Abstract
Background
We describe a runner who completed a self-paced marathon (42.195 km) in a climate chamber with a temperature difference of 100°C, starting at an ambient temperature (Tambient) of −45°C and finishing at an Tambient of +55°C.
Methods
Tambient was set at −45°C at the start, and was steadily increased at a rate of 1°C at 4.5-minute intervals to +55°C. Before the start, after every 10.5 km, and at the end of the marathon, body mass, urine, and sweat production were measured and samples of venous blood and urine were collected. The runner’s temperature was recorded every 10 seconds at four sites, ie, the rectum for body core temperature (Tcore), and at the forehead, right wrist, and right ankle for surface temperatures (Tskin).
Results
The subject took 6.5 hours to complete the marathon, during which Tcore varied by 0.9°C (start 37.5°C, peak 38.4°C). The largest difference (∆) of Tskin was recorded at the ankle (∆16°C). The calculated amount of sweat produced increased by 888% from baseline. In the blood samples, myoglobin (+250%) showed the highest change. Of the pituitary hormones, somatotropic hormone (+391%) and prolactin (+221%) increased the most. Regarding fluid regulation hormones, renin (+1145%) and aldosterone (+313%) showed the greatest increase.
Conclusion
These results show that running a marathon in a climate chamber with a total ∆Tambient of 100°C is possible, and that the Tambient to Tcore relationship is maintained. These results may offer insight into regulatory mechanisms to avoid hypothermia and hyperthermia. The same study is to be performed using more subjects with the same characteristics to validate the present findings.
Keywords: endocrine regulation, thermoregulation, skin temperature, ambient temperature, sweat production
Introduction
Marathon running has become increasingly popular over recent years.1,2 However, many athletes are not satisfied with a classic marathon, so have searched for new running challenges over longer distances than the original distance of 42.195 km3 or running under extreme circumstances, such as extreme heat or extreme cold. To address this affinity for novel running challenges, new events such as ultramarathons in the heat, eg, the Marathon des Sables (www.darbaroud.com), the Badwater ultramarathon (www.badwater.com), and the Kalahari Augrabies extreme marathon (www.extrememarathons.com/augrabies), as well as marathons in extremely low temperatures, such as the Baikal Ice marathon (www.baikal-marathon.com) and the Antarctic Ice marathon (www.icemarathon.com), have been created.
Such extreme physical endurance performance requires a multitude of body systems to interact during both thermogenesis and thermolysis.4 For decades, these unique opportunities with regard to the limits of the different systems maintaining temperature homeostasis in marathoners have been investigated. Buskirk and Beetham5 were the first to report on measurements of post-race rectal temperatures and dehydration in marathoners. The importance of recognizing internal and external influences affecting body core temperature (Tcore) has been observed and modeled by Werner.6 Furthermore, Cheuvront and Haymes performed the first thermoregulation study in female marathoners.7 In 2001, the same authors4 evaluated the recent accumulation of literature with regard to thermoregulation in marathon running and the roles of environment,8–10 dehydration,5,11 metabolic rate,12,13 and gender.14 The proposed concepts dealt with describing how thermoregulation was utilized, whereupon the definition of regulated Tcore in the thermoregulatory system was introduced. The definition of new regulated Tcore (higher or lower from initial Tcore) determined the range of normothermia if an overall ambient temperature (Tambient) to Tcore relationship showed a stable Tcore over a certain time period, and thus, Tcore was autonomically regulated according to variation in Tambient.
Metabolic responses, such as an increase in creatinine, creatine kinase, white blood cell count, and myoglobin, during marathon running have previously been investigated.15 Numerous studies have examined physiologic responses during marathons performed in cold (12°C or lower) environments.12,16–18 On the other hand, there are few studies regarding marathons performed in hot environments.19,20 There is very little research on human athletic performances in unusually extreme environmental conditions. One of the rare examples was a Bushman hunter who was studied because he could hunt for 4–6 hours in the desert at a Tambient of 40–46° and cross more than 30 km, while drinking only about 1 L of water.21
Adams et al systematically examined the effect of Tambient by having one individual running three marathons at the same pace on a treadmill, while confronted with an airflow equivalent of a running speed in a cool (Tambient 10.0°C), moderate (Tambient 22.0°C), or hot (Tambient 35.4°C) environment.16 However, due to the fact that most of the other marathons studied were performed in field conditions, the meteorotropic effect may have changed during our study marathon. For example, differences in Tambient during marathon running in the field have been reported to be as much as 17°C from start to finish.22 However, it is not known how the human thermoregulatory system reacts to extremely cold conditions (−45°C and 60% relative humidity) of Tambient at the beginning of a marathon and extremely high conditions (+55°C and 20% relative humidity) of Tambient at the end of a marathon. Do the thermodynamic properties of the environment add to endogenous (ie, muscle work) heat load limiting thermoregulation in this case? To our knowledge, no study has previously investigated a case under such circumstances, where parameters are exactly modulated and measured in a climate chamber.
In the present case report, we describe a runner attempting to finish a self-paced marathon in a climate chamber with a temperature difference of 100°C. It was the intention of the athlete to be the first runner in history to complete a marathon in a climate chamber while overcoming a Tambient difference of 100°C (373°K). We evaluated how Tcore changed compared with skin temperature (Tskin), and how hormone metabolism changed when exposed to a total Tambient difference of 100°C (373°K) in one well experienced male marathoner. We hypothesized that running a marathon with a total Tambient difference of 100°C would be possible and that Tcore would remain stable, while Tskin would change depending on Tambient. Further metabolic responses as reported by Kratz et al might be accentuated by adding heat stress to exhausting exercise, such as in a marathon.15 A rise in Tambient would stimulate the release of pituitary hormones, such as prolactin which, among others, are a response by the central nervous system to avoid hyperthermia.
Materials and methods
Experimental design
This was a single-subject observational case study monitoring changes in body mass, and hematologic, urinary, and biochemical parameters while running a marathon in a climate chamber in order to overcome a total Tambient difference of 100°C. Tambient was set at −45°C at the start of the marathon and steadily increased to +55°C by the end of the marathon. This human experiment was approved by the director of the Brandenburg Technische Universität, Cottbus, Germany.
Subject
The subject was a 30-year old male with a body height of 1.80 m, a body mass of 93.8 kg, and a body mass index of 29.0 kg/m2. He was an experienced ultraendurance athlete (world champion in the Deca Iron ultratriathlon 2008, a world record holder in the 10-day triathlon, a finisher of the Trans Europe Footrace in 2009 and of the Race across Germany in 2010), and intending to run the first marathon in history under these conditions.
Preliminary test
One day before the experiment, a maximal treadmill test was performed to determine maximum oxygen uptake (VO2max). A running speed of 8.0 km/hour was set as the start speed. Every 3 minutes, the treadmill speed was increased by 2 km/hour until volitional fatigue. VO2 was determined using an expired air analysis by Meta Max 3B® (Cortex Biophysik GmbH, Leipzig, Germany) and heart rate was measured using a portable heart rate monitor (RCX5, Polar Electro Oy, Kempele, Finland). Lactate threshold was determined using Ergonizer version 3.2.1 (K. Röcker, www.ergonizer.de) to enable data analysis.
Climate chamber marathon
For the experiment, the athlete ran clockwise laps of 17.6 m in the climate chamber at the CEBra (Centrum für Energietechnologie Brandenburg) of Brandenburg Technische Universität in Cottbus, Germany (www.tu-cottbus.de/cebra). The investigating team was located outside the climate chamber. Each lap was counted using a laser-assisted photoelectric barrier. A computer counted the laps continuously and showed the distance covered at each moment.
During the marathon, Tcore was measured in the rectum along with Tskin at three sites. Before the start, after 10.5 km, 21.1 km, 31.6 km, and at the end of the study, venous blood samples were drawn, urine and sweat were collected, and body mass was measured. Each measurement took on average 10 (8–12) minutes. The athlete changed clothes for comfort during the breaks. He started running with winter boots, winter gloves, a winter jacket, and a winter hat over his running clothes. After 10.5 km (at about −20°C), no changes in clothing were made. After 21.1 km (approximately +5°C), he took off his winter clothes and ran in his usual running clothes. After 31.6 km (around +30°C), he took off his shirt. Ratings of perceived exertion were not recorded. The hydration status of the athlete was not assessed before the marathon and he consumed food and drinks as he was used to doing during his races.
