Abstract
OBJECTIVES
Few educational opportunities exist in paediatric cardiac critical care units (PCCUs). We introduced a new educational activity in the PCCU in the form of of patient-specific summaries (TPSS). Our objective was to study the role of TPSS in the provision of a positive learning experience to the multidisciplinary clinical team of PCCUs and in improving patient-related clinical outcomes in the PCCU.
METHODS
Prospective educational intervention with simultaneous clinical assessment was undertaken in PCCU in an academic children's hospital. TPSS was developed utilizing the case presentation format for upcoming week's surgical cases and delivered once every week to each PCCU clinical team member. Role of TPSS to provide clinical education was assessed using five-point Likert-style scale responses in an anonymous survey 1 year after TPSS provision. Paediatric cardiac surgery patients admitted to the PCCU were evaluated for postoperative outcomes for TPSS provision period of 1 year and compared with a preintervention period of 1 year.
RESULTS
TPSS was delivered to 259 clinical team members including faculty, fellows, residents, nurse practitioners, nurses, respiratory therapists and others from the Divisions of Anesthesia, Cardiology, Cardio-Thoracic Surgery, Critical Care, and Pediatrics working in the PCCU. Two hundred and twenty-four (86%) members responded to the survey and assessed the role of TPSS in providing clinical education to be excellent based on mean Likert-style scores of 4.32 ± 0.71 in survey responses. Seven hundred patients were studied for the two time periods and there were no differences in patient demographics, complexity of cardiac defect and surgical details. The length of mechanical ventilation for the TPSS period (57.08 ± 141.44 h) was significantly less when compared with preintervention period (117.39 ± 433.81 h) (P < 0.001) with no differences in length of PCICU stay, hospital stay and mortality for the two time periods.
CONCLUSIONS
Provision of TPSS in a paediatric cardiac surgery unit is perceived to be beneficial in providing clinical education to multidisciplinary clinical teams and may be associated with improved clinical outcome.
Keywords: Education, all levels; Health provider; Postoperative care; Outcomes; Paediatric; Congenital heart disease
INTRODUCTION
The survival and outcomes of children after surgical repair continue to improve in the field of congenital heart disease [1]. Sub-specialized units like paediatric cardiac critical care units (PCCUs) have evolved to take care of sick children with heart diseases that address age variations, range of cardiac defects, increased exposure to newer surgical techniques and paediatric-size devices [2]. The preview and treatment of these complex patients are traditionally discussed in cardiac catheterization conferences that have limitations of time, audience attendance and variability in discussion of patient management [3, 4]. Scheduling constraints hinder the attendance of a large proportion of PCCU clinical team members at these conferences.
A multidisciplinary team of care providers belonging to different specialties and subspecialties works together in PCCU [1]. The large and diverse clinical team comprises care providers with multiple levels of medical training, variable sophistication of medical knowledge, and different scheduling patterns. The delivery of high- quality health care in these units depends on developing good communication skills, interdisciplinary collaboration, evidence-based medicine, tools to manage knowledge and shared decision making [5]. We are not aware of published literature regarding patient-specific summaries in PCCU that are directed towards enhancing the confidence and competence of the entire clinical team working in the PCCU to improve the quality of medical care they provide [6–8]. We developed a standardized template of patient-specific summaries (TPSS) that was easy to understand for the diverse multidisciplinary team of care providers working in our PCCU. We hypothesized that the standardized template disseminated every week would be beneficial to the PCCU clinical team to improve their clinical education as measured by responses to an anonymous survey and would be associated with improved clinical outcomes of patients admitted to the PCCU.
