Abstract
Hepatitis C virus (HCV) infection often causes chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma. The development of a HCV cell culture system enabled us to investigate its whole HCV life cycle and develop a better understanding of the pathogenesis of this virus. Post-translational modification plays a crucial role in HCV replication and in the maturation of viral particles. There is growing evidence also suggesting that the ubiquitin-proteasome pathway and the ubiquitin-independent proteasome pathway are involved in the stability control of HCV proteins. Many viruses are known to manipulate the proteasome pathways to modulate the cell cycle, inhibit apoptosis, evade the immune system, and activate cell signaling, thereby contributing to persistent infection and viral carcinogenesis. The identification of functional interactions between HCV and the proteasome pathways will therefore shed new light on the life cycle and pathogenesis of HCV. This review summarizes the current knowledge on the involvement of the ubiquitin-dependent and -independent proteasome pathways in HCV infection and discusses the roles of these two distinct mechanisms in HCV pathogenesis.
Keywords: Hepatitis C virus, Ubiquitin, Proteasome, Degradation, Hepatitis
INTRODUCTION
Hepatitis C virus (HCV) is a single-stranded, positive-sense RNA virus from the family Flaviviridae and is the main cause of chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma[1-5]. More than 170 million people worldwide are chronically infected with HCV[6]. The 9.6-kb HCV genome encodes a unique open reading frame encoding a large precursor polyprotein, which is cleaved co-translationally into at least 10 proteins by two viral proteases and two cellular signalases[4,5,7-10].
The previous establishment of a HCV cell culture system has facilitated studies of the whole viral life cycle[11-13]. The HCV life cycle is tightly regulated by both viral and cellular proteins[5] and evidence is accumulating to show that the stability of HCV proteins is regulated through both the ubiquitin-dependent and ubiquitin-independent proteasome pathways[14-18]. Moreover, HCV infection has been shown to trigger the degradation of host factors[19]. It is well known that many viruses manipulate the ubiquitin-proteasome pathway to promote their propagation by redirecting the cellular ubiquitin machinery to enable replication, egress and evasion of the host immune system[20]. Although the majority of the protein turnover mediated by the proteasome occurs through the canonical ubiquitin-dependent 26S proteasome pathway, a number of viral proteins and host proteins are degraded through the 20S proteasome without prior polyubiquitylation[21,22]. The functional differences between these two proteasome pathways are poorly understood, although a number of proto-oncogenes and tumor suppressors are degraded through both mechanisms, indicative of a system that tightly regulates the turnover of key cellular proteins[23-28].
Ubiquitin is a 76 amino acid polypeptide that is highly conserved among eukaryotic organisms. The ubiquitin/26S proteasome pathway is composed of an enzymatic cascade that ubiquitylates proteins to target them for proteasomal degradation. The E1 ubiquitin-activating enzyme binds ubiquitin through a thioester linkage in an ATP-dependent manner[29,30]. The activated ubiquitin is then transferred to the E2 ubiquitin-conjugating enzyme which works in conjunction with the E3 ubiquitin ligase, which is responsible for conferring substrate specificity[31]. E3 mediates the transfer of ubiquitin to the target protein which is then rapidly degraded by the 26S proteasome[32,33]. A number of studies have revealed the existence of a proteasome-dependent but ubiquitin-independent pathway for protein degradation. Several key molecules, such as p53, p73, c-fos, p21, SRC-3, and the hepatitis B virus X protein are targeted by two distinct degradation pathways that function in a ubiquitin-dependent and ubiquitin-independent manner, respectively[21-28,34,35]. Although the pathophysiological significance of the proteasomal degradation of the HCV proteins and HCV-induced proteasomal degradation of host proteins remains to be elucidated, evidence is accumulating that the proteasome plays an essential role in propagation of HCV[14,15]. The roles of the proteasome pathways in HCV life cycle as well as in viral pathogenesis are further discussed below.
UBIQUITIN-DEPENDENT DEGRADATION OF HCV PROTEINS BY THE PROTEASOME
HCV core protein
The HCV core protein is a major component of the viral nucleocapsid and is a multifunctional factor involved in both the pathogenesis and hepatocarcinogenesis of HCV and is degraded through the ubiquitin-proteasome pathway[5,16,36]. The cellular ubiquitin ligase E6AP was identified as a HCV core-binding protein in our laboratory and shown to mediate the polyubiquitylation of the core protein and thereby target it for proteasomal degradation[14]. E6AP was first identified as the cellular factor that mediates the ubiquitin-dependent degradation of the tumor suppressor p53 in conjunction with the E6 protein of the cancer-associated human papillomavirus types 16 and 18[37,38]. The region between amino acids 58 and 71 of the HCV core protein is responsible for the interaction with E6AP. These 14 amino acids are highly conserved, with the first nine amino acids (PRGRRQPIP) present in the core proteins of all HCV genotypes. This suggests that the E6AP-dependent degradation of HCV core protein is also conserved. Indeed, a knockdown of endogenous E6AP by siRNA increases the production of infectious HCV particles, further suggesting that E6AP negatively regulates HCV propagation[14].