Temperature and humidity in climate chamber
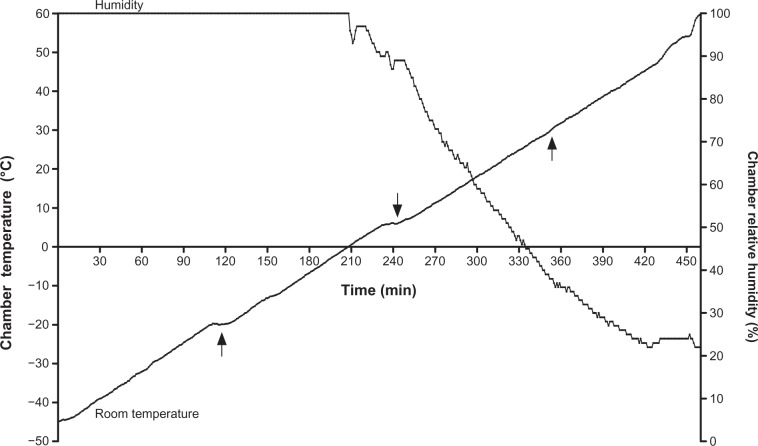
Tambient was set at −45°C at the start and continuously increased to +55°C (Figure 1) at a rate of 1°C per 4.5-minute interval. At the start, humidity was set at 60%. After 210 minutes of running at an Tambient of 0°C, humidity was steadily reduced until it reached 20% by the end of the marathon. Temperature and humidity in the climate chamber were recorded every minute. Percent change was rounded to two decimal digits.
Figure 1.
Room temperature and relative humidity of the climate chamber as a function of race time.
Note: Arrows indicate points during the race when the athlete was allowed to leave the chamber in order to undergo a medical examination.
Food and drinks
The day before the climate chamber marathon, the athlete went with his crew to a supermarket to buy conventional food, such as bread, meat, cheese, fruit, and fluids, including mineral water and soft drinks. The athlete consumed food and drinks ad libitum during the marathon. All food and drinks were provided at ambient room temperature. At each point of measurement, his coached prepared the food and drinks as requested by the athlete. Intake of food and drinks was recorded to estimate the fluid and energy intake in a cumulative histogram (Figure 2). The composition of the fluids and solid food was estimated using the information on the products consumed by the athlete and a nutrition chart.23
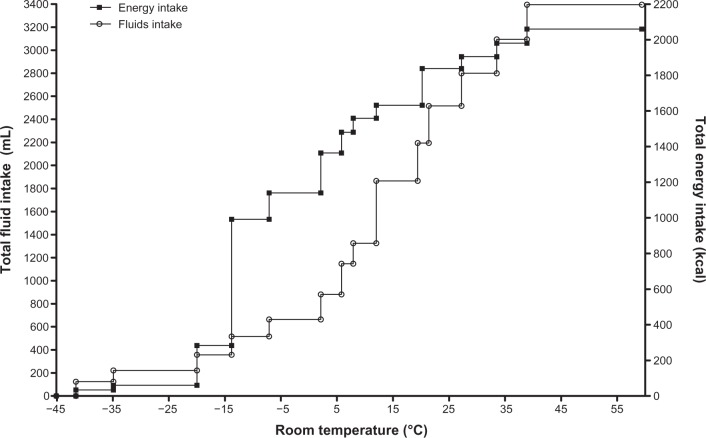
Figure 2.
Fluid intake and energy during the marathon run.
Estimation of sweat production
While running, sweat was collected using a plastic bag attached to a 17 × 25 cm area on the back of the runner. To estimate total sweat production, the sweat produced on this area of the back was extrapolated to the whole body surface area. Body surface area (BSA) was estimated using the formula BSA = weight (kg)0.425 × height (m)0.725 × 0.007184 following Dubois and Dubois.24
Heart rate
Heart rate was recorded continuously during the marathon using a portable heart rate monitor (RCX5, Polar Electro Oy) to estimate energy expenditure, using the heart rate method.25
Temperature
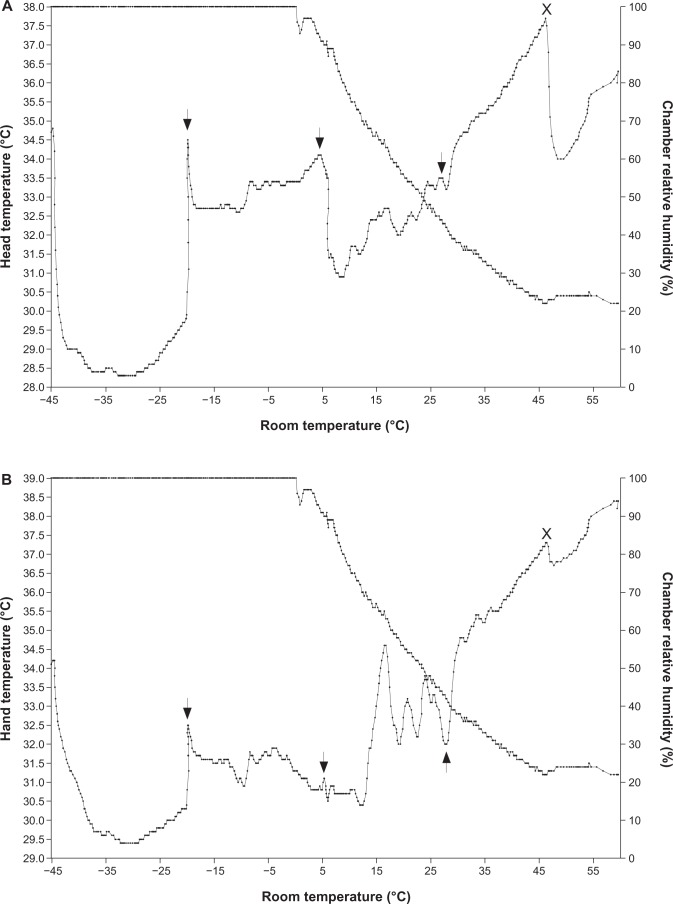
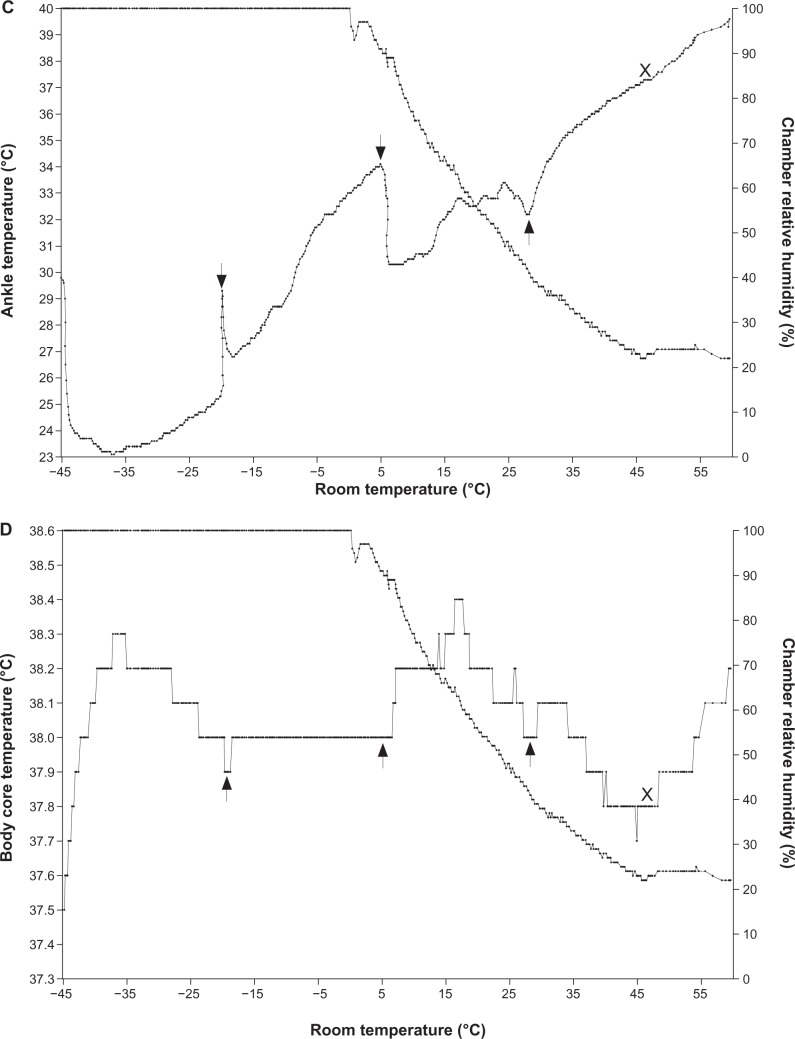
Tcore in the rectum and Tskin on the forehead, right wrist, and right ankle were measured using an EndoTherm Med® device (EndoTherm GmbH, Arlesheim, Switzerland) every 10 seconds while running. The EndoTherm Med thermoelectric probes sensor has a guaranteed accuracy of 0.0625°C. The sensor for measurement of Tcore in the rectum was encased in a silicone capsule and packed into a fingerstall. The sensors used to measure Tskin were fixed using textile ribbons on defined spots. The sensors were evaluated by EndoTherm Control software (www.endotherm.ch) and showed a temperature variation of ±0.1°C (Figure 3).