METHODS
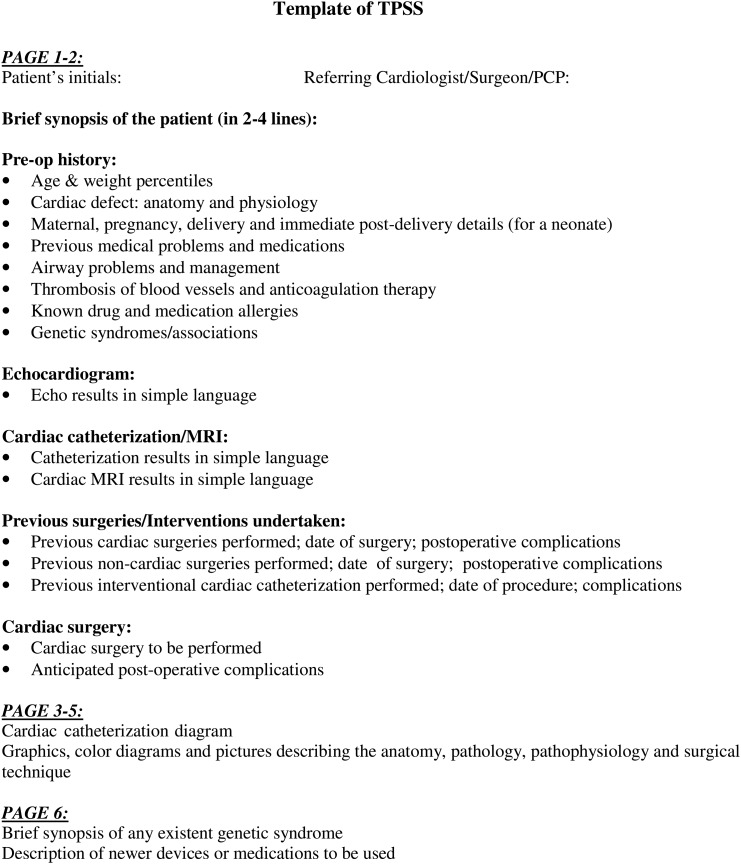
This study was undertaken in the Pediatric Heart Institute at the Monroe Carell Jr. Children's Hospital at Vanderbilt. The Institutional Review Board reviewed and approved the study. The TPSS were prepared for the upcoming week's surgical cases and distributed once every week to each member of the clinical team working in the PCCU (Supplementary data). The clinical team members included faculty, fellows, residents, nursing staff, nurse practitioners, perfusionists, extracorporeal membrane oxygenation (ECMO) technicians, respiratory therapists, nurse anesthetists and others from the Divisions of Anesthesia, Cardiology, Cardio-Thoracic Surgery, Critical Care, and Pediatrics working in the PCCU. The TPSS were based on a case presentation format of children with cardiac lesions undergoing cardiac surgery (Fig. 1). The TPSS included specific sections that addressed the anatomy and pathophysiology of the cardiac defect, cardiac and non-cardiac-related health problems and the anticipated surgical procedure to be performed. The section on cardiac defect displayed colour diagrams, pictures, flow charts, echocardiograph, cardiac magnetic resonance images and cardiac catheterization diagrams to describe the anatomy and pathophysiology of the patient's lesions. The cardiac imaging findings were stated in simple non-technical terminology. The section on health problems focused on the patient's physical growth and nutrition, antenatal, delivery and newborn details for neonates, major medical health problems, difficult airway management, thrombosis of major blood vessels and anticoagulation therapy and any known drug allergies. The cardiac surgical section described the anticipated surgical procedure and the potential postoperative complications. This section also highlighted details of previous surgical procedures including cardiac catheterization and associated postoperative complications. A separate section described newer devices, newer medications or uncommon genetic syndromes. A PCCU critical care faculty member was responsible for the production of TPSS each week. The patient's electronic medical records, paediatric cardiac surgery, cardiology and critical care textbooks, published journal articles and internet media were resourced to prepare the TPSS. An average of 6–8 patients was included in each template and ∼30 min were required per patient to prepare their template. An electronic version of the TPSS was distributed via e-mail to each clinical team member and a hard copy was provided in the PCCU every week. The TPSS was utilized in the PCCU every day for interactive discussions on the postoperative management of the patients. Each month, additions and departures of clinical team members from the PCCU were evaluated to ensure timely delivery of the TPSS to all active members of the team.
