Abstract
Introduction
No data regarding the prevalence of the Brugada-type electrocardiogram (ECG) pattern and the early ventricular repolarization pattern (ERP) in the North African population were available. The aims of this study were to determine the frequency of Brugada-type ECG pattern and ERP in Tunisia and to evaluate ECG descriptors of ventricular repolarization in a population of athletes.
Methods
Over a 2-year period, resting 12-lead ECG recordings were analyzed from athletes (n = 540; 348 males; age 18.3 ± 2.4 years). Brugada-type ECG pattern was defined as Type 1, 2, or 3, and ERP was characterized by an elevation of the J point in the inferior and/or lateral leads. The population was divided into three groups of athletes: ERP group; Brugada-type ECG pattern group; and control group, with neither ERP nor Brugada ECG pattern. Clinical and electrocardiographic parameters were compared among the study groups.
Results
Nine subjects (1.66%) had a Brugada-type ECG pattern. None of them had the coved-type, 3 (0.6%) had the Type 2, and 6 (1.1%) had the Type 3. All subjects were asymptomatic. A Brugada-type ECG pattern was observed in seven males. No female had the Type 2 Brugada ECG pattern. ECG parameters were similar among Brugada-type ECG pattern and control athletes. ERP (119 subjects, 22%) was obtained in 98 males. Heart rate was lower, the QRS duration shorter and QT and Tpeak–Tend intervals were longer in ERP than control groups.
Conclusion
The results indicate that the frequency of the Brugada-type ECG pattern and ERP were respectively 1.66% and 22.00% in athletes, being more prevalent in males. The ERP group experienced shorter QRS duration and longer Tpeak–Tend interval than in the control population.
Keywords: J wave, ERP athletes, T wave
Introduction
The J wave is a defection immediately following the QRS complex of the surface electrocardiogram (ECG). When partially buried in the R wave, the J wave appears as J-point elevation or ST-segment elevation. Renewed interest in early repolarization arose after the discovery of an associated high risk of sudden cardiac death by ventricular fibrillation with both ST elevation in right precordial (V1–V3)1,2 and early repolarization in the inferior or mid to lateral precordial leads.3–5
Conflicting evidence exists on prevalence and prognostic significance of the Brugada-type ECG pattern and early ventricular repolarization pattern (ERP), particularly when found by chance in an asymptomatic individual and in an ethnic population where epidemiological data are lacking. To our knowledge, no data regarding the prevalence of the Brugada-type ECG pattern and the ERP exist in the North African population. The aim of this study was to determine the frequencies of the Brugada-type ECG pattern and ERP and to evaluate ECG descriptors of ventricular repolarization in a population of Tunisian athletes.
Methods
Subjects
Over a 2-year period (2008–2009), resting 12-lead ECG recordings were analyzed from athletes (n = 540; 348 males; 100% white Arabs, aged 18.3 ± 2.4 years, height = 172 ± 12 cm, weight = 63.6 ± 12.3 kg) as part of their physical examination. They were routinely controlled in the Central Sports Medicine Centre of El Menzah in Tunisia. The studied athletes represented 14 disciplines. All those who entered this study had no evidence of organic heart disease as judged from clinical history and physical and echocardiographic examination.
A 12-lead ECG (at a paper speed of 25 mm/s and 1 mV/10 mm standard gain) was recorded from each subject with the same equipment by the same person.
Brugada-type ECG pattern was defined as Type 1, 2, or 3. The consensus report of the Study Group of the Molecular Basis of Arrhythmias laid down precise diagnostic criteria for the Brugada-type ECG pattern,6,7 recognizing three variants of the repolarization pattern in chest leads V1–V3 (Type 1, classical convex ST elevation of ≥2 mm; Type 2, J wave amplitude ≥2 mm with concave ST elevation ≥ 1 mm; and Type 3, J point elevation with the ST segment isoelectric or elevated by <1 mm).
ERP was defined as elevation of the J point (QRS-ST junction) noted as either QRS slurring or notching ≥0.1 mV in more than two adjacent leads in the inferior leads (II, III, and aVF) and/or lateral leads (I, aVL, and V4 through V6).3
PR intervals, P wave duration and amplitude, T wave amplitude, and QRS amplitude were measured on lead II. P wave, T wave and QRS axis were calculated from frontal leads. The maximum QRS duration was assessed in any of the measurable leads of each ECG. Mean RR interval was also measured.
The interval from the peak to the end of the T wave (Tpeak–Tend) and the QT interval were measured on leads V2 or V3 and leads II or V5. The point of T wave offset was defined as the return to the baseline. Tpeak–Tend/QT ratio was also calculated.