Figure 3.
Relative humidity in the climate chamber as well as skin temperature taken at the head (A), hand (B), and ankle (C), and body core temperature (D) as a function of room temperature.
Notes: Arrows indicate points during the race when the athlete was allowed to leave the chamber in order to undergo a medical examination. X indicates external cooling (one 0.8 L bottle of water at room temperature poured over the athlete’s head and body).
Laboratory measurements
Before the start of the marathon and every 10.5 km, body mass was measured and samples of blood, urine, and sweat were collected. Body mass was measured using a commercial scale (Beurer BF 15, Beurer GmbH, Ulm, Germany) to the nearest 0.1 kg, after voiding the urinary bladder. Venous blood samples were drawn in a sitting position. Two serum tubes (Serum Sep Clot Activator, 5 mL, Greiner/Bio-One, Frickenhausen, Germany) and three ethylenediamine tetra-acetic acid (EDTA) tubes (BD Vacutainer®, 3 mL, Becton Dickinson, Heidelberg, Germany) were drawn. One of the EDTA tubes, for the later performed blood count and measurement of lactate dehydrogenase, was stored at room temperature. The two tubes for serum and the remaining two tubes for EDTA plasma were centrifuged immediately at 3000 g for 10 minutes and the plasma was frozen on dry ice.
Urine samples were collected after measuring total urinary volume at the defined times into a Vacuette® system (10 mL, Greiner/Bio-One) and were also stored on dry ice. Sweat samples were collected from the defined skin area on the back. Foil was fixed using Tegaderm film (3M Medica, Neuss, Germany) to the 17 × 25 cm area on the back leading to a small reservoir at the caudal end. After documenting the quantity in mL, the sweat was transferred in empty sterile tubes (7 mL, Greiner/Bio-One) and also stored on dry ice.
After collection, the EDTA blood samples were immediately transferred to the laboratory, and the blood counts were performed within 4 hours of blood sampling. The other serum, plasma, urine, and sweat samples remained stored on dry ice and were transported to the laboratory immediately after the experiment and stored there at −20°C until analysis.
Blood counts were performed using the EDTA blood samples, and included a white blood count with differentiation, red blood count, hemoglobin, hematocrit, and platelets. Hematologic parameters were determined using the Cell-Dyn Sapphire® (Abbott Diagnostics, Wiesbaden, Germany). Osmolality in serum, urine, and sweat was measured using an Osmomat 030 device (Gonotec, Berlin, Germany). Glucose in serum and lactate in plasma were measured using a Biosen 5140 system (Barleben, Magdeburg, Germany). Sodium, potassium, calcium, chloride, creatinine, urea, creatine kinase in serum and urine, C-reactive protein in serum, lactate dehydrogenase in plasma, and glucose in urine were measured using a DxC 800 system (Beckman Coulter, Krefeld Germany). Myoglobin, cardiac troponin I, free triiodothyronine, free thyroxine, thyroid-stimulating hormone (TSH), prolactin, cortisol in serum, and brain natriuretic peptide (BNP) in plasma were measured using an Advia Centaur XP (Siemens, Eschborn, Germany). Insulin in serum was measured using an AxSYM device (Abbott Diagnostics). Insulin-like growth factor 1 and interleukin-6 in serum were measured using the Immulite 2000 (Siemens). Somatotropic hormone in serum, and adrenocorticotropic hormone (ACTH) and renin in plasma were measured using a Liaison® device (diaSorin, Dietzenbach, Germany). Procalcitonin was measured using a Mini-Vidas system (Bio-Merieux, Marcy l′Etoile, France). Aldosterone in plasma was measured using a radioimmunoassay kit (Beckman Coulter). Midregional proatrial natriuretic peptide, midregional proadrenomedullin, c-terminal proendothelin-1, and copeptin in plasma were measured using a Kryptor device (Brahms GmbH, Hennigsdorf, Germany). Sodium, potassium, and calcium in sweat were measured using the AAnalyst 100 (Perkin Elmer, Rodgau, Germany). Albumin in urine was measured using an Immage® 800 device (Beckman Coulter). Metanephrines and normetanephrines in urine were measured using high-performance liquid chromatography (Recipe, Munich, Germany).
Renal parameters
We expressed urine concentration as fractional excretions. This applied to sodium, potassium, urea, and osmolality in urine. We used the general formula: fractional excretion of parameter = [(parameterurine × creatinineserum)/(parameterserum× creatinineurine)] × 100, following Espinel.26 Transtubular potassium gradient was calculated using the equation transtubular potassium gradient = (potassiumurine × osmolalityserum)/(potassiumserum × osmolalityurine) according to West et al.27 Glomerular filtration rate (GFR) was estimated using the four-variable MDRD4 formula (GFR [mL/min/1.73 m2] = 32841 × (creatinine [μmol/L][−1.154]) × age [years][−020]) following Levey et al.28 Creatinine clearance rate was estimated using the Cockcroft-Gault formula.29
Results
Pre-event results
In the incremental test, the athlete achieved a maximum speed of 17 km/hour, a VO2max of 58 mL/kg per minute, and a maximum heart rate of 188 beats per minute. Lactate threshold was set at 10 km/hour.
Performance
The athlete invested a total time of 7 hours 10 minutes, including breaks, to complete the marathon, which comprised a total of 2400 laps for 17.6 m in the climate chamber. He was running for 6 hours 30 minutes at a mean speed of approximately 6.5 km/hour, with a mean heart rate of approximately 112 beats per minute, expending total energy of 4434 kcal. Body mass decreased to 93.1 kg (−1.6%). He drank 3.4 L of fluids and consumed 2050 kcal of energy (Figure 2).
Temperature
Tskin at the head showed a total increase of 9°C (minimum 28.5°C, maximum 37.5°C). Tskin at the hand showed a total increase of 9°C (minimum 29.5°C, maximum 38.5°C). Tskin at the ankle showed a total increase of 16°C (minimum 23°C, maximum 39.5°C). Tcore varied by 0.9°C (minimum 37.5°C, maximum 38.4°C). The variations in Tcore/Tskin during the testing phase out of the climate chamber were depicted at every measurement. Tskin at the head was mainly influenced by the transition Tambient out of the climate chamber (Figure 3).
Sweat
Sweat parameters are shown in Table 1. Estimated sweat production increased from 40.3 mL at 10.5 km to 120.8 mL at 21.1 km. At the end of the marathon, total sweat production was estimated to be 685 mL (+888%). The starting sweat osmolality measurement was 215 mOsm/kg and then fell to 89 mOsm/kg, after which the values remained constant, ending at 95 mOsm/kg. Sodium in sweat increased by 56%, after an initial decrease, ending at a level of 57 mg/L. Calcium in sweat decreased initially (−84%) and continued, ending at 35.3 mg/L. Potassium decreased continuously, resulting in a total change of −83%.
Table 1.
