Abstract
Background
Specific ways community health worker (CHW) programs affect participants’ health care behaviors and interactions with their health care providers, as well as mechanisms by which CHW programs influence these outcomes, are poorly understood. Through a qualitative descriptive study of participants in a successful CHW diabetes self-management program, we sought to answer: 1) What gaps in diabetes care, with a focus on patient-doctor interactions, do participants identify? And 2) How does the program influence participants’ diabetes care and interactions with health care providers, and what gaps, if any, does it address?
Methods
From 2005-2007, we conducted semi-structured interviews with 40 African American and Latino adults with diabetes who had completed or were active in a CHW-led diabetes self-management program developed and implemented using community-based participatory research (CBPR) principles in Detroit. Interviews were audiotaped, transcribed, and coded through a consensual and iterative process.
Results
Participants reported that before participating in the intervention they had received inadequate information from health care providers for effective diabetes self-management, had had low expectations for help from their providers, and had not felt comfortable asking questions or making requests of their health care providers. Key ways participants reported that the program improved their ability to manage their diabetes were by providing 1) clear and detailed information on diabetes and diabetes care that they had not known before REACH; 2) education and training on specific strategies to meet diabetes care goals; 3) sustained and non-judgmental assistance to increase their motivation and confidence to improve their diabetes self-management; and 4) social and peer support that enabled them to better manage their diabetes. The knowledge and confidence gained through the CHW intervention increased participants’ assertiveness in asking questions to and requesting necessary tests and results from their providers.
Conclusions
Our interview findings suggest ways that CHW programs that provide both one-on-one support and group self-management training sessions may be effective in promoting more effective diabetes care and patient-doctor relationships among Latino and African American adults with diabetes. Through these mechanisms, such interventions may help to mitigate racial and ethnic disparities in diabetes care and outcomes.
Keywords: Patient-Physician Communication, Chronic Disease, Diabetes, Patient Self-Management, Community Health Worker Intervention, Community-Based Participatory Research
BACKGROUND
African Americans and Latinos experience a 50-100% higher burden of illness and mortality from diabetes than non-Latino white Americans.[1-5] Nationwide, African American and Latino adults with diabetes have worse glycemic and blood pressure control than white Americans and report experiencing more barriers to diabetes self-management than non-Latino white adults. [6-9]
To address such disparities, Detroit is one of 40 US cities that received funding from the Centers for Disease Control and Prevention (CDC) to implement multi-faceted, community-based interventions as part of the “Racial and Ethnic Approaches to Community Health 2010” (REACH) Initiative. In the REACH Detroit Partnership, community, health system, and academic partners used a social-ecological framework and community-based participatory research (CBPR) methods to target sources of health disparities at multiple levels. After an extensive process of community planning and input, [10-12] we developed and conducted interventions to increase diabetes awareness, community resources and social support for healthy lifestyles, and to strengthen the capacity of health care providers and African American and Latino adults with diabetes in eastside and southwest Detroit to manage and improve diabetes outcomes (see Figure 1).
Figure 1.
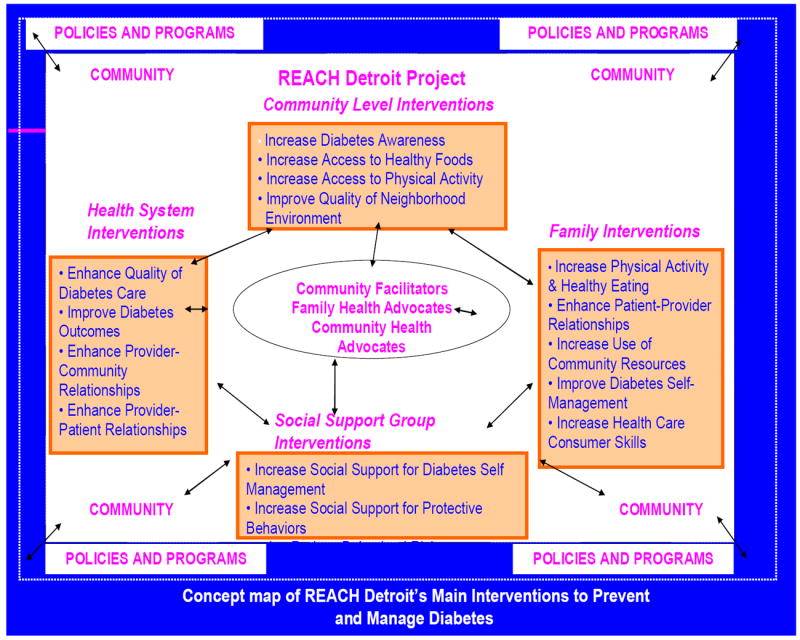
Social-ecological Framework for Targeting Sources of Disparities at Multiple Levels
Interventions using community health workers (CHW) have demonstrated promise in improving health behaviors and outcomes, particularly for racial and ethnic minority communities and those who have traditionally lacked access to adequate health care.[13,14] CHW interventions enlist and train community members who work as bridges between their ethnic, cultural, and/or geographic communities and health care providers to promote health. [15,16] Norris and colleagues in a 2006 systematic review of CHW programs with adults with diabetes found that knowledge about diabetes and self-care increased significantly among adults receiving assistance from CHWs in 5 of 7 studies. CHW programs led to improved diet, physical activity levels, and other self-care behaviors. In two studies, monitoring of glycemic control by providers was improved as were rates of retinopathy screening.[16] While initial results about the effectiveness of CHW programs are encouraging, to date only a few studies have explored the mechanisms by which CHW interventions lead to changes in participants’ diabetes care, [17,18] and little is known about whether—and if so how-- these interventions influence participants’ relations with their formal health care providers.
