Abstract
Background
In industrialized countries, about 5% to 15% of all adults have a pathologically severe fear of dental treatment, and some 3% avoid going to the dentist altogether. The affected persons may, in turn, suffer from severe dental diseases and their psychosocial effects. Many people with dental phobia have other mental disorders as well. These facts motivated us to study the prevalence of fear of dental treatment in a group of patients being treated by our psychosomatic service.
Method
212 patients of our psychosomatic service and 95 healthy controls were studied with the Hierarchical Anxiety Questionnaire (HAQ) to determine the intensity of their fear of dental treatment. Mental disorders were diagnosed with structured clinical interviews according to DSM-IV.
Results
Nearly one patient in three (30.5%, n = 64) suffered from pathologically severe fear of dental treatment; 24 of them (38.5%) had avoided visiting a dentist for longer than one year. Only 4 (4.2%) of the healthy controls were greatly afraid of dental treatment. Certain types of mental disorder were especially highly associated with fear of dental treatment: in particular, anxiety disorders (relative risk [RR] 7.44, 95% confidence interval [CI] 2.68–20.70) and depressive disorders (RR 4.92, 95% CI 1.73–14.05). Patients with post-traumatic stress disorder were affected most commonly: 34 (42%) of these patients were greatly afraid of dental treatment (RR 9.97, 95% CI 3.69–26.90). 75 of the 134 study participants who were afraid of dental treatment (56%) had cancelled a dental appointment, or failed to appear for a scheduled appointment, because of their fears.
Conclusion
Fear of dental treatment commonly accompanies certain types of mental disorder. Patients at high risk should be asked about such fears so that the problem can be recognized early and appropriately treated.
Some 5–15% of adults in industrialized countries suffer from pathologically severe fear of dental treatment (“dental fear”), to the point where they are able to consult a dentist only if they are experiencing severe pain (1). About 3% avoid visiting their dentist altogether (1). Those affected will experience serious dental-medical sequelae and their psychosocial effects (2, 3). Often, patients with dental fear are identified only after years of avoidance (4, 5). Massive damage to the teeth is the inevitable consequence (5). Studies in patients with high fear of dental treatment have shown severe impairments in terms of oral-related quality of life (8, 9), in addition to their obviously worse dental health (6, 7). Thomb et al. found a mean of eight teeth requiring treatment in patients with dental fear who had avoided visiting their dentist for many years (5). Many people who fear dental treatment are ashamed for the state of their teeth (10) and avoid talking or laughing in public (3, 10); some withdraw from social life altogether (2, 3). Their fear of visiting the dentist is so severe that they tolerate massive pain and delay crucially important treatment.
Therapy for dental fear has shown promising results and can be initiated quickly (11). Most of the available data relate to behavioral therapeutic interventions. A meta-analysis (11) showed for 36 out of 38 studies positive changes in self-reported fear. Two studies found no effect whatsoever. After four years of therapy, a mean of 77% of patients visited their dentist regularly. In more than half of the studies, dental treatment was a component of the therapy. An average of 6–10 sessions were assumed for the therapy of dental fear (11).
Dentists are confronted with varying intensities of dental fear on a daily basis. According to a study of the prevalence of dental fear in standard dental practices in Germany, only 0.5% meet the criteria of a dental phobia (12). Dentists often encounter such patients only during emergency sessions. At that point, the need for treatment is urgent; gentle, pain-free treatment is not always possible, and such emergency sessions often provide further confirmatory evidence in the vicious cycle of fear.
From a medical ethical perspective as well as to reduce costs for the health service, a duty arises to improve early detection measures for the disorder. Extensive dental restoration under general anesthesia or more than double the number of sickness notifications compared with the average population put a high burden on the healthcare system (1). This is a challenge for doctors and dentists alike. Close interdisciplinary collaboration between psychotherapists and dentists might succeed in identifying affected patients earlier on and to enable them to have up-to-the-minute dental care.