QT intervals were corrected for heart rate using Fridericia’s [QTc Fri = QT(RR)−1/3] and Sagie-Framingham’s [QTcFr = QT + 0.154 (1000 – RR)] formulas.8,9
All ECG measurements were performed separately by two independent investigators who were blinded to the clinical data of the patients. The interpreters of the ECGs assessed also Brugada-type ECG patterns and ERP simultaneously. The averages of the measurements of the two observers were used for comparisons. The diagnosis of Brugada-type ECG pattern or ERP was made only when both investigators agreed on the classification of the ECG abnormalities.
The population was subsequently divided into three groups: ERP group; Brugada-type ECG pattern group; and control subjects, without either ERP or Brugada type ECG pattern. Clinical and ECG parameters were described for each group and compared with control groups.
Statistical analysis
The age, gender, and ECG findings of the cases were recorded with SPSS (version 12.0, SPSS, Inc, Chicago, IL). Values are expressed as the mean ± SD (standard deviation), n value, and percentage (%). Student’s t-test for independent samples and the chi-squared test were used, when appropriate, comparing two different groups. Two-sided P < 0.05 was considered significant. The study protocol was approved by the Ethics Committee of the Central Sports Medicine Centre of El Menzah in Tunisia.
Results
Prevalence of the Brugada-type ECG pattern
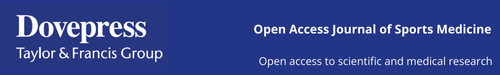
Among 540 athletes, we found nine subjects (1.66%) with a Brugada-type ECG pattern. All the subjects with the Brugada-type ECG pattern had a saddleback-type ECG abnormality and were asymptomatic. Three (0.6%) had the Type 2 (Figure 1), and six (1.1%) had the Type 3. A Brugada-type ECG pattern was obtained in two females and in seven males. No female had the Type 2, and none of the athletes displayed both ERP and Brugada-type ECG pattern.
Figure 1.
Type 2 Brugada-type ECG of an athlete demonstrates saddle-back type ST-segment elevation (>1 mm) in lead V2.
The mean age, mean body area, and mean systemic arterial pressure in Brugada-type ECG pattern athletes were respectively 19.3 ± 1.0 years, 1.77 ± 0.16 m², and 120 ± 18/74 ± 9 mmHg, that were similar to clinical control parameters. However, males are more prevalent in Brugada-type ECG pattern than control athletes (77.7% versus 58.9%; P < 0.0001). Mean ECG parameters are summarized in Table 1. Heart rate, PR interval, P wave duration and amplitude, T wave, P wave, QRS axis, QRS duration, QT intervals, corrected QT intervals, Tpeak–Tend intervals and Tpeak–Tend/QT ratio in Brugada-type ECG pattern group were not statistically different among control athletes.
