Abstract
The menisci are two semilunar-shaped fibrocartilagenous structures, which are interposed between the femoral condyles and tibial plateaux. They have an important role in knee function. Long-term follow-up studies showed that virtually all meniscectomized knees develop arthritic changes with time. The meniscus has functions in load bearing, load transmission, shock absorption, joint stability, joint lubrication, and joint congruity. Because of these functions, meniscal tissue should be preserved whenever possible. A well-trained surgeon can safely rely on clinical examination for diagnosing meniscal injuries. History and clinical examination are at least as accurate as magnetic resonance imaging in the skilled orthopedic surgeon’s hand. When meniscal repair is not possible, partial resection of the meniscus is indicated. Meniscal repair has evolved from open to arthroscopic techniques, which include the inside-out and outside-in suture repairs and the all-inside techniques. Meniscal transplantation is generally accepted as a management alternative option for selected symptomatic patients with previous complete or near-complete meniscectomy.
Keywords: meniscus, arthroscopy, meniscectomy, meniscal repair, sports
Introduction
Anatomy
The menisci are two semilunar-shaped fibrocartilagenous structures, which are interposed between the femoral condyles and tibial plateaux.1 Menisci are composed by a tridimensional complex containing water, collagen (mainly type I), and proteoglycans. Their unique anatomy is comprised of circumferentially oriented collagen fibers which provide resistance to hoop stresses and radially oriented fibers which resist shear forces.2 The lateral meniscus is C-shaped with a short distance between its anterior and posterior horns. The medial meniscus is U-shaped with larger separation of the two horns. The menisci cross-sectional area is triangular, with the tapered edge directed centrally.
The diameter of the menisci measure about 35 mm and are fixed to the joint capsule by their convex-shaped peripheral margin, which has a length of 110 mm.3 The anterior and posterior meniscal horns are firmly attached to bone through insertional ligaments. In each meniscus it is possible to identify a meniscal body (including the horns), the anterior and posterior insertional ligaments and their attachment to bone, called meniscal entheses.
While at birth the whole meniscus is vascularized,4 it is mostly avascular in adults. After the second decade only the peripheral margin is vascularized, with a limited blood supply arising from a perimeniscal capillary plexus.5
The load distributing function of the menisci is largely determined by the attachment to bone at the anterior and posterior enthuses.6,7 The medial meniscus inserts to the tibial plateau at the anterior intercondylar fossa about 6–7 mm anterior to the anterior cruciate ligament insertion by means of a fat fan-shaped structure, the anterior insertional ligament.8,9
The posterior insertional ligament of the medial meniscus attaches to the posterior intercondylar fossa of the tibia between the posterior enthesis of the lateral meniscus and the tibial insertion of the posterior cruciate ligament. The anterior insertional ligament of the lateral meniscus attaches to the anterior intercondylar fossa of the tibia, anterior to the lateral intercondylar tuberulum, just behind the tibial enthesis of the anterior cruciate ligament, and some of its fibres blend with those of the anterior cruciate ligament. The posterior insertional ligament of the lateral meniscus attaches to the tibia posterior to the lateral intercondylar eminence anteriorly to the posterior enthesis of the medial meniscus. The anterior fibres of the posterior insertional ligament of the lateral meniscus insert into the intercondylar fossa (area intercondylaris) of the medial femoral condyle anterior to the origin of posterior cruciate ligament forming the anterior meniscofemoral ligament.9–11
In a morphological cadaveric study concerning location, shape, and size of the meniscal insertions to bone, 92 knee joints were dissected and the anterior transverse ligament, which connects the anterior horns of the medial and lateral menisci, was found in 63 of the specimens (69%).9 In the same study, the posterior meniscofemoral ligament ( Wrisberg) was found in 70 of the knees (76%), and the anterior meniscofemoral ligament (Humphrey) was found in 34 (37%).9
Function
Menisci have an important role in knee function.12 Long-term follow-up studies showed that virtually all meniscectomized knees develop arthritic changes with time.13–16
Moreover, the severity of these changes seems to be proportional to the amount of meniscus removed. The main functions of the menisci are tibiofemoral load transmission, shock absorption, lubrication of the knee joint,17–21 and congruity improvement between the femoral and tibial articular surfaces in all knee flexion and rotation angles, since the menisci follow the motion of the opposing joint surfaces.1,22 30%–55% of the load in a standing position is transmitted by the knee menisci.19 Meniscectomy may determine decrease in contact area up to 50%–70%. The resulting increase in contact stresses on the tibial plateau are regarded as the main reason for the frequent bone and cartilage changes found after meniscectomy.1,23
The stress distribution on a smaller area causes an increase in the trabecular bone density in the proximal tibia, eventually leading to joint degeneration. The load distributing function of the menisci is possible as a result of their strong attachment to the bone through the anterior and the posterior entheses, which prevent the menisci from extruding from the joint during axial loading.1 Menisci contribute significantly to joint lubrication because of their high water content, amounting to 74% of the total weight of the meniscus. Compression forces squeeze the liquid out into the joint space, allowing smoother gliding of the joint surfaces. The menisci act as secondary soft tissue restraints preventing anterior tibial displacement and contributing to the stability of the knee.1,24–26
Epidemiology
The mean annual incidence of meniscal tears is about 60–70 per 100,000,27,28 with a male to female ratio ranging from 2.5:1 to 4:1. Meniscal pathology in younger patients are likely to be consequent to an acute traumatic event, while degenerative changes are more frequent at an older age.29 More than one third of all meniscal tears are associated with an anterior cruciate ligament injury,30 with a peak incidence in men aged 21–30 years and in girls and women aged 11–20 years. On the other hand, degenerative types of meniscal tears commonly occur in men aged between 40 and 60 years.
Diagnosis
A well-trained surgeon can safely rely on clinical examination for diagnosing meniscal injuries. History and clinical examination are at least as accurate as magnetic resonance imaging (MRI) in the skilled orthopedic surgeon’s hand.31 MRI should be reserved for more complicated and confusing cases. The routine ordering of an MRI scan of the knee before examination by a well-trained orthopedic surgeon is not recommended.31 Arthroscopy is the gold standard for the diagnosis of meniscal tears.
