Abstract
OBJECTIVE
To determine whether personality traits (conscientiousness, agreeableness, emotional regulation, extraversion, and openness to experience) are associated with glycemic control and blood glucose monitoring behavior, and change or stability of these outcomes over time, in young people with type 1 diabetes.
RESEARCH DESIGN AND METHODS
A 3-year longitudinal study was conducted using data from 142 individuals with type 1 diabetes, 8–19 years of age. Personality was assessed at baseline using the Five-Factor Personality Inventory for Children. Data relating to glycemic control (HbA1c) and frequency of blood glucose monitoring (based on meter memory) were collected annually. Relationships between personality traits and HbA1c and monitoring frequency were examined using regression models and mixed-design ANOVA.
RESULTS
Three of the Five-Factor domains were independently associated with glycemic control. Individuals high in conscientiousness and agreeableness had a lower and more stable HbA1c across the 3-year study period. In contrast, the HbA1c of individuals scoring low on these traits was either consistently worse or deteriorated over time. Low or high emotional regulation scores were also associated with worse glycemic control. By the third year, these domains, together with initial HbA1c, accounted for 39% of HbA1c variance. Conscientiousness was the only personality factor associated with blood glucose monitoring behavior.
CONCLUSIONS
Results of this study underline the importance of personality in contributing to diabetes outcomes. Attention to a young person’s personality, and appropriate tailoring of diabetes management to ensure an individualized approach, may help to optimize diabetes outcomes.
In Australia, and many other countries, a large proportion of young people with diabetes are not reaching glycemic targets (1–6). This is likely to have life-long consequences. Indeed, those subjects who were randomized to the conventional treatment arm of the Diabetes Control and Complications Trial (7) and who had an average HbA1c of 9.1% during the course of the study continued to develop significantly more micro- and macrovascular complications compared with the intensive group when followed up in the Epidemiology of Diabetes Interventions and Complications study. This occurred despite the rapid convergence of mean HbA1c between the groups at the end of the active study phase (8).
While there are many factors that contribute to suboptimal control, there is mounting evidence that an individual’s personality may play an important role. Several studies in the late 1980s showed that personality traits could account for substantial variability in glycemic control in school-aged children (9,10). However, there has been increasing complexity in treatment regimens since that time. For example, current treatment now involves multiple daily injections or insulin pump therapy. Today, therefore, young people and their families are required to make more complex medical decisions on a daily basis.
The role of personality in these new treatment contexts is not well-understood. Personality can be understood in terms of the Five-Factor model. The Five-Factor model states that there are five broad, independent, and stable dimensions that make up an individual’s personality (11). These factors are termed conscientiousness, agreeableness, emotional regulation, extraversion, and openness to experience. Conscientiousness refers to an individual’s tendency to be reliable, perseverant, and self-disciplined. Agreeableness refers to one’s tendency to be empathetic, considerate, friendly, and helpful. Emotional regulation refers to a person’s capability to regulate their emotional responses to their environment and others. Extraversion refers to an individual’s tendency to be gregarious, assertive, and seek out social situations. Openness refers to one’s tendency to be imaginative, sensitive, and have intellectual curiosity.
Recent work by Vollrath et al. (12) suggests that personality, as measured using the Five-Factor model, influences glycemic control in the first 2 years following diagnosis of type 1 diabetes. In particular, higher levels of conscientiousness and agreeableness appear to have a positive influence on management of blood glucose values, while moderate levels of emotional regulation also appear to be protective (12). Further studies are needed to confirm these relationships between personality and glycemic control and to determine whether this is ameliorated by duration of diabetes. Studies are also needed to examine the role of personality in terms of self-care behavior.
Accordingly, this study was designed to answer two research questions. 1) Are Five-Factor model personality traits associated with a young person’s glycemic control, as measured by HbA1c, and their frequency of self-monitoring of blood glucose (SMBG)? 2) Are these traits associated with change or stability in HbA1c and SMBG over time?