E2 protein
The HCV envelope proteins comprise two glycoproteins, E1 and E2. HCV infection requires the interaction between these proteins and the host cell membrane. HCV attachment and entry into host cells is a multistep process, involving several cell surface molecules, including CD81[39], the LDL receptor[40], scavenger receptor BI[41], claudin-1[42-44], and occludin[43,45]. Several E2 domains also play crucial roles in virus entry[46]. In addition, HCV E2 has been implicated in conferring resistance to interferon (IFN)-α. E2 contains a region homologous to the double stranded RNA-activated protein kinase (PKR) and its substrate, subunit α of the translation initiation factor eIF2α[27]. The unglycosylated form of the E2 protein (E2-p38) is retained in the cytosol and is degraded through the ubiquitin-proteasome pathway[47]. E2-p38, but not the glycosylated form of E2, interacts with PKR and is stabilized by treatment with IFN-α, suggesting that it contributes to the resistance of HCV to IFN-α. The ubiquitin ligase that targets E2-p38 remains to be identified.
NS5A protein
NS5A protein is a major component of the HCV replication complexes and can be found in basally phosphorylated (56 kDa) and hyperphosphorylated (58 kDa) forms. NS5A harbors an amphipathic α-helix at its amino terminus that promotes membrane association. In addition to this helix region, NS5A contains three domains (I-III). The N-terminal domain (domain I) coordinates a single zinc atom per protein molecule[48]. Zinc mesoporphyrin (ZnMP) is a non-heme metalloporphyrin and a synthetic heme analog of the central zinc in the mesoporphyrin macrocycle. ZnMP enhances the polyubiquitylation and proteasomal degradation of NS5A and suppresses HCV RNA replication[49]. The physiological role of the ubiquitin-dependent proteasomal degradation of NS5A protein is still unclear and the ubiquitin ligase that targets NS5A also remains to be identified.
NS5B protein
The HCV NS5B protein functions as an RNA-dependent RNA polymerase. NS5B binds to a ubiquitin-like protein, hPLIC1[50], which contains 589 amino acids and belongs to a family of type 2 ubiquitin-like (ubl) proteins. hPLIC1 harbors a non-cleavable ubiquitin-like (ubl) domain in its amino terminus and a ubiquitin-associated (uba) domain in its carboxyl terminus[51] and physically associates with the proteasome and at least two ubiquitin ligases (E6AP and βTRCP). NS5B binds to the uba domain of hPLIC1, an interaction which enhances the polyubiquitylation and proteasomal degradation of NS5B, suggesting that hPLIC1 regulates HCV RNA replication by affecting NS5B turnover[50]. The responsible E3 ligase for NS5B ubiquitylation again remains to be identified.
UBIQUITIN-INDEPENDENT DEGRADATION OF HCV PROTEINS VIA THE PROTEASOME
Core protein
The HCV core protein specifically interacts with a proteasome activator PA28γ/REGγ in the nucleus and is degraded through a PA28γ-dependent proteasome pathway[18]. In vivo experiments in a mouse model have suggested that PA28γ plays a critical role in HCV-associated insulin-resistance, steatogenesis, and hepatocarcinogenesis[52,53]. The proteasomal turnover of the HCV core protein is regulated by two distinct mechanisms, the E6AP-mediated ubiquitin-dependent pathway and the PA28γ-mediated ubiquitin-independent pathway[14,17] (Figure 1). E6AP enhances the ubiquitylation and degradation of the wild-type HCV core protein, but not a lysine-less mutant counterpart, whereas PA28γ enhances the degradation of both the wild type and lysine-less HCV core protein. A knockdown of either E6AP or PA28γ results in the stabilization of the wild-type core protein. However, the knockdown of PA28γ but not E6AP stabilizes the lysine-less mutant core protein, strongly suggesting that PA28γ enhances the ubiquitin-independent pathway. Knockdown of PA28γ in cells at pre-infection or post-infection with the HCV JFH1 strain impaired viral particle production but exhibited no effect on viral RNA replication[15]. The knockdown of PA28γ enhances the polyubiquitylation of the core protein and impairs HCV production, whereas a knockdown of E6AP reduces polyubiquitylation of core protein and enhances virus production. These findings suggest that HCV production is positively regulated by PA28γ and negatively regulated by E6AP through the degradation of the core protein.
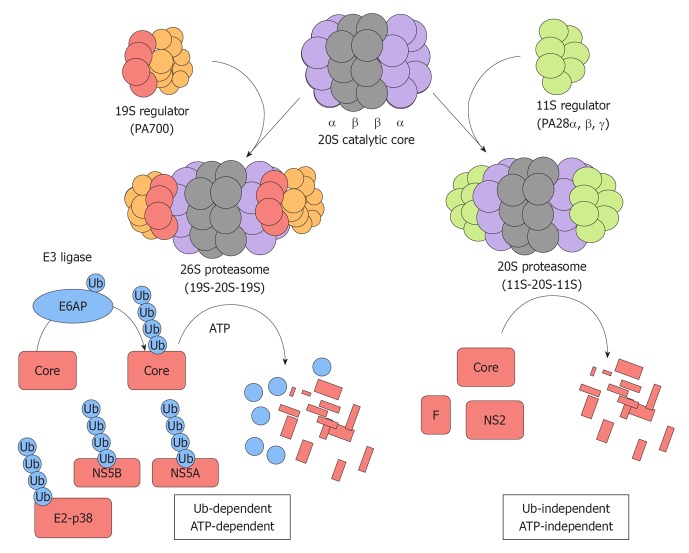
Figure 1.