History
History is the first diagnostic tool for meniscal tears.12 A suspected intra-articular knee lesion must first be fully evaluated by history and physical examination to define the correct indication and avoid unnecessary imaging investigations. The essential first step in the approach to the patient with knee pain is to understand the type of complained pain. A detailed description of the injury mechanisms and symptoms usually allows physicians to establish a diagnosis. Common mechanisms of meniscal tears in sport are noncontact injuries, resulting while cutting, decelerating, or landing from a jump.12
As meniscal degeneration occurs with increasing age, moderate injuries may cause meniscal tears, and often patients are not able to remember the exact injury causing the tear. Usually patients complain of popping, catching, locking, or buckling along with joint line pain. These symptoms are suggestive of meniscal tear but are somewhat nonspecific. Mild synovitis, with swelling for several days after injury may result from meniscal tears. ACL tear are commonly associated with meniscal tears.32–36 The patient usually recalls hearing or feeling a pop at the moment of injury.12
Physical examination
The physical examination must be carried out thoroughly and methodically. Patients with medial meniscal injuries complain of pain in the medial aspect of the knee. McMurray test, Apley grind test, and the bounce home test are positive in medial meniscopathy.
McMurray test
The patient lies supine, the knee is fully flexed. The surgeon grasps the heel. The leg is rotated on the thigh with the knee in full flexion. The leg is flexed to 90° while the foot is maintained first in full internal rotation and then rotated in full external rotation. In patients with a torn meniscus, a click occurs and the patient complains of pain.
Apley grind test
With the patient lying prone, the surgeon grasps the foot, rotates it externally as far as possible, and flexes the knee to 90°. The foot is the rotated internally, and knee is extended. The surgeon then applies his left knee to the back of the patient’s thigh. The tibia is then compressed onto the knee joint while being externally rotated. If addition of compression produces an increase in pain, this grinding test is positive, and meniscal damage is diagnosed.
Bounce home test
With the patient lying supine, the surgeon grasps the foot, flexes completely the knee. The knee is then passively allowed to extend. The knee should extend completely or bounce home into extension with a sharp endpoint. A positive test occurs when full extension cannot be attained.
Imaging
Radiography
Radiographs of the knee exclude bony pathologies, and assess the concomitant presence of arthropatic changes. In the presence of knee arthritis, standing weight-bearing radiographs show reduction of the medial joint space width, osteophytes, subchondral bone cysts, and sclerosis. These radiographic changes are related to various abnormalities including cartilage loss and meniscal subluxation or extrusion from the joint line.
MRI
MRI is highly accurate in diagnosing meniscal and anterior cruciate ligament (ACL) tears. It is the most appropriate screening tool before therapeutic arthroscopy. It is preferable to diagnostic arthroscopy in most patients because it avoids the surgical risks of arthroscopy.37,38 The results of MRI differ for medial and lateral meniscus and ACL, with only 85% accuracy.39,40
The essential characteristics of meniscal tears, such as, location, shape, length, and depth can be revealed by MRI scan.41 The normal meniscus has low signal on all MR imaging sequences. On sagittal MR images, the anterior and posterior horns of the lateral meniscus are nearly equal in size, whereas the posterior horn of the medial meniscus is larger than the anterior horn.
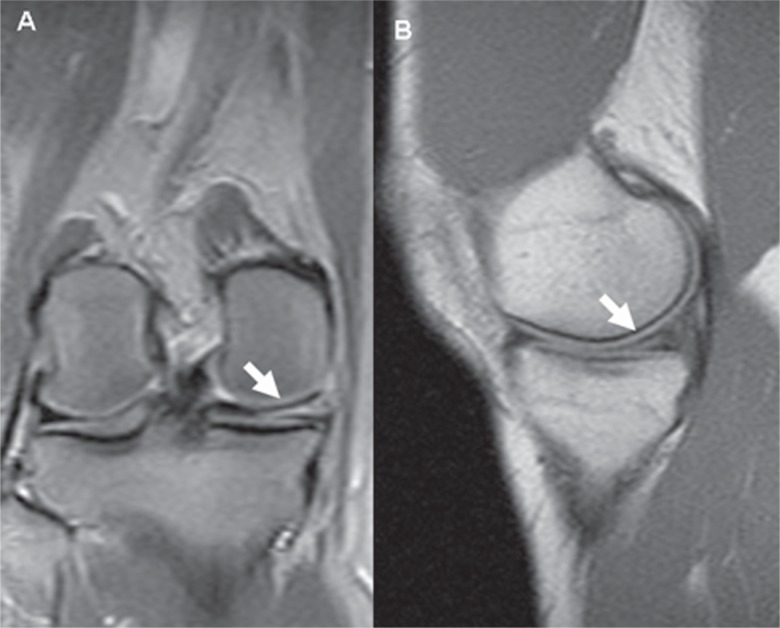
A meniscal tear in a knee without prior meniscal surgery can be seen as either an area of abnormal signal within the meniscus, or abnormal morphology of the meniscus (Figure 1).42 If the abnormal signal extends to the articular surface on two or more images, the sensitivity for a meniscal tear increases from 56%–94% medially and from 30%–90% laterally.42 The sagittal plane is very helpful to evaluate meniscal pathology. The coronal imaging plane improves the detection and characterization of radial, bucket-handle, horizontal, and displaced tears of the meniscal body, and the axial plane helps to diagnose radial, vertical, complex, displaced, and lateral meniscal tears.39
Figure 1.
A) Coronal and B) Sagittal magnetic resonance imaging view of a medial meniscal tear in a knee without prior meniscal surgery.
