Abstract
Background
The incidence of decubitus ulcers is an established quality indicator for external quality assurance in the inpatient setting. Epidemiologic analyses of the frequency of, and risk factors for, decubitus ulcers in routine care are lacking.
Method
We analyzed routine decubitus-ulcer documentation data relating to all inpatients of the University Hospital of Dresden, Germany, from 2007 to 2011 (n = 246 162 patients). The prevalence and incidence of decubitus ulcers and demographic and illness-related risk factors for them were determined with the use of descriptive techniques and logistic regression models. The effort-to-benefit ratio of documenting decubitus ulcers in various care scenarios was calculated in terms of the number of additional patients to be documented for each patient with incident decubitus ulcer.
Results
The prevalence of decubitus ulcers was 1.21%, and their incidence during inpatient treatment was 0.78%, with significant differences across clinical care units (range of ward-specific incidences: 0.0% to 12.7%). Predictors for the development of a new decubitus ulcer during a hospital stay included higher age (odds ratio [OR] 1.03 per year, 95% confidence interval [CI] 1.02–1.03), longer hospital stay (OR 1.03 per day, 95% CI 1.031–1.033), treatment in an intensive care unit (OR 2.88, 95% CI 2.58–3.22), and transfer to the hospital from a residential nursing-care facility (OR 6.05, 95% CI 5.13–7.11). The patient’s sex and the severity of disease were not correlated with the incidence of decubitus ulcers. The effort-to-benefit ratio could be improved if wards with a low incidence of decubitus ulcers (<0.5%) either entirely discontinued the current hospital-wide procedure for documenting decubitus ulcers (with one new ulcer for every 645 patients) or continued it only for patients aged 65 or older (with one new ulcer for every 902 patients).
Conclusion
There are major differences between clinical care units in the risk of decubitus ulcers. Epidemiological analysis of routine quality management data is useful to assess the benefit of measures taken in medical care. Continuing evaluation is essential.
Screening for decubitus ulcers is an important medical issue that has a wider impact than just inpatient care. Decubitus screening typically incorporates preventative measures. In order to assure high quality patient care in German hospitals, there are guidelines available on how to deal with decubitus ulcers, such as the Expertenstandard Dekubitusprophylaxe (1).
The European Pressure Ulcer Advisory Panel (EPUAP) defines decubitus or pressure ulcer as a „localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear.“ (2, 3). Decubitus ulcers are divided into four stages; the spectrum ranges from stage 1 (non-blanchable erythema) to stage 4 (full-thickness tissue loss) (4). Intrinsic risk factors for decubitus ulcers include age, weight, inactivity, and malnutrition. Extrinsic risk factors include rubbing and shearing forces, moisture, positioning and treatment with some medications (for example, analgesics, sedatives, or sleeping pills) (4).
The recognition and subsequent treatment of a decubitus ulcer in a clinical setting is a meaningful indicator of quality of care (5).
Despite its great clinical and health-policy importance, there is a lack of recent epidemiological data on the frequency, severity and risk factors for decubitus ulcers in inpatients. In order to effectively institute evidence-based health care management, the methods for quality management must also adhere to scientific standards. Only when valid data are available can one evaluate and then implement cost-benefit decisions both for patients and service providers (6). In order to address the relevant unanswered questions regarding quality assurance in inpatient care, we analyzed the routine data covering five years of decubitus screening and prophylaxis in a tertiary hospital.
Methods
Type of study and database
The database included all patients admitted to and discharged from the University Hospital of Dresden, Germany, between 2007 and 2011 (n= 251 928). Patients who were admitted before 1 January 2007 or discharged after 31 December 2011 (n = 5766) were excluded so that a total of 246 162 cases were analyzed.
During the entire study period, all inpatients in all clinical care units underwent decubitus screening. The evaluation points were admission, change in general condition (subjective opinion of treating physician), seven days after last evaluation, and at discharge. Specially trained nursing personnel performed the decubitus prophylaxis examination including evaluation of the entire skin surface and documentation of pre-existing or new decubitus ulcers. If the nursing personnel identified a decubitus ulcer, this was confirmed by the treating physician or a consultant and coded either as a primary diagnosis or a (care-relevant) secondary diagnosis (7). In addition, the stage (stage 1–4) and location of the decubitus ulcer were noted.
The primary study outcome was de novo decubitus ulcer developed during hospitalization. In addition, decubitus ulcers already present at the time of admission were analyzed. Both new and pre-existing ulcers were stratified according to patient-related factors (age, sex, patient clinical complexity level [PCCL], care of patient before admission, duration of stay, type of ward (medical, surgical, mixed, psychiatric, palliative) and level of care (intensive care unit versus normal care unit).
