Abstract
Objectives
The purpose of this study was to compare the prevalence of conduct problems in a well-documented sample of Barbadian adolescents malnourished as infants and a demographic comparison group and to determine the extent to which cognitive impairment and environmental factors account for this association.
Methods
Behavioral symptoms were assessed using a 76-item self-report scale in 56 Barbadian youth (11–17 years of age) with histories of protein–energy malnutrition (PEM) limited to the first year of life and 60 healthy classmates. Group comparisons were carried out by longitudinal and cross-sectional multiple regression analyses at 3 time points in childhood and adolescence.
Results
Self-reported conduct problems were more prevalent among previously malnourished youth (P < 0.01). Childhood IQ and home environmental circumstances partially mediated the association with malnutrition. Teacher-reported classroom behaviors at earlier ages were significantly correlated with youth conduct problems, confirming the continuity of conduct problems through childhood and adolescence.
Discussion
Self-reported conduct problems are elevated in children and adolescents with histories of early childhood malnutrition. Later vulnerability to increased conduct problems appears to be mediated by the more proximal neurobehavioral effects of the malnutrition on cognitive function and by adverse conditions in the early home environment.
Keywords: Conduct problem, Malnutrition, Adolescence, Cross-cultural, Longitudinal study
Introduction
Early childhood malnutrition is associated with adverse outcomes in school-aged children and adolescents, including an increased prevalence of conduct problems and aggressive behaviors.1–4 These behaviors are of particular concern because they can forecast lifelong social problems, sometimes serious.5–7 Because malnutrition is estimated to afflict as many as two hundred million children worldwide,2 the potentially increased prevalence of aggressive symptoms in adolescents malnourished earlier in life is of considerable social significance.
The etiology of conduct problems in childhood is not well understood.8 The biological impact of malnutrition on the developing brain leads to a variety of developmental changes that may explain the increased prevalence of conduct problems.9 However, conduct problems may also result more proximally from intervening variables, such as cognitive impairment, a well-recognized outcome of infant malnutrition.10,11 Adverse social circumstances that generally co-exist with malnutrition can also increase the risk of antisocial behaviors and conduct problems.8
In the present report, we examine these issues in the context of the Barbados Nutrition Study (BNS). The BNS has followed over the course of decades the development of a group of Barbadian children with normal birth weights who experienced a single and well-documented episode of moderate–severe protein–energy malnutrition limited to the first years of life12 and compared them to healthy classmates from the same neighborhoods. Index children were identified at hospital admission and subsequently enrolled in a nutritional intervention program until 12 years of age. The malnutrition episode and subsequent physical and mental development were documented in detail. There was no evidence of continuing malnutrition after the early episode; by the end of puberty, all children showed complete catch-up in physical growth.13 At ages 11–17 years, the previously malnourished group had prominent cognitive deficits, including lower IQ,10 poorer performance on a national high school admission examination that was mediated by attention deficits and cognitive impairment at earlier ages14 and impaired fine motor skills,15 even after adjusting for the effects of social contextual variables. We have recently reported an increase in affective problems and depressive symptoms in the adolescent age group.16,17
The current report describes self-reported conduct problems in these previously malnourished Barbadian youth and the comparison group in adolescence. Because parents may not be privy to an adolescent’s behavior outside the home, self-reports may be more accurate than parent reports.18–20 The study addresses two primary questions: (1) Is early malnutrition associated with a higher rate of self-reported conduct problems in adolescence? (2) To what extent do variations in household social conditions and IQ mediate the association between infant malnutrition and adolescent conduct problems? We also explored whether such conduct problems are predicted by disruptive behavior during childhood as observed by teachers.
Methods
Site
Barbados is a Caribbean country whose current population is approximately 260,000, 92% of African descent. Barbados is currently ranked 47 on the Human Development Index.21 In 1970, the infant mortality rate was 46 per 1000 live births; today it stands at 7.8. Whereas malnutrition was of concern when this study was initiated in the late 1960s, it is now virtually eliminated due to the improved economy and island-wide nutrition education.22,23
Design and sampling
All children on the island with identified malnutrition were enrolled in the National Nutrition Centre where they were followed to 12 years of age. After admission to the Centre, children were seen every 6 weeks and their growth, health, and development were routinely documented. Because referral to the Centre was obligatory, ascertainment was free of selection biases.