Table 1.
Clinical and ECG parameters of study cohorts
| Parameter | ERP group | Control group | Brugada-type ECG pattern group | Pa |
|---|---|---|---|---|
| N (%) | 119 (22%) | 412 (76.3%) | 9 (1.7%) | |
| Male gender (n, %) | 98, 82.3% | 243, 58.9% | 7, 77.7% | 0.000 |
| Age (years) | 18.2 ± 2.3 | 18.1 ± 2.9 | 19.3 ± 1 | 0.6 |
| Body area (m²) | 1.78 ± 0.23 | 1.72 ± 0.19 | 1.77 ± 0.16 | 0.009 |
| Weight (kg) | 66.7 ± 12.4 | 62.7 ± 12.1 | 65 ± 9.9 | 0.002 |
| Height (cm) | 172.7 ± 19 | 171.6 ± 9 | 174.1 ± 7.9 | 0.375 |
| Systolic BP (mmhg) | 116 ± 12 | 115 ± 11 | 120 ± 18 | 0.81 |
| Diastolic BP (mmhg) | 70 ± 9 | 68 ± 10 | 74 ± 9 | 0.136 |
| RR (ms) | 867 ± 157 | 781 ± 145 | 815 ± 218 | 0.000 |
| PR interval (ms) | 143 ± 16 | 143 ± 21 | 145 ± 13 | 0.76 |
| QRS interval (ms) | 86 ± 10 | 89 ± 11 | 90 ± 13 | 0.005 |
| QRS axis (°) | 68 ± 25 | 67 ± 27 | 58 ± 26 | 0.9 |
| T axis (°) | 58 ± 18 | 55 ± 20 | 56 ± 7.5 | 0.19 |
| P axis (°) | 56 ± 25 | 56 ± 26 | 65 ± 10 | 0.97 |
| P wave duration (ms) | 94 ± 12 | 94 ± 12 | 98 ± 10 | 0.8 |
| QRS amplitude DII (mV) | 1.6 ± 0.4 | 1.4 ± 0.4 | 1.4 ± 0.7 | 0.000 |
| P wave amplitude DII (mV) | 0.14 ± 0.05 | 0.15 ± 0.05 | 0.160.04 | 0.2 |
| T wave amplitude DII (mV) | 0.48 ± 0.17 | 0.39 ± 0.18 | 0.32 ± 0.11 | 0.000 |
| QT interval DII or V5 (ms) | 389 ± 48 | 370 ± 27 | 366 ± 40 | 0.000 |
| QT interval V2 or V3 (ms) | 383 ± 38 | 370 ± 35 | 367 ± 37 | 0.001 |
| Fridericia c-QT DII or V5 (ms) | 405 ± 20 | 405 ± 27 | 394 ± 31 | 0.9 |
| Fridericia c-QT V2 or V3 (ms) | 403 ± 35 | 405 ± 37 | 396 ± 24 | 0.6 |
| Framingham c-QT DII or V5 (ms) | 405 ± 20 | 405 ± 27 | 394 ± 28 | 0.6 |
| Framingham c-QT V2 or V3 (ms) | 404 ± 33 | 404 ± 31 | 396 ± 24 | 0.8 |
| Tpeak-Tend DII or V5 (ms) | 88 ± 9 | 85 ± 10 | 82 ± 12 | 0.007 |
| Tpeak-Tend V2 or V3 (ms) | 103 ± 14 | 97 ± 14 | 95 ± 12 | 0.000 |
| Tpeak-Tend/QT V2 or V3 ratio | 0.26 ± 0.03 | 0.26 ± 0.07 | 0.25 ± 0.03 | 0.8 |
| Tpeak-Tend/QT Dii or V5 ratio | 0.22 ± 0.02 | 0.23 ± 0.02 | 0.22 ± 0.02 | 0.4 |
Note:
P value calculated between ERP group and control group.
Abbreviations: BP, blood pressure; c-QT, corrected QT interval; ECG, electrocardiogram; ERP, early repolarization pattern.
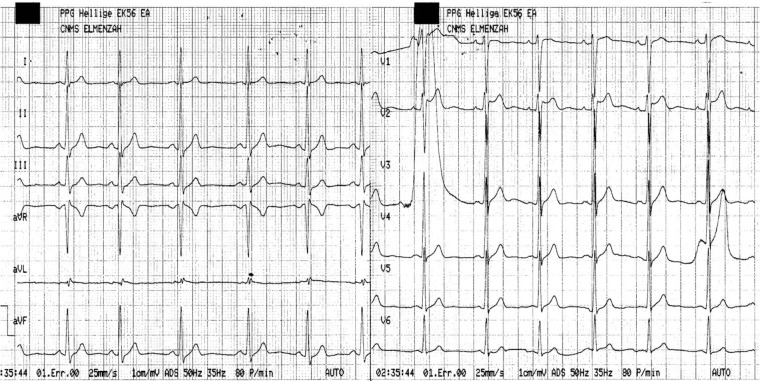
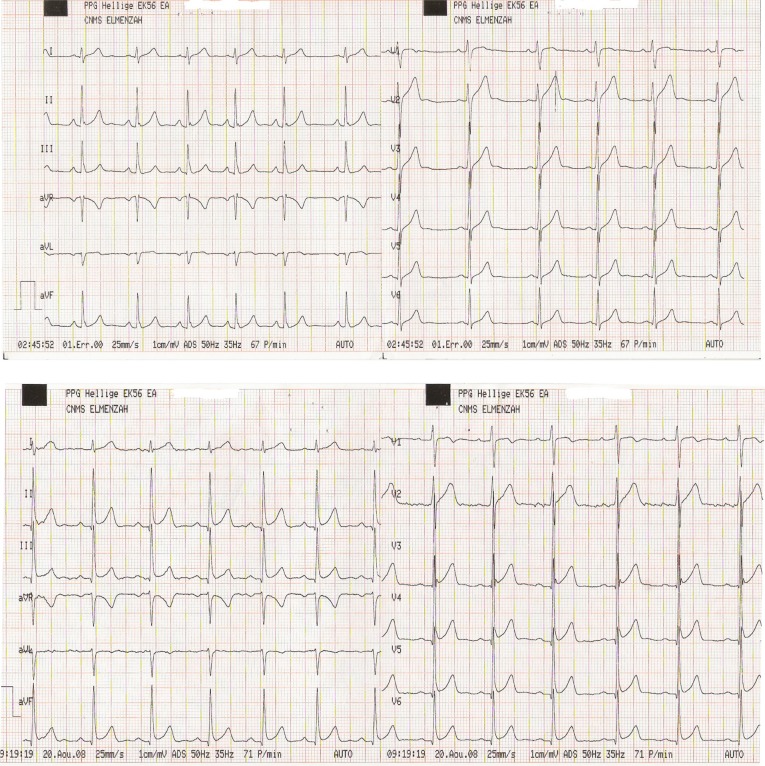
Prevalence of early ventricular repolarization pattern
A total of 119 ECGs (22%) were found to fulfill the criteria for ERP that was obtained in 98 males and in 21 females. Males are more prevalent in ERP than in control group (82.3% versus 58.9%; P < 0.0001).