The Braden scale (8) was used for each patient in each assessment to estimate the risk of a patient developing a new decubitus ulcer. The Braden scale is a validated instrument for estimating decubitus risk using six parameters:
Each item is assigned one to four points (in one case, three); their sum is the total score, ranging between 6 and 23 points; a higher Braden score indicates a lower decubitus risk. The usual cut-off for increased decubitus risk is 19 points (12, 13). An experienced evaluator can determine the Braden score in one to three minutes, as shown by random measurements. The documentation of the Braden score was accomplished in our patients with a special program in the hospital information system (ORBIS). In addition to the Braden score, other potentially relevant data regarding decubitus risk were also recorded; these included demographic characteristics (age and sex), type of care prior to admission, duration of stay, and PCCL.
Statistical analysis
The incidence of new and prevalence of pre-existing decubitus ulcers were first analyzed on an annual basis. Since there was no trend towards an increase or decrease in frequency over the study period, all further analyses were based on data covering the entire period from 2007 through 2011. In addition to the decubitus ulcer incidence during hospitalization (primary outcome) and prevalence on admission, the clinical course of the ulcer during the hospital stay was also considered.
Explorative univariate logistic regression models were employed to identify the determinants of new decubitus ulcers during hospitalization while considering both patient characteristics and the characteristics of the hospitalization. For the cost-benefit analysis, the 30 different specialty services and wards were categorited based on their incidence rates for decubitus ulcers into low (<0.5%), medium (0.5–2.0%) and high (>2.0%) risk sites. The risk factors were analyzed using odds ratios and 95% confidence intervals.
To assess the cost-benefit relation for decubitus screening in different care scenarios, the number of additional patients screened per patient with incident decubitus ulcer was calculated. In this approach we distinguished between scenarios which incorporated the Braden score or did not employ it. The scenarios without Braden score were based upon socio-demographic factors such as the patient’s age, the admitting service, or a combination of both. Scenarios employing the Braden score varied only in the cut-off point for an increased decubitus risk. The scenarios were developed considering both the risk factors identified for new decubitus ulcers and the practical implementation of decubitus screening in daily care.
Results
The prevalence of decubitus ulcers during the entire 5-year period was 1.21% (n = 2971). A total of 1914 patients developed a new decubitus ulcer during their hospitalization (incidence 0.78%), but with clear differences between different specialties (incidence 0.0%–12.7%). In 43.1% (n = 1278) of the patients, the decubitus ulcer improved during the hospitalization. In 11% (n = 327), the ulcer’s stage was higher at discharge. In 36.6% (n = 1089) of patients with decubitus at admission, no decubitus ulcer was present at discharge (Table 1).
Table 1. Prevalence of decubitus ulcers at admission, course during hospitalization and incidence of new decubitus ulcers (University Hospital of Dresden; 2007 through 2011; n= 246162).
| Year | ||||||
|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | 2010 | 2011 | Total | |
| Decubitus prevalence (n; %) |
n=544; 1.20% |
n=550; 1.13% |
n=618; 1.23% |
n=634; 1.24% |
n=625; 1.23% |
n=2971; 1.21% |
|
n=236; 43.4% |
n=199; 36.2% |
n=223; 36.1% |
n=216; 34.1% |
n=215; 34.4% |
n=1089; 36.6% |
|
n=285; 52.4% |
n=257; 46.7% |
n=244; 39.5% |
n=263; 41.5% |
n=229; 36.6% |
n=1278; 43.1% |
|
n=62; 11.4% |
n=55; 10% |
n=71; 11.5% |
n=74; 11.7% |
n=65; 10.4% |
n=327; 11% |
| Decubitus incidence (n; %) |
n=364; 0.80% |
n=416; 0.86% |
n=401; 0.80% |
n=391; 0.76% |
n=342; 0.67% |
n=1914 0.78% |
Low-grade (stage 1 and 2) ulcers were more common than high-grade (stage 3 and 4) ulcers both among pre-existing ulcers and new ones that developed in the hospital. The following stages for new decubitus ulcers were documented in the discharge notes (eTable 1):
eTable 1. Stage of decubitus ulcer in all patients at admission and discharge.
| Stage of decubitus ulcer at discharge | |||||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | Total | ||
| Stage of decubitus ulcer at admission | 0 | 241381 | 783 | 916 | 157 | 58 | 243295 |
| 1 | 608 | 428 | 159 | 41 | 21 | 1257 | |
| 2 | 279 | 114 | 507 | 77 | 16 | 993 | |
| 3 | 72 | 28 | 93 | 255 | 12 | 460 | |
| 4 | 30 | 6 | 16 | 33 | 72 | 157 | |
| Total | 242370 | 1359 | 1691 | 563 | 179 | 246162 | |
Stage 1 decubitus ulcer—784 of 1914 new cases (41%)
Stage 2 decubitus ulcer—915 cases (48%)
Stage 3 decubitus ulcer—157 cases (8%)
Stage 4 decubitus ulcer— 58 cases (3%).