Children in the Barbados Nutrition Study suffered from either marasmus or kwashiorkor in the first year of life; both conditions are part of the spectrum of protein–energy malnutrition disorders, and each condition may also include other forms of nutrient deficiencies.12 In 1977, families of all school-aged children enrolled in the National Nutrition Centre who had been hospitalized in their first year of life (between 1967 and 1972) with a diagnosis of Grade II or III24 marasmus, associated with a deficiency of protein and calories, were invited to participate.25 This group (n = 129) included nearly all children on the island who had experienced one episode of marasmus. Three healthy children, matched by sex, age (within 3 months), and handedness, were identified from the same neighborhoods and classrooms as the index children; one of the three candidates (n = 129) was selected, based on availability of birth data, pre-school height and weight, and immunization data. Other inclusion criteria for participants were normal birth weight, absence of pre- or post-natal complication, and no known encephalopathic events in childhood. Both groups were followed longitudinally.
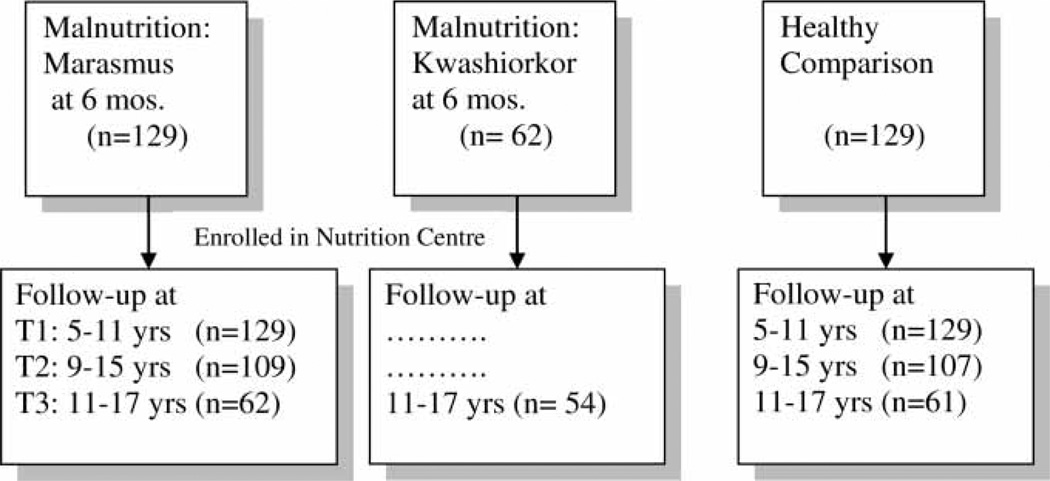
Fig. 1 shows the study design. The malnutrition episode was well documented at baseline in the first year of life at T0 (1967–1972), and physical, mental, and behavioral development was followed up at T1 (1977, 5–11 years), T2 (1982, 9–15 years) and T3 (1984, 11–17 years).
Figure 1.
Research design: Barbados Nutrition Study. Seven participants (six marasmus and one healthy comparison) did not complete the BCBS-SR, resulting in a total of 116 participants in the longitudinal study of T1, T2 and T3 children (marasmus and comparison groups only).
At T3, 54 children who had been hospitalized in the first year of life (also between 1967 and 1972) with kwashiorkor,25 a disorder previously thought to result from protein deficiency, were also recruited into the larger study. At that time, 62 index and 61 control children were selected to participate so as to achieve the best matches to the kwashiorkor group, based on age, sex, and handedness. The current study is based on the marasmus and comparison children who were tested at T3, for whom data at all 3 time points are available; individuals who had kwashiorkor are not included, nor are children who were not selected for the T3 measurement. Because seven participants (six marasmus and one comparison) did not complete the behavior questionnaire, the final N included 56 adolescents from the marasmus group and 60 from the comparison group. The demographic characteristics have been reported elsewhere.16
Informed consent was provided by all families under Protocol E1962, approved by the Boston University Medical Center Institutional Review Board and the Ethics Committee, Ministry of Health, Barbados. Current oversight is provided by the Judge Baker Children’s Center Human Research Review Committee (Assurance No. FWA 00001811). This study was conducted according to the guidelines laid down in the Declaration of Helsinki. Written and/or verbal informed consent was obtained from all participants. When verbal consent was obtained, it was witnessed and formally recorded.