One hypothesized mechanism by which such programs improve diabetes care processes and outcomes is by helping empower patients to be more knowledgeable about their diabetes care and assertive in requesting information and recommendations from their health care providers. [1, 19] National surveys have found higher rates of reported difficulties in communication with health care providers for African- American, Latino, and Asian patients than for non-Latino white patients.[20] Physicians often provide less information to minority than to white patients, and black patients rate their physician visits as less participatory and satisfactory than white patients.[21-24] Black and Latino patients also tend to be less assertive in their encounters with providers than white patients.[1] For example, they are less likely to request necessary screening tests, to ask their providers about treatment recommendations, to raise concerns about their treatments, and to freely question their doctors. [1, 25-26] As shown in Figure 2, such disparities in patient-provider communication may contribute to inequities in information exchange, poorer medical decisions, and less patient satisfaction and commitment, all of which may result in worse health outcomes.[27-32]
Figure 2.
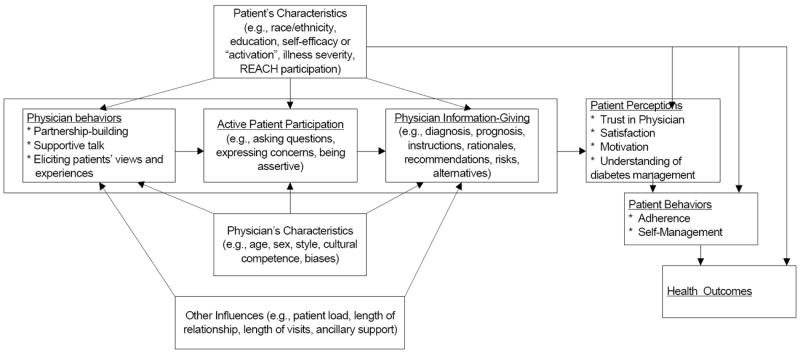
Conceptual Model of Key Domains of Patient-Doctor Interactions for Health Outcomes
Since 2000, the REACH Detroit Partnership has used CBPR principles to implement and evaluate a CHW intervention. As part of this intervention, trained CHWs, known as Family Health Advocates (FHA), are assigned to adults with diabetes to promote healthy lifestyle and diabetes self-management behaviors and to help participants navigate the health care system and be more activated in office visits with their providers, with a focus on the patient behaviors listed in Figure 2. The FHA intervention builds on research showing that activated patients experience greater self-efficacy, physical and mental functioning, and improved health behaviors.[33-36] Ten FHAs from the target communities were hired and, after intensive training, conducted a culturally tailored diabetes self-management and lifestyle education curriculum: The English-language “Journey to Health” for African American participants and English and Spanish versions of “El Camino a la Salud” for Latino participants. The curriculum was based on collaborative ‘empowerment’ models that actively engage patients in setting their own self-care goals, developing problem-solving skills and self-efficacy, and negotiating more effectively with health care providers to ensure diabetes care needs are met. [37-39] The 11 2-hour group sessions were designed to help participants gain knowledge and skills related to healthy eating, physical activity, stress reduction, diabetes self-management, and effective patient-doctor communication. Sessions were held every two to four weeks at community locations. The development, implementation, and evaluation of these curricula are described in depth elsewhere. [12, 40] FHAs also worked individually with participants to help them be aware of their target HbA1C, blood pressure, and lipid levels, when they were due for necessary diabetes screening tests, and to set and follow through on specific behavioral change goals. FHAs encouraged clients to discuss the goals they set with their providers, ask questions about their treatment plans, and alert their providers about screening tests that were due.