RESEARCH DESIGN AND METHODS
Participants for this project were identified from the Diabetes Research into Adolescent Transitions (DRAT) study. The DRAT project was a 3-year longitudinal project examining the self-management of young people with type 1 diabetes, living in rural and urban areas of New South Wales and the Australian Capital Territory. A total of 158 children and adolescents, 8–19 years of age, together with their families, were recruited into the DRAT study, independent of their source of care. As described elsewhere (1,2), the DRAT study involved three annual visits for which a researcher traveled to interview the young person and their family in their home. At each of these annual visits, participants completed a series of validated questionnaires and underwent a structured interview. Data relating to frequency of blood glucose monitoring were obtained from the memory of blood glucose meters for the preceding 2 weeks. A capillary blood sample was also collected, and HbA1c values were determined by a single laboratory using high-performance liquid chromatography (Bio-Rad, Hercules, CA; upper limit of normal 6.0%).
Collection of personality data were initiated during the first wave of annual visits. DRAT participants were informed about this current study via a regular participant newsletter. Participants who had completed their first annual visit were posted a letter inviting them to be involved in this extension of the DRAT study, along with an information sheet, consent form, and personality data collection tool. To improve return rates, the package was followed up by a telephone call from the researcher who had met with the family at the first annual visit, and a reply paid envelope was included in the package to assist participants in returning completed forms. Other participants were approached directly by researchers during their first annual visit, and personality data were completed at this time. A total of 142 of 158 DRAT participants agreed to take part in the personality study.
Personality data collection tool
Personality data were gathered using the Five-Factor Personality Inventory for Children (FFPI-C). The FFPI-C is a validated, untimed pen-and-paper questionnaire designed to measure personality dimensions of conscientiousness, agreeableness, emotional regulation, extraversion, and openness to experience in children and adolescents from 9 years and 0 months of age to 18 years and 11 months of age (13).
The FFPI-C consists of 75 items (15 items per factor), with each item having two opposing anchor statements aimed at assessing trait variability on the personality dimensions. There are five circles between the anchor statements that allow the participant to choose the statement that best reflects their response (13). Raw scores for the Five-Factor domains were summed and converted to T-scores using the manual provided (13). Baseline (year 1) data showed good internal consistency between items. Cronbach alphas ranged from 0.75 (openness) to 0.88 (conscientiousness).
Statistical analyses
To assess for statistical significance of the relationships between personality traits and outcome measures over time, multivariate regressions using the Five-Factor domains as independent variables and HbA1c or frequency of blood glucose monitoring as dependent variables were conducted for each year of data collection. Pearson product correlations were computed between independent and dependent variables, and coefficients are reported in Supplementary Table 1.
Scores for emotional regulation suggested a curvilinear relationship with glycemic control (HbA1c); therefore, a centered quadratic term for this trait was included in the regression analyses, allowing for linear and quadratic regression models to be compared. If the addition of a quadratic term improved the overall fit of a bivariate regression model, the relationship between the independent and dependent variables was considered to be of curvilinear nature (14–16).
An iterative technique was used for regressions. Control variables of age, sex, duration of diabetes, family responsibility, and interaction terms were entered into hierarchical regressions along with all five of the personality traits. This was done for each matched year of data. After this, significant variables were re-entered into forced-entry regression models. The forced-entry models for the second and third years also included the initial outcome measure from the first year to control for its effects (i.e., HbA1c from year 1 was included in year 2 and year 3 HbA1c regressions, and SMBG from year 1 was included in year 2 and year 3 SMBG regressions). The contribution of personality was calculated as the difference in adjusted R2 between a model including all predictors of HbA1c or SMBG and a second model with personality variables excluded.
To assess longitudinal change, mixed-design ANOVAs were used using high and low baseline groups (upper and lower tertiles) for traits found to be significant predictors of outcomes. Baseline personality traits were used based on the temporal stability of these factors (correlation coefficients r = 0.55–0.84). Three groups (upper, middle, and lower quintiles) were created for analyses of emotional regulation and HBA1c based on the nonlinear relationship that was found.
Ethics
The research protocol used in this project was approved by the University of Western Sydney and the University of Sydney Human Ethics committees, as well as the relevant state area health units.