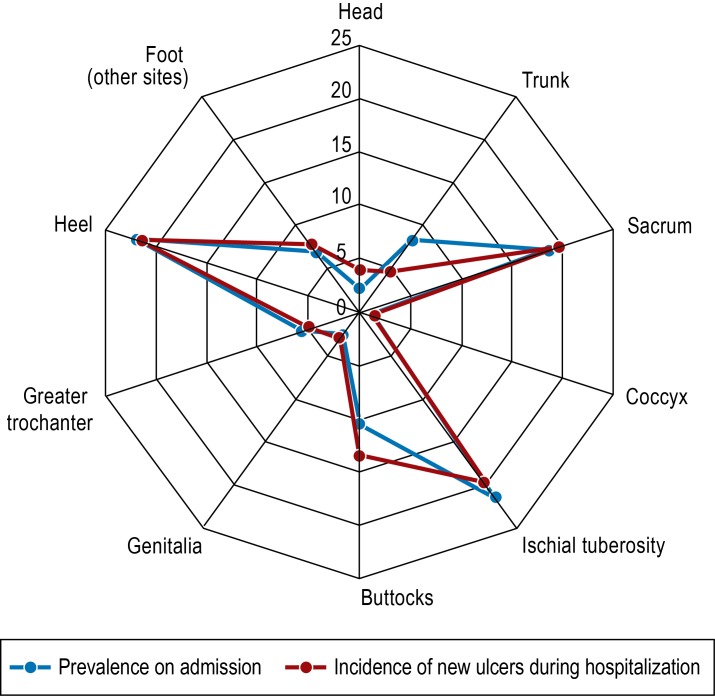
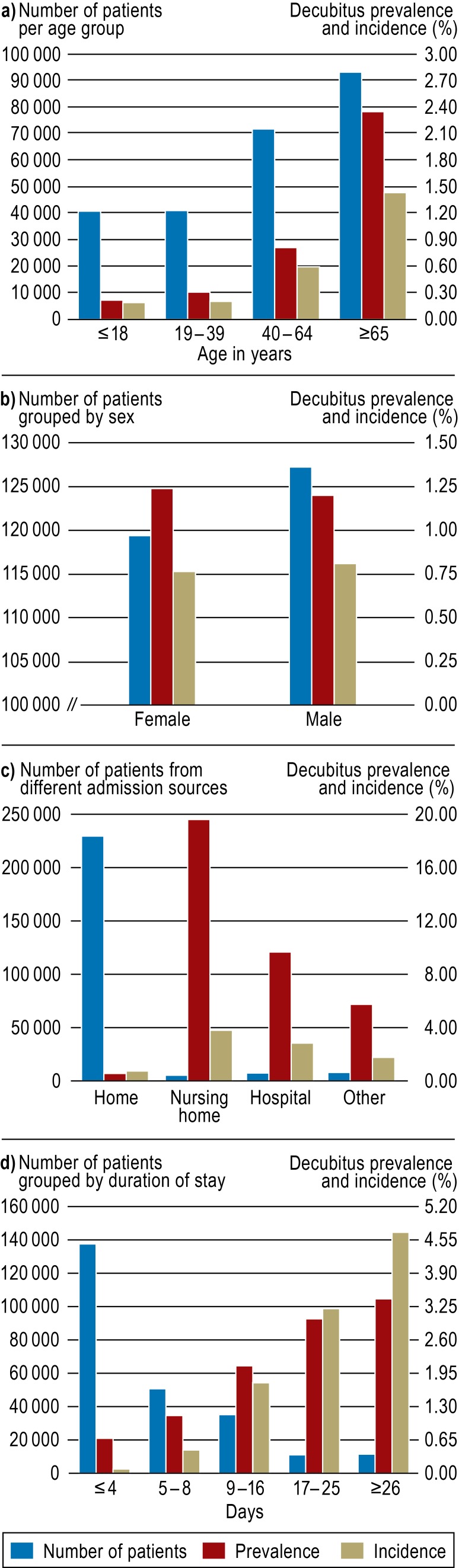
The most common site for both pre-existing and new ulcers were the heel (22%; 21.7%), ischial tuberosity (21.6%; 19.7%), and sacrum (18.5%; 19.5%) (Figure 1). The frequency of both pre-existing and new ulcers rose with increasing patient age and duration of stay. Patients who were transferred from a nursing home or another hospital had a much higher prevalence of decubitus ulcers at admission (almost 20%; 10%) than did those who were admitted from home (prevalence 0.52%). There was no difference between the sexes (Figure 2). The relationship between prevalence or incidence and patient age is shown for each type of care unit in an online supplement (eFigure 1– 3).