Two cohorts of Family Health Advocate Intervention participants were recruited from inner-city Detroit health systems. Participants were African Americans and Latinos from eastside and southwest Detroit, age 18 or older, with physician-diagnosed type 2 diabetes. Recruitment methods, participant characteristics and intervention outcomes for the first cohort have been described elsewhere.[12] Briefly, participants in both cohorts showed statistically and clinically significant improvements compared to a control group in several measures of healthy behaviors, diabetes-related emotional status and HbA1c levels, following 6 months of participation in the intervention and after 12 months.[41]
In response to the quantitative improvements in diabetes outcomes achieved through the FHA intervention, the REACH Detroit Partnership Steering Committee requested that we conduct a qualitative descriptive study to explore possible reasons for the influence of the FHA Intervention on participant outcomes. The aim was to use the information gathered to inform continued refinement of the program and other efforts to reduce racial/ethnic disparities in diabetes outcomes. In consultation with community members and FHAs, we identified two key study questions: 1) What gaps in diabetes care, with a focus on patient-doctor interactions, do REACH Detroit participants identify? And 2) How does a community health worker (CHW) diabetes self-management program influence participants’ diabetes care and interactions with health care providers, and what gaps, if any does it address?
METHODS
Sampling and Data Collection
From 2005-2007, we conducted semi-structured interviews with 20 African American and 20 Latino adults with diabetes who had completed or were currently active in the FHA intervention. We used purposeful sampling to identify participants, stratifying patients by race/ethnicity (half African American, half Latino). We continued interviewing participants until we achieved informational redundancy. With input from FHAs and community members, we developed an interview guide to elicit descriptions of participants’ self-management activities and needs, their interactions with their FHAs and with their health care providers before, during, and after their participation in the Detroit REACH program, and their experiences with and evaluation of the REACH FHA intervention (often called “REACH” by participants). Interviews lasted from 60-90 minutes, and were conducted in participants’ homes. Four trained graduate-level student research assistants from similar ethnic backgrounds to participants conducted all interviews; interviews with Spanish-speaking participants were conducted in Spanish. Participants received $30 to compensate for their time. Written informed consent was obtained from each participant before beginning the interview. The study was approved by the Institutional Review Boards of the University of Michigan School of Medicine and Henry Ford Health System. The key findings reported in this paper have been shared with REACH participants, FHAs, REACH Detroit Partnership Steering Committee members, and community members through several community fora.
Data Analysis
Interviews were audiotaped and transcribed verbatim. All investigators, including the interviewers, discussed each interview in regular team meetings, and developed themes iteratively and through consensus. Interviews were discussed both before the transcript was produced and after team members had read the transcript. Near the completion of the interviews, the team developed a codebook based on these themes (e.g., need for self-management strategies, help received from REACH), again using a consensus and iterative process to ensure that codes were clearly defined and could be applied consistently to the data. Twenty-five of the 40 transcripts were coded by two investigators, who reconciled discrepancies though consensus.[42] The remaining 15 transcripts were coded by one coder. We used QSR NVivo 2, qualitative data analysis software, to sort text segments so that all segments coded with the same code appeared in one report. Each coding report was then summarized by a team member; summaries included key themes and text evidence for those themes.
We ensured the validity of our findings in several ways: verifying a subset of transcripts by comparing them to the audio-recording; regular debriefing of interviewers by the team; rigorous codebook development and application of codes largely through a consensus process; and ongoing participation of team members with diverse professional, cultural, and racial/ethnic backgrounds.
RESULTS
Sample Description
From a list of 151 eligible participants in the FHA Intervention, we tried to contact 91 participants. Of the 75 we spoke with, 52 agreed to participate; 12 completed interviews were unusable due to audio-recording errors. We completed and audio-recorded interviews of 40 participants, 18 of whom had completed the program and 22 who were participating in the second cohort. Twenty participants were Latino, and 20 were African American, with 32 women and 8 men. These percentages reflected the composition of participants in the FHA intervention. The age of interviewed participants ranged from 38 to 72 years. Six interviewees were less than 40 years old, six were aged 40 to 50, 19 aged 51 to 65, and 9 were 66 or older. There were no differences between interviewees and eligible non-participants in race/ethnicity, age, gender, or in reported baseline self-management behaviors and attitudes. Participants interviewed were more likely to have attended more of the group classes (mean 5 vs. 3 classes) than those not interviewed, and 70% of those interviewed had been accompanied to at least one doctor’s visit by their FHA compared to 45% of those not interviewed.