Two distinct proteasome pathways target hepatitis C virus proteins for degradation. The 20S catalytic core is composed of α and β subunits that form a barrel-like structure. The 19S regulator (PA700) can associate with either or both ends of the 20S catalytic core. The combination of one 20S catalytic core and one or two 19S regulator generates the 26S proteasome that is responsible for ubiquitin-dependent ATP-dependent degradation of specific target substrates. E6AP mediates the polyubiquitylation of the hepatitis C virus (HCV) core protein and thereby targets it for ubiquitin-dependent degradation. E2-p38, NS5A, and NS5B are degraded through this ubiquitin-dependent and ATP-dependent proteasome pathway. The proteasome activator, PA28γ, forms a homoheptamer and is implicated in the ubiquitin-independent turnover of the HCV core protein. The F and NS2 proteins are also degraded through the ubiquitin-independent pathway.
F protein
The HCV F protein is encoded by the +1/-2 reading frame encompassed in the 5’ end of the polyprotein coding sequence[54]. The F protein is also known as ARFP (alternative reading frame protein) or as core+1 (which indicates the position of the new ORF)[55]. Translation of the F protein is mediated by a ribosomal frameshift at core protein codons 9-11 (HCV-1a strain). The biological role of the F protein remains to be clarified. The F protein is also highly unstable. It has been suggested that the F protein may bind to the α3 subunit of the 20S proteasome[56]. The α3 subunit facilitates the degradation of the F protein in a dose-dependent manner and a knockdown of the α3 subunit results in the stabilization of the F protein, even in the presence of a replicating HCV genome. The α3-binding domain within the F protein was mapped to the region between amino acids 40 and 60. There are currently three lines of evidence suggesting that the degradation of the F protein is ubiquitin-independent. First, an F protein mutant lacking lysine residues, which therefore cannot be ubiquitylated, is no more stable than the wild-type F protein. Second, F protein expressed in ts85 cells, which harbor a temperature-sensitive E1 ubiquitin-activating enzyme, is not stabilized when the cells are incubated at the non-permissive temperature. Third, the F protein can be degraded by the 20S proteasome in vitro in the absence of any ubiquitylation machinery.
NS2 protein
HCV NS2 protein is a transmembrane protein, composed of a highly hydrophobic N-terminal membrane binding domain and a C-terminal globular and cytosolic protease subdomain. NS2 protease cleaves off the N-terminus of NS3 protein and is involved in the assembly of HCV particles[57,58]. NS2 protein is also a short-lived protein that is rapidly degraded by the proteasome in a phosphorylation-dependent manner through the activity of casein kinase 2 (CK2). NS2 is phosphorylated by CK2 on a serine residue at position 168, which is a part of a consensus CK2 phosphorylation sequence motif (S/TXXE)[59]. This CK2 phosphoacceptor motif is highly conserved among NS2 proteins from all HCV genotypes. No ubiquitin conjugation of NS2 has been detected[59] and lysine mutagenesis has been reported to have no effect on NS2 levels[60]. These results suggest that the degradation of the HCV NS2 protein is ubiquitin-independent but proteasome-dependent.
HCV INFECTION-INDUCED UBIQUITIN-DEPENDENT DEGRADATION OF CELLULAR PROTEINS VIA THE PROTEASOME
Retinoblastoma tumor-suppressor protein
The abundance of the retinoblastoma tumor-suppressor protein (pRb) is negatively regulated in HCV RNA replicon cells[61] and HCVcc-infected cells[19]. The HCV RNA-dependent RNA polymerase NS5B protein forms a complex with pRb, targeting it for degradation, resulting in a reduction of pRb, the activation of the E2F-responsive promoter, and the promotion of cell proliferation[61]. NS5B contains a Leu-x-Cys/Asn-x-Asp motif that is homologous to the Rb-binding domains in the oncoproteins of DNA viruses and interacts with pRb through this motif. The ectopic expression of NS5B induces the polyubiquitylation of pRb, the abundance of which is restored by the siRNA knockdown of E6AP or by the overexpression of a dominant-negative E6AP mutant in HCV RNA replicon cells. This suggests the involvement of E6AP in pRb degradation, induced by HCV. However, it has been reported previously in an in vitro assay that the ubiquitylation of pRb is not promoted by E6AP, either in the presence or absence of NS5B[19]. The precise mechanism by which NS5B-dependent pRb ubiquitylation occurs thus remains to be clarified.
Suppressor of cytokine signaling 3
Suppressor of cytokine signaling 3 (SOCS3) is one of the negative regulators of cytokine signaling that function via the JAK-STAT pathway[62,63]. The SOCS3 protein levels have been found to be decreased in OR6 cells harboring a HCV genotype 1b replicon and also in Huh 7.5.1 cells infected with the HCV genotype 2a strain JFH1[64]. Treatment with the proteasome inhibitor MG132 blocked the inhibitory effects of HCV on the SOCS3 protein levels in both the replicon-harboring OR6 cells and JFH1-infected cells. JFH1 infection increased the ubiquitylation of SOCS3 compared with the mock infected cells. These results have suggested that HCV infection promotes the degradation of SOCS3 through the ubiquitin-dependent proteasome pathway. The underlying mechanism remains to be elucidated.
HCV INFECTION AFFECTS THE IMMUNOPROTEASOME
Proteasomal epitope processing
The induction of CD8+ T cells is dependent on the generation of MHC class I ligands by the proteasome. Whereas the amino-terminus of each epitope can be further defined by post-proteasomal aminoexopeptidases, the carboxyl terminus needs to be defined precisely by the first cleavage. Through the study of a single source outbreak of HCV, Seifert et al[65] have previously identified a mutation at a conserved tyrosine on the HCV NS3 protein, which was a tyrosine to phenylalanine substitution. This mutation was found to impair the correct carboxyl-terminal cleavage of an immune-dominant, HLA-A2 restrictive HCV NS31073-1081 epitope from its mutated polypeptide precursor, not only by the constitutive proteasomes, but also by the immunoproteasome. These mutations impair the induction of HCV-specific CD8+ T cells by affecting the proteasomal antigen-processing machinery.
