Abstract
Objective
To assess whether a history of lumbar stress fracture in pace bowlers in cricket is a risk factor for lower limb muscle strains.
Methods
This was a prospective cohort risk factor study, conducted using injury data from contracted first class pace bowlers in Australia during seasons 1998–1999 to 2008–2009 inclusive. There were 205 pace bowlers, 33 of whom suffered a lumbar stress fracture when playing first class cricket. Risk ratios ([RR] with 95% confidence intervals[CI]) were calculated to compare the seasonal incidence of various injuries between bowlers with a prior history of lumbar stress fracture and those with no history of lumbar stress fracture.
Results
Risk of calf strain was strongly associated with prior lumbar stress fracture injury history (RR = 4.1; 95% CI: 2.4–7.1). Risks of both hamstring strain (RR = 1.5; 95% CI: 1.03–2.1) and quadriceps strain (RR = 2.0; 95% CI: 1.1–3.5) were somewhat associated with history of lumbar stress fracture. Risk of groin strain was not associated with history of lumbar stress fracture (RR = 0.7; 95% CI: 0.4–1.1). Other injuries showed little association with prior lumbar stress fracture, although knee cartilage injuries were more likely in the non-stress fracture group.
Conclusion
Bony hypertrophy associated with lumbar stress fracture healing may lead to subsequent lumbar nerve root impingement, making lower limb muscle strains more likely to occur. Confounders may be responsible for some of the findings. In particular, bowling speed is likely to be independently correlated with risk of lumbar stress fracture and risk of muscle strain. However, as the relationship between lumbar stress fracture history and calf strain was very strong, and that there is a strong theoretical basis for the connection, it is likely that this is a true association.
Keywords: cricket, fast bowling, stress fractures, hamstring strain, calf strain
Introduction
It has been previously proposed that lumbar spine pathology (particularly involving L5 segment) is a risk for hamstring and calf strain.1 This hypothesis is based on traditional clinical teaching, where for many years imaging-negative muscle strains have been thought to have pain arising from lumbar structures. The hypothesis has been supported by the dual observations that: (1) degenerative changes in the lumbar spine are far more common at L5 or L5/S1 segmental level1–3 (2) advancing age is a risk factor for hamstring and calf strain injury which have L5 and S1 nerve supply,1,4 but not apparently lower limb injuries which have upper lumbar plexus nerve supply. Lumbosacral epidural and computed tomography (CT) guided nerve root sleeve injections of cortisone have been successfully used in clinical practice for management of hamstring and calf pain in athletes.1,5 Whilst this theory is sensible, to date there is little direct evidence that lumbar pathology increases the risk of hamstring and calf strain injury.
Cricket fast bowling provides an ideal environment to study the relationship between lumbar spine pathology (particularly stress fractures, Figure 1) and muscle strains, as these injuries are very common injuries in fast bowlers (Figure 2).6–11 Lumbar stress fractures are generally treated conservatively, including in elite athletes.12 Injury surveillance has demonstrated that in terms of missed playing time, lumbar spine injuries (and stress fractures in young fast bowlers in particular) take a great toll on cricketers.13,14 Studies have previously associated a ‘mixed’ action with the development of lumbar spine injuries, particularly stress fractures.7,8,10 More recently lateral flexion of the lumbar spine has been linked to lumbar stress fractures in senior fast bowlers.15
Figure 1.

Pars defects with bony hypertrophy seen on axial CT scan.
Abbreviation: CT, computed tomography.
Figure 2.

The fast bowling action for a left-arm bowler, showing propensity for both muscle strains (from sprinting, acceleration and deceleration) and lumbar stress fractures (from rotation of the lumbar spine).
The hypothesis of the study was that a player with a past history of a lumbar stress fracture would be more likely to suffer a muscle strain injury, particularly a hamstring or calf injury.
Methods
Cricket Australia conducts an annual ongoing injury survey recording injuries in contracted first class players. Methods for this survey have been described previously.14 The methods used for Cricket Australia injury surveillance are non-interventional, conform to the Code of Ethics of the World Medical Association (Declaration of Helsinki) and have been approved by the Cricket Australia Sport Science Sport Medicine Advisory Group.