The results section uses the following convention to indicate number of participants: A few = 1-5, Some = 6-10, A number = 11-19, Half = 20, A majority = 21-25, Many = 26-34, Almost all = 35 or more.
REACH Participants’ Expectations for and Assessments of Their Interactions with Physicians around Diabetes Care (Box 1)
The principal deficiency participants identified in their diabetes health care prior to their participation in REACH was the low quality and quantity of information about how to care for their diabetes they had received from their health care providers. In many described patient-doctor interactions, participants reported receiving inadequate information from their providers on how to manage their diabetes (quotes 1-4). At the same time, participants were reluctant to criticize their providers for this: Almost all participants reported feeling that their providers were trying to do a good job in the face of difficult circumstances with very limited time to do everything.
A majority of participants voiced low expectations that their providers could take the time to provide more comprehensive information on diabetes, with some participants explicitly placing the onus for the quality of their diabetes care on themselves rather than on their providers (quote 2). Almost half of the participants felt that the most they could expect from their doctors was to receive the medications they needed. A few participants noted, however, that their providers did not provide basic information on medications, such as precisely when to take them (quote 3). A number of participants stated that since providers had so little time, they only expected them to provide basic information and put them in touch with other resources to learn what they needed to know (quote 5).
Some participants focused on how proactive they should be in eliciting information from their physicians. Even given limited time for physician visits, some participants expressed the belief that more could be done by providers, patients, or both, to improve interactions. Some participants lamented that they did not know what to ask their providers to get the information they needed to improve self-management or that they wished they knew what they needed to do to gain their provider’s complete attention during a visit (quote 6). As was the case with many participants’ ‘criticisms’ of their providers, the interviewee in quote 6 couched her concern as something that she needs to do rather than expecting it as her due from her physician as a patient. A few participants, however, expressed higher expectations and stated that providers should tell them more about how to manage their diabetes without their having to ask (quote 4).
A few participants described interactions in which physicians took the time to explain and answer questions about their diabetes management (quotes 7-8). For example, an African American woman recounted an interaction in which her physician, in response to her question, explained how to manage her diet and medication and the rationale behind these instructions (quote 7).
Effect of FHA Intervention on Participants’ Diabetes Self-Management Knowledge and Care (Box 2)
Almost all participants reported that the REACH program improved their ability to manage their diabetes by providing knowledge that they had not known prior to REACH and emotional and social support. New knowledge included: 1) rationales that connected self-management tasks to diabetes outcomes and 2) education and training on specific strategies to meet diabetes care goals. They also reported 3) sustained and non-judgmental assistance to increase the motivation and confidence necessary to improve their diabetes self-management, and 4) social and peer support that also enabled them to better manage their diabetes.
REACH Provided Rationale for Performing Self-Management Tasks and Specific Strategies
Participants reported that REACH provided the “whole picture,” a broader context which connected self-management tasks to their effects on diabetes, to help participants understand why it was important to do recommended diabetes care tasks (quotes 9-11). This led to improved understanding and motivated participants to better manage their diabetes.
In addition to receiving information about the rationale for recommended diabetes self-management tasks, participants learned specific strategies from REACH FHAs to accomplish these tasks. While health care providers told participants what they needed to do to manage their diabetes (e.g., ‘lose weight’, ‘eat healthier’, ‘exercise more’), they rarely provided information or suggestions on concrete, feasible strategies to achieve these recommendations. As one participant put it, “You can tell me all day to do something, but it’s not going to help if I don’t know HOW to do it.” Many participants noted that they learned specific information on what to eat and what not to eat, appealing healthy recipes and cooking techniques using foods and approaches they had grown up with, shopping for food, and reading labels (quotes 12-14). They also reported learning how to access neighborhood resources that would help them improve self-management. (e.g., how to find better deals on medications, grocery stores to get produce at a discount, exercise classes, where to get affordable eyeglasses.)