Two studies have reported an increased prevalence of psychological disorders in people with fear of dental treatment. Roy Byrne et al. (13) were the first to conduct a complex psychological diagnostic evaluation, using DSM-III criteria in patients with dental fear. They found at least one further psychiatric disorder in 42% of those investigated. A representative birth cohort study from New Zealand (14) confirmed the frequent presence of mental disorders in participants with a high degree of dental fear and found comorbid disorders in 55% more participants than in those without fear of dental treatment, of whom 42.3% had psychological disorders. An awareness that multimorbidity is common in this setting prompted the decision to approach the problem from a new angle. The present study aims to establish the prevalence of dental fear in a psychosocmatic treatment center, in order to identify underlying psychological disorders, which are often associated with fear of dental treatment. The data were compared with those of a healthy sample.
Method
Study design and recruitment of participants
In the study period from July 2010 to August 2011, patients from the clinic and polyclinic for psychotherapy and psychosomatic medicine at Dresden University Medical Center participated in the study. The patients were surveyed at the start of their therapy. A healthy sample for the purpose of comparison was recruited in the Dresden area. 212 of 221 patients who were contacted participated, and 102 of 105 controls who had been approached completed the study (response rate 96%). The general inclusion criterion was an age of 18 years or older and adequate comprehension of spoken and written German.
Data collection instruments
In addition to sociodemographic data we collected data on the intensity of participants’ fear of dental treatment by using the Hierarchical Anxiety Questionnaire (HAQ) according to Jöhren (15). This questionnaire allows allocation to three groups of dental fear intensity (no/low, moderate, high dental anxiety). Two further questions prompt for participants’ self-assessment of their degree of fear. Subjects report whether they feared dental treatment (yes/no). Participants who rated themselves as fearful of dental treatment were invited—equivalent to the severity scale of the HAQ—to classify themselves as experiencing no/low, moderate, or high dental anxiety. In order to determine avoidance behavior, subjects were asked how long ago they had last visited a dentist and whether they had cancelled or missed appointments for reasons of fear (yes/no). Clinical/psychological diagnostic evaluation was done in the patient sample by using the structured clinical interview according to DSM-IV (17). Controls were questioned by using the short form of the Patient Health Questionnaire (PHQ-D) (19). The presence of panic syndrome or major depression was an exclusion criterion among controls. Further explanations of our method are in the eBox.
Box. Additional comments on our methods.
The study represents a consecutive collection of data. Each patient who was receiving therapy during the data collection period was suitable for inclusion. Participants received verbal and written explanations of the study’s objectives and processes, of data protection and voluntary participation. The ethics committee of the medical faculty at Dresden Technical University (No EK 217072010) approved the study. At the start of treatment, each patient was handed a number of questionnaires for self-completion and underwent a structured clinical interview according to DSM-IV (SCID-I).
Hierarchical anxiety questionnaire (HAQ) according to Jöhren
The HAQ was developed on the basis of the internationally best known instrument of Corah’s Dental Anxiety Scale (16) and includes additional questions regarding seven different treatment scenarios that represent the situations during treatment that trigger most fear in patients. The HAQ records anticipatory as well as situational anxiety. A total of 11 questions can each be answered with five different intensities of fear. On the basis of the summed score, participants are allocated to three fear intensity groups: (<30 = no/low anxiety, 31–38 = moderate anxiety, >38 = high anxiety). The HAQ has a high correlation with the Dental Anxiety Scale (0.88) and a good correlation with the State-Trait Anxiety Inventory (0.66) (15).
Structured clinical interview according to DSM-IV (SCID-I)
The clinical psychological assessment was conducted on the basis of a structured, part-standardized, expert interview according to the SCID-I (17), which is based on the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). In being prescriptive about jumping rules and structural rules, the instrument allows for a high degree of objectivity. Test-retest reliability in recent studies has been reported at a kappa value of 0.61–0.83 (18).
A study of inter-rater agreement is being conducted in order to ensure that reliable diagnoses are made. Since structured interviews are always based on external assessments, the validity is assured by the interviewers. These are specially trained and have longstanding clinical experience. Furthermore, supervision is delivered by a psychologist with clinical experience.
Patient Health Questionnaire (PHQ-D), short form
The short form of the PHQ-D (19) includes a depression module (9 items), an abbreviated panic module (5 items), and a question regarding functional impairment. The PHQ-D was validated on the basis of the SCID-I. The internal consistency of the depression module is α = 0.88 (29).
Statistical analysis
The patients were allocated to groups on the basis of their diagnoses (Table 1). Between 1 and 7 diagnoses were made for each patient; it was therefore possible that patients belonged to several diagnostic groups. It was of particular importance to determine the selective effect of post-traumatic stress disorder; patients with this diagnosis were allocated to a separate group and were not included in the analyses in any other diagnostic groups.