This study was a prospective cohort study comparing future injury risk in bowlers with and without a history of lumbar stress fracture. The analysis was performed for the 205 pace bowlers who were contracted for 11 seasons 1998–1999 to 2008–2009 inclusive. During their contract period, 33 of the pace bowlers suffered from a lumbar stress fracture, with 172 not suffering a lumbar stress fracture. The average age at the start of each season for the fast bowlers in this study was 26.1 years (± 4.2 years).
The comparison was performed to examine the effect, if any, of a history of lumbar stress fracture in fast bowlers on the development of future injuries of a different nature, particularly muscle strains.
Injury definition and diagnosis
In 2005, cricket researchers published consensus international injury definitions for the sport and the methods of this survey adhere to the international definitions.16,17 The definition of a cricket injury is one that either: (1) prevents a player from being fully available for selection in a major match or (2) during a major match, causes a player to be unable to bat, bowl or keep wicket when required by either the rules or the team’s captain.
Diagnosis and injury categorization was that recorded in the injury surveillance system. Although the diagnoses were extracted for analysis in this study, the methods used to obtain the diagnosis were not able to be extracted. Therefore, it is not known, for example, whether the lumbar stress fractures recorded were diagnosed on magnetic resonance imaging MRI scan, single photon emission computed tomography (SPECT) bone scan or computed tomography (CT) scan. Given that all players were professionally contracted, it would be expected that imaging would have been used in all cases where a lumbar stress fracture was diagnosed and the majority of cases where a muscle strain was diagnosed.
Past injury history prior to awarding of a professional contract was also not recorded in the injury surveillance system. It is almost certain that there were multiple cases of fast bowlers who had suffered a lumbar stress fracture in their junior years prior to being professionally contracted, as lumbar stress fracture is a common diagnosis in junior players. The methodology of this study did not allow these cases to be recognized. Season 1998–1999 was the first season of prospective injury surveillance. However, there was retrospective injury surveillance performed at the professional level for the three years prior to this (1995–1996 to 1997–1998)13 which was available to source lumbar stress fracture history for this study.
Statistical analysis
A simple two-by-two χ2 test was not considered an appropriate analysis, as we decided bowlers who suffered a stress fracture should to be included in the stress fracture group after this injury and in the non-stress fracture prior to their injury.
The analysis was made to compare seasonal injury rates for various injury categories between the stress fracture and non-stress fracture group. A risk ratio (RR) was calculated for each injury category, being the seasonal incidence of the prior stress fracture group divided by the seasonal incidence of the non-stress fracture group. Confidence intervals (CI) for these were calculated using Taylor Series expansions.18
Results
A comparison of seasonal injury incidence (for major categories) in fast bowlers with and without a history of lumbar stress fracture is presented in Table 1. Univariate analysis reveals a greater risk of calf strain (in particular), hamstring strain and quadriceps strain in fast bowlers with a history of lumbar stress fracture. The major upper limb injury categories show no difference between those players with and without a history of lumbar stress fracture. There is an apparent negative (inverse) correlation between lumbar stress fracture and knee cartilage injury.
Table 1.
Seasonal risk of various injuries in pace bowlers after lumbar stress fracture
| Injury category | Seasonal incidence (injuries per team per season)
|
Risk ratio | Confidence intervals | |
|---|---|---|---|---|
| Bowlers with history of lumbar stress fracture | Bowlers with no history of lumbar stress fracture | |||
| Shoulder sprains and dislocations | 0.7 | 0.8 | 0.9 | 0.4–1.9 |
| Shoulder tendon injuries | 0.8 | 1.0 | 0.8 | 0.4–1.6 |
| Abdominal muscle strains | 3.4 | 2.9 | 1.2 | 0.8–1.7 |
| Groin strain injuries | 1.5 | 2.3 | 0.7 | 0.4–1.1 |
| Hamstring strains | 3.9 | 2.6 | 1.5 | 1.03–2.1* |
| Quadriceps strains | 1.7 | 0.9 | 2.0 | 1.1–3.5* |
| Knee cartilage injuries | 0.1 | 1.3 | 0.1 | 0.0–0.4* |
| Calf strains | 2.7 | 0.7 | 4.1 | 2.4–7.1* |
| Ankle sprains and joint injuries | 1.3 | 0.9 | 1.5 | 0.8–2.8 |
Significant association at the P < 0.05 level.