RESULTS
Patient characteristics
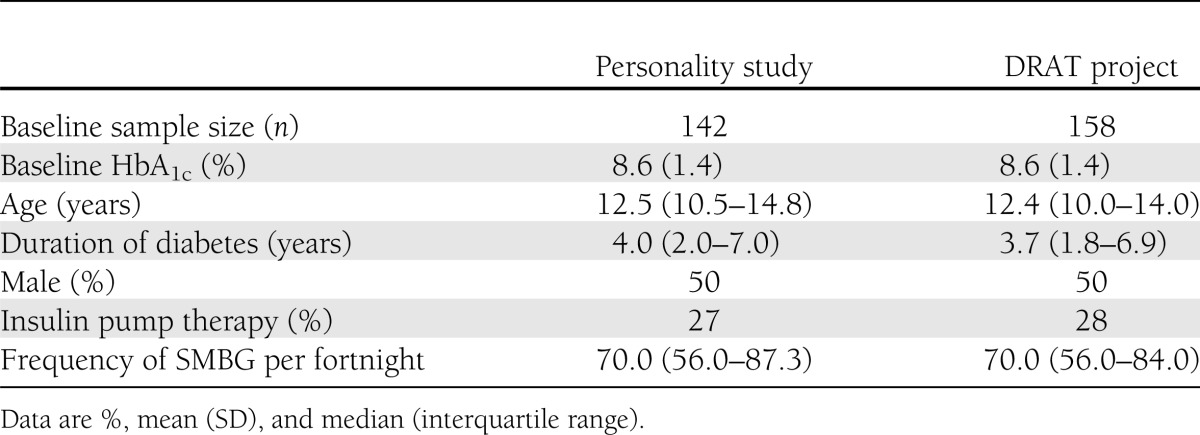
Personality data were gathered from 142 families. Baseline data are shown in Table 1. Overall, glycemic control remained stable over the 3-year study period, with a nonsignificant rise in HbA1c from 8.6% (SD 1.4) in year 1 to 8.8% (SD 1.4) in year 2 and 8.7% (SD 1.3) in year 3.
Table 1.
Baseline characteristics of young people participating in the personality study and DRAT project
Association between personality and glycemic control
Correlations.
Correlations indicated that four of the Five-Factor domains—conscientiousness, agreeableness, emotional regulation, and openness to experience—were associated with HbA1c levels at different points across the 3-year study period (Supplementary Table 1).
Hierarchical regressions.
Hierarchical regressions indicated that conscientiousness, agreeableness, and the centered quadratic term for emotional regulation were significant independent predictors of HbA1c levels. No significant interactions were identified between personality traits and demographic variables. Despite a significant correlation between openness to experience and HbA1c, this personality trait was not an independent predictor of glycemic control.
Forced-entry regressions.
A model including conscientiousness, agreeableness, and the quadratic term for emotional regulation significantly predicted 8% of the variance in HbA1c scores at baseline [R2 = 0.08; F(3,115) = 3.21; P = 0.03]. The quadratic term for emotional regulation was the only significant independent predictor within this model (Table 2).
Table 2.
Standardized β coefficients and R2 in regression models predicting glycemic control (HbA1c) and frequency of SMBG over the 3-year study period
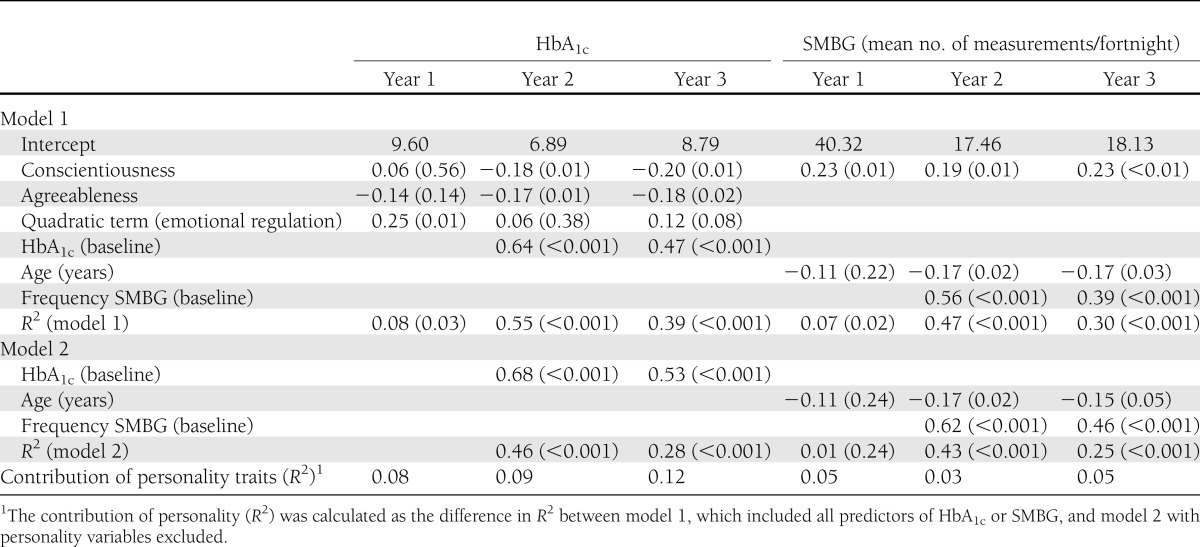
A regression model that included the participants’ HbA1c at baseline together with conscientiousness, agreeableness, and the quadratic term for emotional regulation significantly predicted their second-year HbA1c [R2 = 0.55; F(4,120) = 37.28; P < 0.001]. For this year, conscientiousness and agreeableness were significant independent predictors of glycemic control, whereas the quadratic term for emotional regulation was nonsignificant. The contribution of these personality traits to the overall model was calculated at 9% (Table 2).