Meniscal subluxations are defined as protrusions over the edge of the tibial plateau seen at the level of the body of the meniscus.43,44
Spin-echo or fast spin-echo (FSE) proton density with or without fat saturation, T1, and gradient echo (GRE) are the most commonly used sequences.45
Sensitivity and specificity of MR imaging are 93% and 88% respectively for medial meniscal tears, and 79% and 95% respectively for lateral meniscal tears.46 Used sequences, observer variation, and sample size can determine the differences in sensitivity and specificity.47,48 Regardless of the technique used, the sensitivity for detecting meniscal tears usually is higher in the medial meniscus.37
Classification
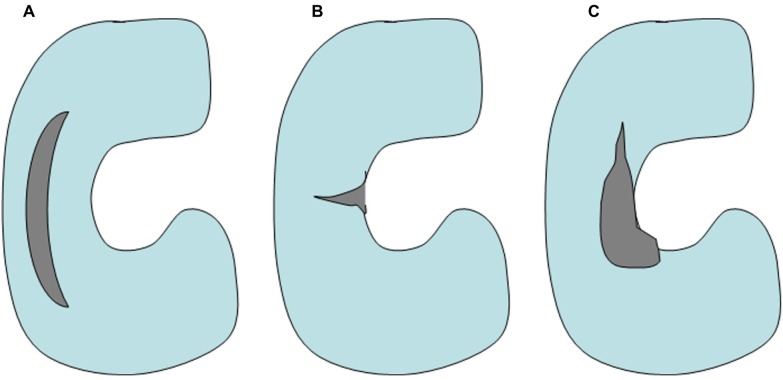
Meniscal tear patterns include vertical tears (longitudinal and radial), oblique, complex (or degenerative),49,50 and horizontal (Figure 2).29,51 Oblique and vertical longitudinal tears represent 81% of meniscal tears.51 Degenerative complex tears are more frequent with increasing age, and most meniscal pathology is found in the posterior horns.
Figure 2.
Schematic drawing, showing A) longitudinal B) radial, and C) complex meniscal tear.
Vertical longitudinal tears are parallel to the long axis of the meniscus, between the circumferential collagen fibers and perpendicular to the tibial plateau.52,53 Vertical longitudinal tears can be complete or incomplete. Complete tears, also known as “bucket handle tears”, usually originate in the posterior horn varying in length, involving up to the two thirds of the meniscus. These tears, more commonly affecting the medial meniscus, are often unstable and can cause mechanical symptoms or true locking of the knee. Incomplete tears also interest the posterior horn, both on the superior and on the inferior surfaces of the menisci. Symptoms may or may not be present.
A vertical radial tear is perpendicular to the long axis of the meniscus and to the tibial plateau,47,53–56 sectioning the circumferential collagen fibers. These tears are usually found at the junction between the posterior and the middle third of the medial meniscus or near the posterior insertion of the lateral meniscus. Vertical radial tears affect the ability of the menisci to transmit the tibiofemoral load and the contact stresses associated with weight-bearing. Usually these tears are not repairable,57 and meniscal debridement is unlikely to restore meniscal complete function, allowing the contact between articular cartilage surfaces and leading to accelerated degenerative changes.45,54–58 As a consequence, a severe effect on the function of the meniscus can be determined even by a small radial tear.57,59
Horizontal tears extend parallel to the tibial plateau, splitting the meniscus into an upper and a lower part,52,53 perforating collagen fiber bundles.
These tears seem to originate near the inner rim of the meniscus and extend towards the capsule, as the result of shear forces generated by axial compression. Their frequency increases with age. Horizontal tears are often associated with meniscal cysts and can lead to localized swelling.
Oblique tears, often called meniscal flap, can occur at any location but are more likely to be found between the posterior and middle third of the meniscus. Flap catching in the joint can cause symptoms and propagation of the tear by the generation of traction on the meniscocapsular junction. Complex or degenerative tears include two or more tear patterns, occurring more frequently in the posterior horn and midbody. These tears are more common in patients aged over 40 years, often in association with degenerative changes of articular cartilage, and represent part of the pathology of degenerative arthritis.60
Management
The meniscus has functions in load bearing, load transmission, shock absorption, joint stability, joint lubrication, and joint congruity.61 Because of these functions, meniscal tissue should be preserved whenever possible.62
Total meniscectomy
Nowadays, total meniscectomy is not a common procedure. However, previously it was a popular procedure, and short term outcome results of this technique were regarded as excellent. In 1948, Fairbank first13 described the potential damaging effects of total meniscectomy. The long-term results of total meniscectomy showed unfavorable long-term outcome results.
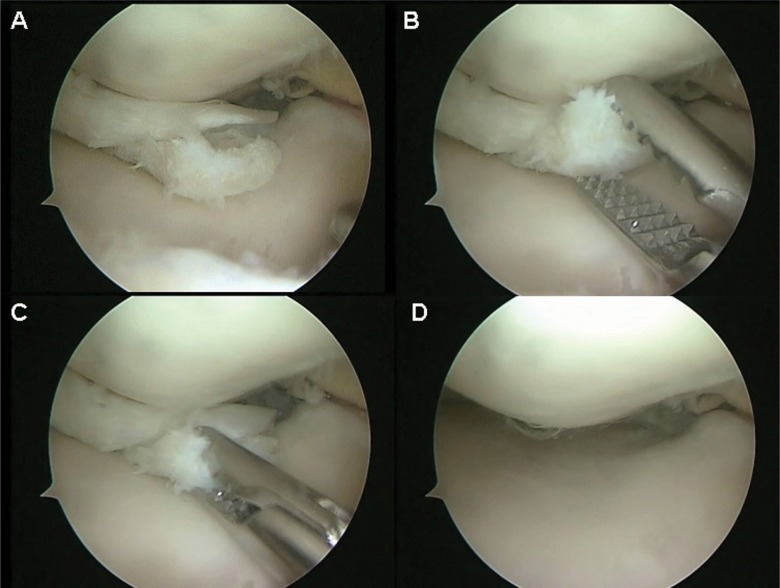
Partial meniscectomy
When meniscal repair is not possible, partial resection of the meniscus is indicated (Figure 3). To avoid the long-term consequences of total meniscectomy, general guidelines have been published.51 However, these guidelines have not been tested in a systematic manner, and are to be regarded at best as expert opinion.
Figure 3.
Partial resection of the medial meniscus for a complex lesion.
A number of studies reported 80%–90% satisfactory clinical results after arthroscopic partial meniscectomy at short-term follow-up (<2 years). However, several long-term studies have questioned whether partial meniscectomy is a benign procedure. Osteoarthritic radiographic changes can occur in 53% of knees that undergo partial meniscectomy compared with 27% of the untreated contralateral knees at 8-year follow-up.63
Repair
Meniscal repair has evolved from open to arthroscopic techniques, which include the inside-out and outside-in suture repairs and the all-inside techniques.64 Inside-out and outside-in techniques involve a mini-incision and securing the meniscus to capsule with suture. The all-inside technique include several options, including arthroscopic suture tying and absorbable fixation devices with names as arrow, fastener, dart, and staple.65–70
According to the literature, no given type of implant is clinically superior to another.71 Sutureless fixation materials have a higher complications rate (poor hold, synovitis, cartilage lesion) and were less successful in animal or cadaveric biomechanical studies. The current trend is towards the use of hybrid implants (fixation material combined with suture wire). However, because of complications such as neuropathic pain after open surgery (first generation devices) and after posterior approach surgery (second generation devices), hybrid implants tend to be reserved for cases of absolute necessity only.