Table 1. Allocation to diagnostic groups.
| Diagnostic group | ICD-10 diagnosis | n | % | |
|---|---|---|---|---|
| Post-traumatic stress disorder (PTSD) | ||||
| Post-traumatic stress disorder | F43.1 | 81 | 38.2 | |
| Anxiety disorders | ||||
| Agoraphobia | F40.0 | 59 | 27.8 | |
| Social phobias | F40.1 | 69 | 32.5 | |
| Panic disorder | F41.0 | 6 | 2.8 | |
| Generalized anxiety disorder | F41.1 | 7 | 3.3 | |
| Obsessive-compulsive disorder | F42.- | 28 | 13.2 | |
| Depressive disorders | ||||
| Depressive episode | F32.- | 55 | 25.9 | |
| Recurrent depressive disorder | F33.- | 92 | 43.4 | |
| Eating disorders | ||||
| Eating disorders | F50.- | 27 | 12.7 | |
| Somatoform disorders | ||||
| Somatoform disorders | F45.- | 51 | 24.1 | |
Absolute and relative (% of a total of n = 212) frequencies of diagnostic allocation
All participants were allocated to one of the three groups of dental fear on the basis of the summed score in the HAQ. Differences between patient groups and healthy subjects were determined by using Pearson’s chi-square test or Fisher’s exact test (where the expected frequencies were below 5). For diagnostic groups differing from controls with regard to the prevalence of dental fear, binary logistic regression was conducted and the highest professional qualification was used for adjustment purposes.
Ages between the two samples were compared by using the t-test. Further differences between groups with regard to sociodemographic data and self-assessment were analyzed using Pearson’s chi-square test or Fisher’s exact test. Only complete data were analyzed (missing values: patient sample n = 2 HAQ, control sample n = 2 avoidance behavior). The software package SPSS 19.0 was used for the statistical analysis.
Results
Seven participants were excluded from the study because of their psychological symptoms in the PHQ-D.
Demographic characteristics
Mean age was 39.0 years (standard deviation [SD] = 12.27 years) in the patient group and 36.8 (SD = 12.85) years in the healthy control group.
The differences between the two samples did not reach significance regarding age distribution (t = 1.414; df = 304; p(t) = 0.158; mean difference = 2.176; 95% confidence interval of the difference –0.852 to 5.205) and sex distribution. Both samples consisted of about two-thirds of women. More patients than controls were divorced. The data regarding the highest professional qualification were significantly different (Table 2).
Table 2. Demographic characteristics of the samples.
| Control group | Patient group | Chi-square test/ Fisher’s exact test | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | χ2 | df | p(χ 2) | ||
| Sex | Male Female |
34 61 |
35.8 64.2 |
62 150 |
29.2 70.8 |
1.307*1 | 1 | 0.253 |
| Fisher’s exact test | p | |||||||
| Marital status | Single Married Separated/divorced Widowed |
51 36 6 2 |
53.7 37.9 6.3 2.1 |
101 63 39 9 |
47.6 29.7 18.4 4.2 |
9.606*2 | 0.020 | |
| Professional qualification | Still in education Apprenticeship/technical college Master craftsman Technical university/university No qualifications Other |
14 50 1 24 0 6 |
14.7 52.6 1.1 25.3 0.0 6.3 |
9 123 7 38 21 14 |
4.2 58.0 3.3 17.9 9.9 6.6 |
24.180*3 | <0.001 | |
*10 cells (0%) have an expected frequency below 5. The minimal expected frequency is 29.71
*21 cell (12.5%) has an expected frequency below 5. The minimal expected frequency is 3.40
*31 cell (8.3%) has an expected frequency below 5. The minimal expected frequency is 2.48
Prevalence of dental fear in the psychosomatic patient group
Almost one in three patients (30.5%, n = 64) had pathologically high levels of dental fear; 24 (38.5%) of these had not visited a dentist in more than a year. 40 (62.5%) of the 64 patients had visited a dentist within the preceding year. In the healthy sample, only 4.2% (n = 4) had high levels of dental fear. Two out of these four controls had not visited a dentist within the preceding year. Both samples did, however, differ to a significant degree in terms of the intensity of their dental fear (χ2= 30.657; df = 2; p(χ2) <0.001).