MHC class I-restricted HCV antigen presentation and the effects of ethanol on this process
In Huh-7 cells co-expressing the HCV core protein and CYP2E1, the core protein slightly enhances 20S proteasome activity through a direct interaction and via the induction of low CYP2E1-dependent oxidative stress[66,67]. This proteasome activation event is, however, reversed after ethanol exposure which considerably reduces proteasome function due to the induction of high oxidative stress[66]. Ethanol-elicited suppression of the proteasome in the liver ultimately results in a reduced generation of antigenic peptides and reduced MHC class I-restricted antigen presentation on hepatocytes[68].
Low-molecular-mass protein 7
The HCV NS3 protein interacts with low-molecular-mass protein 7 (LMP7), a component of the immunoproteasome[69]. The minimal binding domain required for this interaction is located between the pro-sequence region of LMP7 (aa 1-40) and the protease domain of NS3. LMP7 has no effects on NS3 protease activity in vitro. The peptidase activities of LMP7 immunoproteasome, however, are markedly reduced in a HCV RNA subgenomic replicon. These findings suggest that the downregulation of proteasome peptidase activities could interfere with the processing of viral antigens for presentation by MHC class I molecules, thereby contributing to persistent infection by HCV.
CONCLUSION
In the present review, the current knowledge on the involvement of the ubiquitin-proteasome pathway and ubiquitin-independent proteasome pathway on HCV infection is summarized (Figure 1 and Table 1). As is the case with many other virus types, HCV may manipulate the ubiquitin system and the proteasome system to favor its propagation and contribute to viral pathogenesis. The body of knowledge regarding the ubiquitin-system and the proteasome system has markedly grown in recent years[21,22] and it has now been demonstrated that canonical Lys 48-linked polyubiquitin chains are not the only signals that initiate proteasome-mediated degradation. Monoubiquitylation[70], Lys 63-linked chains[71], Lys 11-linked chains[72], and linear chains[73-75] have been reported to have various functions, including the activation of signaling pathways and cell-cycle progression. Nothing is known however about the involvement of de-ubiquitylating enzymes in the HCV life cycle. The future identification of key molecules in the ubiquitin and proteasome systems will likely provide new insights and a better understanding of the life cycle and pathogenesis of HCV, knowledge which will be essential for the design of novel anti-HCV therapeutics.
Table 1.
The ubiquitin-dependent and -independent pathways that target hepatitis C virus proteins for degradation
| HCV protein | E3 ligase | Function | Ref. |
| Ubiquitin-dependent, ATP-dependent, 26S proteasome pathway | |||
| Core | E6AP1 | Inhibit virus production | [14-17] |
| E2-p38 | Unknown1 | Immune avoidance | [47] |
| NS5A | Unknown1 | Inhibit replication | [49] |
| NS5B | Unknown1 | Inhibit replication | [50] |
| Ubiquitin-independent, ATP-independent, 20S proteasome pathway | |||
| Core | PA28γ2 | Enhance virus production, steatosis | [15,18,52,53] |
| F | -2 | Unknown | [56] |
| NS2 | CK22 | Unknown | [57,60] |
E3 ligase;
Host factor. HCV: Hepatitis C virus; CK2: Casein kinase 2.
ACKNOWLEDGMENTS
I am grateful to all of my collaborators who contributed to the studies cited herein, most notably Masayuki Shirakura, Kyoko Murakami, Ryosuke Suzuki, Tetsuro Suzuki, Kohji Moriishi, Yoshiharu Matsuura, Hak Hotta, and Tatsuo Miyamura.
Footnotes
Supported by (in part) Grants in-aid from the Ministry of Health, Labour and Welfare, and the Ministry of Education, Culture, Sports, Science, and Technology, Japan
Peer reviewer: Gualtiero Alvisi, PhD, Department of Infectious Diseases, Heidelberg University, INF345, Heidelberg, 69121, Germany
S- Editor Zhang SS L- Editor A E- Editor Zheng XM
References
- 1.Choo QL, Kuo G, Weiner AJ, Overby LR, Bradley DW, Houghton M. Isolation of a cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science. 1989;244:359–362. doi: 10.1126/science.2523562. [DOI] [PubMed] [Google Scholar]
- 2.Kuo G, Choo QL, Alter HJ, Gitnick GL, Redeker AG, Purcell RH, Miyamura T, Dienstag JL, Alter MJ, Stevens CE. An assay for circulating antibodies to a major etiologic virus of human non-A, non-B hepatitis. Science. 1989;244:362–364. doi: 10.1126/science.2496467. [DOI] [PubMed] [Google Scholar]
- 3.Saito I, Miyamura T, Ohbayashi A, Harada H, Katayama T, Kikuchi S, Watanabe Y, Koi S, Onji M, Ohta Y. Hepatitis C virus infection is associated with the development of hepatocellular carcinoma. Proc Natl Acad Sci USA. 1990;87:6547–6549. doi: 10.1073/pnas.87.17.6547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lemon SM, Walker C, Alter MJ, Yi M. Hepatitis C virus. In: Fields BN, Knipe DM, Howley PM, editors. Fields’ virology. 5th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2007. pp. 1291–1304. [Google Scholar]