Figure 1.
Prevalence and incidence of decubitus ulcers in inpatients based on anatomic location (in %). Prevalence (n= 2971); incidence (n=1914)
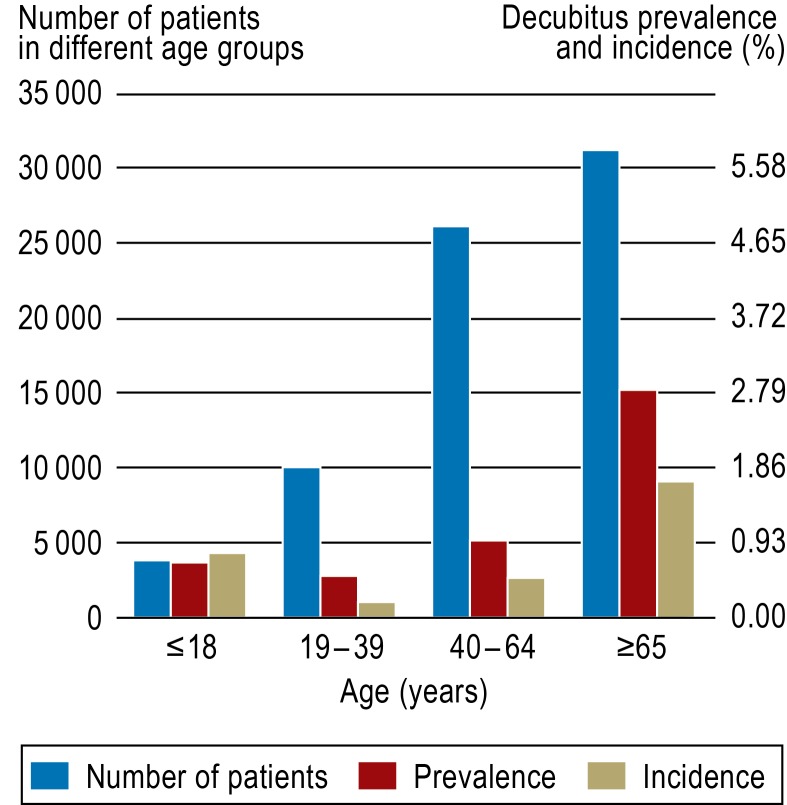
Figure 2.
Analysis of socio-demographic risk factors for decubitus ulcers. Prevalence (n = 2971) and incidence (n = 1914) of decubitus ulcers in inpatients (n = 246 162).
a) Age
b) Sex
c) Source of admission
d) Duration of stay
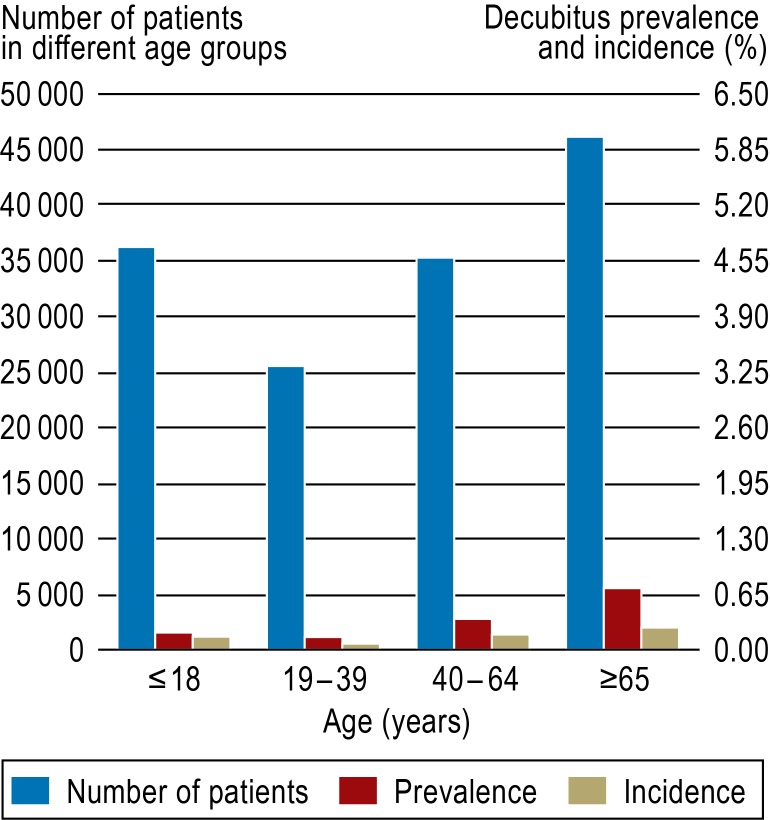
eFigure 1.