Our analysis of the data for the individual diagnostic groups showed clear, disorder specific differences in the frequency distribution in the three HAQ groups. Patients with post-traumatic stress disorder ((χ2= 46.892; df = 2; p((χ2) < 0.001), anxiety disorders ((χ2= 23.172; df = 2; p(χ2) < 0.001), and depressive disorders ((χ2= 12.525; df = 2; p((χ2) = 0.002) differed from healthy controls. No relevant differences were seen for the diagnostic group “eating disorders” (Fisher’s exact test = 4.382; p = 0.089) and somatoform disorders (Fisher’s exact test = 4.559; p = 0.088). Regression analyses showed that the presence of post-traumatic stress disorder (odds ratio [OR] =16.836; 95% CI 5.606–50.567; ß = 2.823; p<0.001) and of anxiety and/or depressive disorders (OR = 7.646; 95% CI to 2.564–22.807; ß = 2.034; p<0.001) were significant predictors of a high degree of dental fear. Participants’ professional qualifications did not affect findings to a statistically significant degree (OR = 0.954; 95% CI 0.770–1.182; ß = –0.047; p = 0.666).
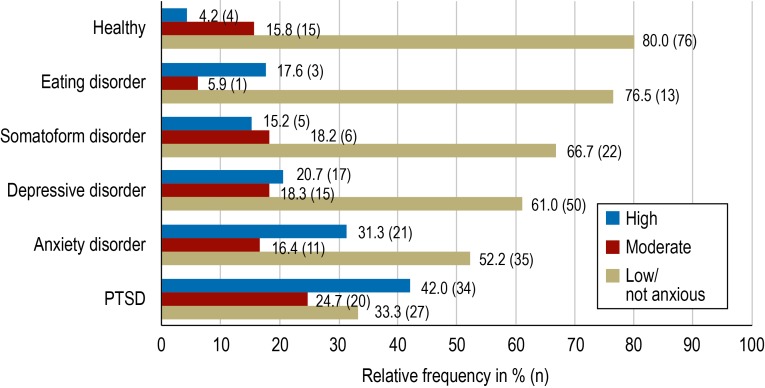
High fear of dental treatment was 10 times more prevalent in patients with post-traumatic stress disorder (42.0%, n = 34) than in healthy subjects (relative risk [RR] = 9.97; 95% CI 3.69–26.90). In the diagnostic group “anxiety disorders,” 31.3% (n = 21) experienced high fear of dental treatment (RR 7.44; 95% CI 2.68–20.70) and in the group “depressive disorders”, 20.7% (n = 17) of patients were affected (RR 4.92; 95% CI 1.73–14.05). The Figure shows the corresponding frequencies for no/low and moderate intensities of dental fear.
Figure.
Frequency distribution
of the intensities of fear of dental treatment within groups PTSD, post-traumatic stress disorder
Self-assessment of the intensity of dental fear
63.8% (n = 134) of patients answered “yes” to the question of whether they were afraid of dental treatment. Of the healthy subjects, only 38.9% (n = 37) reported fear (((χ2=16.414; df = 1; p(((χ2)<0.001). 72.1% (n = 49) of participants who had been identified as highly anxious according to their HAQ scores (n = 68) assessed their fear of dental treatment as high, and 26.5% (n = 18) assessed themselves as “moderately” anxious. 87.5% (n = 49) of those who rated themselves as highly anxious (n = 56) were assessed by the HAQ as having “high anxiety,” and 12.5% (n = 7) were allocated to the moderate category in the HAQ.
A comparison between the three fear intensity groups in the HAQ and those found in the self-assessment yields a highly significant chi-square value (((χ2= 255.826; df = 4; p(((χ2) <0.001). Data for all three anxiety groups (no/low, moderate, high fear of dental treatment) is shown in Table 3.