- 5.Suzuki T, Aizaki H, Murakami K, Shoji I, Wakita T. Molecular biology of hepatitis C virus. J Gastroenterol. 2007;42:411–423. doi: 10.1007/s00535-007-2030-3. [DOI] [PubMed] [Google Scholar]
- 6.Poynard T, Yuen MF, Ratziu V, Lai CL. Viral hepatitis C. Lancet. 2003;362:2095–2100. doi: 10.1016/s0140-6736(03)15109-4. [DOI] [PubMed] [Google Scholar]
- 7.Kato N, Hijikata M, Ootsuyama Y, Nakagawa M, Ohkoshi S, Sugimura T, Shimotohno K. Molecular cloning of the human hepatitis C virus genome from Japanese patients with non-A, non-B hepatitis. Proc Natl Acad Sci USA. 1990;87:9524–9528. doi: 10.1073/pnas.87.24.9524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choo QL, Richman KH, Han JH, Berger K, Lee C, Dong C, Gallegos C, Coit D, Medina-Selby R, Barr PJ. Genetic organization and diversity of the hepatitis C virus. Proc Natl Acad Sci USA. 1991;88:2451–2455. doi: 10.1073/pnas.88.6.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grakoui A, Wychowski C, Lin C, Feinstone SM, Rice CM. Expression and identification of hepatitis C virus polyprotein cleavage products. J Virol. 1993;67:1385–1395. doi: 10.1128/jvi.67.3.1385-1395.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shoji I, Suzuki T, Sato M, Aizaki H, Chiba T, Matsuura Y, Miyamura T. Internal processing of hepatitis C virus NS3 protein. Virology. 1999;254:315–323. doi: 10.1006/viro.1998.9540. [DOI] [PubMed] [Google Scholar]
- 11.Wakita T, Pietschmann T, Kato T, Date T, Miyamoto M, Zhao Z, Murthy K, Habermann A, Kräusslich HG, Mizokami M, et al. Production of infectious hepatitis C virus in tissue culture from a cloned viral genome. Nat Med. 2005;11:791–796. doi: 10.1038/nm1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindenbach BD, Evans MJ, Syder AJ, Wölk B, Tellinghuisen TL, Liu CC, Maruyama T, Hynes RO, Burton DR, McKeating JA, et al. Complete replication of hepatitis C virus in cell culture. Science. 2005;309:623–626. doi: 10.1126/science.1114016. [DOI] [PubMed] [Google Scholar]
- 13.Zhong J, Gastaminza P, Cheng G, Kapadia S, Kato T, Burton DR, Wieland SF, Uprichard SL, Wakita T, Chisari FV. Robust hepatitis C virus infection in vitro. Proc Natl Acad Sci USA. 2005;102:9294–9299. doi: 10.1073/pnas.0503596102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shirakura M, Murakami K, Ichimura T, Suzuki R, Shimoji T, Fukuda K, Abe K, Sato S, Fukasawa M, Yamakawa Y, et al. E6AP ubiquitin ligase mediates ubiquitylation and degradation of hepatitis C virus core protein. J Virol. 2007;81:1174–1185. doi: 10.1128/JVI.01684-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moriishi K, Shoji I, Mori Y, Suzuki R, Suzuki T, Kataoka C, Matsuura Y. Involvement of PA28gamma in the propagation of hepatitis C virus. Hepatology. 2010;52:411–420. doi: 10.1002/hep.23680. [DOI] [PubMed] [Google Scholar]
- 16.Suzuki R, Tamura K, Li J, Ishii K, Matsuura Y, Miyamura T, Suzuki T. Ubiquitin-mediated degradation of hepatitis C virus core protein is regulated by processing at its carboxyl terminus. Virology. 2001;280:301–309. doi: 10.1006/viro.2000.0785. [DOI] [PubMed] [Google Scholar]
- 17.Suzuki R, Moriishi K, Fukuda K, Shirakura M, Ishii K, Shoji I, Wakita T, Miyamura T, Matsuura Y, Suzuki T. Proteasomal turnover of hepatitis C virus core protein is regulated by two distinct mechanisms: a ubiquitin-dependent mechanism and a ubiquitin-independent but PA28gamma-dependent mechanism. J Virol. 2009;83:2389–2392. doi: 10.1128/JVI.01690-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moriishi K, Okabayashi T, Nakai K, Moriya K, Koike K, Murata S, Chiba T, Tanaka K, Suzuki R, Suzuki T, et al. Proteasome activator PA28gamma-dependent nuclear retention and degradation of hepatitis C virus core protein. J Virol. 2003;77:10237–10249. doi: 10.1128/JVI.77.19.10237-10249.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Munakata T, Liang Y, Kim S, McGivern DR, Huibregtse J, Nomoto A, Lemon SM. Hepatitis C virus induces E6AP-dependent degradation of the retinoblastoma protein. PLoS Pathog. 2007;3:1335–1347. doi: 10.1371/journal.ppat.0030139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Randow F, Lehner PJ. Viral avoidance and exploitation of the ubiquitin system. Nat Cell Biol. 2009;11:527–534. doi: 10.1038/ncb0509-527. [DOI] [PubMed] [Google Scholar]