Prevalence (n = 551) and incidence (n = 221) of decubitus ulcers in different age groups in clinical units with low decubitus risk (<0.5%) (n = 142 483)
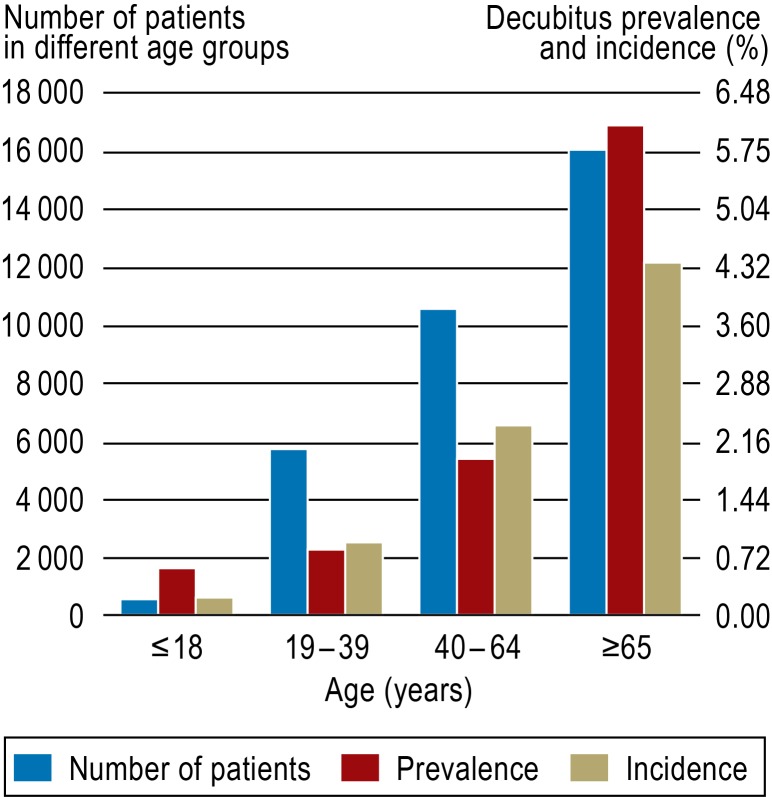
eFigure 3.
Prevalence (n = 1233) and incidence (n = 1002) of decubitus ulcers in different age groups in clinical units with high decubitus risk (>2%) (n = 32 735)
Factors which were associated with an increased risk for developing a new decubitus ulcer during hospitalization included age (odds ratio [OR]: 1.03; 95% confidence interval [95% CI]: 1.02–1.03 per year, Braden score (OR: 1.19; 95% CI: 1.18–1.21 per reduction of one point), duration of stay (OR: 1.03; 95% CI: 1.031–1.033 per day), and treatment in intensive care unit (ICU) (OR: 2.88; 95% CI: 2.58–3.22), as well as transfer from a nursing home (OR: 6.05; 95% CI: 5.13–7.11) or another hospital (OR: 4.58; 95% CI: 3.90–5.39) as compared to admission from home. The incidence was 2.24% in the age group 80–89 years and 6.25% in those 90 years of age or older. Sex and disease severity (PCCL) were not associated with an increased decubitus risk (eTables 2 and 3).
eTable 2. Results of logistic regression analysis of risk factors for decubitus ulcers.
| Risk factors for decubitus ulcers | Odds Ratio (95% Confidence Interval) |
|---|---|
| Age (per year) | 1.03 (1.02–1.03) |
| Age group (Reference; patients <19 years) 19–39 years 40–64 years ≥ 65 years |
1.03 (0.76–1.42) 3.04 (2.38–3.87) 7.44 (5.92–9.36) |
| Sex (Reference: female) | 1.01 (0.91–1.09) |
| Braden score (per point lower score) | 1.19 (1.18–1.21) |
| Care of patient prior to admission (Reference: admitted from home) Nursing home Hospital Other |
6.03 (5.12–7.11) 4.58 (3.90–5.39) 2.65 (2.16–3.25) |
| Severity of disease (PCCL) | 0.99 (0.97–1.002) |
| Duration of stay (per day) | 1.03 (1.031–1.033) |
| Duration of stay, grouped (Reference: 1–4 days) 5 – 8 days 9 – 16 days 17 – 25 days ≥ 26 days |
4.23 (3.41–5.24) 11.94 (9.88–14.42) 20.22 (16.52–24.74) 35.83 (29.56–43.42) |
| Intensive care unit (Reference: normal ward) | 2.88 (2.58–3.22) |
| Clinical care unit (Reference: unit with a decubitus ulcer incidence <0.5%) Unit with decubitus ulcer incidence 0.5–2% Unit with decubitus ulcer incidence >2% |
6.33 (5.44–7.36) 20.32 (17.56–23.52) |
PCCL, patient clinical complexity level
eTable 3. Prevalence, incidence and risk (odds ratio) of decubitus ulcer in 10-year age groups.