Figure 1:
Template design used for preparation of templates of patient-specific summaries (TPSS) for each anticipated cardiac surgery patient admitted to the paediatric critical care unit for postoperative care.
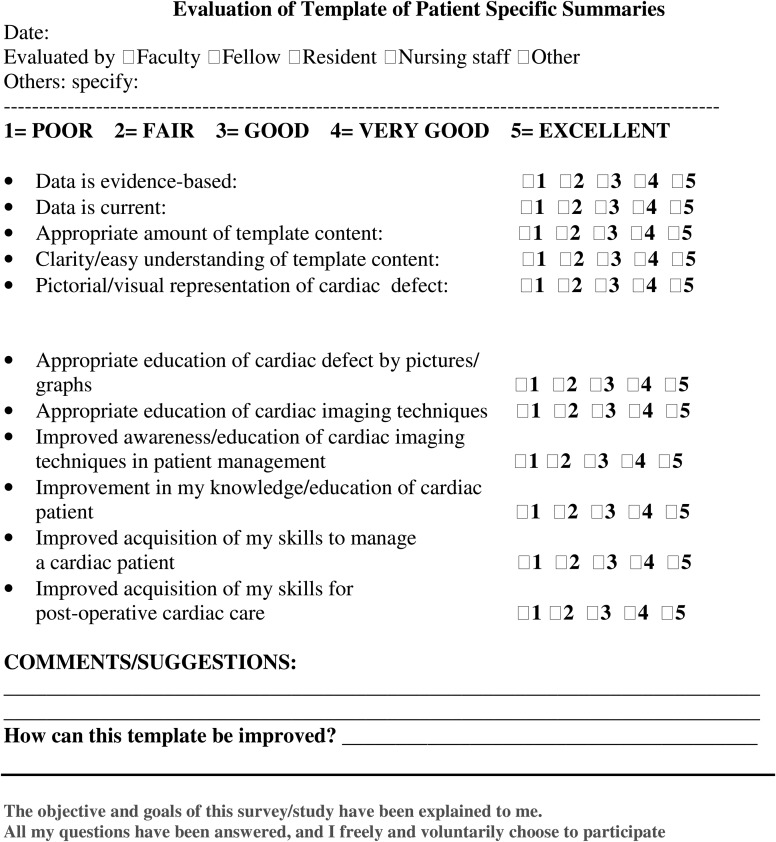
An anonymous survey independently developed by the Hospital Performance Management and Improvement Group evaluated the quality and role of TPSS in providing clinical education to the medical team of PCCU (Fig. 2). The survey was administered to the entire clinical team of PCCU at the end of 1 year of TPSS provision. The survey assessed the quality of the TPSS based on responses to questions into five domains: evidence-base, literature quality, simplicity of template content, visual and pictorial quality and adequacy of template content. The survey assessed the role of TPSS in providing clinical education based on responses to six questions. The six questions assessed whether the TPSS enhanced team member's knowledge of patients with cardiac disease, anatomy of different cardiac defects and cardiac imaging techniques; whether the template changed their attitude about the role of cardiac imaging and if the template facilitated acquisition of skills leading to improvement in managing cardiac patients and making postoperative cardiac care more efficient. The clinical team was asked to respond to each question on a standard Likert-style scale (1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent). The participation in the survey was voluntary, and each care provider was deidentified at submission of responses. The response rate for the survey was analysed based on the number of clinical team members that responded and completed the survey. The clinical team members were distributed into five groups: faculty, fellows, residents, nurses and ‘others’ to test for statistical difference in their responses. ‘Others’ included nurse practitioners, ECMO technicians, respiratory therapists, nurse anesthetists, perfusionists, medical students and scrub technicians. For each sub-category of responses to questions, a mean value was calculated for each response across all items pertaining to that category. A Cronbach's alpha was applied to measure internal consistency across survey items within a given sub-category of response. A Kruskal–Wallis test was applied to compare the distribution of each response across the five different groups simultaneously.