Similar results were obtained for the third year of data collection. As shown in Table 2, the full model, including baseline HbA1c, significantly predicted third-year HbA1c [R2 = 0.39; F(4, 126) = 20.49; P < 0.01]. Once again, conscientiousness and agreeableness were the only significant personality trait predictors of glycemic control within this model. In year 3, personality contributed 12% of the variance in HbA1c results.
Factors associated with change in glycemic control
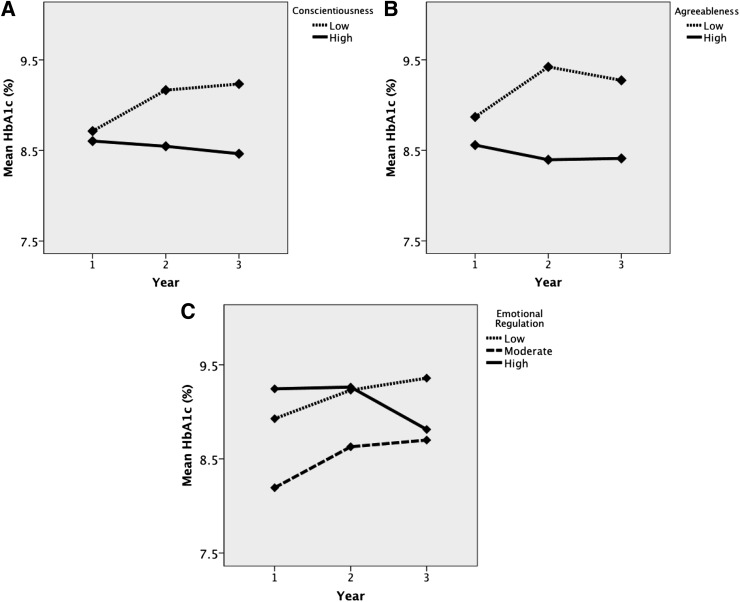
While glycemic control did not change over the study period for the group as a whole [F(2, 278) = 1.34; P = 0.26], there were differences in HbA1c between individuals with high and low levels of conscientiousness [F(1, 100) = 5.09; P = 0.03] and individuals with high and low levels of agreeableness [F(1, 96) = 9.79; P < 0.01].
As shown in Fig. 1A, while HbA1c was similar at entry to the study (year 1), there was an interaction between conscientiousness groups and time [F(2, 200) = 4.48; P = 0.01]. Glycemic control deteriorated over the 3-year study period in individuals in the lowest tertile of conscientiousness [F(2, 98) = 6.10; P < 0.01]. In contrast, no significant changes in HbA1c values were found for the high-conscientiousness group [F(2, 102) = 0.37; P = 0.69].
Figure 1.
Mean HbA1c levels during the 3-year study period, stratified by personality domains. A: Conscientiousness. B: Agreeableness. C: Emotional regulation.
A similar interaction was found between agreeableness group and HbA1c over time [F(2, 192) = 4.91; P < 0.01]. Individuals in the lowest tertile of agreeableness had worsening glycemic control [F(2, 88) = 5.00; P < 0.01], whereas no significant main effect of time on HbA1c values was found for the high-agreeableness group [F(2, 104) = 0.64; P = 0.53].