- 21.Jariel-Encontre I, Bossis G, Piechaczyk M. Ubiquitin-independent degradation of proteins by the proteasome. Biochim Biophys Acta. 2008;1786:153–177. doi: 10.1016/j.bbcan.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 22.Hwang J, Winkler L, Kalejta RF. Ubiquitin-independent proteasomal degradation during oncogenic viral infections. Biochim Biophys Acta. 2011;1816:147–157. doi: 10.1016/j.bbcan.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jariel-Encontre I, Pariat M, Martin F, Carillo S, Salvat C, Piechaczyk M. Ubiquitinylation is not an absolute requirement for degradation of c-Jun protein by the 26 S proteasome. J Biol Chem. 1995;270:11623–11627. doi: 10.1074/jbc.270.19.11623. [DOI] [PubMed] [Google Scholar]
- 24.Asher G, Lotem J, Sachs L, Kahana C, Shaul Y. Mdm-2 and ubiquitin-independent p53 proteasomal degradation regulated by NQO1. Proc Natl Acad Sci USA. 2002;99:13125–13130. doi: 10.1073/pnas.202480499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asher G, Tsvetkov P, Kahana C, Shaul Y. A mechanism of ubiquitin-independent proteasomal degradation of the tumor suppressors p53 and p73. Genes Dev. 2005;19:316–321. doi: 10.1101/gad.319905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jin Y, Lee H, Zeng SX, Dai MS, Lu H. MDM2 promotes p21waf1/cip1 proteasomal turnover independently of ubiquitylation. EMBO J. 2003;22:6365–6377. doi: 10.1093/emboj/cdg600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lonard DM, Nawaz Z, Smith CL, O'Malley BW. The 26S proteasome is required for estrogen receptor-alpha and coactivator turnover and for efficient estrogen receptor-alpha transactivation. Mol Cell. 2000;5:939–948. doi: 10.1016/s1097-2765(00)80259-2. [DOI] [PubMed] [Google Scholar]
- 28.Sheaff RJ, Singer JD, Swanger J, Smitherman M, Roberts JM, Clurman BE. Proteasomal turnover of p21Cip1 does not require p21Cip1 ubiquitination. Mol Cell. 2000;5:403–410. doi: 10.1016/s1097-2765(00)80435-9. [DOI] [PubMed] [Google Scholar]
- 29.Ciechanover A, Heller H, Katz-Etzion R, Hershko A. Activation of the heat-stable polypeptide of the ATP-dependent proteolytic system. Proc Natl Acad Sci USA. 1981;78:761–765. doi: 10.1073/pnas.78.2.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haas AL, Rose IA. The mechanism of ubiquitin activating enzyme. A kinetic and equilibrium analysis. J Biol Chem. 1982;257:10329–10337. [PubMed] [Google Scholar]
- 31.Hershko A, Heller H, Eytan E, Reiss Y. The protein substrate binding site of the ubiquitin-protein ligase system. J Biol Chem. 1986;261:11992–11999. [PubMed] [Google Scholar]
- 32.Ciechanover A, Schwartz AL. The ubiquitin-proteasome pathway: the complexity and myriad functions of proteins death. Proc Natl Acad Sci USA. 1998;95:2727–2730. doi: 10.1073/pnas.95.6.2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ciechanover A, Orian A, Schwartz AL. Ubiquitin-mediated proteolysis: biological regulation via destruction. Bioessays. 2000;22:442–451. doi: 10.1002/(SICI)1521-1878(200005)22:5<442::AID-BIES6>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 34.Hu Z, Zhang Z, Doo E, Coux O, Goldberg AL, Liang TJ. Hepatitis B virus X protein is both a substrate and a potential inhibitor of the proteasome complex. J Virol. 1999;73:7231–7240. doi: 10.1128/jvi.73.9.7231-7240.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim JH, Sohn SY, Benedict Yen TS, Ahn BY. Ubiquitin-dependent and -independent proteasomal degradation of hepatitis B virus X protein. Biochem Biophys Res Commun. 2008;366:1036–1042. doi: 10.1016/j.bbrc.2007.12.070. [DOI] [PubMed] [Google Scholar]
- 36.Polyak SJ, Klein KC, Shoji I, Miyamura T, Lingappa JR. Assemble and Interact: Pleiotropic Functions of the HCV Core Protein. In: Tan SL, editor. Hepatitis C Viruses: Genomes and Molecular Biology. Norfolk: Horizon Bioscience; 2006. p. Chapter 3. [PubMed] [Google Scholar]
- 37.Scheffner M, Huibregtse JM, Vierstra RD, Howley PM. The HPV-16 E6 and E6-AP complex functions as a ubiquitin-protein ligase in the ubiquitination of p53. Cell. 1993;75:495–505. doi: 10.1016/0092-8674(93)90384-3. [DOI] [PubMed] [Google Scholar]
- 38.Huibregtse JM, Scheffner M, Howley PM. Cloning and expression of the cDNA for E6-AP, a protein that mediates the interaction of the human papillomavirus E6 oncoprotein with p53. Mol Cell Biol. 1993;13:775–784. doi: 10.1128/mcb.13.2.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pileri P, Uematsu Y, Campagnoli S, Galli G, Falugi F, Petracca R, Weiner AJ, Houghton M, Rosa D, Grandi G, et al. Binding of hepatitis C virus to CD81. Science. 1998;282:938–941. doi: 10.1126/science.282.5390.938. [DOI] [PubMed] [Google Scholar]
- 40.Agnello V, Abel G, Elfahal M, Knight GB, Zhang QX. Hepatitis C virus and other flaviviridae viruses enter cells via low density lipoprotein receptor. Proc Natl Acad Sci USA. 1999;96:12766–12771. doi: 10.1073/pnas.96.22.12766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scarselli E, Ansuini H, Cerino R, Roccasecca RM, Acali S, Filocamo G, Traboni C, Nicosia A, Cortese R, Vitelli A. The human scavenger receptor class B type I is a novel candidate receptor for the hepatitis C virus. EMBO J. 2002;21:5017–5025. doi: 10.1093/emboj/cdf529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Evans MJ, von Hahn T, Tscherne DM, Syder AJ, Panis M, Wölk B, Hatziioannou T, McKeating JA, Bieniasz PD, Rice CM. Claudin-1 is a hepatitis C virus co-receptor required for a late step in entry. Nature. 2007;446:801–805. doi: 10.1038/nature05654. [DOI] [PubMed] [Google Scholar]