As the majority of injuries had both bowling arm and side of the body injury recorded as part of the injury database, Table 2 presents the relationship between bowling arm and side of the body injury. Most of the lumbar stress fractures occurred on the non-bowling side of the body, as did most of the hamstring strains and abdominal strains. By comparison, most of the quadriceps and calf strains occurred on the bowling side of the body. The side-to-side relationship probably relates mainly to the bowling mechanics where the hip tends to be flexed at delivery on the non-bowling side and extended at delivery on the bowling side. By contrast, the ankle is plantar-flexed at delivery on the non-bowling side and dorsi-flexed on the non-bowling side. This puts the non-delivery hamstring under relatively more stretch at the time of delivery (front foot impact), with the bowling side quadriceps and calf muscles under relatively more stretch (back foot impact).
Table 2.
Relationship of injuries to bowling or non-bowling side of body
| Non-bowling side | Bowling side | Not known or bilateral | |
|---|---|---|---|
| Lumbar stress fractures | 47 | 3 | 7 |
| Abdominal and lumbar muscle strains | 110 | 18 | 11 |
| Groin strain injuries | 39 | 26 | 32 |
| Hamstring strains | 77 | 29 | 29 |
| Quadriceps strains | 19 | 20 | 11 |
| Calf strains | 8 | 39 | 8 |
A table of spinal level lumbar stress fracture is not presented, as it was only a minority of injuries where the spinal level was recorded in the database. Ten lumbar stress fractures were reported to be at L5 level, which was the most common level of those reported.
Discussion
This study reports that fast bowlers with a known history of lumbar stress fracture are more likely to suffer lower limb muscle strains, particularly calf strains, but also hamstring and quadriceps strains. There does not seem to be any relationship between lumbar stress fracture history and other common injuries apart from muscle strains.
This study does have some limitations. The history of lumbar stress fracture is taken from injury survey records and would be missing some cases of lumbar stress fracture which were sustained prior to the bowler in question joining a first class squad (even though some elite players are contracted as early as age 18). In addition, there may be players who, if scanned, would have had radiological evidence of pars defect (indicating past stress fracture) who had not reported any known history, as asymptomatic stress fractures are known to occur.19 Because the methods used did not involve player identification, further questioning of players about prior history for lumbar stress fracture or lumbar imaging could not be performed. However, if anything, the presence of some players with a clinical or radiological history of stress fracture considered part of the non-stress fracture group in this study would have tended to minimize the differences between the groups. This study weakness itself appears to be unable to explain why the incidence of calf strain is so much higher in the group with a known history of stress fracture.
A further limitation is that injury sides and levels of stress fracture were not universally recorded and hence not included in the data analysis. It would strengthen the relationship further, for example, if it could be shown that history of left sided pars stress fracture at L5 level, for example, led to increased risk specifically of left calf strain. The converse appears to be more likely in that bowlers with a history of left (or non-dominant) side stress fracture are probably more likely to suffer from right (or dominant) calf strain. This is probably because the bowling mechanics (Figure 2) independently make non-dominant side stress fractures but dominant side calf strains more common. If it is presumed that there is a link between the two injuries then it must be taken for granted that non-dominant side stress fracture is associated with increased risk of degenerative changes or pars interarticularis hypertrophy in the lumbar spine on both non-dominant and dominant side of the relevant spinal level.
Being a univariate study, confounders may be responsible for some of the associations described. In particular, bowling speed and/or various techniques may be independently correlated with risk of lumbar stress fracture and risk of muscle strain.20
The study revealed an interesting inverse relationship between knee cartilage injury and lumbar stress fracture. This could perhaps be related to bowling mechanics (players who develop momentum more from run-up speed may be more likely to get knee injuries, whereas players who develop momentum more from body rotation may be more likely to suffer lumbar stress fractures). However, it is also potentially due to other confounders as there seems to be less biological explanation as to why a bowler with a history of lumbar stress fracture would be relatively immune from knee cartilage injury.