Table 3. Comparison of self rated fear and categorization on the Hierarchical Anxiety Questionnaire (HAQ).
| Self assessment of fear | ||||||
|---|---|---|---|---|---|---|
| No anxiety or low anxiety | Moderate anxiety | Highanxiety | Total | |||
| Hierarchical AnxietyQuestionnaire (HAQ) | No/low anxiety | Number % within HAQ % within self assessment Corrected residuals |
156 86.2% 91.2% 12.8 |
25 13.8% 32.1% –5.7 |
0 0.0% 0.0% –10.0 |
181 100.0% 59.3% |
| Moderate anxiety | Number % within HAQ % within self assessment Corrected residuals |
14 25.0% 8.2% –5.2 |
35 62.5% 44.9% 7.0 |
7 12.5% 12.5% –1.3 |
56 100.0% 18.4% |
|
| High anxiety | Number % within HAQ % within self assessment Corrected residuals |
1 1.5% 0.6% –10.3 |
18 26.5% 23.1% 0.2 |
49 72.1% 87.5% 13.0 |
68 100.0% 22.3% |
|
| Total | Number % within HAQ % within self assessment |
171 56.1% 100.0% |
78 25.6% 100.0% |
56 18.4% 100.0% |
305 100.0% 100.0% |
|
Avoidance behavior
Of 134 patients and 35 controls who answered “yes” to the question of whether they experienced fear of dental treatment, 56.0% (n = 75) of patients and 22.9% (n = 8) of controls had cancelled or not attended dental appointments because of their fear. Among patients who rated themselves as highly anxious (n = 50), this was the case for 82.0% (n = 41). Three out of 6 highly anxious controls had also cancelled appointments for that reason.
Discussion
The results show that pathologically high fear of dental treatment is a common comorbidity in several mental disorders. Almost one in three patients in our psychosomatic treatment center is affected by dental fear. 62.5% of highly anxious patients had visited a dentist within the past year. This means that compared to the general population in Germany, they are clearly below the average: According to the German Oral Health Study (20), 76.1% of adults visit their dentist at least once a year. Avoiding already arranged appointments is a clear indicator of dental fear (21); 82% of patients who rated themselves as highly anxious displayed such avoidance behavior. The highest prevalence rates of a high degree of dental fear were seen in patients with post-traumatic stress disorder (42.0%), anxiety disorders (31.3%), and depressive disorders (20.7%).
To date, studies have determined comorbidities in fear of dental treatment on the basis of samples of affected patients. Locker et al. (14) and Roy-Byrne et al. (13) confirmed an increased prevalence of one or more anxiety disorders in people with high dental fear. Locker et al. (14) did not find significant differences in the prevalence of depressive disorders in participants with high and low degrees of dental fear, but in our study high degrees of dental fear were observed in 20.7% of patients with depressive or recurrent depressive disorders. This result is consistent with our expectations. People with depressive disorders are more often affected by specific phobias. The lifetime comorbidity of the two disorders is 24.3% (22).
Since Locker et al. (14) studied exclusively 18 year olds, and since the incidence of depressive disorders rises notably only from late adolescence and after the 20th year of life (23), they observed only anxiety disorders (which usually develop in childhood or early adolescence), but not depressive disorders. The Zurich Cohort Study showed that almost half of young adults with just anxiety disorder develop depression additionally to, or superseding, the anxiety disorder in adolescence (24). Roy-Byrne et al. (13), who—like us—investigated a broad age range, reported a lifetime prevalence of comorbid affective disorders of 43% in patients who are subject to dental fear.
To date, the importance of post-traumatic stress disorder for dental fear had remained unknown. Some studies have found a link between the experience of sexual violence and dental fear (25–28). These studies did not include a psychological diagnosis on the basis of standardized instruments; the psychological symptoms of the study participants therefore remained vastly unexplained. Our own study investigated patients with different origins of their trauma, who were grouped on the basis of the psychopathology they had in common. In patients with post-traumatic stress disorder, we found the highest relative risk for fear of dental treatment. The majority of those affected developed the mental disorder as a result of emotional and physical abuse and/or of experiences of sexual violence in childhood and adolescence. Sexual violence has an important role in the development and persistence of dental fear (25– 28). The effects of physical or emotional injury are thus far unknown and should be investigated in future studies. The results regarding participants’ self-assessment of the intensity of their fear are consistent with those from the questionnaire survey. In routine clinical practice, asking about fear of dental treatment and its intensity is therefore useful in order to gain awareness of the problem without having to spend enormous amounts of time. Our data collection—a naturalistic study—represents the typical cross-sectional profile of psychosomatic treatment centers in Germany. Owing to the high response rate in the questionnaire survey, selection bias due to participants’ interest in the topic can be excluded. As the data collection instruments meet the criteria of DSM-IV, international comparability is ensured. Using structured interviews for the purposes of diagnostic evaluation ensures a high degree of objectivity in allocating a diagnosis in the patient sample. Only the most common mental disorders at the syndrome level were captured by using the PHQ-D for the control sample; the presence of further disorders cannot be ruled out.