Measures
Wechsler Intelligence Scale for Children26 (T1)
This standard IQ test was administered with minor alteration of items to include familiar local exemplars.
Teacher Behavior Questionnaire (T1)
This 30-item questionnaire, which has been used by us in earlier studies of the Barbados cohort,27 was completed by teachers who were blind to the nutritional history of the child. Four items (scores ranging from 1 to 4 or 1 to 6) with high face validity were identified as indicators of conduct problems for purposes of exploratory analysis.
Household Standard of Living (T1)
The socioeconomic context was measured using the 50-item Barbados Ecology Questionnaire (BEQ), which was based on a scale used in Jamaica28 and modified for use in Barbados.29,30 The questionnaire assessed psychosocial, socioeconomic and home environmental conditions that were most relevant to the social context at the time and was administered at each time point to primary caretakers and validated by home visits. Factor analysis was based on the three measurement points combined to permit longitudinal comparison. This analysis identified a first principal component that appeared to represent the household standard of living (HSOL).31 Scores had a zero mean and unit variance.
Child Behavior Questionnaire (T3)
This 76-item self-report questionnaire was administered at T3 and developed specifically for Barbados to describe behavioral dimensions but not to diagnose specific psychiatric disorders.32 It was administered by a Barbadian child psychologist who was blind to the child’s nutritional history. Most items were rated on a 4-point scale from Never to Always. The items were reduced by exploratory principal components factor–extraction, described in detail elsewhere.33 Table 1 lists the 13 items that contributed most strongly (factor loading ≥0.40) to the first unrotated principal component, which appears to represent conduct problems. It accounted for 9% of total variance, with an eigen-value of 6.37, and acceptable reliability (Cronbach alpha = 0.71). This Conduct Scale was standardized to have zero mean and unit variance.
Table 1.
Items from the first unrotated factor (and factor loadings) derived from a principal component analysis of the self-reported behavior scale
| 0.61 | Do you ever cheat at games with other children? |
| 0.60 | Do you ever tell lies? |
| 0.59 | Do you talk back to people? |
| 0.55 | Are you ever mean or cruel to other children? |
| 0.52 | Do you ever boss other children around? |
| 0.48 | Have you ever had a nail-biting problem? |
| 0.47 | Do you misbehave after being warned? |
| 0.44 | Do you ever boast or brag? |
| 0.43 | How often do you fight with other children (outside the family)? |
| −0.41 | Have you been well-behaved since early childhood? |
| −0.42 | Are you obedient and do what you are told? |
| −0.43 | How cooperative are you with your parents? |
| −0.43 | How well do you get along with others? |
Note: Although only items with factor loadings >0.40 are reported, factor analyses were calculated using all items in the questionnaire.
Statistical methods
All analyses were conducted using SAS, version 9.2.33 The Pearson correlations were computed between the malnutrition variable and the other variables (IQ and HSOL) in the model. A series of multiple regression analyses were then implemented to evaluate the potential mediating effects of the cognitive variables in the relationship of malnutrition to adolescent conduct problems. The first set of analyses evaluated malnutrition status as a predictor of conduct problems (T3). Next, malnutrition status as a predictor of conduct problems was evaluated, adjusting for household environment or IQ, the primary hypothesized mediators, both at T1. The final set evaluated malnutrition as a predictor of conduct problems, adjusting for both household environment and IQ simultaneously. Preliminary analyses indicated that age and sex were not predictors in these models, and so they were dropped. The mediation effects were evaluated by determining the extent to which the direct effect (of malnutrition) was diminished when the hypothesized mediating variables were added to the model. The Pearson correlations were used to compute the association between classroom behaviors (teacher-reported) at ages 5–11 and adolescent self-reported conduct problems.
Results
The individuals who participated at all three times did not differ from those who participated at T1 and/or T2 only in their age, sex, or HSOL, arguing against selection bias. As shown in Table 2, previously malnourished youth (with histories of marasmus) self-reported significantly more conduct problems than did the comparison youth. (Similar findings were present for the youth with histories of kwashiorkor, but these data are not presented.) Although the mean age and sex of the previously malnourished participants and comparison youth were similar, there were nonetheless significant group differences with respect to childhood IQ and HSOL at 5–11 years of age of living, consistent with earlier reports from this series.11,29 These differences led us to consider possible mediating roles for IQ and the HSOL.