This study provides more direct evidence for the relationship between lumbar stress fractures and calf strains, as opposed to hamstring strains, as the observed correlation was much stronger. Hamstring strains are a more common injury in many sports and have subsequently been the focus of more research. If the lumbar-spine-hamstring injury nexus is accepted (which this study itself does not prove) it could help explain the observed relationship over many studies between hamstring weakness and hamstring injury susceptibility. Many previous studies have reported positively about this relationship,21–25 although one major study revealed no relationship.26 There is a study in which the rate of hamstring injuries in a college American football team was shown to decrease after a protocol was introduced to correct preseason strength deficits.27 The reduction of injuries was very impressive, but the intervention was not randomized and consequently confounding variables could not be excluded as having influenced the results. Individual strength results of players who sustained injuries were also not presented. The fact that the results from college American footballers have not been reproduced elsewhere in the following two decades suggests that reversal of subtle strength deficits may be very difficult, particularly in older players who are more susceptible to lumbar degenerative changes. If lumbar spine degenerative changes and/or bony hypertrophy were interacting to reduce hamstring strength in affected athletes, it could help to explain why low strength is both a risk factor but not necessarily easy to reverse. There has been a report of a correlation between hamstring-quadriceps ratio deficits and history of low-back injury,28 adding weight to this theory.
Despite the study limitations described, a lack of correlation between side and level of injury and failure to consider all confounding factors, this study provides further evidence that there is a relationship between history of lumbar spine injury and development of calf muscle strain. As the relationship between lumbar spine injury and hamstring strain was weaker, it is less supported by the data presented in this study, although it is certainly not refuted either.
The relationship between lumbar stress fracture history and calf strain supports the L5 nerve theory previously proposed.1 It suggests that if there is entrapment of the L5 nerve root that this may be occurring at the neural foramen (Figure 3 and 4(a), 4(b)). It adds justification to the procedure which is sometimes used in cricketers to prescribe imaging-guided lumbar cortisone injections around the nerve roots in cases of ‘muscle soreness’ which are strain mimicking but perhaps not true muscle strains.5 This study also adds further understanding of the pathogenesis of calf (and perhaps hamstring) strains in older athletes.
Figure 3.
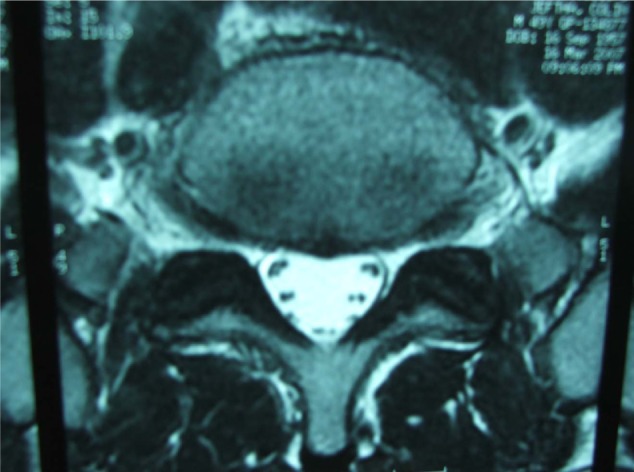
Axial MRI of lumbo-sacral junction, where it can be appreciated that L5 nerve may possibly be entrapped at the neural foramen by a protruding disc or bony hypertrophy.
Abbreviation: MRI, magnetic resonance imaging.
Figure 4(A).
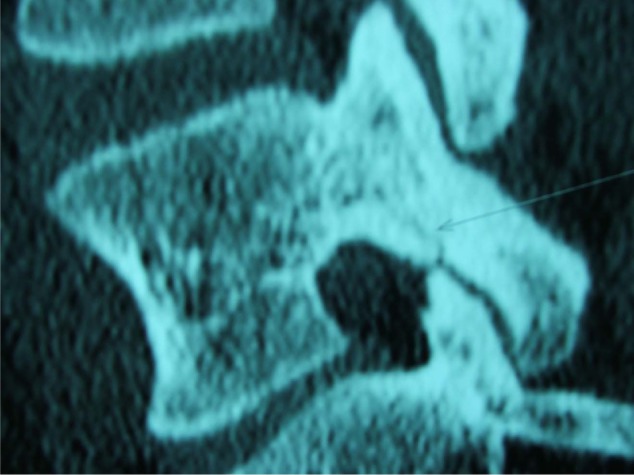
Coronal CT scan showing acute stress fracture, which may narrow the neural foramen if it heals with bony hypertrophy.
Abbreviation: CT, computed tomography.
Figure 4(B).