Many participants noted that it was only through participation in the REACH intervention that they realized how much they had not known before about how to care for their diabetes (quote 9). In Quote 9, the interviewee notes that perhaps if he had known more [before participating in REACH] then he would have been able to ask his doctor to explain more things to him. A number of respondents noted the importance of FHAs devoting time and effort to provide them with individual attention and to thoroughly review and reinforce information in depth, providing specific examples of strategies to meet behavioral goals (quote 15-16). Of note, however, a few participants, while expressing appreciation for their FHA’s support, expressed concern about the depth of the FHAs’ own knowledge about diabetes. As one participant explained, “They try to be helpful as much as they know, because they’re really just learning themselves, I think…some things that maybe they couldn’t really give you the answer to, which I think they should know a little more…I think we asked her something one time and I can’t remember what it was that she couldn’t really answer either.”
Participants Received Vital Emotional and Informational Support from Their FHAs and the Community of REACH Participants
A majority of participants noted the importance of the emotional and/or information support they received from both their FHAs and other REACH participants. Some participants used words to describe FHAs such as “caring,” “the friendliness of her voice,” and “I felt a connection.” Some participants spoke specifically of the importance of FHAs in serving as ‘coaches’ to help motivate them and follow their progress closely, providing supportive and non-judgmental assistance (quotes 18-19). A few participants explicitly noted how they trusted their FHA not to judge them when they “messed up” which helped motivate them to just keep trying to do better next time, in contrast to their fear that their physician would be “mad” if they had not achieved expected results (quotes 19-20). One participant, however, did specifically criticize that FHAs do not themselves have diabetes: “I guess the only problem that I have with REACH is that none of [the FHAs] are diabetic. And I know they say well, we’re not diabetics but we’ve been trained. But then you still don’t know how I feel…Being trained and going through it are two different things.”
A few participants, although they regularly saw physicians, described REACH as being the first time they had not felt alone in dealing with a difficult illness, using phrases such as “it’s been so very lonely…you need someone to help you get over the fences,” and “they’re acknowledging me…you don’t have to sit there with all these confusions going on in your mind.” (quote 21) There were a number of participants, however, who did not describe feeling alone in dealing with their illness before REACH. Although they found REACH helpful, these participants felt they already had emotional support and some of the knowledge they needed. For them, REACH was a source of better information more than an emotional experience.
Another important source of motivation, and of useful information, was the community of REACH participants. Participants spoke of exchanging experiences of living with diabetes with people they could identify with (quotes 22 and 23). As described in quote 23, participants also gained information from each other on specific strategies to meet self-management goals, information that in the volume, degree of detail, and relevance to their everyday lives was more useful than information they received from their physicians.
Effect of Participation in the CHW Intervention on Interactions with Physicians (Box 3)
Many participants had little specific to say about how participating in the FHA intervention affected their interactions with their physicians. As one participant noted:
“There hasn’t been any change in the way I act with my doctor. It’s basically the same, but through the REACH program, you know, we learned a lot of things that I guess you could say the doctor didn’t have time to sit down and explain to us.”
An exception for some participants, however, was how learning “what they had not known” about diabetes care before participating in the intervention influenced their expectations of their physicians and their comfort in asking questions and seeking more information. For example, a participant said: “Now I feel more comfortable talking with my doctor and asking all that I think that I need to know. I know more, so I can ask more. I’m not so afraid.” (quote 25) As discussed earlier, prior to participating in REACH, lack of knowledge was in some cases accompanied by low expectations participants had of visits with their physicians; a few noted explicitly that before REACH they felt they could not make any extra demands on their providers. (quote 25) Before REACH, most participants also did not know specific techniques to improve interactions with their physicians, such as writing down all their questions before they went to the doctor (quotes 31-32).
In these accounts, when participants started asking their physicians more questions, the physicians responded positively, reinforcing and further explaining what their patients had learned from REACH (quotes 24-28). One participant reported that her physician seemed surprised when she realized that her patient hadn’t known to ask these questions (quote 27).
The theme of having more confidence—and less fear-- to ask questions and make specific requests of doctors was especially pronounced among Latino participants. As one Latino woman noted, “[My FHA] helped me see that when you ask questions, nothing bad happens…..they don’t send you to the police or take you to the ‘immi” [INS]”.(quote 29). One participant said that she had had low expectations of visits with her physicians because she came from a country “where when you go to a doctor or public hospital you understand that the doctor is doing you a favor to even see you.” (quote 30) Several participants specifically described the strategies they learned through REACH to prepare themselves to ask questions and make requests to their physicians in office visits (quotes 31-32).