Figure 2:
Survey questions to assess quality and value of the templates of patient-specific summaries (TPSS).
The clinical outcomes of all cardiac surgery patients admitted for postoperative care to the PCCU were evaluated for the entire year (2008) the TPSS were introduced in the PCCU and compared with the preceding year (2007) that lacked the TPSS. Patient variables including age (days), weight (kg), height (cm), gender, cardiopulmonary bypass time (min), cross-clamp time (min) and complexity of cardiac surgery based on Risk Adjusted Classification for Congenital Heart Surgery, Version 1 [9] were studied. Clinical outcomes including the length of mechanical ventilation (h), length of PCCU stay (days), length of hospital stay (days) and mortality were studied for both the time periods. Mortality was defined as death within the first 30 postoperative days or during the entire hospital stay if hospitalization exceeded 30 days. The patient data and clinical outcomes were acquired from the electronic medical records of the institution. A Wilcoxon rank-sum test was used to analyse clinical outcomes including the length of mechanical ventilation, length of PCCU stay and length of hospital stay. A χ2 test was used to analyse mortality rates between the preintervention and intervention periods.
RESULTS
The templated patient-specific summaries were distributed to 259 clinical team members in the PCCU over the 1-year period. When surveyed, 224 clinical team members responded for a response rate of 86%. Thirty of the 32 faculties (94%), 19 of 19 fellows (100%), 42 of 49 residents (86%), 82 of 94 nursing staff (87%) and 51 of 55 others (93%) responded to the survey.
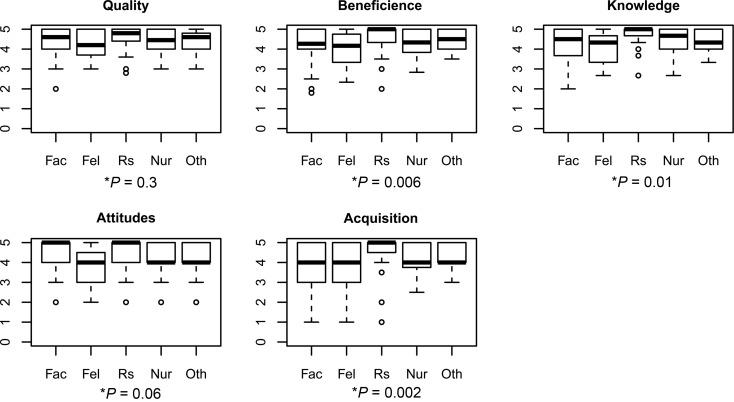
The PCCU clinical team members' responses to the survey questions are given in Table 1. The clinical team responded with a mean Likert-style score of 4.41 ± 0.63 (maximum score of 5) when assessing the quality of the summaries. A Cronbach's alpha of 0.93 (maximum of 1) demonstrated a high degree of internal consistency within the responses to five questions assessing the quality of the TPSS. There was no statistically significant difference in the response pattern of the five categories of care providers (P = 0.3). The clinical team responded with a mean Likert-style score of 4.32 ± 0.71 when assessing the role of TPSS in providing clinical education. A Cronbach's alpha of 0.93 demonstrated a high degree of internal consistency within the responses to six questions assessing the value of TPSS. The Kruskal–Wallis test comparing the distribution of responses among the five clinical groups simultaneously revealed that resident physicians demonstrated the greatest benefit from the educational program (P < 0.01) (Fig. 3).