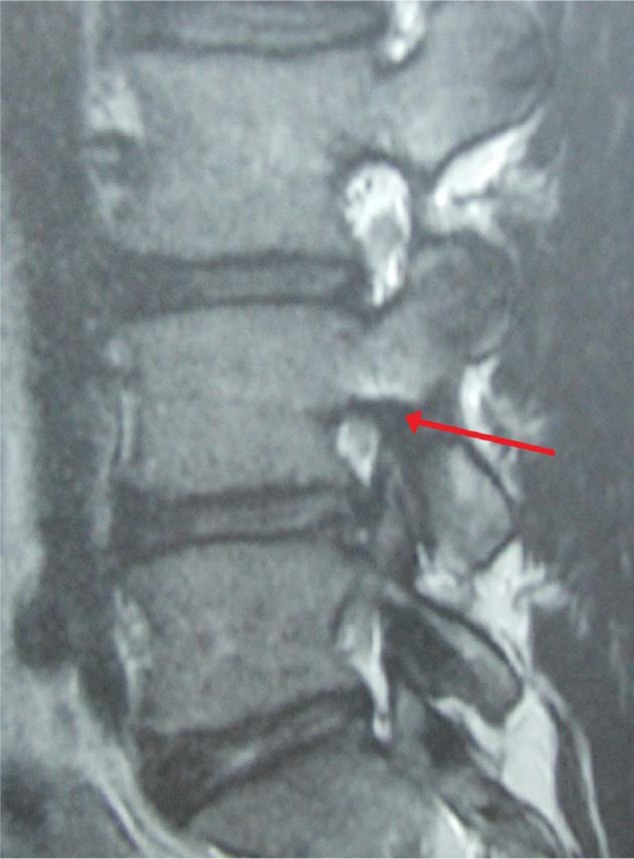
Coronal MRI scan showing narrowing of a neural foramen by apparent bony hypertrophy.
Abbreviation: MRI, magnetic resonance imaging.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Orchard J, Farhart P, Leopold C. Lumbar spine region pathology and hamstring and calf injuries in athletes: is there a connection? Br J Sports Med. 2004;38:502–504. doi: 10.1136/bjsm.2003.011346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jenis L, An H. Spine update. Lumbar foraminal stenosis. Spine. 2000;25(3):389–394. doi: 10.1097/00007632-200002010-00022. [DOI] [PubMed] [Google Scholar]
- 3.Ong A, Anderson J, Roche J. A pilot study of the prevalence of lumbar disc degeneration in elite athletes with lower back pain at the Sydney 2000 Olympic Games. Br J Sports Med. 2003;37:263–266. doi: 10.1136/bjsm.37.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orchard J. Intrinsic and extrinsic risk factors for muscle strain injury in Australian football. Am J Sports Med. 2001;29(3):300–303. doi: 10.1177/03635465010290030801. [DOI] [PubMed] [Google Scholar]
- 5.Szalai K, Illyes A. Sacral epidural steroid injection used for the prevention of hamstring injuries. Facta Univesitatis Series: Physical Education in Sport. 2005;3(1):37–44. http://facta.junis.ni.ac.yu/pe/pe2005/pe05-04.pdf [Google Scholar]
- 6.Engstrom C, Walker D. Pars interarticularis stress lesions in the lumbar spine of cricket fast bowlers. Med Sci Sports Exerc. 2007;39(1):28–33. doi: 10.1249/01.mss.0000241642.82725.ac. [DOI] [PubMed] [Google Scholar]
- 7.Elliott B, Hardcastle P, Burnett A, Foster D. The influence of fast bowling and physical factors on radiological features in high performance young fast bowlers. Sports Med Train Rehabil. 1992;3:113–130. [Google Scholar]
- 8.Annear PT, Chakera TM, Foster DH, Hardcastle PH. Pars interarticularis stress and disc degeneration in cricket’s potent strike force: the fast bowler. Aust N Z J Surg. 1992;62(10):768–773. doi: 10.1111/j.1445-2197.1992.tb06915.x. [DOI] [PubMed] [Google Scholar]
- 9.Bell PA. Spondylolysis in fast bowlers: principles of prevention and a survey of awareness among cricket coaches. Br J Sports Med. 1992;26(4):273–275. doi: 10.1136/bjsm.26.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foster D, John D, Elliott B, Ackland T, Fitch K. Back injuries to fast bowlers in cricket: a prospective study. Br J Sports Med. 1989;23(3):150–154. doi: 10.1136/bjsm.23.3.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hardcastle P. Lumbar pain in fast bowlers. Aust Fam Physician. 1991;20(7):943. 46–51. [PubMed] [Google Scholar]
- 12.Sys J, Michielsen J, Bracke P, Martens M, Verstreken J. Nonoperative treatment of active spondylolysis in elite athletes with normal X-ray findings: literature review and results of conservative treatment. Euro Spine J. 2001;10(6):498–504. doi: 10.1007/s005860100326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orchard J, James T, Alcott E, Carter S, Farhart P. Injuries in Australian cricket at first class level 1995/96 to 2000/01. Br J of Sports Med. 2002;36(4):270–275. doi: 10.1136/bjsm.36.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orchard J, James T, Portus M. Injuries to elite male cricketers in Australia over a 10-year period. J Sci Med Sport. 2006;9(6):459–467. doi: 10.1016/j.jsams.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Portus M, Galloway H, Elliott B, Lloyd D. Pathomechanics of lower back injuries in junior and senior fast bowlers: a prospective study. (Abstract) Sport Health. 2007;25(2):8–9. [Google Scholar]