Table 2.
Descriptive statistics (means, standard deviations) showing differences between previously malnourished and comparison youth (N = 116)
| Malnourished (n = 56) |
Comparison (n = 60) |
P | |
|---|---|---|---|
| Age in years, Mean ± SD | 15.01 ± 1.49 | 15.04 ± 1.58 | NS |
| Males, N (%) | 31 (55.36%) | 35 (58.33%) | NS |
| IQ: T1 | 92.54 ± 13.86 | 104.92 ± 10.54 | <0.001 |
| Standard of living: T1 | −0.90 ± 0.89 | −0.25 ± 0.77 | <0.001 |
| Conduct problems: T3 | 0.29 ± 1.18 | −0.27 ± 0.84 | <0.01 |
IQ and standard of living as mediators of relationship between adolescent conduct problems
These analyses were undertaken to determine whether HSOL29 or cognitive impairment arising from malnutrition11 mediate the increased prevalence of conduct problems in previously malnourished adolescents. The history of infant malnutrition was correlated with HSOL at T1 (r= −0.37, P < 0.001), IQ at T1 (r = −0.45, P < 0.001), and conduct problems in adolescence at T3 (r = 0.27, P < 0.01). Moreover, both the HSOL (r = −0.27, P < 0.01) and IQ (r = −0.29, P < 0.01) were correlated with adolescent conduct problems. This pattern of correlations meets the preliminary criteria for mediation.
Table 3 shows the relevant regression models. As may be seen in the first row of the table, in unadjusted analyses, malnutrition was a significant predictor of adolescent conduct (P < 0.01), with differences between the two groups of approximately 0.54 standard deviation units on the conduct scale (The coefficient for malnutrition in Table 3 is standardized and must be multiplied by approximately 2 to signify the effect of malnutrition). With both childhood IQ and HSOL entered into the model, the malnutrition effect was attenuated (approximately 0.26) and no longer significant; specifically, the magnitude of the effect of malnutrition decreased by approximately 50% (see the last row of the table). Additional analyses reported in Table 3 indicate that the attenuation is due to the combined effects of both factors (see second and third rows of table).
Table 3.
Regression analyses showing predictive relationships between infant malnutrition and adolescent conduct problems (at 5–11 years), adjusting for HSOL and IQ
| Dependent variable | Predictors | Standardized β coefficients | SE | R2 | F |
|---|---|---|---|---|---|
| Malnutrition | 0.27** | 0.09 | 0.07 | 8.81** | |
| Malnutrition | 0.19* | 0.10 | |||
| 0.11 | 6.74** | ||||
| Standard of living (T1) | −0.20* | 0.10 | |||
| Malnutrition | 0.17† | 0.10 | |||
| Conduct problems (T3) | 0.11 | 6.78** | |||
| Childhood IQ (T1) | −0.21* | 0.10 | |||
| Malnutrition | 0.13 | 0.10 | |||
| Standard of living (T1) | −0.16† | 0.10 | 0.13 | 5.53** | |
| Childhood IQ (T1) | −0.17† | 0.10 |
P< 0.05;
P<0.01;
0.1 > P>0.05.
Classroom behaviors at 5–11 years predict youth conduct problems
Table 4 shows teacher ratings at 5–11 years of age for the two malnutrition groups on relevant questionnaire items, as well as correlations of those ratings with adolescent self ratings. All four items showed a higher level prevalence of aberrant behavior in the previously malnourished children as compared with the comparison group. Teacher reports of problem behavior significantly predicted self-reports of conduct problems six years later at 11–17 years of age, confirming the continuity of disruptive behaviors over time and providing validation for the self-reports.
Table 4.