Table 1:
Survey responses for the template of patient-specific summaries (TPSS) by the paediatric critical care unit clinical team members
| Questions in the survey | Faculty (n = 30) | Fellows (n = 19) | Residents (n = 42) | Nurses (n = 82) | Others (n = 49) | P-value |
|---|---|---|---|---|---|---|
| Quality of template | 4.4 ± 0.7 | 4.2 ± 0.9 | 4.6 ± 0.6 | 4.4 ± 0.6 | 4.4 ± 0.5 | 0.3 |
| Educational value of template | 4.1 ± 0.9 | 4.0 ± 0.9 | 4.6 ± 0.6 | 4.3 ± 0.7 | 4.4 ± 0.5 | 0.006 |
| Enhancement of knowledge | 4.2 ± 0.9 | 4.1 ± 0.8 | 4.7 ± 0.5 | 4.4 ± 0.7 | 4.5 ± 0.5 | 0.01 |
| Change in attitudes | 4.4 ± 0.8 | 3.9 ± 0.9 | 4.4 ± 0.9 | 4.1 ± 1.0 | 4.3 ± 0.8 | 0.06 |
| Acquisition of clinical skills | 3.9 ± 1.2 | 3.8 ± 1.2 | 4.6 ± 0.8 | 4.2 ± 0.8 | 4.3 ± 0.6 | 0.002 |
Response values represent Likert scale response (1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent) shown as mean ± SD; P-value based on Kruskal–Wallis test.
Figure 3:
Box plot of survey responses of clinical team members of the paediatric cardiac critical care unit (PCCU) to the templates of patient-specific summaries (TPSS). Fac: faculty; Fel: fellow; Rs: residents; Nur: nurses; Oth: others *Krushal–Wallis P-value for overall test of differences between different categories of clinical team members.
The patient characteristics for the cardiac surgery patients admitted to the PCCU for postoperative management for the preintervention and intervention periods are given in Table 2. There was no significant difference in any of the variables studied for these time periods. The clinical outcomes of these patients for the preintervention and intervention periods are given in Table 3. There was a statistically significant reduction (P < 0.001) in the length of mechanical ventilation for patients during the intervention period when compared with the preintervention period.
Table 2:
Patient demographics for the preintervention and intervention (TPSS) periods
| Patient characteristics | Preintervention period (2007) | Intervention period (2008) | P-value |
|---|---|---|---|
| Total number of patients | 379 | 321 | |
| Age (days)a | 191 (63.5, 1073.5) | 174 (17, 1017) | 0.44c |
| Weight (kg)a | 6.15 (3.9, 13.2) | 6.15 (3.5, 12.5) | 0.52c |
| Height (cm)a | 64 (54.8, 92.5) | 64 (53, 91) | 0.57c |
| Gender | |||
| Maleb | 200 (58%) | 180 (56%) | 0.42d |
| Femaleb | 179 (42%) | 141 (44%) | |
| CPB time (min)a | 105 (61, 155) | 106 (66, 146) | 0.87c |
| Xct time (min)a | 37 (15, 61) | 36 (13, 56) | 0.4c |
| RACHS-1 | |||
| 1b | 47 (12%) | 31 (10%) | 0.33d |
| 2b | 135 (36%) | 117 (36%) | |
| 3b | 104 (27%) | 94 (29%) | |
| 4b | 35 (9%) | 25 (8%) | |
| 5–6b | 25 (7%) | 33 (10%) | |
| Unrankableb | 33 (11%) | 21 (7%) | |
CPB: cardiopulmonary bypass time; Xct: cross-clamp time; RACHS: complexity of cardiac surgery based on Risk Adjusted Classification for Congenital Heart Surgery; TPSS: templates of patient-specific summaries.
aValues as number (%).
bValues as median (IQR).
cP-value based on Wilcoxon rank-sum test.
dP-value based on χ2 test.