Open repair
Open repair of meniscus tears has provided successful long-term results ranging from 84%–100%.
Open meniscal repair offers the advantage of better preparation of the tear site. However, only the most peripheral of tears in the red-red zone are amenable to this technique because of exposure and accessibility. Long-term follow-up of open meniscal repairs has revealed good success rates.72 In this technique, a small incision is performed, similar to that made in an arthroscopic inside-out meniscus repair. The capsule and synovium are incised, allowing direct observation of the tear. To our knowledge, no prospective studies have been published to report the results of open meniscal repair. Currently, the specific indication for open repair technique in a patient with a posterior medial meniscus tear (within 2 mm of the meniscosynovial junction) is a tight medial compartment. In this case, the visibility of the meniscus from an anterior portal is very difficult and the all-inside technique with knot tying can be challenging.
Arthroscopic inside-out repair
Henning73,74 first described the inside-out technique of arthroscopic meniscal repair. The inside-out meniscal repair technique involves fixation of a tear by placing sutures from inside the knee to a protected area on the outside of the joint capsule. Inside-out techniques use zone-specific cannulas to pass sutures through the joint and across the tear. The sutures are swaged onto flexible needles. A small posterior joint line incision is used to retrieve the sutures and tie directly on the capsule. The use of a posterior retractor, such as a gynecologic speculum, is vital in order to protect the posterior neurovascular structures.
Advantages of this technique include the ability to achieve consistent perpendicular suture placement through the meniscal tear in the posterior horn. However, this also carries the risks of neurovascular injury while placing the needle from inside the joint to outside. A posterior incision is required to place a retractor to protect the neurovascular structures when using this technique.
Inside-out repairs have yielded favorable results in numerous retrospective reports,21,40,45,60 with success rates of the studies based primarily on clinical results ranging from 73%–91%.75–83
Arthroscopic outside-in repair
The outside-in techniques have been described by Warren84 and Morgan and Casscells.85 Outside-in techniques involve passing sutures percutaneously through spinal needles at the joint line across the tear, and then retrieving the sutures intra-articularly under arthroscopic observation. The needles are passed through the meniscus rim and then through the meniscus body fragment. A small incision is then made at the joint line, where the protruding suture ends are retrieved and tied directly on the capsule. An alternative technique is to retrieve the intra-articular portion of the suture with another pass across the tear using a wire snare and tying the suture back on itself on the capsule. A potential disadvantage of the outside-in technique is difficulty in reducing the tear and opposing the edges while passing the sutures.
Arthroscopic all-inside repair
The all-inside technique was traditionally used to perform repairs of the far posterior horns, where a posterior accessory portal is used, along with passing a suture with a suture hook device.86,87 The suture would then be tied intra-articularly. More recently, arthroscopic all-inside meniscal repair techniques recently have become popular because they seem to avoid many of the potential complications of other meniscal repair techniques and decrease operative time. Technologic advances include a number of implantable anchors, arrows, screws, and staples that facilitate meniscal repair without the need for accessory incisions or portals. These devices can be made of permanent or absorbable materials. Although the pullout strength of some of these devices approximates those of mattress sutures in cadaveric studies,88,89 there have been no long-term clinical studies that compare them to more traditional repair techniques.
Meniscal transplantation
Meniscal transplantation is generally accepted as a management alternative option for selected symptomatic patients with previous complete or near-complete meniscectomy. Four methods of graft type have been described, including fresh allograft, fresh-frozen, cryopreserved and freeze-dried ( lyophilized). Human immunodeficiency virus (HIV), hepatitis B and C, and syphilis are potentially transferable diseases with meniscal transplant surgery via graft material. The documented risk for HIV transmission is estimated to be at 1 in 8 million.90 Secondary sterilization of allografts has previously been undertaken using gamma radiation, ethylene oxide, or chemical sterilization.
Unfortunately, the dose of gamma radiation deemed effective at eradicating HIV (2.5 mrad) produces detrimental changes in the mechanical structure of the allograft.91
Ethylene oxide is no longer used as one of its byproducts has been shown to cause synovitis.92
Although appropriate size-matching of the graft to the donor site is believed to influence meniscal function postoperatively,93 there is no consensus on the tolerable value of meniscal size mismatch and no studies have quantified sizing errors effects. Most authors accept a sizing mismatch of less than 5%.
Fixation of the graft is crucial for restoration of meniscal function. Main techniques for fixation are soft-tissue sutures, bony plugs, or a bony bridge. Cadaveric studies suggest that suture fixation alone is not able to restore the normal tibiofemoral load transmission, a critical function in articular cartilage protection. This result can be achieved with bony fixation of the anterior and posterior horns94,95 and better results were reported using this procedure.96 However, some authors have reported satisfactory results with soft-tissue fixation alone.97,98 Bony fixation requires accurate anatomical graft placement, and cadaveric studies reported poor mechanical properties in case of malpositioning of the bony anchors.99,100 A medial meniscal graft shoud be fixed using two bony plugs (one for the anterior and one for the posterior horn), while a bony bridge is more suitable for the lateral meniscus, because of the closeness of the two horns.
The success of allograft transplantation is defined by three main parameters: the short-term recovery of symptoms, the improvement of patient function, and the long-term prevention of degenerative knee changes after partial/total meniscectomy. Even though results from the available studies are difficult to compare because of the lack of a uniform outcome measure, current evidence suggests that meniscal allograft transplantation provides pain relief and improvement level of function for daily activities in short and intermediate follow-up.101 Long-term effect on degenerative joint disease progression remains.101 Best results appear to be obtained in patients aged under 40 years complaining of knee pain, with a normal knee alignment, stable knee joint and limited early degenerative changes (Outerbridge Grade 3 or less).