Teacher-reported classroom behavior at 5–11 years (means, standard deviation) and their correlation (r) with self-reported conduct problems at 11–17 years (N = 116)
| Teacher-reported behaviors | Index | Comparison | F value | R |
|---|---|---|---|---|
| Does he/she have any behavior or conduct problems?† | 1.3(0.5) | 1.5(0.5) | 4.65* | 0.31*** |
| How well does child pay attention to you in class?‡ | 4.2(0.9) | 3.6(1.0) | 11.3** | −0.27** |
| How obedient is he/she? Does the child do what he is told?‡ | 4.8(1.0) | 4.3(1.0) | 5.92* | −0.23* |
| How cooperative is he/she with you?‡ | 4.7(0.8) | 4.2(1.0) | 11.68*** | −0.32*** |
P < 0.05;
P< 0.01;
P< .001.
Higher score connotes fewer problems.
Higher scores connote more problems.
Discussion
The present study confirms that malnutrition in the first year of life is associated with an increased prevalence of conduct problems in adolescence, as indicated by the self-report from the adolescents themselves. These same behaviors were also associated with the HSOL and childhood IQ measured at 5–11 years of age, and these partially mediated the malnutrition effects.
An elevation in conduct problems has been observed consistently in these youth, even after adjusting for the potential contribution of their home environments. When they were of school age (5–11 years), their teachers reported more conduct problems than in the previously malnourished group.26 Their early classroom behavior was significantly associated with the increased prevalence of self-reported conduct problems at 11–17 years (Table 4). Increased disruptive behavior and conduct problems were also reported by teachers and parents at 9–15 years of age.32,34 It is well-recognized, however, that the youth self-reports can differ substantially from the adult observer reports, especially in adolescence.18–20 Many of the reported behaviors presumably occur with peers, when the adolescents are not in the presence of adults. However, the current self-report ratings suggest that conduct problems persisted into adolescence in these Barbadian youth and are consistent with the earlier observations by their teachers and parents.
Our findings extend the earlier studies of the effects of childhood malnutrition.1,2,4 The Mauritius study documented parent reports of aggressive behavior in the malnourished children at age 11 and parent and teacher reports of conduct disorder at age 17.1 An enrichment program administered between 3 and 5 years reduced the prevalence of conduct disorder at 17 years of age in malnourished children relative to controls.35 While malnutrition was documented at 3 years of age, the Mauritius children most likely suffered from chronic malnutrition, which could have contributed to these findings. In contrast, the Jamaica study reported increased aggression (oppositional behavior) tendencies from parent reports in the stunted group,2,4 regardless of an intervention at 2 years of age. There was no increase in antisocial behavior at 17 years of age by self-report. At adolescent ages, the treated and untreated stunted groups were smaller than their non-stunted controls, further suggesting that this cohort also suffered from chronic undernutrition.
The participants in the Barbados Nutrition Study, in contrast to both of these earlier studies, had normal birth weights, and malnutrition was confined to the first year of life. Enrolled in the Barbados Nutrition Centre program till 12 years of age, the Barbadian youth recovered fully from malnutrition and reached their full growth potential by the end of puberty.13 The Barbados sample, thus, confirms that conduct problems associated with early childhood malnutrition can persist despite good health and recovery of physical growth by puberty. However, the persistence of conduct problems in these youth raises concerns about their long-term outcomes that are currently being evaluated in the 40-year follow-up of this sample. For example, survivors of the Dutch famine who were exposed to intrauterine malnutrition had elevated antisocial behavior in adulthood.36
Mechanisms by which early malnutrition leads to later aggressive behavior remain speculative.8 Siever37 has implicated failure of the ‘top-down’ prefrontal control systems and hyper-reactivity of the amygdala and other limbic regions, both impacted by early childhood malnutrition.9 Cappadocia et al.38 further noted the importance of the environment, which may also influence aggressive behavior in children. Other perinatal risk factors have also been shown to increase the prevalence of antisocial behavior in adolescents.3 A developmental pathway leading from the early biological insult to increased neurological damage, impaired academic performance and an increase in the prevalence of antisocial behaviors, may explain this outcome. Animal models of early malnutrition have similarly confirmed the perturbation of neurobiological systems linked to aggression, including alterations in the seroteonergic afferent system9,39,40 and altered stress response.41 However, the extent to which these biological changes bear a causal relationship to aggression, or can be validly translated to the human setting remains to be established.
This study had several limitations. First, because the study at T3 included only children with histories of kwashiorkor and demographically-matched children from the marasmus and healthy comparison groups, about half of the original children from the latter groups were not tested at this time point. Comparison of those individuals who participated at T3 with those who did not, however, revealed no differences on key demographic variables, arguing against selection bias.