Table 3:
Clinical outcomes of postoperative paediatric cardiac surgery patients admitted to the PCCU for the preintervention and intervention (TPSS) periods
| Clinical outcomes | Preintervention period (2007) | Intervention period (2008) | P-value |
|---|---|---|---|
| Length on mechanical ventilation (h)a | 22 (12, 80) | 18 (7, 50) | <0.001c |
| Length of PCCU stay (days)a | 3 (1, 7) | 3 (2, 6) | 0.85c |
| Length of hospital stay (days)a | 7 (4, 12) | 7 (5, 15) | 0.32c |
| Deathb | 24 (6.3%) | 24 (7.4%) | 0.78d |
PCCU: paediatric cardiac critical care unit; TPSS: templates of patient-specific summaries.
aValues as median (IQR).
bValues as number (%).
cP-value based on Wilcoxon rank-sum test.
dP-value based on χ2 test.
DISCUSSION
Our study reveals that provision of TPSS in a PCCU is perceived to be beneficial in providing clinical education to the entire clinical team. Simultaneously, the provision of these summaries is associated with a reduction in the duration of mechanical ventilation for the postoperative cardiac surgery patients admitted to the critical care unit.
In paediatric cardiac surgery, the patient's intensive care management begins with their initial presentation at the clinic, conventional hospitalization or even the initial multidisciplinary discussion rather than with postoperative care [10]. Postoperative management in the PCCU requires a multidisciplinary collaboration between physicians (surgeon, cardiologist, intensivist, anesthesiologist and neonatologist) and other clinical disciplines, including nursing, advanced nurse practitioners, respiratory therapy, pharmacology and nutrition support [11]. Clinical education of every team member of the PCCU is vital for delivery of high-quality health care [10]. There is a limited learning opportunity in meetings and forums to discuss and understand the complex congenital heart defects. Development of specialized intensive care units and duty hour restrictions limit the active involvement of resident physicians in the management of children with complex congenital heart disease [6]. Lack of availability of residents, clinical workload and limited protected time put further constraints to their education in the intensive care unit [12]. The knowledge base of clinical fellows rotating in the PCCU from Divisions of Pediatric Critical Care, Cardiology, Cardio-Thoracic Surgery and Anesthesia is limited to their field of expertise [6]. Education is imparted to the PCCU fellows intermittently rather than as a daily, continuous learning process [6]. Much less is known about the knowledge base and educational opportunities of other health care providers in PCCU. In our study, TPSS were consistently delivered every week in a timely fashion in a standardized and easy-to-read format to every team member of the PCCU. The TPSS facilitated clinical education by helping each team member to understand their patient's cardiac defect, cardiac imaging, cardiac surgery, and anticipated postoperative problems in addition to their medical problems. We believe that weekly provision of TPSS and its active use by the clinical team for interactive discussions followed several principles of successful adult education, including being learner-based and relevant to learners’ needs, and possessing engagement and reinforcement that led to its validation in an independent and anonymous survey in our study [13, 14].
The delivery of medical care in specialized critical care units like PCCU is based on a multidisciplinary team approach rather than hierarchal systems and is associated with less demarcation of responsibilities and coupled with increased levels of communication among team members [10]. Clinical decisions in patient management in our PCCU are initiated by the critical care faculty in active conjunction with the multidisciplinary team comprising bedside nurse, clinical nurse practitioners, respiratory therapists, residents, fellows and faculty from pediatric cardiology and cardio-thoracic surgery. Provision of standardized learning experience from the TPSS to each and every team member in the PCCU enhanced the knowledge base of the cardiac defect and the anticipated postoperative complications and course of their primary patient. The increased levels of confidence and knowledge of every team member facilitated their active involvement in clinical decision making in the postoperative patient management. The TPSS was actively used in the PCCU during the daily multidisciplinary morning and evening rounds as well as during the nursing, resident and fellow physicians shift handovers. Provision of TPSS thus facilitated the integration of multidisciplinary PCCU team in clinical management that is vital for improving communication and outcomes in intensive care units [15]. Failure of communication remains one of the major human-based factors contributing to the occurrence of adverse events [16]. We believe that sustained and consistent provision of knowledge through TPSS improved the levels of clinical education and communication among PCCU team members that played an important role in improving clinical outcomes during the study period.