Conclusion
In routine clinical practice, it is easy to ask patients whether they experience fear of dental treatment. In patients with post-traumatic stress disorder, anxiety disorders, or depressive disorders, the possibility of dental fear should always be borne in mind. Doctors from different medical specialties, who are in close contact with such patients, can help early detection of the disorder through targeted questioning. Awareness of the problem should also prompt dentists to think about post-traumatic stress disorder in phobic patients. Treating patients with mental multimorbidities is the biggest challenge for psychotherapists and dentists and requires close interdisciplinary collaboration.
Key Messages.
The intensity of dental fear was determined in 212 patients in a psychosomatic treatment center and in 95 healthy controls.
Almost one in three patients with one or several mental disorders is affected by pathologically high dental fear. In the healthy control sample, only 4.2% are affected.
42.0% of patients with post-traumatic stress disorder, 31.3% with anxiety disorders, and 20.7% with depressive disorders are affected by a high degree of dental fear.
Affected persons are aware of their fear and mostly rate their degree of fear correctly.
Patients at increased risk should be asked about dental fear in a targeted manner, in order to improve early detection.
Acknowledgments
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Mehrstedt M. Kröning: Ansanger Verlag GmbH; 2007. Zahnbehandlungsängste: Analyse empirischer Forschungsergebnisse aus der Literatur und Untersuchungsergebnisse aus der Praxis. [Google Scholar]
- 2.Berggren U. Psychosocial effects associated with dental fear in adult dental patients with avoidance behaviours. Psychol Health. 1993;8:185–196. [Google Scholar]
- 3.Kent G, Rubin G, Getz T, Humphris G. Development of a scale to measure the social and psychological effects of severe dental anxiety: social attributes of the Dental Anxiety Scale. Community Dent Oral Epidemiol. 1996;24:394–397. doi: 10.1111/j.1600-0528.1996.tb00886.x. [DOI] [PubMed] [Google Scholar]
- 4.Kvale G, Raadal M, Vika M, Johnsen BH, Skaret E, Vatnelid H, Øiamo I. Treatment of dental anxiety disorders. Outcome related to DSM-IV diagnoses. Eur J Oral Sci. 2002;110:69–74. doi: 10.1034/j.1600-0722.2002.11204.x. [DOI] [PubMed] [Google Scholar]
- 5.Thomb A, Sartory G, Jöhren P. Comparison of one-session treatment and benzodiazepine in dental phobia. J Consul Clin Psychol. 2000;68:378–387. doi: 10.1037//0022-006x.68.3.378. [DOI] [PubMed] [Google Scholar]
- 6.Wennström A, Wide Boman U, Stenman U, Ahlqwist M, Hakeberg M. Oral health, sense of coherence and dental anxiety among middle-aged women. Acta Odontol Scand. 2013;71:256–262. doi: 10.3109/00016357.2012.671362. [DOI] [PubMed] [Google Scholar]
- 7.Armfield JM, Slade GD, Spencer AJ. Dental fear and adult oral health in Australia. Community Dent Oral Epidemiol. 2009;37:220–230. doi: 10.1111/j.1600-0528.2009.00468.x. [DOI] [PubMed] [Google Scholar]
- 8.Mehrstedt M, John MT, Tönnies S, Micheelis W. Oral health-related quality of life in patients with dental anxiety. Community Dent Oral Epidemiol. 2007;35:357–363. doi: 10.1111/j.1600-0528.2007.00376.x. [DOI] [PubMed] [Google Scholar]
