Abstract
Background
Evidence shows that high Medicare spending is not associated with better health outcomes at a regional level, and that high spending in hospitals is not associated with better process quality. But the relationship between hospital spending and inpatient mortality is less well understood.
Objective
To determine the association between hospital spending and risk-adjusted inpatient mortality.
Design
Retrospective cohort study.
Setting
Database of discharge records from 1999–2008 for 208 California hospitals included in the Dartmouth Atlas of Health Care
Patients
2,545,352 patients hospitalized during 1999–2008 with one of six major medical conditions.
Measurements
Inpatient mortality rates among patients admitted to hospitals with varying levels of end-of-life hospital spending.
Results
For each of six admitting diagnoses – acute myocardial infarction, congestive heart failure, acute stroke, gastrointestinal hemorrhage, hip fracture, and pneumonia – patient admission to higher-spending hospitals was associated with lower risk-adjusted inpatient mortality. During 1999–2003, for example, patients admitted with acute myocardial infarction to California hospitals in the highest quintile of hospital spending had lower inpatient mortality than those admitted to hospitals in the lowest quintile (odds ratio of mortality 0.862, 95% confidence interval 0.742–0.983). Predicted inpatient deaths would increase by 1,831 if all patients admitted with acute myocardial infarction were cared for in hospitals in the lowest quintile of spending rather than the highest. The association between hospital spending and inpatient mortality did not vary by geographic region or hospital size.
Limitations
Unobserved predictors of mortality create uncertainty about whether greater inpatient hospital spending leads to lower inpatient mortality.
Conclusion
Hospitals that spend more at the end of life have lower inpatient mortality for a variety of major admitting medical conditions.
Primary funding source
National Institute on Aging, RAND Bing Center for Health Economics
A convincing set of studies demonstrate that U.S. regions which spend more on medical care have similar or poorer patient outcomes compared to lower spending areas.(1, 2) Regions vary widely in both spending and quality of care, with high spending regions engaging in more use of specialists, diagnostic tests and imaging, and inpatient hospital care, yet generally producing no better care.(2) The implication of these studies for health care reform and for curbing growth in health care spending is heavily debated.(3–6)
Examining variation in total medical spending across regions provides an informative overall picture; however, medical spending may lead to better patient outcomes in some circumstances (e.g. inpatient hospital spending) while not in others.(7) For example, a recent study of six California teaching hospitals found that patients with congestive heart failure (CHF) had lower mortality when treated at hospitals where lengths of stay and total costs were higher.(7) A related study of Pennsylvania acute care hospitals demonstrated that patients in hospitals with higher intensity in end-of-life treatment (e.g. intensive care unit admission, mechanical ventilation, etc.) experienced lower rates of post-admission mortality.(8)
Building on this prior work, we analyzed the association between hospital spending – the sum of spending on inpatient physician visits, hospital room charges, laboratory testing, diagnostic imaging, medication administration, and procedures – and inpatient mortality for the periods 1999–2003 and 2004–2008 for six major medical conditions in 208 California hospitals. For 1999–2003, we used overall hospital spending during the last two years of life of Medicare fee-for-service beneficiaries, drawing on the most recent Dartmouth Atlas. Hospital spending in the Dartmouth Atlas does not vary by medical condition. For 2004–2008, a period for which Dartmouth Atlas hospital spending was unavailable, we computed diagnosis-specific hospital- level spending based on patients who died while hospitalized. For each diagnosis in each time period, we estimated patient-level logistic models of the association between hospital spending and inpatient hospital mortality. In addition to patient socio-demographic and hospital/region factors, we used validated risk-adjustment models developed by the Agency for Healthcare Research and Quality (AHRQ) to account for underlying co-morbidities affecting inpatient mortality.
METHODS
We analyzed hospital spending and inpatient mortality in 208 California hospitals for the periods 1999–2003 and 2004–2008. We selected all California hospitals that were included in the most recent Dartmouth Atlas, which reported hospital spending measures for 1999–2003. Whether or not a hospital was included in the Atlas, and therefore in our study, was based on the number of Medicare fee-for-service beneficiaries admitted to that hospital. Our sample of hospitals accounted for about 2/3 of all California discharges over the study periods.
Sample
We studied six medical conditions: acute myocardial infarction (AMI), CHF, acute stroke, gastrointestinal hemorrhage, hip fracture, and pneumonia. These conditions were chosen because the processes of care associated with them are important inpatient quality indicators(9), the acute conditions themselves are closely related to chronic conditions in the Dartmouth Atlas, and the conditions comprised a substantial portion of all admissions in the hospitals studied (11% during 1999–2003 and 10% during 2004–2008).
We identified all admissions during 1999–2003 and 2004–2008 based on de-identified discharge records from the California Office of Statewide Health Planning and Development. These de-identified data were determined to be exempt from human-subjects review by the institutional review board at the RAND Corporation. In addition to a hospital ID, each discharge record included patient age, gender, admission year and quarter, International Classification of Disease Version 9 (ICD-9) codes for principal and secondary diagnoses and procedures, disposition (e.g., in-hospital death), charges, and 5-digit zip-code of residence. Following prior research(10), we linked each discharge record to patient zip-code level socio-demographic data from the 2000 Census, including: median household income, average Social Security income, percent poor, percent employed, percent with less than a high-school education, percent Hispanic, percent single, percent urban, percent elderly, percent elderly living in institutions, and percent of the non-institutionalized elderly with various disabilities. We then created diagnosis-specific patient samples for each hospital from ICD-9 discharge codes, according to the criteria of the AHRQ Inpatient Quality Indicators (Version 3.2, AHRQ, Rockville, Maryland). Patients admitted with AMI included transfers from other hospitals; our results were unchanged when transfers were excluded.