Our study has several limitations. The study was conducted at a single institution and external validity has not been assessed. The survey assessed the perception of learner's knowledge and skills acquisition; however, no other formal testing was undertaken to assess the same. The survey questions did not address inter-personnel communication, although we believe that a decrease in the communication barrier among the clinical team members from different subspecialties working in the PCCU was partly responsible for improved clinical outcomes. The time period of TPSS provision was associated with a significant reduction of duration of mechanical ventilation; however, we did not see a reduction in the length of PCCU stay or hospital stay between the preintervention and intervention time periods. The duration of PCCU and hospital stay is dependent on institution practices and social issues, including the establishment of feeding patterns in neonatal patients. Besides, early extubation after paediatric cardiac surgery has not been found to be associated with significant reduction in PCCU and hospital length of stay [17]. Our survey results revealed that residents benefitted maximally from TPSS; however, with the increasing complexity of cardiac patients and high turnover of multidisciplinary clinical team members, it would be best to provide TPSS to each and every member of the paediatric heart institution. The lack of provision of TPSS to the cardiology floor clinical team in our study may have been partly responsible for the lack of reduction of hospital stay in the intervention period. A number of unmeasured confounder variables between the intervention and preintervention periods may have been responsible for the observed differences in clinical outcome. During the time period of TPSS provision, there were no major changes in the structure or staffing turnover in the Divisions of Anesthesia, Cardiac Surgery, Cardiology, or Critical Care that work in the PCCU (data not shown). Likewise, none of these divisions were simultaneously conducting new protocols or policies that were intended to facilitate earlier extubation. Preparation of TPSS is laborious and time consuming. Paediatric heart institutions need to realize the value of this education tool and provide protected time for personals responsible for preparation and provision of TPSS. Currently, a simplified version of TPSS is prepared by the Clinical Nurse Educator and provided in our PCCU. Finally, our study design was quasiexperimental (pre-/post-study design) in nature and only a carefully designed randomized study with appropriate controls can confirm this association with confidence. This study design, however, is often undertaken as a result of the difficulty in finding an applicable control group and the ethical concerns about randomization in a quality improvement study [18].
Despite these limitations, our study demonstrates that provision of TPSS to a multidisciplinary, multispecialty clinical team working in a PCCU is perceived to be beneficial in providing clinical education. As the survival after surgical repair of congenital heart disease continues to improve, postoperative outcomes in paediatric cardiac surgery are being measured by the duration of mechanical ventilation, and length of stay in the intensive care unit and the hospital [19, 20]. The provision of TPSS in our study is clinically associated with a reduction in the length of the mechanical ventilation of postoperative paediatric cardiac surgery patients admitted in our PCCU. Further work needs to be undertaken to reproduce similar beneficial effects in other cardiac critical care units.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Conflict of interest: none declared.
