therefore, we solely present the year 7 data for simplicity.
CONCLUSIONS
In black and white young adult men and women, frequent (4–6 days/week) and daily (7 days/week) breakfast consumption was associated with a decreased risk of developing abdominal obesity, obesity, metabolic syndrome, hypertension, and type 2 diabetes over 18 years of follow-up relative to their peers with infrequent breakfast consumption (0–3 days/week). These findings remained significant for daily breakfast intake for all outcomes except type 2 diabetes after accounting for baseline measures of adiposity. However, the inverse relationship between greater breakfast frequency and type 2 diabetes risk remained independent of BMI in black men and white men and women, whereas in black women, there was no association between breakfast intake and type 2 diabetes incidence. Of note, counter to our hypothesis, the results were not explained by the overall quality of the dietary pattern.
Prospective research examining a range of breakfast intake frequencies with metabolic outcomes is limited. In the only other study to examine a range of breakfast intakes, there was a gradient of BMI change in adolescents across categories of breakfast frequency, with never eaters experiencing the greatest increase and daily eaters experiencing the smallest increase (8). In the Health Professionals Study, breakfast consumers (yes vs. no) had a lower risk of a 5-kg weight gain over 10 years (9). In a tangentially related study, greater intake frequency of both refined and whole grain ready-to-eat cereals was associated in a dose-dependent manner with lower mean weight gain and lower risk of becoming overweight (BMI 25 kg/m2) (10). In a similar examination of Physicians’ Health Study data, there was an inverse association between greater intake of cereal and risk of developing hypertension, although with greater limits in the interpretation due to the dietary assessment (12). In a study of Australian children who were followed up as young adults, those who reported yes at both childhood and young adulthood at a dichotomous assessment of breakfast consumption (yes vs. no) had lower levels of clinical cardiometabolic risk factors relative to those who skipped at different life-course points (14).
Two different studies have examined aspects related to breakfast in relation to type 2 diabetes. In the Health Professionals Study, men who did not eat breakfast (yes vs. no) were at an increased risk of developing type 2 diabetes, and those who had a high Western dietary pattern score and did not eat breakfast experienced an even greater risk of incident type 2 diabetes (13). The Physicians’ Health Study also found that more frequent intake of ready-to-eat cereal, especially whole grain cereal, was inversely associated with risk of incident type 2 diabetes (11). Two other studies have linked aspects of breakfast intake with reduced risk of mortality during their follow-up periods (28,29).
In summary, our study and these other studies all suggest that breakfast intake, or frequent consumption of foods associated with breakfast intake, is important for metabolic health. CARDIA provides a unique and thorough look at the topic with data on the spectrum of possible breakfast intake frequencies as a dietary behavior. This ability to examine the range of breakfast intake uniquely distinguishes it from previous research on the topic and better aligns the data with real-world behavior (8,15,16). Furthermore, the quality of the overall dietary pattern is important for health (16), but this did not explain our results, suggesting that the act of “breaking the fast” may have important metabolic health implications beyond the quality of the overall dietary pattern. The data from the Health Professionals Study also supports this assertion (13).
There are a number of plausible mechanisms whereby eating breakfast may improve acute and long-term factors salient for metabolic risk. As summarized by Timlin and Pereira (6), a spectrum of research provides evidence that the act of eating breakfast, as well as the content, plays important roles in factors related to appetite and hormone, glucose, insulin, and lipid metabolism. Indeed, the time of day and frequency of eating, as well as content, have important independent effects on energy intake, dietary content, and hormonal response that are central to energy balance and thus adiposity (30,31). Greater breakfast intake frequency was strongly and inversely associated with long-term risk of obesity in this study. This appears to be a mechanism by which breakfast intake may reduce risk for metabolic syndrome, type 2 diabetes, and hypertension. Since these estimates were not completely mediated by adiposity in our statistical models, this suggests that breakfast intake impacts other avenues, likely hormonal glucose, insulin, and lipid metabolism factors central to these conditions (32).