| Decubitus ulcer prevalence (in %) | Decubitus ulcer incidence (in %) | Odds ratio (95% confidence interval) | |
|---|---|---|---|
| 0–9 years | 0.18 | 0.15 | Reference |
| 10–19 years | 0.31 | 0.27 | 1.82 (1.17–2.83) |
| 20–29 years | 0.33 | 0.22 | 1.43 (0.93–2.18) |
| 30–39 years | 0.28 | 0.19 | 1.27 (0.82–1.99) |
| 40–49 years | 0.62 | 0.45 | 3.01 (2.11–4.3) |
| 50–59 years | 0.87 | 0.63 | 4.2 (3.01–5.87) |
| 60–69 years | 1.15 | 0.77 | 5.12 (3.71–7.06) |
| 70–79 years | 1.80 | 1.23 | 8.27 (6.04–11.32) |
| 80–89 years | 4.04 | 2.24 | 15.16 (11.04–10.81) |
| over 89 years | 11.92 | 6.25 | 31.26 (22.03–44.35) |
There were considerable differences between the medical and surgical units with the incidence of decubitus ulcers ranging from 0.01% to 5.45% on medical wards and 0.34% to 10.94% on surgical wards. The incidence was low on the psychiatry and psychosomatic medicine wards (0.0%–0.24%), while 5.69% of the patients on the palliative care ward developed ulcers. There was also a clear difference between normal care units (NCU) and intensive care units (ICU). The NCUs had an incidence of 0.60% while that of the ICUs was 4.78% (0.49–12.7%) (Table 2)
Table 2. Decubitus ulcer incidence in clinical care units.
| Type of care | Decubitus incidence rate (range of units providing same type of care) |
|---|---|
| Medical | 1.42% (0.01–5.51%) |
| Surgical | 2.76% (0.34–10.93%) |
| Medical/surgical | 0.21% (0.13–0.30%) |
| Psychiatric | 0.08% (0.0–0.24%) |
| Palliative* | 5.69% |
| Intensive care unit (ICU) | 4.78% (0.49–12.7%) |
| Normal care unit (NCU) | 0.60% (0.0–2.03%) |
*no range; only one unit
Because of the marked heterogeneity in the risk of developing a decubitus ulcer between the medical and surgical specialties, the wards were stratified into three types of risk:
Low risk of decubitus ulcer (<0.5%): This group included all psychiatric units, 7 of 16 medical units and 2 of the 9 surgical units. The average Braden score was 22.03 points with a standard deviation of 2.28.
Medium risk of decubitus ulcer (0.5%–2%): Included here were 6 of the 16 medical units, 4 of the 9 surgical units and 2 of the 7 ICUs. The average Braden score was 21.11 points with a standard deviation of 3.35.
High risk of decubitus ulcer (>2 %): Included here were 3 of the 16 medical units and three of the nine surgical units, as well as five of the seven ICUs and the palliative medicine unit. The average Braden score was 18.46 points with a standard deviation of 4.72.
Analysis of the cost–benefit relationship
If one employs the scenario of „screening only in units with high or medium risk,“ around 88% of patients with new decubitus ulcers would be included in the screening program, while the incidence of ulcers in the patients not affected by this quality management measure would be 0.16%. This corresponds to screening another 645 patients to identify one decubitus ulcer. In this scenario, 142 483 of the 246 162 patients (57.9%) would not have undergone decubitus screening.
An alternative strategy to optimize the cost–benefit relationship is the scenario „screening all patients in units with high or medium risk and all patients 65 years of age or older in low-risk units.“ With this approach 96 489 patients (39.2%) would not be screened for decubitus ulcers. An additional 902 patients would then have to be screened to detect one decubitus ulcer. The incidence in the unscreened patients would be 0.11%. In comparison to these two scenarios, more complex schemes employing the Braden score show no advantages (Table 3).