- 43.Liu S, Yang W, Shen L, Turner JR, Coyne CB, Wang T. Tight junction proteins claudin-1 and occludin control hepatitis C virus entry and are downregulated during infection to prevent superinfection. J Virol. 2009;83:2011–2014. doi: 10.1128/JVI.01888-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang W, Qiu C, Biswas N, Jin J, Watkins SC, Montelaro RC, Coyne CB, Wang T. Correlation of the tight junction-like distribution of Claudin-1 to the cellular tropism of hepatitis C virus. J Biol Chem. 2008;283:8643–8653. doi: 10.1074/jbc.M709824200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ploss A, Evans MJ, Gaysinskaya VA, Panis M, You H, de Jong YP, Rice CM. Human occludin is a hepatitis C virus entry factor required for infection of mouse cells. Nature. 2009;457:882–886. doi: 10.1038/nature07684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zeisel MB, Fofana I, Fafi-Kremer S, Baumert TF. Hepatitis C virus entry into hepatocytes: molecular mechanisms and targets for antiviral therapies. J Hepatol. 2011;54:566–576. doi: 10.1016/j.jhep.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 47.Pavio N, Taylor DR, Lai MM. Detection of a novel unglycosylated form of hepatitis C virus E2 envelope protein that is located in the cytosol and interacts with PKR. J Virol. 2002;76:1265–1272. doi: 10.1128/JVI.76.3.1265-1272.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tellinghuisen TL, Marcotrigiano J, Rice CM. Structure of the zinc-binding domain of an essential component of the hepatitis C virus replicase. Nature. 2005;435:374–379. doi: 10.1038/nature03580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hou W, Tian Q, Zheng J, Bonkovsky HL. Zinc mesoporphyrin induces rapid proteasomal degradation of hepatitis C nonstructural 5A protein in human hepatoma cells. Gastroenterology. 2010;138:1909–1919. doi: 10.1053/j.gastro.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gao L, Tu H, Shi ST, Lee KJ, Asanaka M, Hwang SB, Lai MM. Interaction with a ubiquitin-like protein enhances the ubiquitination and degradation of hepatitis C virus RNA-dependent RNA polymerase. J Virol. 2003;77:4149–4159. doi: 10.1128/JVI.77.7.4149-4159.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kleijnen MF, Shih AH, Zhou P, Kumar S, Soccio RE, Kedersha NL, Gill G, Howley PM. The hPLIC proteins may provide a link between the ubiquitination machinery and the proteasome. Mol Cell. 2000;6:409–419. doi: 10.1016/s1097-2765(00)00040-x. [DOI] [PubMed] [Google Scholar]
- 52.Miyamoto H, Moriishi K, Moriya K, Murata S, Tanaka K, Suzuki T, Miyamura T, Koike K, Matsuura Y. Involvement of the PA28gamma-dependent pathway in insulin resistance induced by hepatitis C virus core protein. J Virol. 2007;81:1727–1735. doi: 10.1128/JVI.01683-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moriishi K, Mochizuki R, Moriya K, Miyamoto H, Mori Y, Abe T, Murata S, Tanaka K, Miyamura T, Suzuki T, et al. Critical role of PA28gamma in hepatitis C virus-associated steatogenesis and hepatocarcinogenesis. Proc Natl Acad Sci USA. 2007;104:1661–1666. doi: 10.1073/pnas.0607312104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu Z, Choi J, Yen TS, Lu W, Strohecker A, Govindarajan S, Chien D, Selby MJ, Ou J. Synthesis of a novel hepatitis C virus protein by ribosomal frameshift. EMBO J. 2001;20:3840–3848. doi: 10.1093/emboj/20.14.3840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Varaklioti A, Vassilaki N, Georgopoulou U, Mavromara P. Alternate translation occurs within the core coding region of the hepatitis C viral genome. J Biol Chem. 2002;277:17713–17721. doi: 10.1074/jbc.M201722200. [DOI] [PubMed] [Google Scholar]
- 56.Yuksek K, Chen WL, Chien D, Ou JH. Ubiquitin-independent degradation of hepatitis C virus F protein. J Virol. 2009;83:612–621. doi: 10.1128/JVI.00832-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jones CT, Murray CL, Eastman DK, Tassello J, Rice CM. Hepatitis C virus p7 and NS2 proteins are essential for production of infectious virus. J Virol. 2007;81:8374–8383. doi: 10.1128/JVI.00690-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jirasko V, Montserret R, Appel N, Janvier A, Eustachi L, Brohm C, Steinmann E, Pietschmann T, Penin F, Bartenschlager R. Structural and functional characterization of nonstructural protein 2 for its role in hepatitis C virus assembly. J Biol Chem. 2008;283:28546–28562. doi: 10.1074/jbc.M803981200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Franck N, Le Seyec J, Guguen-Guillouzo C, Erdtmann L. Hepatitis C virus NS2 protein is phosphorylated by the protein kinase CK2 and targeted for degradation to the proteasome. J Virol. 2005;79:2700–2708. doi: 10.1128/JVI.79.5.2700-2708.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Welbourn S, Jirasko V, Breton V, Reiss S, Penin F, Bartenschlager R, Pause A. Investigation of a role for lysine residues in non-structural proteins 2 and 2/3 of the hepatitis C virus for their degradation and virus assembly. J Gen Virol. 2009;90:1071–1080. doi: 10.1099/vir.0.009944-0. [DOI] [PubMed] [Google Scholar]