DISCUSSION
These interviews with African American and Latino adults participating in or having recently completed a community health worker (CHW)-led diabetes self-management program supported a number of prior findings from quantitative studies on deficiencies in patient-doctor interactions. Striking themes were lack of adequate information from health care providers for effective diabetes self-management, participants’ low expectations for help from their providers, and participants’ hesitation to make specific requests of their health care providers before participating in the intervention. [1, 21-26] Interestingly, however, most of these reported deficiencies in patient-physician interactions only emerged in response to queries about what participants had gained from REACH rather than in response to direct queries about perceived deficiencies in the diabetes care they received from health care providers. Overall, almost all participants—even those who later discussed in depth the information and support they had not received from their health care providers—voiced satisfaction with their personal physicians and care received from their providers.
These interview findings suggest important ways that the FHA intervention improved diabetes self-management and understanding among participants. While almost all participants accepted the brief nature of clinic visits, they highlighted key contrasts between the quality of their experiences with physicians and their experiences with REACH. In particular, participants expressed their appreciation of FHAs’ provision of thorough information, explanations, and demonstrations of specific ways to improve behaviors (teaching “how” and not just “what”); and receiving sustained positive, non-judgmental support and encouragement from REACH FHAs and other peer participants. Participants reported that their visits with physicians had been constrained by both time and a lack of participant knowledge about how and what to ask their physicians—as well as by their overall low expectations for what they could receive from their physicians. As a result, before REACH, many participants had received fragmented and incomplete information and did not know where to start in managing their diabetes better. With the additional knowledge, information on specific strategies to improve diabetes self-management, training in strategies to improve patient-doctor communication (e.g., writing questions down before clinic visits) and confidence gained from REACH, participants better knew what questions to ask their doctor, how to approach asking these questions, and how to evaluate whether they were receiving the necessary tests and services. Our findings reinforced ways that greater patient activation may positively influence physician communication, as physicians often assume that if patients wanted information, they would ask for it. [19-20, 24] This, along with a patient’s lack of knowledge and a provider’s time constraints, may play off each other—the doctor might ask the patient if they have any questions, and if the patient, not knowing what to ask, responds, ‘no’, then the doctor may feel that they have adequately addressed the need to respond to the patient’s questions.
Our findings build on prior evaluations of CHW interventions to provide insights into specific ways that CHW interventions can effectively complement and enhance formal diabetes health care. As postulated in earlier studies, [13-16, 43] the well-trained FHAs provided a low-cost way to provide more time-intensive and community-based diabetes self-management training and support. In addition, FHAs served as important bridges between participants and the health care system, helping coach participants on more effective communication and areas to discuss with their health care providers. Because they came from similar backgrounds, there was less social distance between FHAs and REACH participants, helping create trust and comfort to work effectively together to improve diabetes-specific behaviors. As important as the FHAs’ one-on-one interactions with participants was the group support and information exchange among participants at the group sessions. Indeed, a good part of the benefits of interventions such as REACH may lie in creating a community that provides sustained emotional support and encouragement and a venue for sharing information about how to manage diabetes.
Our findings also reinforce the findings of two prior studies that explored factors explaining the success of CHWs in promoting healthy behaviors and self-management. KM Reisnschmidtd et al surveyed Latino women participants in a CHW-led chronic disease screening promotion program who emphasized the importance of the sustained, non-judgmental support and encouragement provided by the CHW in reducing barriers to health care and motivating their enhanced self-care. [17] In semi-structured interviews conducted by KL Davis et al with participants in a range of CHW programs supporting diabetes self-management, participants noted the value of CHWs explaining how to do something rather than just telling them what to do, as well as the ongoing follow-up and support provided by CHWs. [18]
Our findings must be interpreted in the face of several limitations. First, our findings are based on a small group of African-American and Latino adults with diabetes living in inner-city neighborhoods who had access to regular health care. Lack of access to health care is a significant source of racial and ethnic disparities in diabetes care and outcomes that we did not address in this study. Second, as with any study based on self-report, our findings are subject to social desirability bias. Although we assured participants of the confidentiality of their interviews and did not request the names of their health care providers, participants’ reluctance to report critical opinions of their health care providers may have contributed to our somewhat paradoxical findings that participants reported high satisfaction with their providers while delineating significant deficiencies in their care and interactions with providers when discussing how REACH had contributed to their diabetes care. Third, all of our interviews were with participants who had either finished the REACH Detroit intervention or were actively participating in the interventions. Thus, their reports of their relations with health care providers before their participation in REACH were subject to recall bias and influence from their participation in the intervention. Moreover, participants who agreed to be interviewed may have been more engaged in the program and hold more favorable views of the intervention than those who declined to be interviewed.