Table 3. Scenarios for decubitus screening.
| Decubitus (with and without screening) | No decubitus (with and without screening) | % of recognized decubitus ulcers | % of healthy individuals not screened | Incidence of decubitus ulcers among screened | Incidence of decubitus ulcers among non-screened | Number of patients to be additionally screened per patient with new decubitus ulcer | |
|---|---|---|---|---|---|---|---|
| Scenarios not incorporating Braden score | |||||||
| Screening in units with high and medium risk, no screening in units with low risk | 1693 221 |
101 986 142 262 |
88,45% | 58.24% | 1.63% | 0.16% | 645 |
| Screening in units with high and medium risk, screening of patients ≥ 65 years of age in units with low risk | 1807 107 |
147 866 96 382 |
94.41% | 39.46% | 1.21% | 0.11% | 902 |
| Screening in units with high risk, no screening in units with medium or low risk | 1002 912 |
31 733 212 515 |
52.35% | 87.01% | 3.06% | 0.43% | 234 |
| Screening in units with high risk and patients ≥ 65 years of age in units with medium or low risk | 1632 282 |
108 230 136 018 |
85.27% | 55.69% | 1.49% | 0.21% | 483 |
| Screening only of patients ≥ 65 years of age, regardless of risk level of unit | 1331 583 |
91 823 152 425 |
69.54% | 62.41% | 1.43% | 0.38% | 262 |
| Scenarios incorporating the Braden score | |||||||
| Screening in units with high risk and in all patients with Braden score <17 | 1421 493 |
50 497 193 751 |
74.24% | 79.33% | 2.74% | 0.73% | 137 |
| Screening in units with high risk and in all patients with Braden score <16 | 1351 563 |
46 970 197 278 |
70.59% | 80.77% | 2.80% | 0.28% | 351 |
Discussion
In addition to the patient’s age, duration of stay and type of hospital ward, the patient’s prior medical or nursing care also plays an important role. Patients transferred from a nursing home or another hospital had a 6-fold or 4-fold, respectively, increased decubitus risk, as compared to patients admitted from home. There were also striking differences between different clinical care units. Despite an increasing number of admissions, constant average age and number of nursing personnel, there was no change in the incidence of decubitus ulcers during the observation period.
The absolute prevalence and incidence in our cohort is comparable to that of Stausberg who found an incidence of 0.7% to 2.7% but did not differentiate between different types of care units (14).
Since January 2013, decubitus ulcers can be coded as “present on admission,” allowing the distinction between pre-existing ulcers and those acquired during hospitalization. We made the same distinction in our analyses. Our study shows the importance of distinguishing between pre-existing and hospital-acquired decubitus ulcers in accessing quality of care. When interpreting the quality indicator „incidence of decubitus ulcers,“ we feel that the patient’s age, duration of stay, type of hospital ward, and care prior to admission all must be considered.
Our model scenarios for decubitus ulcer screening and documentation provide a basis for the further development of this quality management parameter in an evidence-based fashion. When decubitus screening is limited to the groups most likely to benefit, nursing time is freed up for other aspects of patient care. The decision to institute one of the models we have suggested to reduce decubitus screening to patients or care units with a high risk is not a simple management decision; it also raises medicopolitical and ethical issues. Points to be carefully considered are the number of patients needed to be screened to identify one additional decubitus ulcer, the costs of the screening, and the number of patients with decubitus ulcers who had been screened.
In any event, any reduction in decubitus screening measures—if such a move is even considered—should be evidence based and prospectively evaluated.
The German recommendation “Expertenstandard Dekubitusprophylaxe” makes no official recommendations on what tools should be used to determine decubitus risk (8). Using the Braden score to decide which patients should be screened produced no advantages in our exploratory analyses of alternative scenarios. In our opinion, at this time the use of a tool to assess individual patient risk, such as the Braden score, seems relatively unhelpful because it does not lead to any direct changes in the type or level of care of the patient.
Strengths and weaknesses of the study
This study covers every patient admitted to our hospital from 2007 through 2011. The completeness of the data and the large number of patients are strengths of our study. We used the Braden score, a validated method for assessing risk of decubitus ulcer, which was determined prospectively by trained personnel (9– 11). Routine data from quality management projects have not been extensively investigated to determine their validity. There have been no internal random samples taken to check the data. Furthermore, no external evaluation of the validity and reliability of the data was carried out.
The University Hospital of Dresden is a large tertiary care center. This study includes all the many clinical care areas. We are confident that our results are generalizable to other tertiary care centers in Germany. It is possible that some results are not applicable to more specialized hospitals. This is most likely to be the case when considering the scenarios to assess cost–benefit relationships. The identified risk factors for the development of new decubitus ulcers in inpatients such as age, duration of stay and the type of care prior to admission seem generally applicable.
We were unable to evaluate the individual items in the Braden scale or to compare the prophylactic measures with the final therapeutic outcome. It is certainly possible that the use of such measures in patients without a pre-existing decubitus ulcer reduced the incidence of new ulcers.