- 61.Munakata T, Nakamura M, Liang Y, Li K, Lemon SM. Down-regulation of the retinoblastoma tumor suppressor by the hepatitis C virus NS5B RNA-dependent RNA polymerase. Proc Natl Acad Sci USA. 2005;102:18159–18164. doi: 10.1073/pnas.0505605102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Starr R, Willson TA, Viney EM, Murray LJ, Rayner JR, Jenkins BJ, Gonda TJ, Alexander WS, Metcalf D, Nicola NA, et al. A family of cytokine-inducible inhibitors of signalling. Nature. 1997;387:917–921. doi: 10.1038/43206. [DOI] [PubMed] [Google Scholar]
- 63.Endo TA, Masuhara M, Yokouchi M, Suzuki R, Sakamoto H, Mitsui K, Matsumoto A, Tanimura S, Ohtsubo M, Misawa H, et al. A new protein containing an SH2 domain that inhibits JAK kinases. Nature. 1997;387:921–924. doi: 10.1038/43213. [DOI] [PubMed] [Google Scholar]
- 64.Shao RX, Zhang L, Peng LF, Sun E, Chung WJ, Jang JY, Tsai WL, Hyppolite G, Chung RT. Suppressor of cytokine signaling 3 suppresses hepatitis C virus replication in an mTOR-dependent manner. J Virol. 2010;84:6060–6069. doi: 10.1128/JVI.02484-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Seifert U, Liermann H, Racanelli V, Halenius A, Wiese M, Wedemeyer H, Ruppert T, Rispeter K, Henklein P, Sijts A, et al. Hepatitis C virus mutation affects proteasomal epitope processing. J Clin Invest. 2004;114:250–259. doi: 10.1172/JCI20985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Osna NA, White RL, Krutik VM, Wang T, Weinman SA, Donohue TM. Proteasome activation by hepatitis C core protein is reversed by ethanol-induced oxidative stress. Gastroenterology. 2008;134:2144–2152. doi: 10.1053/j.gastro.2008.02.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Osna NA. Hepatitis C virus and ethanol alter antigen presentation in liver cells. World J Gastroenterol. 2009;15:1201–1208. doi: 10.3748/wjg.15.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Osna NA, White RL, Thiele GM, Donohue TM. Ethanol metabolism alters major histocompatibility complex class I-restricted antigen presentation in liver cells. Hepatology. 2009;49:1308–1315. doi: 10.1002/hep.22787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Khu YL, Tan YJ, Lim SG, Hong W, Goh PY. Hepatitis C virus non-structural protein NS3 interacts with LMP7, a component of the immunoproteasome, and affects its proteasome activity. Biochem J. 2004;384:401–409. doi: 10.1042/BJ20040858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Boutet SC, Disatnik MH, Chan LS, Iori K, Rando TA. Regulation of Pax3 by proteasomal degradation of monoubiquitinated protein in skeletal muscle progenitors. Cell. 2007;130:349–362. doi: 10.1016/j.cell.2007.05.044. [DOI] [PubMed] [Google Scholar]
- 71.Hofmann RM, Pickart CM. In vitro assembly and recognition of Lys-63 polyubiquitin chains. J Biol Chem. 2001;276:27936–27943. doi: 10.1074/jbc.M103378200. [DOI] [PubMed] [Google Scholar]
- 72.Kim HT, Kim KP, Lledias F, Kisselev AF, Scaglione KM, Skowyra D, Gygi SP, Goldberg AL. Certain pairs of ubiquitin-conjugating enzymes (E2s) and ubiquitin-protein ligases (E3s) synthesize nondegradable forked ubiquitin chains containing all possible isopeptide linkages. J Biol Chem. 2007;282:17375–17386. doi: 10.1074/jbc.M609659200. [DOI] [PubMed] [Google Scholar]
- 73.Kirisako T, Kamei K, Murata S, Kato M, Fukumoto H, Kanie M, Sano S, Tokunaga F, Tanaka K, Iwai K. A ubiquitin ligase complex assembles linear polyubiquitin chains. EMBO J. 2006;25:4877–4887. doi: 10.1038/sj.emboj.7601360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tokunaga F, Nakagawa T, Nakahara M, Saeki Y, Taniguchi M, Sakata S, Tanaka K, Nakano H, Iwai K. SHARPIN is a component of the NF-κB-activating linear ubiquitin chain assembly complex. Nature. 2011;471:633–636. doi: 10.1038/nature09815. [DOI] [PubMed] [Google Scholar]
- 75.Ikeda F, Deribe YL, Skånland SS, Stieglitz B, Grabbe C, Franz-Wachtel M, van Wijk SJ, Goswami P, Nagy V, Terzic J, et al. SHARPIN forms a linear ubiquitin ligase complex regulating NF-κB activity and apoptosis. Nature. 2011;471:637–641. doi: 10.1038/nature09814. [DOI] [PMC free article] [PubMed] [Google Scholar]