Since there was a statistically significant curvilinear relationship between emotional regulation and HbA1c, the upper, middle, and lower quintile groups for baseline emotional regulation were compared to examine the role of this trait in long-term glycemic control. There was a significant interaction between emotional regulation and HbA1c scores over time [F(4, 190) = 3.01; P = 0.02]. Between-group differences also approached significance [F(2, 95) = 2.88; P = 0.06].
Within-group analyses indicated no significant changes in glycemic control within the low emotional regulation group [F(2, 56) = 1.80; P = 0.18] or the high emotional regulation group [F(2, 74) = 2.18; P = 0.12]. However, there was significant decline in glycemic control within the moderate emotional regulation group [F(2, 60) = 5.44; P < 0.01]. As seen in Fig. 1C, individuals with low emotional regulation had consistently worse glycemic control across the study period compared with those with moderate emotional regulation, while HbA1c trended down steeply in the final year for those high in emotional regulation.
Association between personality and SMBG
Correlations.
Correlations indicated that conscientiousness, emotional regulation, and agreeableness were associated with blood glucose monitoring at different points across the 3-year study period (Supplementary Table 1).
Hierarchical regressions.
Hierarchical regressions indicated that age and conscientiousness were the only significant independent predictors of blood glucose monitoring. No significant interactions between demographics and personality traits were found.
Forced-entry regressions.
A model including conscientiousness and age significantly predicted 7% of the variance in blood glucose monitoring at baseline [R2= 0.07; F(2, 118) = 4.10; P = 0.02]. A model including baseline number of blood glucose estimations, age, and conscientiousness significantly predicted blood glucose monitoring behavior in the second year; however, the trait of conscientiousness only contributed to 3% of the variance (Table 2). In the third year, a similar model predicted 30% variance in SMBG behavior [R2= 0.30; F(3, 127) = 18.33; P < 0.00], with conscientiousness providing 5% of this contribution.
Older participants monitored less frequently than their younger counterparts, whereas participants who scored high in the domain of conscientiousness consistently performed a higher frequency of blood glucose monitoring (mean number of SMBG in a fortnight: 81.0 [SD 43.7] vs. 66.8 [SD 24.7] in year 1; 79.0 [SD 33.7] vs. 62.4 [SD 22.3] in year 2 and 76.2 [SD 27.7] vs. 58.8 [SD 26.9] in year 3; F(1, 98) = 9.53; P < 0.01).
CONCLUSIONS
The current study suggests that personality traits may be a predictor of how well a young person with type 1 diabetes does over time in terms of glycemic control and self-monitoring behavior. Earlier work of Vollrath et al. (12) showed that high agreeableness and high conscientiousness were associated with better glycemic control in the first 2 years of living with diabetes. These results are replicated in this current study. Moreover, the current study shows that these traits continue to play a role regardless of duration of diabetes. Although the HbA1c of the participants who were high on these two traits in our study was above target, it remained stable over the 3 years.
Of more concern, however, were those participants who were low on conscientiousness and/or agreeableness. In these individuals, glycemic control was either consistently worse or deteriorated over time. Therefore, low scores on these personality traits may be risk factors for poor or worsening glycemic control and confirm that baseline personality scores may have a continuous effect on diabetes management outcomes.
It is intuitive that conscientiousness would also play a role in self-care behavior. Indeed, Skinner et al. (17) showed that conscientiousness, as well as emotional regulation, influenced type 1 diabetes self-management behavior through a mediating effect on a person’s treatment beliefs. More broadly, conscientiousness has been found to be associated with better adoption of health-protective behaviors relating to issues such as tobacco use and physical activity (18). In this current study, those participants with high scores on conscientiousness performed a higher frequency of blood glucose estimations. Importantly, this group continued to show high levels of self-care in relation to monitoring throughout the study period. Conversely, participants with low scores on this trait, as well as older participants, monitored less frequently. The relationship between agreeableness and self-care is less obvious. Although agreeableness was associated with glycemic control, it did not predict self-monitoring behaviors.