REFERENCES
- 1.Chang AC. Pediatric cardiac intensive care: current state of the art and beyond the millennium. Curr Opin Pediatr. 2000;12:238–46. doi: 10.1097/00008480-200006000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Varma A. Pediatric cardiac intensive care units. The way forward. Ann Pediatr Cardiol. 2011;4:127–8. doi: 10.4103/0974-2069.84649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beller GA, Bonow RO, Fuster V. ACCF 2008 Recommendations for training in adult cardiovascular medicine core cardiology training (COCATS 3) (Revision of the 2002 COCATS training statement) J Am Coll Cardiol. 2008;51:335–8. doi: 10.1016/j.jacc.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 4.Mathewson JW. Building a pediatric cardiac catheterization laboratory and conference room: design considerations and filmless imaging. Pediatr Cardiol. 1996;17:279–94. doi: 10.1007/s002469900064. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 6.Su L, Munoz R. Isn't it the right time to address impact of pediatric cardiac intensive care units on medical education? Pediatrics. 2007;120:e1117–1119. doi: 10.1542/peds.2006-2487. [DOI] [PubMed] [Google Scholar]
- 7.Dimitroff A, Davis WK. Content analysis of research in undergraduate medical education. Acad Med. 1996;71:61–7. doi: 10.1097/00001888-199601000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Prystowsky JB, Bordage G. An outcomes research perspective on medical education: the predominance of trainee assessment and satisfaction. Med Educ. 2001;35:331–6. doi: 10.1046/j.1365-2923.2001.00910.x. [DOI] [PubMed] [Google Scholar]
- 9.Jenkins KJ. Risk adjustment for congenital heart surgery: the RACHS-1 method. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2004;7:180–4. doi: 10.1053/j.pcsu.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 10.Fraisse A, Le Bel S, Mass B, Macrae D. Pediatric cardiac intensive care unit: current setting and organization in 2010. Arch Cardiovasc Dis. 2010;10:546–51. doi: 10.1016/j.acvd.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Baden HP, Berger J, Brilli RI, Burns JP, Checchia PA, Dalton HJ, et al. Pediatric cardiac critical care patients should be cared for by intensivists. J Am Coll Cardiol. 2006;48:221–2. doi: 10.1016/j.jacc.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 12.Chudgar SM, Cox CE, Que LG, Andolsek K, Knudsen NW, Clay AS. Current teaching and evaluation methods in critical care medicine: has the Accreditation Council for Graduate Medical Education affected how we practice and teach in the intensive care unit? Crit Care Med. 2009;37:49–60. doi: 10.1097/CCM.0b013e31819265c8. [DOI] [PubMed] [Google Scholar]
- 13.Knowles MS. The Modern Practice of Adult Education: Andragogy versus Pedagogy. New York, NY: New York Association Press; 1970. [Google Scholar]
- 14.Candy PC. Self-direction for Lifelong Learning: A Comprehensive Guide to Theory and Practice. San Francisco, CA: Jossey-Bass Publishers; 1991. [Google Scholar]
- 15.Jain M, Miller D, Belt D, King D, Berwick DM. Decline in ICU adverse events, nosocomial infections and cost through a quality improvement initiative focusing on teamwork and culture change. Qual Saf Health Care. 2006;15:235–9. doi: 10.1136/qshc.2005.016576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348:2526–34. doi: 10.1056/NEJMsa020847. [DOI] [PubMed] [Google Scholar]
- 17.Alghamdi AA, Singh SK, Hamilton BC, Yadava M, Holtby H, Van Arsdell GS. Early extubation after pediatric cardiac surgery: systematic review, meta-analysis, and evidence-based recommendations. J Card Surg. 2010;25:586–95. doi: 10.1111/j.1540-8191.2010.01088.x. [DOI] [PubMed] [Google Scholar]
- 18.Black MD, Schorr C, Levy MM. Knowledge translation and the multifaceted intervention in the intensive care unit. Crit Care Med. 2012;40:1324–8. doi: 10.1097/CCM.0b013e3182431673. [DOI] [PubMed] [Google Scholar]
- 19.Clarke DR, Lacour-Gayet F, Jacobs JP, Jacobs ML, Maruszewski B, Pizarro C, et al. The assessment of complexity in congenital cardiac surgery based on objective data. Cardiol Young. 2008;18(Suppl2):169–76. doi: 10.1017/S1047951108002850. [DOI] [PubMed] [Google Scholar]
- 20.Heinrichs J, Sinzobahamvya N, Arenz C, Kallikourdis A, Photiadis J, Schindler E, et al. Surgical management of congenital heart disease: evaluation according to the Aristotle score. Eur J Cardiothorac Surg. 2010;37:210–7. doi: 10.1016/j.ejcts.2009.06.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.