In conclusion, whereas most interviewees reported being largely satisfied with their personal physicians both before and after their participation in REACH, participants clearly delineated deficiencies they identified both in their own prior diabetes knowledge and in their interactions with physicians—most areas identified mainly through their discussions of what they had gained through REACH rather than through direct criticism of their physicians. The deficiencies participants cited in their prior knowledge, motivation, and support necessary to manage their diabetes have been identified in multiple studies as key to diabetes self-management and clinical outcomes. Moreover, such low expectations of and unassertiveness in requesting information and test results from providers have been hypothesized to contribute to racial and ethnic disparities in chronic disease care. [1] Our interview findings suggest a number of ways that community health worker programs that provide both one-on-one support and group self-management training sessions may be effective in improving diabetes self-management and care for African American and Latino adults with diabetes, thereby mitigating racial and ethnic disparities in diabetes outcomes.
Acknowledgments
This work was supported by the Blue Cross Blue Shield Foundation of Michigan (703RFP), the Centers for Disease Control and Prevention (CDC), REACH 2010 (U50CCU522189), the Department of Veterans Affairs (VA) Health Services Research & Development (HSR&D) Service (DIB 98-001), and the Michigan Diabetes Research and Training Center (NIDDK P60DK-20572). Dr. Heisler is a VA HSR&D Career Development awardee.
References
- 1.Smedley BD, Stith AY, Nelson AR Institute of Medicine. Committee on Understanding and Eliminating Racial and Ethinic Disparities in Health C: Unequal treatment confronting racial and ethnic disparities in healthcare. Washington, D.C: National Academy Press; 2002. [Google Scholar]
- 2.Harris MI, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care. 1999;22(3):403–8. doi: 10.2337/diacare.22.3.403. [DOI] [PubMed] [Google Scholar]
- 3.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic Disparities in Diabetic Complications in an Insured Population. JAMA. 2002;287(19):2519–2527. doi: 10.1001/jama.287.19.2519. [DOI] [PubMed] [Google Scholar]
- 4.Cowie CC, Port FK, Wolfe RA, Savage PJ, Moll PP, Hawthorne VM. Disparities in incidence of diabetic end-stage renal disease according to race and type of diabetes. N Engl J Med. 1989;321(16):1074–9. doi: 10.1056/NEJM198910193211603. [DOI] [PubMed] [Google Scholar]
- 5.Pugh JA, Stern MP, Haffner SM, Eifler CW, Zapata M. Excess incidence of treatment of end-stage renal disease in Mexican Americans. Amer J Epidemiol. 1988;127(1):135–44. doi: 10.1093/oxfordjournals.aje.a114773. [DOI] [PubMed] [Google Scholar]
- 6.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136(8):565–74. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 7.Cowie CC, Harris MI. Ambulatory medical care for non-Hispanic whites, African-Americans, and Mexican-Americans with NIDDM in the U.S. Diabetes Care. 1997;20(2):142–7. doi: 10.2337/diacare.20.2.142. [DOI] [PubMed] [Google Scholar]
- 8.Chin MH, Zhang JX, Merrell K. Diabetes in the African-American Medicare population. Morbidity, quality of care, and resource utilization. Diabetes Care. 1998;21(7):1090–5. doi: 10.2337/diacare.21.7.1090. [DOI] [PubMed] [Google Scholar]
- 9.Heisler M, Faul JD, Hayward RA, Langa KM, Blaum C, Weir D. Mechanisms for Racial and Ethnic Disparities in Glycemic Control in Middle-aged and Older Americans in the Health and Retirement Study. Arch Intern Med. 2007;167(17):1853–1860. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- 10.Kieffer E, Willis S, Odoms A, Guzman R, Loveluck J. REACH Detroit Partnership: Community-based Planning to Address Health Disparities in the Eastside and Southwest Communities of Detroit. 2000 [Google Scholar]
- 11.Kieffer EC, Willis SK, Odoms-Young AM, et al. Reducing disparities in diabetes among African-American and Latino residents of Detroit: the essential role of community planning focus groups. Ethn Dis. 2004;14(3 Suppl 1):S27–37. [PubMed] [Google Scholar]
- 12.Two Feathers J, Kieffer E, Palmisano G, Anderson M, Janz N, Spencer M, Guzman R, Heisler M, James S. Development, implementation and evaluation of the REACH Detroit Diabetes Lifestyle Curriculum. Diabetes Educator. 2007;33(3):509–520. doi: 10.1177/0145721707301371. [DOI] [PubMed] [Google Scholar]