ERP was present in the inferior leads (II, III, aVF) in 37 patients (31.1%), in the lateral leads (I, aVL, V4–V6) in 71 patients (59.6%), and in both the inferior and lateral leads in 11 patients (9.2%) (Figures 2A and 2B).
Figure 2.
Sample electrocardiograms from two athletes, demonstrating early ventricular repolarization (ERP)-type ECG. ERP defined as ≥1 mm elevation of the QRS–ST junction (J point) in either inferior leads (Type 2) (A) or inferior and lateral leads (Type 3) (B).
Weight and body area were significant, although only marginally higher in ERP athletes than in controls. Mean age, mean height, and systolic and diastolic blood pressure were similar between the two groups.
PR interval, P wave duration and amplitude, QRS, P wave, and T wave axis were similar between ERP group and controls. ERP athletes had lower heart rate, greater QRS and T wave amplitude, and a slightly but significantly shorter QRS duration than the controls.
The duration of the QT interval was longer in ERP athletes than in control athletes, but no difference was observed when the QT interval was corrected for heart rate (Table 1). Tpeak–Tend intervals were longer in the ERP athletes than in control athletes. However, Tpeak–Tend/QT ratio was not different between the two groups (Table 1).
Discussion
The frequency of Brugada-type ECG pattern and ERP were found to differ among ethnic groups. No data regarding the frequency of the J wave sign exist in North African populations.
Brugada-type ECG pattern
Our results indicate that the frequency of the Brugada-type ECG pattern was 1.66% in athletes, with a saddleback-type ECG abnormality in all cases. Epidemiological data suggest that Brugada-type ECG pattern is ubiquitous, but it varies significantly among ethnic populations, higher in south-eastern Asian countries, an event possibly reflecting the geographical genetic distribution of the disease.6,10 Large epidemiological information has been reported from Asian,11–21 European,22–30 and American31–34 populations, and the data available are difficult to compare because of differences in the diagnostic criteria applied, and differences in the characteristics of the populations selected (sex ratio, age, healthy subjects or tertiary hospital patients) (Table 2).
Table 2.
Comparison of the prevalence of Brugada-type ECG in different ethnic populations
| Study | Year of publication | Origin | N | Males (%) | Age (years) | Nature of population | Sex ratio of BS M/F | Prevalence of BS Type 1 (%) | Prevalence of all BS types (%) | FU | Sudden death during FU |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Asian population | |||||||||||
| Furuhashi et al11 | 2001 | Japan | 8612 | 69.5 | 49.2 (22–84) |
Health examination | 11/1 | 0.05 | 0.14 | NA | NA |
| Mastuo et al12 | 2001 | Japan | 4788 | 40.8 | 45 ± 10.5 | Health examination | 27/5 | NA | 0.14 | 41 years | 5 |
| Atarashi et al13 | 2001 | Japan | 10,000 | 89.1 | 42 ± 9 | Health examination | 16/0 | NA | 0.16 | NA | NA |
| Yamakawa et al14 | 2004 | Japan | 20,387 | 51.1 | 9.7 ± 3.2 | School children | 1/1 | 0.0049 | 0.0098 | NA | NA |
| Yoshinaga et al15 | 2004 | Japan | 7022 | 100 | 15 | Male adolescents | 7 | 0.06 | 0.1 | NA | NA |
| Oe etal16 | 2005 | Japan | 21,944 | 41.4 | 6–7 | Children, CBP | 2/2 | 0.005 | 0.02 | 6.8 ± 1 years | 0 |
| Babaee Bigi et al17 | 2007 | Iran | 3895 | 46 | 38.2 ± 11.9 | Tertiary hospital | 66/44 | 0.54 | 2.56 | NA | NA |
| Gervacio-Domingo et al18 | 2008 | Philippines | 3907 | NA | ≥20 | Healthy subjects | 68/26 | 0.2 | 2.1 | NA | NA |
| Wajed et al19 | 2008 | Pakistan | 1100 | 64.7 | NA | Healthy young students | 7/2 | NA | 0.8 | NA | NA |
| Tsuji et al20 | 2008 | Japan | 13,904 | 26 | 58 ± 10 | Health examination | 80/18 | 0.26 | 0.7 | 7.8 ± 1.6 years | 1 |
| Sidik et al21 | 2009 | China(br/)Singapore | 392 | 55.9 | 49.9 ± 19.1 | Tertiary medical center | 27/1 | 4.8 | 7.1 | 30.4 person-years | 0 |
| European population | |||||||||||
| Hermida et al22 | 2000 | France | 1000 | 63.2 | 39 ± 10 | Normal subjects | 52/9 | 0.1 | 0.61 | 49 ± 30 months | 0 |
| Viskin et al23 | 2000 | Israel | 592 | 58.4 | 36 ± 10 | Tertiary hospital | NA | 0 | NA | NA | |
| Bianco et al24 | 2001 | Italy | 155 | 100% | 30.9 ± 10.1 | Competitive athletes | 12 | 7.7 | NA | NA | NA |
| Junttila et al25 | 2004 | Finland | 2749 | 100% | 18–30 | Finnish air force | NA | 0 | 0.61 | 19 ± 2 years | 0 |
| Blangy et al26 | 2005 | France | 35,309 | 47% | 37.2 | Health examination | 14/6 | 0.016 | 0.05 | 30 months | 0 |