Topics for future research
After changing the standards for decubitus screening and prophylaxis, an accompanying and continuous evaluation is needed. If patients at low risk are not screened, they may not receive prophylaxis. One must determine whether this lack of prophylaxis influences the incidence of decubitus ulcers. The evidence for the relationship between various risk factors and the development of decubitus ulcers is limited. Additional possibly relevant risk factors, which we did not consider, include the nutritional status of the patient and other factors which could be grouped as “activities of daily living.“
Key Messages.
This study used routine data to determine the frequency and risk factors of decubitus ulcers for inpatients in a tertiary care facility.
During the time period 2007 through 2011, the prevalence of decubitus ulcers at admission was 1.21%. The incidence of new decubitus ulcers during hospitalization was 0.78%
Risk factors for the development of a decubitus ulcer during hospitalization included higher age, and longer duration of stay, as well as transfer from a nursing home or other hospital. The incidence of decubitus ulcers varied markedly between different types of clinical care units.
The cost–benefit ratio for decubitus screening may be improved by limiting the screening to certain clinical units, older patients or those with other risk factors.
Health services research can make a significant contribution to maximizing cost–benefit ratios by making possible consecutive implementation of scientifically-supported management decisions.
eFigure 2.
Prevalence (n = 1187) and incidence (n = 691) of decubitus ulcers in different age groups in clinical units with medium decubitus risk (0.5–2%) (n = 70 944)
Acknowledgments
Translated from the original German by Walter Burgdorf, MD.
We thank the nursing personnel for collecting the data and the members of the nursing management and screening teams for constructive discussion.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Fechner Björn-Ola. Indikatoren für die Bewertung von Komplikationsraten. Dtsch Arztebl. 2012;109(41):A 2026–A 2030. [Google Scholar]
- 2.European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel 2009. European Pressure Ulcer Advisory Panel. www.epuap.org/guidelines/QRG_Prevention_in_German.pdf. (last accessed on 23 May 2012) [Google Scholar]
- 3.European Pressure Ulcer Advisory Panel 2009. Leitlinie Dekubitus Prävention. Washington, DC. National Pressure Ulcer Advisory Panel. 2007 [Google Scholar]
- 4.Bienstein C, Schröder G, Braun M, Neander K-D. Stuttgart, New York: Thieme Verlag; 1997. Dekubitus: Die Herausforderung für Pflegende; pp. 42–63. [Google Scholar]
- 5.Gesundheitsberichterstattung des Bundes. www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GBEDownloadsT/dekubitus. pdf?__blob=publicationFile. Berlin: Robert-Koch-Institut; Dekubitus. (last accessed on 26 June 2013) [Google Scholar]
- 6.Eberlein-Gonska M. Was ist an Qualitätsmanagement evidenzbasiert? Reflexionen über eine scheinbar einfache Frage. Bundesgesundheitsbl. 2011;54:148–153. doi: 10.1007/s00103-010-1204-y. [DOI] [PubMed] [Google Scholar]
- 7.Institut für das Entgeltsystem im Krankenhaus. Deutsche Kodierrichtlinien. www.dkgev.de/media/file/8223.Deutsche_Kodierrichtlinien_Version_2011_Endversion_A4_im_PDF-5.0-Format_100924.pdf. 2011 (last accessed on 20 June 2013) [Google Scholar]
- 8.Deutsches Netzwerk für Qualitätsentwicklung in der Pflege. Expertenstandard Dekubitusprophylaxe in der Pflege. (1st revised edition 2010) Osnabrück. 2010 [Google Scholar]
- 9.Bergstrom N, Braden B. The Braden Scale for predicting pressure sore risk. Nursing Research. 1987;47:205–210. [PubMed] [Google Scholar]
- 10.Bergstrom N, Demuth PJ, Braden B. A clinical trial of the Braden Scale for predicting pressure sore risk. Nursing Clinics of North America. 1989;22:417–428. [PubMed] [Google Scholar]
- 11.Braden B, Bergstrom N. Clinical utility of the Braden Scale for predicting pressure sore risk. Advances in Skin & Wound Care. 1989;2:44–51. [Google Scholar]
- 12.Bergstrom N, Braden B, Kemp M, Champagne M, Ruby E. Predicting Pressure Ulcer Risk: A multisite study of the predictive validity of the Braden Scale. Nursing Research. 1998;47:261–269. doi: 10.1097/00006199-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Braden B, Bergstrom N. Predictive validity of the Braden Scale for pressure score risk in a nursing home population. Research in Nursing & Health. 1994;17:459–470. doi: 10.1002/nur.4770170609. [DOI] [PubMed] [Google Scholar]
- 14.Stausberg KM. Häufigkeit des Dekubitus an einem Universitätsklinikum. Dtsch Med Wochenschr. 2005;130:2311–2315. doi: 10.1055/s-2005-918568. [DOI] [PubMed] [Google Scholar]