Change in sweat parameters from the plastic bag attached to the back of the runner
| 1 0.5 km (−45°C to −20°C) | 21.1 km (−20°C to +5°C) | Δ to 10.5 km (%) | 31.6 km (+5°C to+30°C) | Δ to 10.5 km (%) | 42.195 km (+30°C to+55°C) | Total Δ (%) | |
|---|---|---|---|---|---|---|---|
| Estimated total sweat production (mL) | 40.3 | 120.8 | +199.7 | 125.7 | +211.9 | 398.2 | +888.0 |
| Osmolality (mOsm/kg) | 215 | 89.0 | −58.6 | 77.0 | −64.1 | 95.0 | −55.8 |
| Sodium (mmol/L) | 7.148 | 4.709 | −34.1 | 6.609 | −7.5 | 11.213 | +56.8 |
| Potassium (mmol/L) | 22.015 | 6.864 | −68.8 | 4.294 | −80.5 | 3.734 | −83.0 |
| Calcium (mmol/L) | 9.22 | 1.475 | −84.0 | 0.778 | −91.5 | 0.880 | −90.4 |
| Chloride* | |||||||
Note:
Due to method, not measurable.
Laboratory results
Hematologic and biochemical parameters
Hematologic and biochemical parameters are shown in Table 2 (complete blood count) and Table 3 (serum and plasma). During the marathon, white blood cells increased, ending at 81%, with a change in percentages of monocytes and neutrophils (+38% and +10%, respectively). Red blood count, hemoglobin, hematocrit, mean cell volume, mean cell hemoglobin, and mean corpuscular hemoglobin concentration remained unchanged. Platelet count increased by 32%. Osmolality (−1%), sodium (0%), potassium (+5%), calcium (+8%), and chloride (−1%) in serum showed minor changes. Serum creatinine increased by 10% and creatine kinase in serum by 66%. Glucose and lactate dehydrogenase increased by 33% and 8%, respectively. Lactate in plasma increased by 98%. Myoglobin increased by 250%. Cardiac troponin I and procalcitonin were immeasurably low through the whole marathon (<0.01 ng/L and <0.05 ng/L, respectively). Inflammation parameters, such as C-reactive protein, remained unchanged, in contrast with interleukin-6, which increased by more than 165%. BNP was immeasurably low before the start but increased steadily to reach 11 ng/L. Midregional proatrial natriuretic peptide increased at 10.5 km (+33%), and had decreased by 4% by the end of the marathon. Midregional proadrenomedullin decreased until reaching 31.6 km (−3%), then increased to a final level which was 10% higher than prestart, and c-terminal proendothelin-1 increased continuously by 79%. Copeptin increased at 10.5 km to 8.3 pmol/L, but after that point remained immeasurably low as at the start, and increased again to reach 18.2 pmol/L at 42.195 km.
Table 2.
Change in hematologic parameters
| Prestart | 10.5 km | Δ to prestart (%) | 21.1 km | Δ to prestart (%) | 31.6 km | Δ to prestart (%) | 42.195 km | Total Δ (%) | |
|---|---|---|---|---|---|---|---|---|---|
| WBC count (Gpt/L) | 5.59 | 5.95 | 6.4 | 6.49 | +16.1 | 7.55 | +35.0 | 10.1 | +80.6 |
| RBC count (Tpt/L) | 4.85 | 4.96 | +2.2 | 4.8 | −1.0 | 4.83 | −0.4 | 5.2 | +7.2 |
| MCV (f) | 92.9 | 92.1 | −0.8 | 92.1 | −0.8 | 91.8 | −1.1 | 91.2 | −1.8 |
| MCH (fmol) | 2.02 | 2.03 | +0.5 | 2.07 | +2.4 | 2.07 | +2.4 | 2.0 | −0.9 |
| MCHC (mmol/L) | 21.8 | 22.0 | +0.9 | 22.5 | +3.2 | 22.5 | +3.2 | 22.0 | +0.9 |
| Platelet count (Gpt/L) | 274 | 294 | +7.3 | 293 | +6.9 | 308 | +12.4 | 363 | +32.4 |
| Neutrophils (%) | 52.1 | 63.3 | +21.5 | 64.6 | +23.9 | 60.5 | +16.1 | 57.3 | +9.9 |
| Eosinophils (%) | 2.00 | 1.04 | −48.0 | 0.8 | −60.0 | 1.21 | −39.5 | 1.4 | −30.0 |
| Basophils (%) | 0.14 | 0.43 | +207.1 | 0.5 | +257.1 | 0.47 | +235.7 | 0.2 | +42.8 |
| Monocytes (%) | 3.52 | 5.15 | +46.3 | 5.22 | +48.3 | 6.45 | +83.2 | 4.85 | +37.7 |
| Lymphocytes (%) | 42.3 | 30.0 | −29.0 | 28.9 | −31.6 | 31.4 | −25.7 | 36.2 | −14.4 |
| Hemoglobin (mmol/L) | 9.81 | 10.1 | +2.9 | 9.93 | +1.2 | 9.99 | +1.8 | 10.4 | +6.0 |
| Hematocrit | 0.45 | 0.46 | +2.2 | 0.44 | −2.2 | 0.44 | −2.2 | 0.47 | +4.4 |
Abbreviations: WBC, white blood cells; RBC, red blood cells; MCV, mean cell volume; MCH, mean cell hemoglobin; MCHC, mean corpuscular hemoglobin.
Table 3.
Change in biochemical parameters
| Prestart | 10.5 km | Δ to prestart (%) | 21.1 km | Δ to prestart (%) | 31.6 km | Δ to prestart (%) | 42.195 km | Total Δ (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Serum | |||||||||
| Osmolality (mOsm/kg) | 299 | 298 | −0.3 | 294 | −1.6 | 300 | +0.3 | 296 | −1.0 |
| Sodium (mmol/L) | 137 | 136 | −0.7 | 138 | +0.7 | 139 | +1.4 | 137 | 0.0 |
| Potassium (mmol/L) | 3.86 | 4.44 | +15.0 | 4.63 | +19.9 | 4.48 | +16.0 | 4.04 | +4.6 |
| Calcium (mmol/L) | 2.37 | 2.45 | +3.3 | 2.42 | +2.1 | 2.44 | +2.9 | 2.55 | +7.5 |
| Chloride (mmol/L) | 102 | 101 | −0.9 | 100 | −1.9 | 101 | −0.9 | 101 | −0.9 |
| Creatinine (μmol/L) | 92.0 | 92.0 | 0.0 | 95.0 | +3.2 | 96.0 | +4.3 | 101 | +9.7 |
| Glucose (mmol/L) | 4.3 | 4.9 | +13.9 | 5.4 | +25.5 | 4.5 | +4.6 | 5.7 | +32.5 |
| Insulin-level (μE/mL) | 15.0 | 6.5 | −56.6 | 13.4 | −10.6 | 1.8 | −88.0 | 4.10 | −72.6 |
| Lactate dehydrogenase (μmol/L) | 2.53 | 2.82 | +11.4 | 2.85 | +12.6 | 2.75 | +8.7 | 3.25 | +28.4 |
| Urea (mmol/L) | 7.42 | 6.87 | −7.4 | 6.41 | −13.6 | 6.42 | −13.4 | 6.41 | −13.6 |
| CK (μmol/L) | 6.24 | 6.82 | +9.2 | 7.29 | +16.8 | 8.27 | +32.5 | 10.4 | +66.6 |
| Myoglobin (μg/L) | 59.4 | 91.0 | +53.2 | 122 | +105.3 | 180 | +203.0 | 208 | +250.1 |
| Cardiac troponin I (ng/L) | <0.01 | <0.01 | ** | <0.01 | ** | <0.01 | ** | <0.01 | ** |
| Procalcitonin (ng/mL) | <0.05 | <0.05 | ** | <0.05 | ** | <0.05 | ** | <0.05 | ** |
| CRP (mg/L) | 1.0 | 1.0 | 0.0 | 1.0 | 0.0 | 1.0 | 0.0 | 1.0 | 0.0 |
| Interleukin 6 (pg/mL) | <2.0 | <2.0 | ** | <2.0 | ** | <2.0 | ** | 5.3 | >165 |
| Plasma | |||||||||
| Lactate (mmol/L) | 1.21 | 1.95 | +61.1 | 2.94 | +142.9 | 1.88 | +55.3 | 2.40 | +98.3 |
| BNP (ng/L) | <10.0 | <10.0 | ** | 10.2 | ** | 11.9 | ** | 11.0 | ** |
| MR-proANP (pmol/L) | 49 | 65 | +32.6 | 53 | +8.1 | 57 | +16.3 | 47 | −4.0 |
| MR-proADM (pmol/L) | 0.31 | 0.31 | 0.0 | 0.28 | −9.6 | 0.3 | −3.2 | 0.34 | +9.6 |
| CT-proET-1 (pmol/L) | 34 | 40 | +17.6 | 44 | +29.4 | 45 | +32.3 | 61 | +79.4 |
Note:
Calculation not possible.