- 13.Lewin SA, Dick J, Pond P, et al. Lay health workers in primary and community health care. The Cochrane Database of Systematic Reviews. 2005;(1) doi: 10.1002/14651858.CD004015.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Swider S. Outcome effectiveness of community health workers: An integrative literature review. Public Health Nurs. 2002;19(1):11–20. doi: 10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- 15.Navarro AM. Por La Vida model intervention enhances use of cancer screening tests among Latinas. American Journal of Preventive medicine. 1998;15(1):32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- 16.Norris SL, Chowdhury FM, Van Let K, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;(2006):544–556. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 17.Reinschmidt K, Hunter J, Fernández M, Lacy-Martínez C, Guernsey de Zapien J, Meister J. Understanding the success of promotoras in increasing chronic diseases screening. Journal of Health Care for the Poor and Underserved. 2006;17(2):256–64. doi: 10.1353/hpu.2006.0066. [DOI] [PubMed] [Google Scholar]
- 18.Davis K, O’Toole M, Brownson C, Llanos P, Fisher E. Teaching how, not what: the contributions of community health workers to diabetes self-management. The Diabetes Educator. 2007;33(Suppl 6):208S–215S. doi: 10.1177/0145721707304133. [DOI] [PubMed] [Google Scholar]
- 19.Stewart AL, Napoles-Springer A, Perez-Stable EJ. Interpersonal processes of care in diverse populations. Milbank Q. 1999;77(3):305–39. 274. doi: 10.1111/1468-0009.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Collins KS. Findings from the Commonwealth Fund 2001 Health Care Quality Survey. New York: The Commonwealth Fund; 2002. Diverse Communities, Common Concerns: Assessing Health Care Quality for Minority Americans. [Google Scholar]
- 21.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12(2):93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 22.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–9. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 23.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians’ participatory decision-making style. Results from the Medical Outcomes Study. Med Care. 1995;33(12):1176–87. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–15. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 25.Shavers VL, Lynch CF, Burmeister LF. Racial differences in factors that influence the willingness to participate in medical research studies. Ann Epidemiol. 2002;12(4):248–56. doi: 10.1016/s1047-2797(01)00265-4. [DOI] [PubMed] [Google Scholar]
- 26.Young M, Klingle RS. Silent partners in medical care: a cross-cultural study of patient participation. Health Commun. 1996;8(1):29–53. doi: 10.1207/s15327027hc0801_2. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–27. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 28.Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med. 1995;40(7):903–18. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- 29.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–33. see comments. [PMC free article] [PubMed] [Google Scholar]
- 30.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17(4):243–252. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med. 2003;18(8):624–33. doi: 10.1046/j.1525-1497.2003.31968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. How well do patients’ assessments of their diabetes self-management correlate with actual glycemic control and receipt of recommended diabetes services? Diabetes Care. 2003;26(3):738–43. doi: 10.2337/diacare.26.3.738. [DOI] [PubMed] [Google Scholar]
- 33.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 34.Bandura A. A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. Social Foundations of Thought and Action. [Google Scholar]
- 35.Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med. 2003;18(11):893–902. doi: 10.1046/j.1525-1497.2003.21132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21(10):1644–51. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 37.Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment. Results of a randomized controlled trial. Diabetes Care. 1995;18(7):943–9. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- 38.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient Self-management of Chronic Disease in Primary Care. JAMA. 2002;288(19):2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 40.Gilliland SS, Azen SP, Perez GE, Carter JS. Strong in body and spirit: lifestyle intervention for Native American adults with diabetes in New Mexico. Diabetes Care. 2002;25(1):78–83. doi: 10.2337/diacare.25.1.78. [DOI] [PubMed] [Google Scholar]
- 41.Two Feathers J, Kieffer EC, Palmisano G, et al. Racial and Ethnic Approaches to Community Health (REACH) Detroit Partnership: Improving Diabetes-Related Outcomes among African American and Latino Adults. Amer J Public Health. 2005;95(9):1552–60. doi: 10.2105/AJPH.2005.066134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–40. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 43.Educators AAoD: Diabetes Community Health Workers. The Diabetes Educator. 2003;29(5):818–824. doi: 10.1177/014572170302900511. [DOI] [PubMed] [Google Scholar]