Conclusions
When possible, meniscal repair should be performed to try to maintain meniscal integrity and prevent long-term degenerative changes that occur after meniscectomy. When meniscal repair is not possible, partial meniscectomy can be considered saving as much viable meniscal tissue as possible.
In patients with severe injury, which makes the meniscus irreparable total meniscectomy can be required. Meniscal transplantation can be an option if symptoms referable to the meniscectomized joint are present.29,62
Footnotes
Disclosures
The authors report no conflicts of interest in this work.
References
- 1.Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998;193(Pt 2):161–178. doi: 10.1046/j.1469-7580.1998.19320161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cole BJ, Carter TR, Rodeo SA. Allograft meniscal transplantation: background, techniques, and results. Instr Course Lect. 2003;52:383–396. [PubMed] [Google Scholar]
- 3.Kohn D, Rudert M, Wirth CJ, Plitz W, Reiss G, Maschek H. Medial meniscus replacement by a fat pad autograft. An experimental study in sheep. Int Orthop. 1997;21(4):232–238. doi: 10.1007/s002640050157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen W, Tillmann B. Age-related blood and lymph supply of the knee menisci. A cadaver study. Acta Orthop Scand. 1995;66(4):308–312. doi: 10.3109/17453679508995550. [DOI] [PubMed] [Google Scholar]
- 5.Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10(2):90–95. doi: 10.1177/036354658201000205. [DOI] [PubMed] [Google Scholar]
- 6.Gao J, Oqvist G, Messner K. The attachments of the rabbit medial meniscus. A morphological investigation using image analysis and immunohistochemistry. J Anat. 1994;185(Pt 3):663–667. [PMC free article] [PubMed] [Google Scholar]
- 7.Gao J, Messner K. Natural healing of anterior and posterior attachments of the rabbit meniscus. Clin Orthop Relat Res. 1996;(328):276–284. doi: 10.1097/00003086-199607000-00042. [DOI] [PubMed] [Google Scholar]
- 8.Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy. 1995;11(4):386–394. doi: 10.1016/0749-8063(95)90188-4. [DOI] [PubMed] [Google Scholar]
- 9.Kohn D, Moreno B. Meniscus insertion anatomy as a basis for meniscus replacement: a morphological cadaveric study. Arthroscopy. 1995;11(1):96–103. doi: 10.1016/0749-8063(95)90095-0. [DOI] [PubMed] [Google Scholar]
- 10.Wan AC, Felle P. The meniscofemoral ligaments. Clin Anat. 1995;8(5):323–326. doi: 10.1002/ca.980080503. [DOI] [PubMed] [Google Scholar]
- 11.Poynton AR, Javadpour SM, Finegan PJ, O’Brien M. The meniscofemoral ligaments of the knee. J Bone Joint Surg Br. 1997;79(2):327–330. doi: 10.1302/0301-620x.79b2.6893. [DOI] [PubMed] [Google Scholar]
- 12.Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34(4):252–257. doi: 10.1136/bjsm.34.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Am. 1948;30B(4):664–670. [PubMed] [Google Scholar]
- 14.Laasonen EM, Wilppula E. Why a meniscectomy fails. Acta Orthop Scand. 1976;47(6):672–675. doi: 10.3109/17453677608988758. [DOI] [PubMed] [Google Scholar]
- 15.Noble J, Turner PG. The function, pathology, and surgery of the meniscus. Clin Orthop Relat Res. 1986;(210):62–68. [PubMed] [Google Scholar]
- 16.Soballe K, Hansen AJ. Late results after meniscectomy in children. Injury. 1987;18(3):182–184. doi: 10.1016/0020-1383(87)90133-1. [DOI] [PubMed] [Google Scholar]
- 17.Bargar WL, Moreland JR, Markolf KL, Shoemaker SC, Amstutz HC, Grant TT. In vivo stability testing of post-meniscectomy knees. Clin Orthop Relat Res. 1980;(150):247–252. [PubMed] [Google Scholar]
- 18.Krause WR, Pope MH, Johnson RJ, Wilder DG. Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am. 1976;58(5):599–604. [PubMed] [Google Scholar]
- 19.Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res. 1980;(149):283–290. [PubMed] [Google Scholar]
- 20.Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints – Part 1: Tibial surface of the knee. J Biomech Eng. 1983;105(3):216–225. doi: 10.1115/1.3138409. [DOI] [PubMed] [Google Scholar]
- 21.Ahmed AM, Burke DL, Yu A. In-vitro measurement of static pressure distribution in synovial joints – Part 2: Retropatellar surface. J Biomech Eng. 1983;105(3):226–236. doi: 10.1115/1.3138410. [DOI] [PubMed] [Google Scholar]
- 22.Bylski-Austrow DI, Ciarelli MJ, Kayner DC, Matthews LS, Goldstein SA. Displacements of the menisci under joint load: an in vitro study in human knees. J Biomech. 1994;27(4):421–431. doi: 10.1016/0021-9290(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 23.Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthritic knee joints. Acta Orthop Scand. 1980;51(6):871–879. doi: 10.3109/17453678008990887. [DOI] [PubMed] [Google Scholar]
- 24.Jackson F, Miller J. Alternative approaches to control – quo vadit? Vet Parasitol. 2006;139(4):371–384. doi: 10.1016/j.vetpar.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 25.Shoemaker SC, Markolf KL. The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee. Effects of partial versus total excision. J Bone Joint Surg Am. 1986;68(1):71–79. [PubMed] [Google Scholar]
- 26.Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64(6):883–888. [PubMed] [Google Scholar]
- 27.Hede A, Jensen DB, Blyme P, Sonne-Holm S. Epidemiology of meniscal lesions in the knee. 1,215 open operations in Copenhagen 1982–84. Acta Orthop Scand. 1990;61(5):435–437. doi: 10.3109/17453679008993557. [DOI] [PubMed] [Google Scholar]