Second, the data reported here were collected in the 1970s and early 1980s, when the well-developed behavioral screening tools for children and adolescents in common use today were not available or had not been sufficiently tested in developing countries. Thus, the continuity of disruptive behavior over time in this sample, based on teacher, parent, and self-reports, that used an instrument essentially developed for this study, is reassuring and validates the self-report instrument. Because the Barbados Nutrition Study is currently collecting comprehensive data on these adolescents in mid-life, these findings, even though based on archival data with psychometric limitations, remain significant. They provide a platform for evaluating the lifetime implications of an early episode of malnutrition and its sequelae for adult outcomes.
In sum, the current study reinforces prior findings that an early episode of moderate–severe malnutrition, even when limited to the first year of life, can increase risk for conduct problems in adolescence. Given the continuing risk for infant malnutrition in many parts of the world, these findings have important public health implications for the mental health of children and adolescents. Moreover, since conduct problems in adolescence can forecast antisocial behavior in adulthood,5–7 the long-term social burden of early malnutrition may be considerable.31 The adult follow-up component of the Barbados Nutrition Study will hopefully provide evidence pertaining to this latter concern.
Acknowledgements
This research was conducted with the cooperation of the Ministries of Health and Education, Barbados. The authors acknowledge the late Sir Frank C. Ramsey, our long time collaborator and Director of the Barbados Nutrition Centre, who followed these children for most of their lives and whose efforts resulted in the elimination of malnutrition from the island of Barbados. We would also like to express our gratitude to the dedicated parents and children who have participated in the study over their lifetimes. The research was supported by NIH/R01MH65877 and NIH/R01HD60986.
References
- 1.Liu J, Raine A, Venables PH, Mednick SA. Malnutrition at age 3 years and aggressive behavior problems at ages 8, 11, and 17 years. Am J Psychiatry. 2004;161:2005–2013. doi: 10.1176/appi.ajp.161.11.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walker SP, Chang SM, Powell CA, Simonoff E, Grantham-McGregor SM. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychological stimulation. J Nutr. 2007;137:2464–2469. doi: 10.1093/jn/137.11.2464. [DOI] [PubMed] [Google Scholar]
- 3.Chang SM, Walker SP, Grantham-McGregor S, Powell CA. Early childhood stunting and later behaviour and school achievement. J Child Psychol Psychiatry. 2002;43:775–783. doi: 10.1111/1469-7610.00088. [DOI] [PubMed] [Google Scholar]
- 4.Walker SP, Chang SM, Powell CA, Simonoff E, Grantham-McGregor SM. Effects of psychosocial stimulation and dietary supplementation in early childhood on psychosocial functioning in late adolescence: follow-up of randomized controlled trial. BMJ. 2006;333:472. doi: 10.1136/bmj.38897.555208.2F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simonoff E, Elander J, Holmshaw J, Pickles A, Murray R, Rutter M. Predictors of antisocial personality: continuities from childhood to adult life. Br J Psychiatry. 2004;184:118–127. doi: 10.1192/bjp.184.2.118. [DOI] [PubMed] [Google Scholar]
- 6.Sourander A, Jensen P, Davies M. Who is at greatest risk of adverse long-term outcomes? The Finnish from a boy to a man study. J Am Acad Child Adolesc Psychiatry. 2007;46:1148–1161. doi: 10.1097/chi.0b013e31809861e9. [DOI] [PubMed] [Google Scholar]
- 7.Colman I, Murray J, Abbott RA. Outcomes of conduct problems in adolescence: 40 year follow-up of national cohort. BMJ. 2009;338:a2981. doi: 10.1136/bmj.a2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu J, Raine A. The effect of childhood malnutrition on externalizing behavior. Curr Opin Pediatr. 2006;18:565–570. doi: 10.1097/01.mop.0000245360.13949.91. [DOI] [PubMed] [Google Scholar]