| Bozkurt et al27 | 2006 | Turkey | 1238 | 77.8% | 38.9 ± 17.6 | Tertiary hospital and university students | 5/1 | 0.08 | 0.48 | NA | NA |
| Letsas et al28 | 2007 | Greece | 11,488 | 57.7% | 15–98 | Tertiary hospital | 23/2 | 0.02 | 0.22 | 24 ± 12 months | 0 |
| Gallagher et al29 | 2008 | Italy | 12,012 | 90.8% | 29 ± 9 | Healthy subjects | 23/0 | 0.016 | 0.19 | 10.1 ± 5.5 years | 1 patient/0.3% per patient of year FU |
| Sinner et al30 | 2009 | German | 4149 | 49% | 50.6 ± 13.9 | General population | 0 | 0 | 0 | NA | NA |
| American population | |||||||||||
| Monroe and Littman31 | 2000 | USA | 12,000 | NA | NA | Urban teaching hospital | NA | 0.016 | 0.43 | NA | NA |
| Greer and Glancy32 | 2003 | USA | 27,328 | NA | NA | Medical center | NA | 0 | 0.065 | NA | NA |
| Donohue and 33 | 2008 | USA | 1348 | NA | 52.7 ± 16.2 | Tertiary hospital | 1/1 | 0 | 0.14 | NA | NA |
| Patel et al34 | 2009 | USA | 162,590 | NA | NA | Tertiary medical center | 13/7 | 0.005 | 0.012 | NA | NA |
| North African population | |||||||||||
| This study | 2010 | Tunisia | 540 | 348 | 18.3 ± 2.4 | Athletes | 7/2 | 0 | 1.16 | NA | NA |
Abbreviations: BS, Brugada sign; FU, follow-up; F, female; M, male; NA, not available; CBP, community-based population.
In accordance with different studies,23,25,30 we did not document any person with Brugada Type 1 ECG pattern.
Considering the dynamic nature of the ECG features, the true incidence of Brugada-type ECG pattern might have been underestimated.29
Only one previous study had evaluated the prevalence of Brugada-type ECG pattern in an athletic cohort of 155 males with a reported prevalence of 7.7%, with a Brugada Type 1 ECG pattern in all cases.24
The disparities between the present study and the Bianco et al study24 may be explained by differences between the two study populations. Bianco et al have included only males, older (mean age of the population: 30.9 ± 10.1 years), and competitive athletes.24
In southern Europe, Hermida et al22 found a high prevalence of concave ST-segment elevation in 1000 European men (6%) and a far lower prevalence of convex ST-segment elevation (0.1%). Monroe and Littman31 found 52 cases of the Brugada-type ECG among approximately 12,000 unselected noncardiac hospitalized patients. In their report, the convex pattern was present in only two cases. In adolescents and in school children, the frequency of Brugada-type ECG pattern was very low even in regions of Southeast Asia where the Brugada syndrome is endemic.14–16 Yamakawa et al14 have demonstrated a tendency for the prevalence of Brugada-type ECG pattern to increase with age. In the present study, we did not evaluate the prognostic value of Brugada type ECG pattern. Previous studies have suggested that Brugada-type ECG pattern has a benign natural course, independent of the ethnic origin of the study population.12,20,21,28,29
ERP
Of our healthy “young athletes”, 22% had J-point elevation, a figure consistent with the 22%35 to 27%37 of young athletes with J-point elevation reported by others.35–37 Bianco et al24 identified a higher ERP prevalence (89%) in their competitive athlete group (age 30.9 ± 10.1 years). The athletes included in our study and those described by Rosso et al35 were noncompetitive.
The ERP has long been considered to be a “benign” ECG manifestation that is seen more commonly in young healthy men and athletes.37–40 No athletes with ERP, reported by Bianco et al24 had suffered from major ventricular arrhythmias from the time of the study (2001) onward to 2009.40 However, mounting evidence suggests that the ERP may be associated with a risk for ventricular fibrillation, depending on the location of ERP, magnitude of the J wave, and degree of ST elevation.3–5,41,42
Recently, Sinner et al42 have reported a high prevalence of ERP (13.1%) in a population-based cohort of middle-aged individuals (35–74 years). After a mean follow-up of 18.9 years, ERP was associated with about a 2–4-fold increased risk of cardiac mortality in individuals between 35 and 54 years. An inferior localization of ERP was associated with a particularly increased risk.42
Heart rate was found to be lower in ERP subjects than in controls, as previously reported.24,37,43,44 A greater vagotonia in ERP subjects has been previously reported as a possible contributing factor.37,43 The distribution of J-point elevation in our study was similar to that described by Rosso et al.35 Athletes had more commonly J-point elevation in lateral leads (V4–V6, Type 1) than in the inferior leads (Type 2).