- 28.Nielsen AB, Yde J. Epidemiology of acute knee injuries: a prospective hospital investigation. J Trauma. 1991;31(12):1644–1648. doi: 10.1097/00005373-199112000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10(3):168–176. doi: 10.5435/00124635-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Poehling GG, Ruch DS, Chabon SJ. The landscape of meniscal injuries. Clin Sports Med. 1990;9(3):539–549. [PubMed] [Google Scholar]
- 31.Kocabey Y, Tetik O, Isbell WM, Atay OA, Johnson DL. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy. 2004;20(7):696–700. doi: 10.1016/j.arthro.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Franceschi F, Longo UG, Ruzzini L, Papalia R, Maffulli N, Denaro V. Quadriceps tendon-patellar bone autograft for anterior cruciate ligament reconstruction: a technical note. Bull NYU Hosp Jt Dis. 2008;66(2):120–123. [PubMed] [Google Scholar]
- 33.Capuano L, Hardy P, Longo UG, Denaro V, Maffulli N. No difference in clinical results between femoral transfixation and bio-interference screw fixation in hamstring tendon ACL reconstruction. A preliminary study. Knee. 2008;15(3):174–179. doi: 10.1016/j.knee.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 34.Longo UG, King JB, Denaro V, Maffulli N. Double-bundle arthroscopic reconstruction of the anterior cruciate ligament: does the evidence add up? J Bone Joint Surg Br. 2008;90(8):995–999. doi: 10.1302/0301-620X.90B8.20083. [DOI] [PubMed] [Google Scholar]
- 35.Longo UG, Maffulli N, Denaro V. Minimally invasive total knee arthroplasty. N Engl J Med. 2009;361(6):633–634. author reply 634. [PubMed] [Google Scholar]
- 36.Maffulli N, Longo UG, Denaro V. Anterior cruciate ligament tear. N Engl J Med. 2009;360(14):1463. doi: 10.1056/NEJMc082471. author reply 1463. [DOI] [PubMed] [Google Scholar]
- 37.Fox MG. MR imaging of the meniscus: review, current trends, and clinical implications. Radiol Clin North Am. 2007;45(6):1033–1053. doi: 10.1016/j.rcl.2007.08.009. vii. [DOI] [PubMed] [Google Scholar]
- 38.Fox MG. MR imaging of the meniscus: review, current trends, and clinical implications. Magn Reson Imaging Clin N Am. 2007;15(1):103–123. doi: 10.1016/j.mric.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Bridgman S, Richards PJ, Walley G, MacKenzie G, Clement D, McCall I, Griffiths D, Maffulli N. The effect of magnetic resonance imaging scans on knee arthroscopy: randomized controlled trial. Arthroscopy. 2007;23(11):1167–1173. doi: 10.1016/j.arthro.2007.05.020. e1161. [DOI] [PubMed] [Google Scholar]
- 40.Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84:5–23. doi: 10.1093/bmb/ldm022. [DOI] [PubMed] [Google Scholar]
- 41.Derrett S, Walley GD, Bridgman SA, Richards P, Maffulli N. Magnetic resonance imaging, knee arthroscopy, and clinical decision making: a descriptive study of five surgeons. Int J Technol Assess Health Care. 2009;25(4):577–583. doi: 10.1017/S0266462309990419. [DOI] [PubMed] [Google Scholar]
- 42.Evans PJ, Bell GD, Frank C. Prospective evaluation of the McMurray test. Am J Sports Med. 1993;21(4):604–608. doi: 10.1177/036354659302100420. [DOI] [PubMed] [Google Scholar]
- 43.Rubin DA, Paletta GA., Jr Current concepts and controversies in meniscal imaging. Magn Reson Imaging Clin N Am. 2000;8(2):243–270. [PubMed] [Google Scholar]
- 44.Rubin DA, Kettering JM, Towers JD, Britton CA. MR imaging of knees having isolated and combined ligament injuries. AJR Am J Roentgenol. 1998;170(5):1207–1213. doi: 10.2214/ajr.170.5.9574586. [DOI] [PubMed] [Google Scholar]
- 45.Helms CA. The meniscus: recent advances in MR imaging of the knee. AJR Am J Roentgenol. 2002;179(5):1115–1122. doi: 10.2214/ajr.179.5.1791115. [DOI] [PubMed] [Google Scholar]
- 46.Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Myriam Hunink MG. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology. 2003;226(3):837–848. doi: 10.1148/radiol.2263011892. [DOI] [PubMed] [Google Scholar]
- 47.De Smet AA, Norris MA, Yandow DR, Quintana FA, Graf BK, Keene JS. MR diagnosis of meniscal tears of the knee: importance of high signal in the meniscus that extends to the surface. AJR Am J Roentgenol. 1993;161(1):101–107. doi: 10.2214/ajr.161.1.8517286. [DOI] [PubMed] [Google Scholar]
- 48.De Smet AA, Norris MA, Yandow DR, Graf BK, Keene JS. Diagnosis of meniscal tears of the knee with MR imaging: effect of observer variation and sample size on sensitivity and specificity. AJR Am J Roentgenol. 1993;160(3):555–559. doi: 10.2214/ajr.160.3.8430552. [DOI] [PubMed] [Google Scholar]
- 49.Binfield PM, Maffulli N, King JB. Patterns of meniscal tears associated with anterior cruciate ligament lesions in athletes. Injury. 1993;24(8):557–561. doi: 10.1016/0020-1383(93)90038-8. [DOI] [PubMed] [Google Scholar]
- 50.Maffulli N, Chan KM, Bundoc RC, Cheng JC. Knee arthroscopy in Chinese children and adolescents: an eight-year prospective study. Arthroscopy. 1997;13(1):18–23. doi: 10.1016/s0749-8063(97)90205-x. [DOI] [PubMed] [Google Scholar]
- 51.Metcalf RW, Burks RT, Metcalf MS, McGinty JB. Arthroscopic meniscectomy. In: McGinty JB, Caspari RB, Jackson RW, Poehling GG, editors. Operative Arthroscopy. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1996. pp. 263–297. [Google Scholar]