- 9.Galler JR, Shumsky JS, Morgane PJ. Malnutrition and brain development. In: Walker WA, Watkins JB, editors. Nutrition in pediatrics: basic science and clinical application. 2nd edn. Neuilly-sur-Seine, France: J.B. Decker Europe, Inc; 1996. pp. 196–212. [Google Scholar]
- 10.Galler JR, Ramsey FC, Forde V, Salt P, Archer E. Long-term effects of early kwashiorkor compared with marasmus. II. Intellectual performance. J Pediatr Gastroenterol Nutr. 1987;6(6):847–854. doi: 10.1097/00005176-198711000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Galler JR, Ramsey F, Solimano G, Lowell WE, Mason E. The influence of early malnutrition on subsequent behavioral development. I. Degree of impairment in intellectual performance. J Am Acad Child Psychiatry. 1983;22(1):8–15. doi: 10.1097/00004583-198301000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Waterlow JC. Classification and definition of protein calorie malnutrition. BMJ. 1982;3:566–569. doi: 10.1136/bmj.3.5826.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galler JR, Ramsey F, Salt P, Archer E. Long term effects of early kwashiorkor compared with marasmus I) Physical growth and sexual maturation. J Pediatr Gastroenterol Nutr. 1987;6:841–846. doi: 10.1097/00005176-198711000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Galler JR, Ramsey F, Morley DS, Archer E, Salt P. The longterm effects of early kwashiorkor compared with marasmus. IV. Performance on the national high school entrance examination. Pediatr Res. 1990;28:235–239. doi: 10.1203/00006450-199009000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Galler JR, Ramsey FC, Salt P, Archer E. Long-term effects of early kwashiorkor compared with marasmus. III. Fine motor skills. J Pediatr Gastroenterol Nutr. 1987;6(6):855–859. doi: 10.1097/00005176-198711000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Galler JR, Bryce CP, Waber DP, Hock RS, Exner NM, Eaglesfield GD, et al. Childhood malnutrition predicts depressive symptoms at ages 11–17. J Child Psychol Psychiatry. 2010;51(7):789–798. doi: 10.1111/j.1469-7610.2010.02208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waber DP, Eaglesfield GD, Fitzmaurice GM, Bryce CP, Galler JR. Developmental pathways from early childhood malnutrition to adolescent depressive symptoms in Barbadian youth. J Dev Behav Pediatr. 2011;32(3):225–232. doi: 10.1097/DBP.0b013e31820b7707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutter M, Tizard J, Whitmore K. Education, health and behavior. London, England: Longmans; 1970. [Google Scholar]
- 19.Achenbach TM, Verhulst FC, Baron GD, Akkerhuis GW. Epidemiological comparisons of American and Dutch children: I. Behavioral/emotional problems and competencies reported by parents for ages 4 to 16. J Am Acad Child Adolesc Psychiatry. 1987a;26:317–325. doi: 10.1097/00004583-198705000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Achenbach TM, Verhulst FC, Edelbrock C, Baron GD, Akkerhuis GW. Epidemiological comparisons of American and Dutch children. II. Behavioral/emotional problems reported by teachers for ages 6 to 11. J Am Acad Child Adolesc Psychiatry. 1987b;26:326–332. doi: 10.1097/00004583-198705000-00007. [DOI] [PubMed] [Google Scholar]
- 21.United Nations Development Programme. UNDP Annual Report 2011. New York (NY): Office of Communications, United Nations Development Programme; 2011. [Google Scholar]
- 22.Ramsey F, Demas N, Trotter P. The National Health and Nutrition Survey of Barbados, 1981. Washington, DC: Pan American Health Organization; 1984. [Google Scholar]
- 23.Ramsey FC. Dr. Frank Ramsey: an autobiography. Barbados, West Indies: Dynamic Colour Inc; 2006. [Google Scholar]
- 24.Gomez F, Galvan RG, Cravioto J, Frenk S. Malnutrition in infancy and childhood, with special reference to kwashiorkor. Adv. Pediatr. 1955;7:131–169. [PubMed] [Google Scholar]