The QRS duration was significantly shorter in ERP athletes than in controls. This is in accordance with previously published data,24 but discordant with the Dilaveris et al study.44 Disparities may be explained by differences in the populations studied and possible differences in the level of physical conditioning.
In accordance with previous publications, mean QT duration was significantly higher in ERP athletes than in control athletes.24,37,44 However, corrected QT intervals were similar between these two groups, which is in accordance with the Mehta and Jain study37 but in contrast with other studies finding lower corrected QT in ERP subjects than in controls.44 Tpeak–Tend intervals were significantly higher in ERP than in control athletes. Tpeak–Tend/QT ratio showed no difference between these two groups.
Study limitations
First, considering the dynamic nature of the ECG features, the true prevalence of Brugada-type ECG pattern and ERP might have been underestimated in this study. Second, we have identified differences in QT duration on leads V2 and II, which may be explained by differences in the projection of the T-wave loop between the ECG leads, or may simply be due to inaccuracies in defining the end of the T wave. Third, the physical activity level depending on the corresponding disciplines was not evaluated. Therefore, possible association between the presence of ERP and the athlete discipline was not investigated. Finally, no follow-up was described to ERP and Brugada-type ECG pattern, so no prognostic value of these ECG patterns were available.
Conclusion
The results indicate that the frequency of the Brugada-type ECG pattern and ERP were respectively 1.66% and 22% in athletes, being more prevalent in males. These results are similar to the findings of studies performed in European and American countries. ERP was associated with shorter QRS duration and longer Tpeak–Tend interval. Further population-based investigation is warranted to determine the prognostic value of the J-point elevation.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20(6):1391–1396. doi: 10.1016/0735-1097(92)90253-j. [DOI] [PubMed] [Google Scholar]
- 2.Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998;97(5):457–460. doi: 10.1161/01.cir.97.5.457. [DOI] [PubMed] [Google Scholar]
- 3.Haissaguerre M, Derval N, Sacher F, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008;358(19):2016–2023. doi: 10.1056/NEJMoa071968. [DOI] [PubMed] [Google Scholar]
- 4.Nam GB, Kim YH, Antzelevitch C. Augmentation of J waves and electrical storms in patients with early repolarization. N Engl J Med. 2008;358(19):2078–2079. doi: 10.1056/NEJMc0708182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tikkanen JT, Anttonen O, Junttila MJ, et al. Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med. 2009;361(26):2529–2537. doi: 10.1056/NEJMoa0907589. [DOI] [PubMed] [Google Scholar]
- 6.Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference. Heart Rhythm. 2005;2(4):429–440. doi: 10.1016/j.hrthm.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Wilde AA, Antzelevitch C, Borggrefe, et al. Proposed diagnostic criteria for the Brugada syndrome: consensus report. Circulation. 2002;106(19):2514–2519. doi: 10.1161/01.cir.0000034169.45752.4a. [DOI] [PubMed] [Google Scholar]
- 8.Fridericia LS. Die systolenduer im elektrokardiogramm bei normalen menschen und bei herzkranken. Acta Med Scand. 1920;53:469–486. [Google Scholar]
- 9.Sagie A, Larson MG, Goldberg RJ, Bengtson JR, Levy D. An improved method for the adjusting the QT interval for heart rate (The Framigham Heart Study) Am J Cardiol. 1992;70(7):797–801. doi: 10.1016/0002-9149(92)90562-d. [DOI] [PubMed] [Google Scholar]
- 10.Benito B, Brugada J, Brugada P. Brugada syndrome. Prog Cardiovasc Dis. 2008;51(1):1–22. doi: 10.1016/j.pcad.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Furuhashi M, Uno K, Tsuchihashi K, et al. Prevalence of asymptomatic ST segment elevation in right precordial leads with right bundle branch block (Brugada-type ST shift) among the general Japanese population. Heart. 2001;86(2):161–166. doi: 10.1136/heart.86.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matsuo K, Akahoshi M, Nakashima E, et al. The prevalence, incidence and prognostic value of the Brugada type electrocardiogram: a population-based study of four decades. J Am Coll Cardiol. 2001;38(3):765–770. doi: 10.1016/s0735-1097(01)01421-8. [DOI] [PubMed] [Google Scholar]