A few studies with experimental designs examined the effects of eating breakfast or a larger portion of daily energy intake in the morning on weight loss with some suggestion of benefit, but with mixed results possibly due to study design and sample size (33,34). Other small experimental studies have found that omitting breakfast and the composition of breakfast have effects on appetite and metabolic parameters that could impact long-term metabolic risk (35–37). Further trials have demonstrated that the content of breakfast is likely important for lower metabolic risk as breakfast meals emphasizing low-glycemic whole grains had beneficial effects on appetite and metabolic parameters throughout the day (36,38–40). The sensitivity analysis we performed examining different breakfast-type foods aligns with this point. Overall, the small base of prospective and experimental research on breakfast intake suggests that it may have an independent beneficial role in metabolic health. Prospective population studies examining breakfast habits and larger and longer experimental studies examining specific mechanisms addressing both the act of eating breakfast and the content would provide a more definitive level of evidence on breakfast intake and metabolic health. They would also inform the level of emphasis that should be given to this dietary habit in relevant dietary interventions and overall dietary recommendations.
Our study has a number of strengths: long-term, prospective study design, with high rates of follow-up; standardized, valid, and reliable measurements of dietary practices; extensive clinical measures and data on covariates with which to explore confounders and mediators of the associations under investigation; and the demographics of the cohort, young adult black and white men and women from four U.S. metropolitan areas who have been examined during a period of life when substantial weight gain occurs and metabolic complications develop. Limitations include some level of measurement error with the dietary assessment, although this would most likely result in nondifferential misclassification with respect to any of the outcomes and likely underestimation of risk. The foods explicitly consumed at breakfast were also not assessed in CARDIA. Although a working scientific definition of breakfast has been proposed in the time since CARDIA began (6), there was no explicit definition of what constituted a breakfast meal in the CARDIA study. The self-report of other lifestyle-related data may also result in some misclassification and residual confounding in our models. Because of this, it is possible that the association between daily breakfast intake and significantly reduced metabolic risk is a proxy for an overall better diet and lifestyle.
In conclusion, young adults who reported eating breakfast everyday had a significantly lower risk of an array of metabolic outcomes relative to their peers who infrequently or never ate breakfast, independent of adiposity and the overall quality of the dietary pattern. Our study and other burgeoning evidence (8–14) suggest that the science is catching up to the early nutritional beliefs related to the topic and eating a daily breakfast meal is a dietary habit that may be highly relevant for metabolic health.
Acknowledgments
The CARDIA Study is funded by the CARDIA contract with the National Heart, Lung, and Blood Institute (N01-HC-48047 through N01-HC-48050 and N01-HC-95095). D.S.L. was funded in part by a career grant from the National Institute of Diabetes and Digestive and Kidney Diseases (K24-DK-082730). A.O.O. and M.A.P. were funded in part by a grant from the Bell Institute of Health and Nutrition at General Mills. No other potential conflicts of interest relevant to this article were reported.
A.O.O. designed the analysis, performed the statistical analysis, and wrote the manuscript. D.R.J. and M.A.P. contributed to the design of the analysis, interpreted data, and edited the manuscript. L.M.S., L.V.H., and D.S.L. interpreted data and edited the manuscript. A.O.O. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in abstract form at the 72nd Scientific Sessions of the American Diabetes Association, Philadelphia, Pennsylvania, 8–12 June 2012.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc13-0316/-/DC1.