Abbreviations: CK, creatine kinase; CRP, C-reactive protein; BNP, brain natriuretic peptide; MR-proANP, midregional proatrial natriuretic peptide; MR-proADM, midregional proadrenomedullin; CT-proET-1, c-terminal proendothelin-1.
Hypothalamopituitary feedback and renin-angiotensin-aldosterone systems
The hypothalamopituitary response is shown in Table 4. Free triiodothyronine and free thyroxine increased by 4% and 3%, respectively, whereas TSH increased by 65%. Prolactin increased by 222% from baseline after decreasing at the start of the marathon. Somatotropic hormone showed an increase of 4150% in the first quarter of the marathon, with a fall again to baseline. The final somatotropic hormone level was increased (+391%) compared with baseline. Insulin-like growth factor 1 increased by 4%. ACTH decreased continuously to a level which was 94% lower than baseline at the end of the study. The cortisol concentration decreased by 72% at 31.6 km, and thereafter increased to half of the baseline value by the end of the study. Insulin decreased by 73%. Renin increased by 82% at 31.6 km, and showed a further increase to a total of 1146%. Aldosterone increased by 120% at 31.6 km to the previous value at 21.5 km. By the end of the marathon, aldosterone had increased by 314%.
Table 4.
Change in hypothalamopituitary response
| Prestart | 10.5 km | Δ to prestart (%) | 21.1 km | Δ to prestart (%) | 31.6 km | Δ to prestart (%) | 42.195 km | Total Δ (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Prolactin (ng/mL) | 4.1 | 2.5 | −39.0 | 4.6 | +12.2 | 5.30 | +29.2 | 13.2 | +221.9 |
| Somatotropic hormone (μg/L) | 0.12 | 5.1 | +4,150.0 | 0.15 | +25.0 | <0,10 | ** | 0.59 | +391.6 |
| IGF-1 (μg/L) | 220 | 232 | +5.4 | 223 | +1.3 | 229 | +4.0 | 229 | +4.0 |
| ACTH (ng/L) | 28.0 | 13.5 | −51.7 | 3.64 | −87.0 | <1.6 | ** | <1.6 | ** |
| Aldosterone (ng/L) | 78.1 | 61.2 | −21.6 | 69.1 | −11.5 | 152 | +94.6 | 323 | +313.5 |
| Cortisol (nmol/L) | 468 | 194 | −58.5 | 132 | −71.7 | 115 | −75.4 | 258 | −44.8 |
| TSH, basal (mU/L) | 2.19 | 2.25 | +2.7 | 2.19 | 0.0 | 2.63 | +20.0 | 3.62 | +65.3 |
| fT3 (pmol/L) | 5.0 | 5.1 | +2.0 | 4.90 | −2.0 | 5.0 | 0.0 | 5.2 | +4.0 |
| fT4 (pmol/L) | 16.6 | 17.0 | +2.4 | 16.8 | +1.2 | 16.0 | −3.6 | 17.1 | +3.0 |
| Copeptin (pmol/L) | <4.8 | 8.3 | ** | <4.8 | ** | <4.8 | ** | 18.2 | ** |
| Renin direct (μg/L) | 7.90 | 7.30 | −7.5 | 12.5 | +58.2 | 22.7 | +187.3 | 98.4 | +1145.5 |
Note:
Calculation not possible.
Abbreviations: ACTH, adrenocorticotropic hormone; IGF-1, insulin-like growth factor 1; TSH, thyroid-stimulating hormone; fT3, free triiodothyronine; fT4, free thyroxine.
Urinary parameters
Values for urinary parameters during the marathon are shown in Table 5. Kidney function is shown in Table 6. Urine volume decreased continuously to −83% (870 mL at 10.5 km, 430 mL at 21.1 km, 220 mL at 36.6 km, 150 mL at 42.195 km). Estimated GFR decreased gradually to −10%, and albumin in urine decreased gradually by 51%. Urine osmolality showed an initial decrease of 50% at 21.1 km, and thereafter remained unchanged (5% change until 42.125 km). Urinary urea was 22% higher at the end of the study compared with baseline. Urinary glucose decreased after an initial increase (+300%) to a value at 42.195 km, which was 100% higher than the baseline. There was also an increase in urinary metanephrines (+10%) and normetanephrines (+11%). Fractional sodium excretion increased in comparison with the prestart level until 21.1 km. At 42.195 km, fractional sodium excretion had decreased to −74% compared with the initial value. Fractional urea excretion decreased by 28% after an initial increase. The potassium to sodium ratio and the transtubular potassium gradient remained stable (+4% and +1%, respectively). Creatinine clearance decreased after an initial stable value to −10% compared with baseline.
Table 5.
Change in urine parameters
| Prestart | 1 0.5 km | Δ to prestart (%) | 21.1 km | Δ to prestart (%) start (%) | 31.6 km | Δ to pre-start (%) to pre-start (%) | 42.195 km | Total Δ (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Estimated GFR (mL/minute) | 90.82 | 90.82 | 0.0 | 87.53 | −3.6 | 86.49 | −4.7 | 81.58 | −10.2 |
| Albumin in urine (mg/mmol Crea) | 0.99 | 0.86 | −13.1 | 0.43 | −56.5 | 0.45 | −54.5 | 0.48 | −51.5 |
| Osmolality (mOsm/kg) | 600 | 363 | −39.5 | 624 | +4.0 | 722 | +20.3 | 756 | +26.0 |
| Sodium in urine (mmol/mmol Krea) | 23.85 | 30.11 | +26.2 | 28.91 | +21.2 | 19.48 | −18.3 | 12.15 | −49.0 |
| Chloride in urine (mmol/mmol Krea) | 26.7 | 36.85 | +38.0 | 30.76 | +15.2 | 19.83 | −25.7 | 12.85 | −51.8 |
| Potassium in urine (mmol/mmol Krea) | 6.96 | 11.33 | +62.8 | 11.22 | +61.2 | 7.85 | +12.7 | 5.78 | −16.9 |
| Calcium in urine (mmol/mmol Krea) | 0.63 | 0.42 | −33.3 | 0.38 | −39.6 | 0.29 | −53.9 | 0.27 | −57.1 |
| Creatinine in urine (μmol/L) | 5,206 | 2,696 | −48.2 | 5,434 | +4.3 | 8,467 | +62.6 | 11,281 | +116.6 |
| Urea in urine (mmol/L) | 274 | 141 | −48.5 | 210 | −23.3 | 283 | +3.2 | 335 | +22.2 |
| Glucose in urine (mmol/mmol Krea) | 0.02 | 0.08 | +300.0 | 0.07 | +250.0 | 0.05 | +150.0 | 0.04 | +100.0 |
| Metanephrines in urine (μg/mmol Krea) | 9.23 | 8.15 | −11.7 | 10.50 | +13.7 | 12.28 | +33.0 | 10.19 | +10.4 |
| Normetanephrines in urine (μg/mmol Krea) | 15.38 | 17.7 | +15.0 | 11.42 | −25.7 | 16.17 | +5.1 | 17.02 | +10.6 |
Abbreviation: GFR, glomerular filtration rate.
Table 6.