- 52.Jee WH, McCauley TR, Kim JM. Magnetic resonance diagnosis of meniscal tears in patients with acute anterior cruciate ligament tears. J Comput Assist Tomogr. 2004;28(3):402–406. doi: 10.1097/00004728-200405000-00017. [DOI] [PubMed] [Google Scholar]
- 53.Jee WH, McCauley TR, Kim JM, Jun DJ, Lee YJ, Choi BG, Choi KH. Meniscal tear configurations: categorization with MR imaging. AJR Am J Roentgenol. 2003;180(1):93–97. doi: 10.2214/ajr.180.1.1800093. [DOI] [PubMed] [Google Scholar]
- 54.Magee T, Shapiro M, Williams D. Comparison of high-field-strength versus low-field-strength MRI of the shoulder. AJR Am J Roentgenol. 2003;181(5):1211–1215. doi: 10.2214/ajr.181.5.1811211. [DOI] [PubMed] [Google Scholar]
- 55.Magee T, Shapiro M, Williams D. MR accuracy and arthroscopic incidence of meniscal radial tears. Skeletal Radiol. 2002;31(12):686–689. doi: 10.1007/s00256-002-0579-8. [DOI] [PubMed] [Google Scholar]
- 56.Tuckman GA, Miller WJ, Remo JW, Fritts HM, Rozansky MI. Radial tears of the menisci: MR findings. AJR Am J Roentgenol. 1994;163(2):395–400. doi: 10.2214/ajr.163.2.8037039. [DOI] [PubMed] [Google Scholar]
- 57.Harper KW, Helms CA, Lambert HS, 3rd, Higgins LD. Radial meniscal tears: significance, incidence, and MR appearance. AJR Am J Roentgenol. 2005;185(6):1429–1434. doi: 10.2214/AJR.04.1024. [DOI] [PubMed] [Google Scholar]
- 58.Maffulli N, Longo UG, Gougoulias N, Loppini M, Denaro V. Long-term Health Outcomes of Youth Sports Injuries. Br J Sports Med. 2009 doi: 10.1136/bjsm.2009.069526. [DOI] [PubMed] [Google Scholar]
- 59.Kidron A, Thein R. Radial tears associated with cleavage tears of the medial meniscus in athletes. Arthroscopy. 2002;18(3):254–256. doi: 10.1053/jars.2002.30650. [DOI] [PubMed] [Google Scholar]
- 60.De Maeseneer M, Shahabpour M, Vanderdood K, Van Roy F, Osteaux M. Medial meniscocapsular separation: MR imaging criteria and diagnostic pitfalls. Eur J Radiol. 2002;41(3):242–252. doi: 10.1016/s0720-048x(01)00394-1. [DOI] [PubMed] [Google Scholar]
- 61.Henning CE, Lynch MA. Current concepts of meniscal function and pathology. Clin Sports Med. 1985;4(2):259–265. [PubMed] [Google Scholar]
- 62.Greis PE, Holmstrom MC, Bardana DD, Burks RT. Meniscal injury: II. Management. J Am Acad Orthop Surg. 2002;10(3):177–187. doi: 10.5435/00124635-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 63.Fauno P, Nielsen AB. Arthroscopic partial meniscectomy: a long-term follow-up. Arthroscopy. 1992;8(3):345–349. doi: 10.1016/0749-8063(92)90066-k. [DOI] [PubMed] [Google Scholar]
- 64.McCarty EC, Marx RG, DeHaven KE. Meniscus repair: considerations in treatment and update of clinical results. Clin Orthop Relat Res. 2002;(402):122–134. [PubMed] [Google Scholar]
- 65.Albrecht-Olsen P, Kristensen G, Burgaard P, Joergensen U, Toerholm C. The arrow versus horizontal suture in arthroscopic meniscus repair. A prospective randomized study with arthroscopic evaluation. Knee Surg Sports Traumatol Arthrosc. 1999;7(5):268–273. doi: 10.1007/s001670050162. [DOI] [PubMed] [Google Scholar]
- 66.Busenkell GL, Lee CS. Arthroscopic meniscal repair: a posterior cannulated technique. Arthroscopy. 1992;8(2):247–253. doi: 10.1016/0749-8063(92)90045-d. [DOI] [PubMed] [Google Scholar]
- 67.Barrett GR, Treacy SH, Ruff CG. Preliminary results of the T-fix endoscopic meniscus repair technique in an anterior cruciate ligament reconstruction population. Arthroscopy. 1997;13(2):218–223. doi: 10.1016/s0749-8063(97)90157-2. [DOI] [PubMed] [Google Scholar]
- 68.DeHaven KE. Meniscus repair. Am J Sports Med. 1999;27(2):242–250. doi: 10.1177/03635465990270022301. [DOI] [PubMed] [Google Scholar]
- 69.Escalas F, Quadras J, Caceres E, Benaddi J. T-Fix anchor sutures for arthroscopic meniscal repair. Knee Surg Sports Traumatol Arthrosc. 1997;5(2):72–76. doi: 10.1007/s001670050029. [DOI] [PubMed] [Google Scholar]
- 70.Hurel C, Mertens F, Verdonk R. Biofix resorbable meniscus arrow for meniscal ruptures: results of a 1-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2000;8(1):46–52. doi: 10.1007/s001670050010. [DOI] [PubMed] [Google Scholar]
- 71.Beaufils P, Hulet C, Dhenain M, Nizard R, Nourissat G, Pujol N. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95(6):437–442. doi: 10.1016/j.otsr.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 72.DeHaven KE, Sebastianelli WJ. Open meniscus repair. Indications, technique, and results. Clin Sports Med. 1990;9(3):577–587. [PubMed] [Google Scholar]
- 73.Henning CE, Lynch MA, Yearout KM, Vequist SW, Stallbaumer RJ, Decker KA. Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res. 1990;(252):64–72. [PubMed] [Google Scholar]
- 74.Henning CE, Clark JR, Lynch MA, Stallbaumer R, Yearout KM, Vequist SW. Arthroscopic meniscus repair with a posterior incision. Instr Course Lect. 1988;37:209–221. [PubMed] [Google Scholar]
- 75.Barber FA. Meniscus repair: results of an arthroscopic technique. Arthroscopy. 1987;3(1):25–30. doi: 10.1016/s0749-8063(87)80006-3. [DOI] [PubMed] [Google Scholar]
- 76.Barber FA, Click SD. Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy. 1997;13(4):433–437. doi: 10.1016/s0749-8063(97)90120-1. [DOI] [PubMed] [Google Scholar]
- 77.Barrett GR, Field MH, Treacy SH, Ruff CG. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy. 1998;14(8):824–829. doi: 10.1016/s0749-8063(98)70018-0. [DOI] [PubMed] [Google Scholar]