References
- 1.Lawrence F. Eat Your Heart Out: Why the Food Business Is Bad for the Planet and Your Health. Vol. 1 London, Penguin Books, 2008 [Google Scholar]
- 2.Bernay E, Miller MC. Propaganda Brooklyn, NY, Ig Publishing, 2005 [Google Scholar]
- 3.Tuttle WW, Wilson M, Daum K. Effect of altered breakfast habits on physiologic response. J Appl Physiol 1949;1:545–559 [DOI] [PubMed] [Google Scholar]
- 4.Ingoldsby ME. Be smart—eat a good breakfast. Am J Nurs 1951;51:559–560 [PubMed] [Google Scholar]
- 5.PHYSIOLOGIC results of breakfast habits. Nutr Rev 1957;15:196–198 [DOI] [PubMed] [Google Scholar]
- 6.Timlin MT, Pereira MA. Breakfast frequency and quality in the etiology of adult obesity and chronic diseases. Nutr Rev 2007;65:268–281 [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010 7th Ed. Washington D.C., U.S. Government Printing Office, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics 2008;121:e638–e645 [DOI] [PubMed] [Google Scholar]
- 9.van der Heijden AA, Hu FB, Rimm EB, van Dam RM. A prospective study of breakfast consumption and weight gain among U.S. men. Obesity (Silver Spring) 2007;15:2463–2469 [DOI] [PubMed] [Google Scholar]
- 10.Bazzano LA, Song Y, Bubes V, Good CK, Manson JE, Liu S. Dietary intake of whole and refined grain breakfast cereals and weight gain in men. Obes Res 2005;13:1952–1960 [DOI] [PubMed] [Google Scholar]
- 11.Kochar J, Djoussé L, Gaziano JM. Breakfast cereals and risk of type 2 diabetes in the Physicians’ Health Study I. Obesity (Silver Spring) 2007;15:3039–3044 [DOI] [PubMed] [Google Scholar]
- 12.Kochar J, Gaziano JM, Djoussé L. Breakfast cereals and risk of hypertension in the Physicians’ Health Study I. Clin Nutr 2012;31:89–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mekary RA, Giovannucci E, Willett WC, van Dam RM, Hu FB. Eating patterns and type 2 diabetes risk in men: breakfast omission, eating frequency, and snacking. Am J Clin Nutr 2012;95:1182–1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ. Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr 2010;92:1316–1325 [DOI] [PubMed] [Google Scholar]
- 15.So HK, Nelson EA, Li AM, et al. Breakfast frequency inversely associated with BMI and body fatness in Hong Kong Chinese children aged 9-18 years. Br J Nutr 2011;106:742–751 [DOI] [PubMed] [Google Scholar]
- 16.Sijtsma FP, Meyer KA, Steffen LM, et al. Longitudinal trends in diet and effects of sex, race, and education on dietary quality score change: the Coronary Artery Risk Development in Young Adults study. Am J Clin Nutr 2012;95:580–586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988;41:1105–1116 [DOI] [PubMed] [Google Scholar]
- 18.Bild DE, Jacobs DR, Liu K, et al. Seven-year trends in plasma low-density-lipoprotein-cholesterol in young adults: the CARDIA Study. Ann Epidemiol 1996;6:235–245 [DOI] [PubMed] [Google Scholar]
- 19.Levine DA, Lewis CE, Williams OD, et al. Geographic and demographic variability in 20-year hypertension incidence: the CARDIA study. Hypertension 2011;57:39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith DE, Lewis CE, Caveny JL, Perkins LL, Burke GL, Bild DE. Longitudinal changes in adiposity associated with pregnancy. The CARDIA Study. Coronary Artery Risk Development in Young Adults Study. JAMA 1994;271:1747–1751 [PubMed] [Google Scholar]
- 21.McDonald A, Van Horn L, Slattery M, et al. The CARDIA dietary history: development, implementation, and evaluation. J Am Diet Assoc 1991;91:1104–1112 [PubMed] [Google Scholar]