Changes in kidney parameters compared with prestart
| Prestart | 10.5 km | Δ to prestart (%) | 21.1 km | Δ to prestart (%) | 31.6 km | Δ to prestart (%) | 42.195 km | Total Δ (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Fractional sodium excretion (%) | 0.31 | 0.76 | +145.1 | 0.37 | +19.1 | 0.16 | −48.3 | 0.08 | −74.2 |
| Fractional urea excretion (%) | 65.26 | 70.04 | +7.3 | 57.28 | −12.2 | 49.98 | −23.4 | 46.79 | −28.3 |
| Potassium-to-sodium ratio (ratio) | 0.03 | 0.03 | +15.8 | 0.03 | +19.1 | 0.03 | +14.4 | 0.03 | +4.7 |
| Transtubular potassium gradient (ratio) | 3.62 | 3.11 | −14.1 | 5.14 | +42.2 | 4.22 | +16.6 | 3.65 | +0.9 |
| Creatinine clearance (mL/minute) | 139.12 | 140.15 | +0.7 | 134.73 | −3.2 | 130.93 | −5.9 | 124.72 | −10.4 |
Discussion
In this study, we followed an athlete who had the intention to become the first runner in history to complete a self-paced marathon in a climate chamber whilst overcoming a temperature difference of 100°C (373°K). He decided to start at −45°C, which would be the mean temperature in a marathon in extremely low temperatures, such as the Baikal Ice marathon and the Antarctic Ice marathon, and to finish at +55°C, which would be the mean temperature of a marathon in the heat, such as the Marathon des Sables or the Badwater ultramarathon. While adaptations to extreme cold or extreme heat are known, we tried to investigate and describe changes in temperature and regulating systems in one athlete running between a lower critical temperature and an upper critical temperature in a thermoneutral zone. We investigated how Tcore changed compared with Tskin, and how hormone metabolism was influenced during a total Tambient difference of 100°C. The major finding was that running a marathon with a total Tambient difference of 100°C was possible. Furthermore, the Tambient to Tcore relationship was maintained (Tcore ∆0.9°C), even when thermoregulation was extremely challenged by endurance exercise, as during a marathon and an additional external heat load.
Differences in skin temperatures between ankle and wrist
Tcore in mammals is typically in the range of 37°C–39°C. Tcore in our athlete never exceeded this range. The changes in Tcore were similar to the changes reported by Cheuvront and Haymes,4 with deviations due to breaks for measurements and external cooling. Assuming the range of normothermia by Kanouse et al,14 we hypothesized that the increase in Tcore before the first break and after the second break was due to a temporary inability to defend regulated Tcore against a continually increasing Tambient. This increase was only temporary and regressed, demonstrating that the primary mission of thermoregulation is to defend Tcore against a challenging Tambient.14 We found a variation in Tcore and Tskin measurements during the testing phase outside the climate chamber. Tambient out of the climate chamber affected each point of measurement, but mostly Tskin at the head. This may be due to the changing Tambient outside the climate chamber, but it should also be noted that ingestion of cold fluids acts as a cooling element.30 The Tskin variation developed differently, with the highest difference measured at the ankle with a ∆ of 16°C. Tskin at the ankle was the most distant site from Tcore, but also nearer to a working muscle than, eg, Tskin at the wrist. Therefore, Tskin was the site most able to assimilate Tambient and, therefore, Tskin at the ankle was least defended by regulatory circuits to keep Tcore in range.
Differences in sweat production over time
At a Tambient of −35°C, the Tcore to Tskin gradient was high (head to core 9.7°C; hand to core 8.7°C; ankle to core 14.7°C, respectively) and humidity in the climate chamber was set at 80%. The evaporative capacity seemed to be lower at that time compared with the time in the middle of the marathon. This may explain the sweat production at 10.5 km of 40.3 mL and osmolality in sweat of 215 mOsm/kg. As the Tcore to Tskin gradient decreased, the sweat volume increased, and serum osmolality was slightly increased at 31.6 km. In temperate or cool conditions, a large skin-to-ambient temperature gradient facilitates radiant and convective heat loss, and reduces blood flow requirements to the skin, which may explain the tolerance for the high Tcore observed during marathons in cool conditions.31 For methodologic reasons, the initial evolution of ion concentration in sweat, as proposed by Shamsuddin et al,32 could not be shown. After the low sweat osmolality at 10.5 km, we suggest that the following stable values we recorded demonstrate good adaption under changing environmental conditions. Furthermore, the index of ion concentration in sweat at the end of the study may indicate a capacity for reabsorption in the eccrine sweat duct.
Continuous increase in BNP and interleukin-6
Pathologic values identified in the laboratory parameters were reassessed against references for marathon runners.15 Thereafter, all hematologic values were within range, except for creatine kinase in serum and creatinine in urine before the start of the marathon. In contrast, serum creatinine was within range, and its value rose to 10% above its initial baseline. Approximately 40% of marathoners experience a transient increase in serum creatinine, and the data suggest that acute kidney injury with a transient and minor change in renal filtration function occurs with the stress of marathon running.33 Following the stages of the Acute Kidney Injury Network,34 our marathoner was in stage 1. At the start, creatine kinase values were outside the adapted level of 6.24 μmol/L suggested by Kratz et al, and rose again to an end value of 10.4 μmol/L.15 However, a massive increase in creatine kinase is common, and is widely accepted as an indirect marker of skeletal muscle damage while running.35–39 There is a suspicion that the extreme increases in serum creatine kinase activity may be related to development of exertional rhabdomyolysis.40 Another factor impairing kidney function is the redirection of blood flow, whereby exercising blood is directed more to the working muscles than to the kidneys, which decreases renal perfusion.19 Furthermore, proendothelin-1 was increased by +79%. Maeda et al discussed the possibility of reduced kidney perfusion by an exercise-induced increase in production of endothelin-1 in the kidneys.41 The increase in endothelin-1 causes decreased blood flow to the kidneys via two pathways, ie, a vasoconstrictive action and attenuation of nitric oxide production. BNP increased continuously, and an increase in BNP was considered to be a sign of high cardiovascular performance due to a low blood volume.11,42 Following Hew-Butler et al, BNP may assist arginine vasopressin and atrial natriuretic peptide in the regulation of fluid balance during extreme physical stress.43 Values during the marathon showed a more continual increase of BNP, whereas arginine vasopressin and atrial natriuretic peptide fuctuated more, which supports this hypothesis. The positive effects of atrial natriuretic peptide seen during a marathon could reflect regulation of body temperature by influencing the sweat glands as well as stimulation of lipolysis, compensating for the enormous energy demand.44 Furthermore, we noted that compared with exercise at room temperature, plasma levels of epinephrine, norepinephrine, and cortisol were all higher during exercise in the heat.45
There were increased counts for inflammatory parameters such as leucocytes and interleukin-6. Surprisingly, the plasma C-reactive protein concentration was immeasurably low. Therefore, recovery of plasma C-reactive protein levels possibly occurred during the recovery time after finishing the marathon, as reported by Waśkiewicz et al.46 Cytokines, particularly interleukin-1 and interleukin-6, act as endogenous pyrogens in the brain. Interleukin-1 and interleukin-6 stimulate thermogenesis via synthesis of prostaglandins and corticotropin-releasing factors.47 This induction of thermogenesis by peripheral interleukin-6 seems not to last, but influences the new regulated Tcore.48
Increase in TSH and decrease in ACTH
Several stress hormones, including cortisol, somatotropic hormone, and normetanephrines were released, in urine during prolonged exercise together with increasing Tambient. These findings are compatible with the results reported by Niess et al,49 who suggested that elevated Tambient primarily affected the cardiocirculatory and hormonal systems, resulting in changes in neutrophil and monocyte cell trafficking. In contrast, the acute immune response seems not to be influenced further by additional heat stress during endurance exercise, which is also compatible with our results. TSH increased by 65.3%. It is known that thyroid hormones increase nonshivering thermogenesis in cold conditions by stimulating uncoupling protein-1.50 We found no increase in TSH at 10.5 km during the marathon when Tambient was low. This fact was most probably due to the predominance of endogenous thermogenesis while running. Prolactin increased by 221.9%, together with an increase in TSH of 65.3%. It has been reported that an increase in prolactin is directly related to an increase in TSH during prolonged exhaustive exercise.51 Jimenez et al reported prolactin increases only during passive hyperthermia and not while exercising.52 In the present case, an additive exogenous heat load may have contributed to the increased prolactin levels towards the end of the study, and thus support the use of prolactin as a biomarker for development of central fatigue.53 In contrast, ACTH decreased after an initial increase at 10.5 km continuously to the end value. An initial peak of ACTH is most probably explained by the cold environment54 stimulating the release of glucocorticoids, which would then increase the availability of glucose and assist lipolysis. The rise in temperature may play a consequential role, because vasoconstriction and also cortisol must be inhibited for thermolytic reasons in a hot environment.55 The decrease in cortisol after a peak may be explained by this fact. The peak at the end of the study may have been due to the psychologic stress of running in such high temperatures. Alternatively, following the suggestions of Niessner et al,44 the increase in adrenocortical steroids may have compensated for the negative influence of atrial natriuretic peptide on natriuresis and blood pressure, which would explain this peak at the end too. Renin increased steadily to +1146% at 42.195 km, as did aldosterone, which increased by +314%. This metabolic response may support the fact that plasma osmolality, serum sodium concentration, and safe Tcore were maintained. Therefore, we show in this case study that humans were able to exercise in extreme conditions while drinking water ad libitum, as suggested by Nolte et al.56
Limitations and implications for future research
This case study performed under controlled conditions shows the individual response of one athlete. The results might be different in another athlete, and different again in the same athlete on a further attempt. Sweat sampling was performed on the back of the athlete and extrapolated to the total surface of the athlete. However, sweating might be different on different parts of the body, so the total amount of sweat produced in this study might have been higher than reported. The athlete lost 1.6% of his body mass. However, he completed the marathon in 6.5 hours. Whether his performance could have been worse or better with a more regimented drinking/food intake strategy cannot be commented upon without further research. The same study is to be performed in more subjects with the same characteristics to validate the present findings.