- 9.Wide Boman U, Wennström A, Stenman U, Hakeberg M. Oral health-related quality of life, sense of coherence and dental anxiety: An epidemiological crosssectional study of middle-aged women. BMC Oral Health. 2012;12 doi: 10.1186/1472-6831-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore R, Brødsgaard I, Rosenberg N. The contribution of embarrassment to phobic dental anxiety: a qualitative research study. BMC Psychiatry. 2004;4 doi: 10.1186/1471-244X-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kvale G, Berggren U, Milgrom P. Dental fear in adults: a meta-analysis of behavioral interventions. Community Dent Oral Epidemiol. 2004;32:250–264. doi: 10.1111/j.1600-0528.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 12.Schwichtenhövel J. Dissertation zur Erlangung der Doktorwürde der Universität Bern. Bern: Medizinische Fakultät; 2008. Zahnbehandlungsangst und ihre Wechselwirkung mit der Mundgesundheit und der mundgesundheitsbezogenen Lebensqualität. [Google Scholar]
- 13.Roy-Byrne PP, Milgrom P, Khoon-Mei T, Weinstein P, Katon W. Psychopathology and psychiatric diagnosis in subjects with dental phobia. J Anxiety Disord. 1994;8:19–31. [Google Scholar]
- 14.Locker D, Poulton R, Thomson WM. Psychological disorders and dental anxiety in a young adult population. Community Dent Oral Epidemiol. 2001;29:456–463. doi: 10.1034/j.1600-0528.2001.290607.x. [DOI] [PubMed] [Google Scholar]
- 15.Jöhren P. Validierung eines Fragebogens zur Erkennung von Zahnbehandlungsangst (HAF) Zahnärztl Welt Ref. 1999;108:104–114. [Google Scholar]
- 16.Corah NL. Development of a dental anxiety scale. J Dent Res. 1969;48:596–602. doi: 10.1177/00220345690480041801. [DOI] [PubMed] [Google Scholar]
- 17.Wittchen HU, Wunderlich U, Gruschwitz S, Zaudig M. Göttingen: Hogrefe Verlag; 1997. Strukturiertes klinisches Interview für DSM IV (SKID) [Google Scholar]
- 18.Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the structured clinical interview for DSM-IV axis I disorders (SCID I) and axis II disorders (SCID II) Clin Psychol Psychother. 2011;18:75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- 19.Löwe B, Spitzer RL, Zipfel S, Herzog W. Autorisierte deutsche Version des Prime MD Patient Health Questionnaire (PHQ). 2. Auflage. New York: Pfizer; 2002. PHQ-D Gesundheitsfragebogen für Patienten. Manual Komplettversion und Kurzform. [Google Scholar]
- 20.Micheelis W, Schiffner U. Köln: Deutscher Ärzte-Verlag; 2006. Vierte Deutsche Mundgesundheitsstudie (DMS IV) [Google Scholar]
- 21.Kleinknecht RA. The assessment of dental fear. Behav Ther. 1978;9:626–634. [Google Scholar]
- 22.Kessler RC, Nelson CB, McGonagale KA, Liu J, Swartz M, Blazer DG. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry. 1996;168:17–30. [PubMed] [Google Scholar]
- 23.Onken M, Ströhle A. Komorbidität von Angst und Depression. In: Bauer M, Berghöfer A, Adli M, editors. Akute und therapieresistente Depressionen. Pharmakotherapie - Psychotherapie - Innovationen. 2nd ed. Berlin, Heidelberg: Springer; 2005. pp. 105–114. [Google Scholar]
- 24.Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Arch Gen Psychiatry. 2003;60:993–1001. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 25.Hays KF, Stanley SF. The impact of childhood sexual abuse on women’s dental experiences. J Child Sex Abus. 1996;5:65–74. [Google Scholar]
- 26.Walker EA, Milgrom PM, Weinstein P, Getz T, Richardson R. Assessing abuse and neglect and dental fear in women. J Am Dent Assoc. 1996;127:485–490. doi: 10.14219/jada.archive.1996.0240. [DOI] [PubMed] [Google Scholar]
- 27.Willumsen T. Dental fear in sexually abused women. Eur J Oral Sci. 2001;109:291–296. doi: 10.1034/j.1600-0722.2001.00069.x. [DOI] [PubMed] [Google Scholar]
- 28.Leeners B, Stiller R, Block E, Görres G, Imthurn B, Rath W. Consequences of childhood sexual abuse experiences on dental care. J Psychosom Res. 2007;62:581–588. doi: 10.1016/j.jpsychores.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 29.Gräfe K, Zipfel S, Herzog W, Löwe B. Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D)” Ergebnisse der deutschen Validierungsstudie. Diagnostica. 2004;50:171–181. [Google Scholar]