- 16.Orchard J, Newman D, Stretch R, Frost W, Mansingh A, Leipus A. Methods for injury surveillance in international cricket. Br J of Sports Med. 2005;39(4):E22. doi: 10.1136/bjsm.2004.012732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orchard J, Newman D, Stretch R, Frost W, Mansingh A, Leipus A. Methods for injury surveillance in international cricket. J Sci Med Sport. 2005;8(1):1–14. doi: 10.1016/s1440-2440(05)80019-2. [DOI] [PubMed] [Google Scholar]
- 18.Hennekens C, Buring J. Epidemiology in Medicine. Boston: Little, Brown and Company; 1987. [Google Scholar]
- 19.Ranson C, Kerslake R, Burnett A, Batt M, Abdi S. Magnetic resonance imaging of the lumbar spine in asymptomatic professional fast bowlers in cricket. J Bone Joint Surg (Br) 2005;87(8):1111–1116. doi: 10.1302/0301-620X.87B8.16405. [DOI] [PubMed] [Google Scholar]
- 20.Portus M, Mason B, Elliott B, Pfitzner M, Done R. Technique factors related to ball release speed and trunk injuries in high performance cricket fast bowlers. Sports Biomechanics. 2004;3(2):263–284. doi: 10.1080/14763140408522845. [DOI] [PubMed] [Google Scholar]
- 21.Burkett LN. Causative factors in hamstring strains. Med Sci Sports. 1970;2(1):39–42. [PubMed] [Google Scholar]
- 22.Christensen C, Wiseman D. Strength, the common variable in hamstring strains. Athletic Training. 1972;7:36–40. [Google Scholar]
- 23.Yamamoto T. Relationship between hamstring strains and leg muscle strength. A follow-up study of collegiate track and field athletes. J Sports Med Phys Fitness. 1993;33(2):194–199. [PubMed] [Google Scholar]
- 24.Orchard J, Marsden J, Lord S, Garlick D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1997;25:81–85. doi: 10.1177/036354659702500116. [DOI] [PubMed] [Google Scholar]
- 25.Jonhagen S, Nemeth G, Eriksson E. Hamstring injuries in sprinters. the role of concentric and eccentric hamstring muscle strength and flexibility. Am J Sports Med. 1994;22:262–266. doi: 10.1177/036354659402200218. [DOI] [PubMed] [Google Scholar]
- 26.Bennell K, Wajswelner H, Lew P, Schall-Riaucour A, Leslie S, Plant D, et al. Isokinetic strength testing does not predict hamstring injury in Australian Rules footballers. Br J Sports Med. 1998;32:309–314. doi: 10.1136/bjsm.32.4.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heiser TM, Weber J, Sullivan G, Clare P, Jacobs RR. Prophylaxis and management of hamstring muscle injuries in intercollegiate football players. Am J Sports Med. 1984;12(5):368–370. doi: 10.1177/036354658401200506. [DOI] [PubMed] [Google Scholar]
- 28.Koutedakis Y, Frischknecht R, Murthy M. Knee flexion to extension peak torque ratios and low-back injuries in highly active individuals. Int J Sports Med. 1997;18:290–295. doi: 10.1055/s-2007-972636. [DOI] [PubMed] [Google Scholar]