- 78.Eggli S, Wegmuller H, Kosina J, Huckell C, Jakob RP. Long-term results of arthroscopic meniscal repair. An analysis of isolated tears. Am J Sports Med. 1995;23(6):715–720. doi: 10.1177/036354659502300614. [DOI] [PubMed] [Google Scholar]
- 79.Jakob RP, Staubli HU, Zuber K, Esser M. The arthroscopic meniscal repair. Techniques and clinical experience. Am J Sports Med. 1988;16(2):137–142. doi: 10.1177/036354658801600208. [DOI] [PubMed] [Google Scholar]
- 80.Johnson MJ, Lucas GL, Dusek JK, Henning CE. Isolated arthroscopic meniscal repair: a long-term outcome study (more than 10 years) Am J Sports Med. 1999;27(1):44–49. doi: 10.1177/03635465990270011501. [DOI] [PubMed] [Google Scholar]
- 81.Perdue PS, Jr, Hummer CD, 3rd, Colosimo AJ, Heidt RS, Jr, Dormer SG. Meniscal repair: outcomes and clinical follow-up. Arthroscopy. 1996;12(6):694–698. doi: 10.1016/s0749-8063(96)90172-3. [DOI] [PubMed] [Google Scholar]
- 82.Ryu RK, Dunbar WHt. Arthroscopic meniscal repair with two-year follow-up: a clinical review. Arthroscopy. 1988;4(3):168–173. doi: 10.1016/s0749-8063(88)80021-5. [DOI] [PubMed] [Google Scholar]
- 83.Stone RG, Frewin PR, Gonzales S. Long-term assessment of arthroscopic meniscus repair: a two- to six-year follow-up study. Arthroscopy. 1990;6(2):73–78. doi: 10.1016/0749-8063(90)90001-t. [DOI] [PubMed] [Google Scholar]
- 84.Warren RF, Levy IM. Meniscal lesions associated with anterior cruciate ligament injury. Clin Orthop Relat Res. 1983;(172):32–37. [PubMed] [Google Scholar]
- 85.Morgan CD, Casscells SW. Arthroscopic meniscus repair: a safe approach to the posterior horns. Arthroscopy. 1986;2(1):3–12. doi: 10.1016/s0749-8063(86)80003-2. [DOI] [PubMed] [Google Scholar]
- 86.Morgan CD. The “all-inside” meniscus repair. Arthroscopy. 1991;7(1):120–125. doi: 10.1016/0749-8063(91)90093-d. [DOI] [PubMed] [Google Scholar]
- 87.Cooper DE, Arnoczky SP, Warren RF. Meniscal repair. Clin Sports Med. 1991;10(3):529–548. [PubMed] [Google Scholar]
- 88.Dervin GF, Downing KJ, Keene GC, McBride DG. Failure strengths of suture versus biodegradable arrow for meniscal repair: an in vitro study. Arthroscopy. 1997;13(3):296–300. doi: 10.1016/s0749-8063(97)90024-4. [DOI] [PubMed] [Google Scholar]
- 89.Albrecht-Olsen P, Lind T, Kristensen G, Falkenberg B. Failure strength of a new meniscus arrow repair technique: biomechanical comparison with horizontal suture. Arthroscopy. 1997;13(2):183–187. doi: 10.1016/s0749-8063(97)90153-5. [DOI] [PubMed] [Google Scholar]
- 90.Buck BE, Resnick L, Shah SM, Malinin TI. Human immunodeficiency virus cultured from bone. Implications for transplantation. Clin Orthop Relat Res. 1990;(251):249–253. [PubMed] [Google Scholar]
- 91.Vangsness CT, Jr, Garcia IA, Mills CR, Kainer MA, Roberts MR, Moore TM. Allograft transplantation in the knee: tissue regulation, procurement, processing, and sterilization. Am J Sports Med. 2003;31(3):474–481. doi: 10.1177/03635465030310032701. [DOI] [PubMed] [Google Scholar]
- 92.Jackson DW, Windler GE, Simon TM. Intra-articular reaction associated with the use of freeze-dried, ethylene oxide-sterilized bone-patella tendon-bone allografts in the reconstruction of the anterior cruciate ligament. Am J Sports Med. 1990;18(1):1–10. doi: 10.1177/036354659001800101. discussion 10–11. [DOI] [PubMed] [Google Scholar]
- 93.Rodeo SA. Meniscal allografts – where do we stand? Am J Sports Med. 2001;29(2):246–261. doi: 10.1177/03635465010290022401. [DOI] [PubMed] [Google Scholar]
- 94.Chen MI, Branch TP, Hutton WC. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy. 1996;12(2):174–181. doi: 10.1016/s0749-8063(96)90007-9. [DOI] [PubMed] [Google Scholar]
- 95.Alhalki MM, Howell SM, Hull ML. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med. 1999;27(3):320–328. doi: 10.1177/03635465990270030901. [DOI] [PubMed] [Google Scholar]
- 96.Rodeo SA, Seneviratne A, Suzuki K, Felker K, Wickiewicz TL, Warren RF. Histological analysis of human meniscal allografts. A preliminary report. J Bone Joint Surg Am. 2000;82-A(8):1071–1082. doi: 10.2106/00004623-200008000-00002. [DOI] [PubMed] [Google Scholar]
- 97.Verdonk PC, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R. Transplantation of viable meniscal allograft. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 1):109–118. doi: 10.2106/JBJS.E.00875. [DOI] [PubMed] [Google Scholar]
- 98.Verdonk PC, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R. Transplantation of viable meniscal allograft. Survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87(4):715–724. doi: 10.2106/JBJS.C.01344. [DOI] [PubMed] [Google Scholar]
- 99.Szomor ZL, Martin TE, Bonar F, Murrell GA. The protective effects of meniscal transplantation on cartilage. An experimental study in sheep. J Bone Joint Surg Am. 2000;82(1):80–88. doi: 10.2106/00004623-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 100.Sekaran SV, Hull ML, Howell SM. Nonanatomic location of the posterior horn of a medial meniscal autograft implanted in a cadaveric knee adversely affects the pressure distribution on the tibial plateau. Am J Sports Med. 2002;30(1):74–82. doi: 10.1177/03635465020300012601. [DOI] [PubMed] [Google Scholar]
- 101.Crook TB, Ardolino A, Williams LA, Barlow IW. Meniscal allograft transplantation: a review of the current literature. Ann R Coll Surg Engl. 2009;91(5):361–365. doi: 10.1308/003588409X428559. [DOI] [PMC free article] [PubMed] [Google Scholar]