Conclusion
The metabolic responses cited above may be, amongst others, responsible for regulating different feedback/forward loops and thresholds in the thermoregulation circuit. The results in our subject suggest a multitude of metabolic responses in reaction to variations in environmental conditions during continuous exercise. Regulatory mechanisms contribute to avoidance of hypothermia or hyperthermia. None of our laboratory results were cause for medical concern. More accurate responses, especially during extremely thermostable conditions, concerning detailed regulatory mechanisms remain elusive. The results of this case study describe the response of one selected subject and may not be generalizable. The same study is to be performed on more subjects with the same characteristics to validate the present findings.
Acknowledgments
The authors thank Holger Häusler and Lothar Kleinod for their technical assistance with the climate chamber. Furthermore, they thank Andreas Heertsch, business manager of EndoTherm GmbH, Arlesheim, Switzerland, for making valuable equipment available during the study period. We also thank Therese Fässler for her help in translation.
Footnotes
Disclosure
The authors have no conflict of interest in this work.
References
- 1.Jokl P, Sethi PM, Cooper AJ. Master’s performance in the New York City Marathon 1983–1999. Br J Sports Med. 2004;38:408–412. doi: 10.1136/bjsm.2002.003566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lepers R, Cattagni T. Do older athletes reach limits in their performance during marathon running? Age (Dordr) 2012;34:773–781. doi: 10.1007/s11357-011-9271-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horton D, Wortley G. Ultra-endurance runners; Proceedings of the Southeast Regional Chapter of the American College of Sports Medicine annual meeting; February 14-16, 2011; Greenville, SC. [Google Scholar]
- 4.Cheuvront SN, Haymes EM. Thermoregulation and marathon running: biological and environmental influences. Sports Med. 2001;31:743–762. doi: 10.2165/00007256-200131100-00004. [DOI] [PubMed] [Google Scholar]
- 5.Buskirk ER, Beetham WP. Dehydration and body temperature as a result of marathon running. Med Sport. 1960;14:493–506. [Google Scholar]
- 6.Werner J. The concept of regulation for human-body temperature. J Therm Biol. 1980;5:75–82. [Google Scholar]
- 7.Cheuvront SN, Haymes EM. Ad libitum fluid intakes and thermoregulatory responses of female distance runners in three environments. J Sports Sci. 2001;19:845–854. doi: 10.1080/026404101753113796. [DOI] [PubMed] [Google Scholar]
- 8.Suping Z, Guanglin M, Yanwen W, Ji L. Study of the relationships between weather conditions and the marathon race, and of meteorotropic effects on distance runners. Int J Biometeorol. 1992;36:63–68. doi: 10.1007/BF01208915. [DOI] [PubMed] [Google Scholar]
- 9.Trapasso LM, Cooper JD. Record performances at the Boston marathon: biometeorological factors. Int J Biometeorol. 1989;33:233–237. doi: 10.1007/BF01051083. [DOI] [PubMed] [Google Scholar]
- 10.Nielsen B. Olympics in Atlanta: a fight against physics. Med Sci Sports Exerc. 1996;28:665–668. doi: 10.1097/00005768-199606000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Montain SJ, Coyle EF. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol. 1992;73:1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [DOI] [PubMed] [Google Scholar]
- 12.Maughan RJ. Thermoregulation in marathon competition at low ambient-temperature. Int J Sports Med. 1985;6:15–19. doi: 10.1055/s-2008-1025806. [DOI] [PubMed] [Google Scholar]
- 13.Noakes TD, Myburgh KH, Du Pleiss J, et al. Metabolic rate, not percent dehydration, predicts rectal temperature in marathon runners. Med Sci Sports Exerc. 1991;23:443–449. [PubMed] [Google Scholar]
- 14.Kanosue K, Crawshaw LI, Nagashima K, Yoda T. Concepts to utilize in describing thermoregulation and neurophysiological evidence for how the system works. Eur J Appl Physiol. 2010;109:5–11. doi: 10.1007/s00421-009-1256-6. [DOI] [PubMed] [Google Scholar]
- 15.Kratz A, Lewandrowski KB, Siegel AJ, et al. Effect of marathon running on hematologic and biochemical laboratory parameters, including cardiac markers. Am J Clin Pathol. 2002;118:856–863. doi: 10.1309/14TY-2TDJ-1X0Y-1V6V. [DOI] [PubMed] [Google Scholar]
- 16.Adams WC, Fox RH, Fry AJ, MacDonald IC. Thermoregulation during marathon running in cool, moderate, and hot environments. J Appl Physiol. 1975;38:1030–1037. doi: 10.1152/jappl.1975.38.6.1030. [DOI] [PubMed] [Google Scholar]
- 17.Nelson PB, Ellis D, Fu F, Bloom MD, Omalley J. Fluid and electrolyte balance during a cool weather marathon. Am J Sports Med. 1989;17:770–772. doi: 10.1177/036354658901700608. [DOI] [PubMed] [Google Scholar]
- 18.Whiting PH, Maughan RJ, Miller JDB. Dehydration and serum biochemical changes in marathon runners. Eur J Appl Physiol. 1984;52:183–187. doi: 10.1007/BF00433390. [DOI] [PubMed] [Google Scholar]
- 19.Nielsen B, Hales JRS, Strange S, Christensen NJ, Warberg J, Saltin B. Human circulatory and thermoregulatory adaptations with heat acclimation and exercise in a hot, dry environment. J Physiol. 1993;460:467–485. doi: 10.1113/jphysiol.1993.sp019482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watson P, Black KE, Clark SC, Maughan RJ. Exercise in the heat: Effect of fluid ingestion on blood-brain barrier permeability. Med Sci Sports Exerc. 2006;38:2118–2124. doi: 10.1249/01.mss.0000235356.31932.0a. [DOI] [PubMed] [Google Scholar]
- 21.Foster C, Foster D, Hutchinson M. Africa: Speaking with Earth and Sky. Claremont, South Afric: David Philip Publishers; 2005. [Google Scholar]
- 22.New York Road Runner’s Club Inc . New York City Marathon Media Guide. New York, NY: Organizers and Producers of the NYC Marathon; 1998. [Google Scholar]
- 23.Kirchhoff E. Online-publication of the German food composition table “Souci-Fachmann-Kraut” on the Internet. J Food Compost Anal. 2002;15:465–472. [Google Scholar]
- 24.Dubois D, Dubois EF. A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med. 1916;17:863–871. [Google Scholar]
- 25.Crouter SE, Albright C, Bassett DR. Accuracy of polar S410 heart rate monitor to estimate energy cost of exercise. Med Sci Sports Exerc. 2004;36:1433–1439. doi: 10.1249/01.mss.0000135794.01507.48. [DOI] [PubMed] [Google Scholar]
- 26.Espinel CH. The FENa test. Use in the differential diagnosis of acute renal failure. JAMA. 1976;236:579–581. doi: 10.1001/jama.236.6.579. [DOI] [PubMed] [Google Scholar]