Of interest, the work by Vollrath et al. (12) showed that children low on neuroticism (now known as emotional regulation) also had better glycemic control. Emotional regulation refers to a person’s capacity to control their emotional responses to their environment and others, and those scoring low on this factor are prone to be emotionally over reactive and more vulnerable to negative emotional states (19). In contrast to Vollrath et al. (12), our study showed a curvilinear relationship between emotional regulation and glycemic control. Individuals with either low or high scores on this trait had consistently higher HbA1c values across the first 2 years of the study compared with those with moderate scores. There is some prior evidence of a curvilinear relationship between emotional regulation and progression of diabetes complications. A study by Brickman et al. (20) demonstrated that, in adults with diabetes, extreme scores on emotional regulation (either low or high) were related to more rapid deterioration in renal function. The findings of the current study and that of Brickman et al. (20) may be explained by the law of Yerkes and Dodson (21), which states that task performance increases with emotional arousal up to an “optimum point,” beyond which reductions in performance occur. Therefore, people high in emotional regulation may be unconcerned about the long-term effects of poor glycemic control. Those low in emotional regulation are likely to be distressed, and this may influence their ability to look after themselves. Notably, these kinds of relationships are masked when using traditional linear statistical approaches.
The findings of this study are significant, as they underline the importance of personality in determining self-management in young people with type 1 diabetes over time. Personality traits show some continuity from childhood onwards; however, traits are not generally considered to be fixed until 30 years of age (22). Further research is needed to identify the extent to which a young person’s personality can be modified. In the meantime, there may be benefits in clinicians taking personality into account and helping young people manage rather than change their personality. For example, knowing whether a young patient is not particularly conscientious would be helpful in understanding the possible reasons for their poor attention to regular blood glucose monitoring. Focusing on simple strategies to raise behavior-awareness and to improve self-organization, time-management, and planning skills may help to improve blood glucose monitoring behaviors. These strategies may include the use of telephone reminders or providing young people with blood glucose meters with alerts. In contrast, for those who are low on emotional regulation, strategies that focus on reducing stress and anxiety may be of higher priority than using reminders or fostering time-management skills. Similarly, knowledge that a young person is particularly conscientious or emotionally well-regulated would free up precious clinic time to concentrate on other aspects of their care or equally provide a sound basis for engaging this particular attribute to ensure continued good self-management practices. Future studies are needed to examine the potential of personality-based interventions in diabetes care. Research trial interventions that develop, implement, and evaluate health care professionals’ skills in monitoring and fostering attributes of personality and their impact on improving self-management of this group of people are also needed.
It is important to acknowledge the limitations of this study. While this study was the largest of its kind, the results were based on a comparatively small sample of participants. Relative to the sample size, a high number of correlations were performed, increasing the possibility of type I or type II error. However, results of this study are consistent with earlier findings (12,17). The general lack of significant relationships between personality traits and first-year outcomes is intriguing. However, the Five-Factor model variables showed high temporal stability within participants, and further detailed research is needed to understand these findings.
Despite these limitations, the results of this study indicate that personality may be one of the many factors that contribute to less than optimal self-care behaviors and suboptimal glycemic control in young people with type 1 diabetes. Harnessing those personality traits associated with improved outcomes, as well as developing effective methods of working with those traits associated with worse outcomes, may serve to optimize diabetes care.
Acknowledgments
This research was supported by the Australian Research Council Linkage Grant “Children and Adolescents with Type 1 Diabetes: Determining Critical Pathways to Self-Management,” identification number LP0667910, and industry partners the Diabetes Centre, Royal Prince Alfred Hospital, Sydney, Australia, and Novo Nordisk Pharmaceuticals. No other potential conflicts of interest relevant to this article were reported.
D.W. designed the study, collected the data, and conducted statistical analyses. C.J. designed the study, collected the data, and reviewed the manuscript. L.M. provided statistical advice and reviewed the manuscript. L.B.-S. collected and managed the data and edited the manuscript. K.H. collected the data. L.S. and J.O. designed the study, collected the data, and cowrote the manuscript. D.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the young people and their families for participation in this project.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-1743/-/DC1.