- 25.Gomez F, Galvan RR, Frenk S, Cravioto Munoz J, Chavez R, Vazquez J. Mortality in second and third degree malnutrition. 1956. Bull World Health Organ. 2000;78(10):1275–1280. [PMC free article] [PubMed] [Google Scholar]
- 26.Wechsler D. Wechsler intelligence scale for children. 4th edn. San Antonio, TX: Harcourt Assessment; 2003. (WISC-IV) [Google Scholar]
- 27.Galler JR, Ramsey F, Solimano G, Lowell WE. The influence of early malnutrition on subsequent behavioral development: II. Classroom behavior. J Am Acad Child Adolesc Psychiatry. 1983;22:16–22. doi: 10.1097/00004583-198301000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Richardson SA. The background histories of schoolchildren severely malnourished in infancy. Adv Pediatr. 1974;21:167–195. [PubMed] [Google Scholar]
- 29.Galler JR, Ramsey F. The influence of early malnutrition on subsequent development. VI) The role of the microenvironment of the household. Nutr Behav. 1985;2:161–173. [Google Scholar]
- 30.Galler JR. The interaction of nutrition and environment in behavioral development. In: Dobbing J, editor. Early nutrition and later achievement. New York: Academic Press; 1987. pp. 175–207. [Google Scholar]
- 31.Galler JR, Bryce CP, Waber DP, Zichlin ML, Fitzmaurice GM, Eaglesfield GD. Socioeconomic outcomes in adults malnourished in the first year of life: a 40-year study. Pediatrics. 2012 Jul;130(1):e1–e7. doi: 10.1542/peds.2012-0073. doi: 10.1542/peds.2012-0073. Epub 2012 Jun 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Galler JR, Ramsey F. A follow-up study of the influence of early malnutrition on development: Behavior at home and at school. J Am Acad Child Adolesc Psychiatry. 1989;28:254–261. doi: 10.1097/00004583-198903000-00018. [DOI] [PubMed] [Google Scholar]
- 33.SAS Institute, Inc. SAS/STAT user’s guide, version 9.2. 9th edn. Cary, NC: SAS Institute; 2008. [Google Scholar]
- 34.Galler JR, Ramsey F, Solimano G. Influence of early malnutrition on subsequent behavioral development. V) Child’s behavior at home. J Am Acad Child Adolesc Psychiatry. 1985;24:58–64. doi: 10.1016/s0002-7138(09)60410-6. [DOI] [PubMed] [Google Scholar]
- 35.Raine A, Mellingen K, Liu J, Venables P, Mednick SA. Effects of environmental enrichment at ages 3–5 years on schizotypal personality and antisocial behavior at ages 17 and 23 years. Am J Psychiatry. 2003;160(9):1627–1635. doi: 10.1176/appi.ajp.160.9.1627. [DOI] [PubMed] [Google Scholar]
- 36.Neugebauer R, Hoek HW, Susser E. Prenatal exposure to wartime famine and development of antisocial personality disorder in early adulthood. JAMA. 1999;282(5):455–462. doi: 10.1001/jama.282.5.455. [DOI] [PubMed] [Google Scholar]
- 37.Siever LJ. Neurobiology of aggression and violence. Am J Psychiatry. 2008;165:429–442. doi: 10.1176/appi.ajp.2008.07111774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cappadocia MC, Desrocher M, Pepler D, Schroeder JH. Contextualizing the neurobiology of conduct disorder in an emotion dysregulation framework. Clin Psychol Rev. 2009;29:506–518. doi: 10.1016/j.cpr.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 39.Blatt GJ, Chen JC, Rosene DL, Volicer L, Galler JR. Prenatal protein malnutrition effects on the serotonergic system in the hippocampal formation: an immunocytochemical, ligand bonding, and neurochemical study. Brain Res Bull. 1994;34:507–518. doi: 10.1016/0361-9230(94)90025-6. [DOI] [PubMed] [Google Scholar]
- 40.Medeiros JM, Silva CM, Sougey EB, Costa JA, Castro CM, Castro RM. Action of selective serotonin reuptake inhibitor on aggressive behavior in adult rats submitted to the neonatal malnutrition. Arq Neuropsiquiatr. 2001;59(3-A):499–503. doi: 10.1590/s0004-282x2001000400004. [DOI] [PubMed] [Google Scholar]
- 41.Rosene DL, Lister JP, Schwagerl AL, Tonkiss J, McCormick CM, Galler JR. Prenatal protein malnutrition in rats alters the c-Fos response of neurons in the anterior cingulate and medial prefrontal region to behavioral stress. Nutr Neurosci. 2004;7:281–289. doi: 10.1080/10284150400015573. [DOI] [PubMed] [Google Scholar]