- 22.Nettleton JA, Steffen LM, Ni H, Liu K, Jacobs DR., Jr Dietary patterns and risk of incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 2008;31:1777–1782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nettleton JA, Schulze MB, Jiang R, Jenny NS, Burke GL, Jacobs DR., Jr A priori-defined dietary patterns and markers of cardiovascular disease risk in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 2008;88:185–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacobs DR, Jr, Sluik D, Rokling-Andersen MH, Anderssen SA, Drevon CA. Association of 1-y changes in diet pattern with cardiovascular disease risk factors and adipokines: results from the 1-y randomized Oslo Diet and Exercise Study. Am J Clin Nutr 2009;89:509–517 [DOI] [PubMed] [Google Scholar]
- 25.Liu K, Slattery M, Jacobs D, Jr, et al. A study of the reliability and comparative validity of the cardia dietary history. Ethn Dis 1994;4:15–27 [PubMed] [Google Scholar]
- 26.Jacobs DR, Jr, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and reliability of a short physical activity history: CARDIA and the Minnesota Heart Health Program. J Cardiopulm Rehabil 1989;9:448–459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–3421 [PubMed] [Google Scholar]
- 28.Breslow L, Breslow N. Health practices and disability: some evidence from Alameda County. Prev Med 1993;22:86–95 [DOI] [PubMed] [Google Scholar]
- 29.Liu S, Sesso HD, Manson JE, Willett WC, Buring JE. Is intake of breakfast cereals related to total and cause-specific mortality in men? Am J Clin Nutr 2003;77:594–599 [DOI] [PubMed] [Google Scholar]
- 30.de Castro JM. The time of day of food intake influences overall intake in humans. J Nutr 2004;134:104–111 [DOI] [PubMed] [Google Scholar]
- 31.Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obes Rev 2007;8:21–34 [DOI] [PubMed] [Google Scholar]
- 32.Leroith D. Pathophysiology of the metabolic syndrome: implications for the cardiometabolic risks associated with type 2 diabetes. Am J Med Sci 2012;343:13–16 [DOI] [PubMed] [Google Scholar]
- 33.Schlundt DG, Hill JO, Sbrocco T, Pope-Cordle J, Sharp T. The role of breakfast in the treatment of obesity: a randomized clinical trial. Am J Clin Nutr 1992;55:645–651 [DOI] [PubMed] [Google Scholar]
- 34.Keim NL, Van Loan MD, Horn WF, Barbieri TF, Mayclin PL. Weight loss is greater with consumption of large morning meals and fat-free mass is preserved with large evening meals in women on a controlled weight reduction regimen. J Nutr 1997;127:75–82 [DOI] [PubMed] [Google Scholar]
- 35.Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr 2005;81:388–396 [DOI] [PubMed] [Google Scholar]
- 36.Pal S, Lim S, Egger G. The effect of a low glycaemic index breakfast on blood glucose, insulin, lipid profiles, blood pressure, body weight, body composition and satiety in obese and overweight individuals: a pilot study. J Am Coll Nutr 2008;27:387–393 [DOI] [PubMed] [Google Scholar]
- 37.Pereira MA, Erickson E, McKee P, et al. Breakfast frequency and quality may affect glycemia and appetite in adults and children. J Nutr 2011;141:163–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barkoukis H, Marchetti CM, Nolan B, Sistrun SN, Krishnan RK, Kirwan JP. A high glycemic meal suppresses the postprandial leptin response in normal healthy adults. Ann Nutr Metab 2007;51:512–518 [DOI] [PubMed] [Google Scholar]
- 39.Nilsson AC, Ostman EM, Granfeldt Y, Björck IM. Effect of cereal test breakfasts differing in glycemic index and content of indigestible carbohydrates on daylong glucose tolerance in healthy subjects. Am J Clin Nutr 2008;87:645–654 [DOI] [PubMed] [Google Scholar]
- 40.Isaksson H, Rakha A, Andersson R, Fredriksson H, Olsson J, Aman P. Rye kernel breakfast increases satiety in the afternoon - an effect of food structure. Nutr J 2011;10:31. [DOI] [PMC free article] [PubMed] [Google Scholar]