References
- 1.Hatherly K, Smith L, Overland J, et al. Glycemic control and type 1 diabetes: the differential impact of model of care and income. Pediatr Diabetes 2011;12:115–119 [DOI] [PubMed] [Google Scholar]
- 2.Hatherly K, Smith L, Overland J, Johnston C, Brown-Singh L. Application of Australian clinical management guidelines: the current state of play in a sample of young people living with type 1 diabetes in the state of New South Wales and the Australian Capital Territory. Diabetes Res Clin Pract 2011;93:379–384 [DOI] [PubMed] [Google Scholar]
- 3.Danne T, Mortensen HB, Hougaard P, et al. Hvidøre Study Group on Childhood Diabetes Persistent differences among centers over 3 years in glycemic control and hypoglycemia in a study of 3,805 children and adolescents with type 1 diabetes from the Hvidøre Study Group. Diabetes Care 2001;24:1342–1347 [DOI] [PubMed] [Google Scholar]
- 4.Holmes CS, Chen R, Streisand R, et al. Predictors of youth diabetes care behaviors and metabolic control: a structural equation modeling approach. J Pediatr Psychol 2006;31:770–784 [DOI] [PubMed] [Google Scholar]
- 5.O’Hagan M, Harvey JN, Brecon Group Glycemic control in children with type 1 diabetes in wales: influence of the pediatric diabetes specialist nurse. Diabetes Care 2010;33:1724–1726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helgeson VS, Siminerio L, Escobar O, Becker D. Predictors of metabolic control among adolescents with diabetes: a 4-year longitudinal study. J Pediatr Psychol 2009;34:254–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med 1993;32:977–986 [DOI] [PubMed] [Google Scholar]
- 8.Epidemiology of Diabetes Interventions and Complications (EDIC) Design, implementation, and preliminary results of a long-term follow-up of the Diabetes Control and Complications Trial cohort. Diabetes Care 1999;22:99–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lane JD, Stabler B, Ross SL, Morris MA, Litton JC, Surwit RS. Psychological predictors of glucose control in patients with IDDM. Diabetes Care 1988;11:798–800 [DOI] [PubMed] [Google Scholar]
- 10.Stabler B, Lane JD, Ross SL, Morris MA, Litton J, Surwit RS. Type A behavior pattern and chronic glycemic control in individuals with IDDM. Diabetes Care 1988;11:361–362 [DOI] [PubMed] [Google Scholar]
- 11.McCrae RR, Costa PT. A five-factor theory of personality. In Handbook of Personality: Theory and Research. Pervin LA, John OP, Eds. New York, Guilford, 1999, p. 139–153 [Google Scholar]
- 12.Vollrath ME, Landolt MA, Gnehm HE, Laimbacher J, Sennhauser FH. Child and parental personality are associated with glycaemic control in type 1 diabetes. Diabet Med 2007;24:1028–1033 [DOI] [PubMed] [Google Scholar]
- 13.McGhee RL, Ehrler DJ, Buckhalt JA. Five-Factor Personality Inventory-Children: Examiners Manual. Austin, Pro-Ed, 2007 [Google Scholar]
- 14.Keeley J, Zayac R, Correia C. Curvilinear relationships between statistics anxiety and performance among undergraduate students: evidence for optimal anxiety. Stat Educ Res J 2008;7:4–15 [Google Scholar]
- 15.Keith TZ. Multiple Regression and Beyond. New York, Pearson, 2006 [Google Scholar]
- 16.Mallery P. SPSS for Windows Step by Step: A Simple Guide and Reference 16.0 update. 9th ed. New York, Pearson, 2009 [Google Scholar]
- 17.Skinner TC, Hampson SE, Fife-Schaw C. Personality, personal model beliefs, and self-care in adolescents and young adults with type 1 diabetes. Health Psychol 2002;21:61–70 [PubMed] [Google Scholar]
- 18.Bogg T, Roberts BW. Conscientiousness and health-related behaviours: a meta-analysis of the leading behavioral contributors to mortality. Psychol Bull 2004;130:887–919 [DOI] [PubMed] [Google Scholar]
- 19.Digman JM. Personality structure: emergence of the five-factor model. Annu Rev Psychol 1990;41:417–440 [Google Scholar]
- 20.Brickman AL, Yount SE, Blaney NT, Rothberg ST, De-Nour AK. Personality traits and long-term health status. The influence of neuroticism and conscientiousness on renal deterioration in type-1 diabetes. Psychosomatics 1996;37:459–468 [DOI] [PubMed] [Google Scholar]
- 21.Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comp Neurol Psychol 1908;18:459–482 [Google Scholar]
- 22.McCrae RR, Costa PT., Jr The stability of personality: observations and evaluations. Curr Dir Psychol Sci 1994;3:173–175 [Google Scholar]