- 13.Atarashi H, Ogawa S, Harumi K, et al. Idiopathic Ventricular Fibrillation Investigators Three-year follow-up of patients with right bundle branch block and ST segment elevation in the right precordial leads: Japanese Registry of Brugada Syndrome. Idiopathic Ventricular Fibrillation Investigators. J Am Coll Cardiol. 2001;37(7):1916–1920. doi: 10.1016/s0735-1097(01)01239-6. [DOI] [PubMed] [Google Scholar]
- 14.Yamakawa Y, Ishikawa T, Uchino K, et al. Prevalence of right bundle-branch block and right precordial ST-segment elevation (Brugada-type electrocardiogram) in Japanese children. Circ J. 2004;68(4):275–279. doi: 10.1253/circj.68.275. [DOI] [PubMed] [Google Scholar]
- 15.Yoshinaga M, Anan R, Nomura Y, et al. Prevalence and time of appearance of Brugada electrocardiographic pattern in young male adolescents from a three-year follow-up study. Am J Cardiol. 2004;94(9):1186–1189. doi: 10.1016/j.amjcard.2004.07.092. [DOI] [PubMed] [Google Scholar]
- 16.Oe H, Takagi M, Tanaka A, et al. Prevalence and clinical course of the juveniles with Brugada-type ECG in Japanese population. Pacing Clin Electrophysiol. 2005;28(6):549–554. doi: 10.1111/j.1540-8159.2005.40020.x. [DOI] [PubMed] [Google Scholar]
- 17.Babaee Bigi MA, Aslani A, Shahrzad S. Prevalence of Brugada sign in patients presenting with palpitation in southern Iran. Europace. 2007;9(4):252–255. doi: 10.1093/europace/eum023. [DOI] [PubMed] [Google Scholar]
- 18.Gervacio-Domingo G, Isidro J, Tirona J, et al. The Brugada type 1 electrocardiographic pattern is common among Filipinos. J Clin Epidemiol. 2008;61(10):1067–1072. doi: 10.1016/j.jclinepi.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 19.Wajed A, Aslam Z, Abbas SF, et al. Frequency of Brugada-type ECG pattern (Brugada sign) in an apparently healthy young population. J Ayub Med Coll Abbottabad. 2008;20(3):121–124. [PubMed] [Google Scholar]
- 20.Tsuji H, Salto T, Morisaki K, Iwasaka T. Prognosis of subjects with Brugada-type electrocardiogram in a population of middle-aged Japanese diagnosed during a health examination. Am J Cardiol. 2008;102(5):584–587. doi: 10.1016/j.amjcard.2008.04.066. [DOI] [PubMed] [Google Scholar]
- 21.Sidik NP, Quay CN, Loh FC, Chen LY. Prevalence of Brugada sign and syndrome in patients presenting with arrhythmic symptoms at a Heart Rhythm Clinic in Singapore. Europace. 2009;11(5):650–656. doi: 10.1093/europace/eup079. [DOI] [PubMed] [Google Scholar]
- 22.Hermida JS, Lemoine JL, Aoun FB, Jarry G, Rey JL, Quiret JC. Prevalence of the Brugada syndrome in apparently healthy population. Am J Cardiol. 2000;86(1):91–94. doi: 10.1016/s0002-9149(00)00835-3. [DOI] [PubMed] [Google Scholar]
- 23.Viskin S, Fish R, Eldar M, et al. Prevalence of the Brugada sign in idiopathic ventricular fibrillation and healthy controls. Heart. 2000;84(1):31–36. doi: 10.1136/heart.84.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bianco M, Bria S, Gianfelici A, Sanna N, Palmieri V, Zeppilli P. Does early repolarization in the athlete have analogies with the Brugada syndrome? Eur Heart J. 2001;22(6):504–510. doi: 10.1053/euhj.2000.2247. [DOI] [PubMed] [Google Scholar]
- 25.Junttila MJ, Raatikainen MJ, Karjalainen J, Kauma H, Kesaniemi YA, Huikuri HV. Prevalence and prognosis of subjects with Brugada-type ECG pattern in a young and middle aged Finnish population. Eur Heart J. 2004;25(10):874–878. doi: 10.1016/j.ehj.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 26.Blangy H, Sadoul N, Coutelour JM, et al. Prevalence of Brugada syndrome among 35309 inhabitants of Lorraine screened at a preventive medicine centre. Arch Mal Coeur Vaiss. 2005;98(3):175–180. [PubMed] [Google Scholar]
- 27.Bozkurt A, Yas D, Seydaoglu G, Acarturk E. Frequency of Brugada-type ECG pattern (Brugada sign) in southern Turkey. Int Heart J. 2006;47(4):541–547. doi: 10.1536/ihj.47.541. [DOI] [PubMed] [Google Scholar]