- 27.West ML, Marsden PA, Richardson RMA, Zettle RM, Halperin ML. New clinical approach to evaluate disorders of potassium excretion. Miner Electrolyte Metab. 1986;12:234–238. [PubMed] [Google Scholar]
- 28.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 29.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 30.Lee JKW, Shirreffs SM. The influence of drink temperature on thermoregulatory responses during prolonged exercise in a moderate environment. J Sports Sci. 2007;25:975–985. doi: 10.1080/02640410600959947. [DOI] [PubMed] [Google Scholar]
- 31.Kenefick RW, Cheuvront SN, Sawka MN. Thermoregulatory function during the marathon. Sports Med. 2007;37:312–315. doi: 10.2165/00007256-200737040-00010. [DOI] [PubMed] [Google Scholar]
- 32.Shamsuddin AKM, Yanagimoto S, Kuwahara T, Zhang Y, Nomura C, Kondo N. Changes in the index of sweat ion concentration with increasing sweat during passive heat stress in humans. Eur J Appl Physiol. 2005;94:292–297. doi: 10.1007/s00421-005-1314-7. [DOI] [PubMed] [Google Scholar]
- 33.McCullough PA, Chinnaiyan KM, Gallagher MJ, et al. Changes in renal markers and acute kidney injury after marathon running. Nephrology (Carlton) 2001;16:194–199. doi: 10.1111/j.1440-1797.2010.01354.x. [DOI] [PubMed] [Google Scholar]
- 34.Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brancaccio P, Lippi G, Maffulli N. Biochemical markers of muscular damage. Clin Chem Lab Med. 2010;48:757–767. doi: 10.1515/CCLM.2010.179. [DOI] [PubMed] [Google Scholar]
- 36.Kim HJ, Lee YH, Kim CK. Biomarkers of muscle and cartilage damage and inflammation during a 200 km run. Eur J Appl Physiol. 2007;99:443–447. doi: 10.1007/s00421-006-0362-y. [DOI] [PubMed] [Google Scholar]
- 37.Kim HJ, Lee YH, Kim CK. Changes in serum cartilage oligomeric matrix protein (COMP), plasma CPK and plasma hs-CRP in relation to running distance in a marathon (42.195 km) and an ultra-marathon (200 km) race. Eur J Appl Physiol. 2009;105:765–770. doi: 10.1007/s00421-008-0961-x. [DOI] [PubMed] [Google Scholar]
- 38.Miles MP, Andring JM, Pearson SD, et al. Diurnal variation, response to eccentric exercise, and association of inflammatory mediators with muscle damage variables. J Appl Physiol. 2008;104:451–458. doi: 10.1152/japplphysiol.00572.2007. [DOI] [PubMed] [Google Scholar]
- 39.Noakes TD, Kotzenberg G, McArthur PS, Dykman J. Elevated serum creatine-kinase mb and creatine-kinase bb-isoenzyme fractions after ultra-marathon running. Eur J Appl Physiol. 1983;52:75–79. doi: 10.1007/BF00429029. [DOI] [PubMed] [Google Scholar]
- 40.Skenderi KP, Kavouras SA, Anastasiou CA, Yiannakouris N, Matalas AL. Exertional rhabdomyolysis during a 246-km continuous running race. Med Sci Sports Exerc. 2006;38:1054–1057. doi: 10.1249/01.mss.0000222831.35897.5f. [DOI] [PubMed] [Google Scholar]
- 41.Maeda S, Miyauchi T, Iemitsu M, et al. Endothelin receptor antagonist reverses decreased NO system in the kidney in vivo during exercise. Am J Physiol Endocrinol Metab. 2004;286:E609–E614. doi: 10.1152/ajpendo.00373.2003. [DOI] [PubMed] [Google Scholar]
- 42.Gonzalez-Alonso J, Mora-Rodriguez R, Below PR, Coyle EF. Dehydration markedly impairs cardiovascular function in hyperthermic endurance athletes during exercise. J Appl Physiol. 1997;82:1229–1236. doi: 10.1152/jappl.1997.82.4.1229. [DOI] [PubMed] [Google Scholar]
- 43.Hew-Butler T, Noakes TD, Soldin SJ, Verbalis JG. Acute changes in endocrine and fluid balance markers during high-intensity, steady-state, and prolonged endurance running. unexpected increases in oxytocin and brain natriuretic peptide during exercise. Eur J Endocrinol. 2008;159:729–737. doi: 10.1530/EJE-08-0064. [DOI] [PubMed] [Google Scholar]
- 44.Niessner A, Ziegler S, Slany J, Billensteiner E, Woloszczuk W, Geyer G. Increases in plasma levels of atrial and brain natriuretic peptides after running a marathon: are their effects partly counterbalanced by adrenocortical steroids? Eur J Endocrinol. 2003;149:555–559. doi: 10.1530/eje.0.1490555. [DOI] [PubMed] [Google Scholar]
- 45.Brenner IKM, Zamecnik J, Shek PN, Shephard RJ. The impact of heat exposure and repeated exercise on circulating stress hormones. Eur J Appl Physiol. 1997;76:445–454. doi: 10.1007/s004210050274. [DOI] [PubMed] [Google Scholar]
- 46.Waśkiewicz Z, Kłapcińska B, Sadowska-Krępa E, et al. Acute metabolic responses to a 24-h ultra-marathon race in male amateur runners. Eur J Appl Physiol. 2011;112:1679–1688. doi: 10.1007/s00421-011-2135-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rothwell NJ. CNS regulation of thermogenesis. Crit Rev Neurobiol. 1994;8:1–10. [PubMed] [Google Scholar]
- 48.Vybiral S, Barczayova L, Pesanova Z, Jansky L. Pyrogenic effects of cytokines (IL-1 beta, interleukin-6, TNF-alpha) and their mode of action on thermoregulatory centers and functions. J Therm Biol. 2005;30:19–28. [Google Scholar]
- 49.Niess AM, Fehrenbach E, Lehmann R, et al. Impact of elevated ambient temperatures on the acute immune response to intensive endurance exercise. Eur J Appl Physiol. 2003;89:344–351. doi: 10.1007/s00421-003-0809-3. [DOI] [PubMed] [Google Scholar]
- 50.Silva JE. Physiological importance and control of non-shivering facultative thermogenesis. Front Biosci. 2011;3:352–371. doi: 10.2741/s156. [DOI] [PubMed] [Google Scholar]
- 51.Hackney AC, Dobridge JD. Thyroid hormones and the interrelationship of cortisol and prolactin: influence of prolonged, exhaustive exercise. Endokrynol Pol. 2009;60:252–257. [PubMed] [Google Scholar]
- 52.Jimenez C, Melin B, Savourey G, Launay J-C, Alonso A, Mathieu J. Effects of passive hyperthermia versus exercise-induced hyperthermia on immune responses: hormonal implications. Eur Cytokine Netw. 2007;18:154–161. doi: 10.1684/ecn.2007.0101. [DOI] [PubMed] [Google Scholar]
- 53.Wright HE, Selkirk GA, Rhind SG, McLellan TM. Peripheral markers of central fatigue in trained and untrained during uncompensable heat stress. Eur J Appl Physiol. 2012;112:1047–1057. doi: 10.1007/s00421-011-2049-2. [DOI] [PubMed] [Google Scholar]
- 54.Nakamura K. Central circuitries for body temperature regulation and fever. Am J Physiol Regul Integr Comp Physiol. 2011;301:R1207–R1228. doi: 10.1152/ajpregu.00109.2011. [DOI] [PubMed] [Google Scholar]
- 55.Yang S, Zhang L. Glucocorticoids and vascular reactivity. Curr Vasc Pharmacol. 2004;2:1–12. doi: 10.2174/1570161043476483. [DOI] [PubMed] [Google Scholar]
- 56.Nolte HW, Noakes TD, Van Vuuren B. Trained humans can exercise safely in extreme dry heat when drinking water ad libitum. J Sports Sci. 2011;29:1233–1241. doi: 10.1080/02640414.2011.587195. [DOI] [PubMed] [Google Scholar]