- 28.Letsas K, Gavrielatos G, Efremidis M, et al. Prevalence of Brugada sign in a Greek tertiary hospital population. Europace. 2007;9(11):1077–1080. doi: 10.1093/europace/eum221. [DOI] [PubMed] [Google Scholar]
- 29.Gallagher MM, Forleo GB, Behr ER, et al. Prevalence and significance of Brugada-type ECG in 12,012 apparently healthy European subjects. Int J Cardiol. 2008;130(1):44–48. doi: 10.1016/j.ijcard.2007.07.159. [DOI] [PubMed] [Google Scholar]
- 30.Sinner MF, Pfeufer A, Perz S, et al. Spontaneous Brugada electrocardiogram patterns are rare in the German general population: results from the KORA study. Europace. 2009;11(10):1338–1344. doi: 10.1093/europace/eup205. [DOI] [PubMed] [Google Scholar]
- 31.Monroe MH, Littman L. Two-year case collection of the Brugada syndrome electrocardiogram pattern at a large teaching hospital. Clin Cardiol. 2000;23(11):849–851. doi: 10.1002/clc.4960231112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greer RW, Glancy DL. Prevalence of the Brugada electrocardiographic pattern at the Medical Center of Louisiana in New Orleans. J La State Med Soc. 2003;155(5):242–246. [PubMed] [Google Scholar]
- 33.Donohue D, Tehrani F, Jamehdor R, Lam C, Movahed MR. The prevalence of Brugada ECG in adult patients in a large university hospital in the western United States. Am Heart Hosp J. 2008;6(1):48–50. doi: 10.1111/j.1751-7168.2008.06418.x. [DOI] [PubMed] [Google Scholar]
- 34.Patel SS, Anees S, Ferrick KJ. Prevalence of a Brugada pattern electrocardiogram in an urban population in the United States. Pacing Clin Electrophysiol. 2009;32(6):704–708. doi: 10.1111/j.1540-8159.2009.02354.x. [DOI] [PubMed] [Google Scholar]
- 35.Rosso R, Kogan E, Belhassen B, et al. J-point elevation in survivors of primary ventricular fibrillation and matched control subjects. J Am Coll Cardiol. 2008;52(15):1231–1238. doi: 10.1016/j.jacc.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 36.Gussak I, Antzelevitch C. Early repolarization syndrome: clinical characteristics and possible cellular and ionic mechanisms. J Electrocardiol. 2000;33(4):299–309. doi: 10.1054/jelc.2000.18106. [DOI] [PubMed] [Google Scholar]
- 37.Mehta MC, Jain AC. Early repolarization on scalar electrocardiogram. Am J Med Sci. 1995;309(6):305–311. doi: 10.1097/00000441-199506000-00001. [DOI] [PubMed] [Google Scholar]
- 38.Wasserburger RH, Alt WJ. The normal RS-T segment elevation variant. Am J Cardiol. 1961;8:184–192. doi: 10.1016/0002-9149(61)90204-1. [DOI] [PubMed] [Google Scholar]
- 39.Ya n GX, Lankipalli RS, Burke JF, Musco S, Kowey PR. Ventricular repolarization components on the electrocardiogram: cellular basis and clinical significance. J Am Coll Cardiol. 2003;42(3):401–409. doi: 10.1016/s0735-1097(03)00713-7. [DOI] [PubMed] [Google Scholar]
- 40.Bianco M, Zeppilli P. Early repolarization in the athletes. J Am Coll Cardiol. 2009;53:2200. doi: 10.1016/j.jacc.2009.01.070. [DOI] [PubMed] [Google Scholar]
- 41.Kalla H, Yan GX, Marinchak R. Ventricular fibrillation in a patient with prominent J (Osborn) waves and ST segment elevation in the inferior electrocardiographic leads: a Brugada syndrome variant? J Cardiovasc Electrophysiol. 2000;11(1):95–98. doi: 10.1111/j.1540-8167.2000.tb00743.x. [DOI] [PubMed] [Google Scholar]
- 42.Sinner MF, Reinhard W, Müller M, et al. Association of early repolarization pattern on ECG with risk of cardiac and all-cause mortality: a population-based prospective cohort study (MONICA/KORA) PLoS Med. 2010;7(7):e1000314. doi: 10.1371/journal.pmed.1000314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haydar ZR, Brantley DA, Gittings NS, Wright JG, Fleg JL. Early repolarization: an electrocardiographic predictor of enhanced aerobic fitness. Am J Cardiol. 2000;85(2):264–266. doi: 10.1016/s0002-9149(99)00632-3. [DOI] [PubMed] [Google Scholar]
- 44.Dilaveris P, Pantazis A, Gialafos E, Gialafos J, Toutouzas P, Stefanadis C. Assessment of ventricular repolarization alterations in subjects with early repolarization. Int J Cardiol. 2004;96(2):273–279. doi: 10.1016/j.ijcard.2003.07.020. [DOI] [PubMed] [Google Scholar]