Inpatient spending
For 1999–2003, we took average hospital spending from the 2008 Dartmouth Atlas of Health Care.(11) This edition tracked spending in the last two years of life among fee-for-service Medicare patients with at least 1 of 9 severe chronic illnesses. Because patients at the end of life are arguably similar in the overall severity of illness, hospital spending measures that focus on end-of-life spending are more closely related to a hospital’s overall approach to spending and care rather than to the severity of its patients’ illnesses.(2, 11) The Dartmouth Atlas calculates hospital spending by assigning patients to the hospital at which most inpatient care was received.(11, 12) The measure includes reimbursements to the hospital and physicians and is adjusted for age, sex, race and primary chronic diagnosis; it is not disease-specific. In an Appendix, we examined the relationship between inpatient mortality and a surrogate measure of end of life hospital care based on the number of days a patient spent in the hospital and the number of inpatient physician visits received over the last two years of life (Dartmouth Hospital Care Intensity index).(11) By focusing on specific aspects of care rather than spending, this measure is not directly affected by geographic variation in price adjustments and Medicare disproportionate share payments. (11, 13, 14)
For the period 2004–2008, Dartmouth hospital spending estimates were unavailable. We therefore used hospital charges to compute disease-specific median hospital spending for patients admitted with one of six diagnoses who died while hospitalized. Because patients could not be linked across hospital admissions, costs were from the final hospitalization rather than total costs for these decedents in the last two years of life. We assumed unmeasured severity of illness to be comparable among patients who died while hospitalized, acknowledging that this is an imperfect way to adjust for mortality risk—particularly if sicker patients migrate towards intensive tertiary care hospitals. We used hospital-specific cost-to-charge ratios to convert hospital charges to costs. Hospital spending for the period 2004–2008 was therefore disease-specific, while spending during 1999–2003 was not. For both 1999–2003 and 2004–2008, we converted spending to 2001 dollars using the producer price index for general medical and surgical hospitals.
Other controls
We linked patient discharges to hospital- and region-level data including: hospital size, teaching status(10) (reported in the American Hospital Association’s Annual Survey(15)), quartile of discharge volume by condition(10), and quartile of managed-care penetration (based on hospital discharges) in the Dartmouth hospital referral region.(1, 10)
Analysis
For each diagnosis in each time period, we estimated patient-level logistic models of the following form:
Where:
Deathi,h = Indicator for death of patient i in hospital h
pred_mortalityi = AHRQ patient-level predicted mortality risk
spendingh = Hospital spending in hospital h
Spending varied at the hospital level (spendingh) and was divided into quintiles(10); we considered linear and quadratic specifications in sensitivity analysis. For 1999–2003, hospital spending (from Dartmouth Atlas) was not disease-specific, whereas it was for 2004–2008.
For patients admitted with each disease, we accounted for underlying health risks affecting inpatient mortality by applying risk parameters from a validated AHRQ risk-adjustment tool.(7) The AHRQ risk-parameters are estimated from national discharge data and can be applied to other discharge data to predict diagnosis-specific inpatient mortality for each patient. We applied the AHRQ risk parameters to each patient in the California discharge data to obtain patient-level predicted mortality (pred_mortalityi) based on a patient’s age category (e.g., 55–59), gender (interacted with age), and relevant diagnoses and procedure codes for the admitting diagnosis. The advantage of applying AHRQ’s risk parameters (rather than directly estimating them from the California data) was that the AHRQ model estimated risk parameters from nationally representative data. In addition to adjusting for predicted mortality, we adjusted for the number of Charlson-Deyo co-morbidities(10, 16), zip code level-socio-demographic factors based on zip code of residence(10), and year of discharge. Hospital and regional factors were described earlier. A sensitivity analysis used indicator variables for hospital referral regions to allow for geographic differences in physician practice patterns that could affect spending as well as inpatient mortality(17, 18); this analysis also controls for regional differences in diagnostic practices.(19) STATA version 11 (STATA Corp, College Station, Texas) was used for statistical analyses and the 95% CI reflects 0.025 in each tail, or P ≤.05.
We predicted for each diagnosis and time period the number of lives saved if all patients in the sample had been admitted to hospitals in the top spending quintile versus the bottom.(20) Lives saved were calculated by multiplying the total number of admissions to hospitals studied by the absolute difference in predicted inpatient mortality between hospitals in the first and fifth quintiles of spending.
We also explored whether hospital size or geography (Southern California vs. rest of state) modified the association between hospital spending and inpatient mortality. Southern California was defined as Imperial, Los Angeles, Riverside, Santa Barbara, San Bernardino, San Diego, and Ventura counties. We dichotomized hospital size into greater or less than the median number of hospital beds (220 in our sample) in 2001 financial reports. We did not examine effect modification by hospital teaching status as all but one teaching hospital were in the top two quintiles of spending.
Because this study was observational, the results could reflect unmeasured confounders. We conducted a sensitivity analysis to assess the degree of confounding needed to eliminate the estimated association between hospital spending and inpatient mortality. We assumed that (a) the unmeasured confounder is binary and hospital-specific; (b) is independent of measured confounders; and (c) there is no interaction between the unmeasured confounder and spending. We used a log-linear approximation to the logistic model.(21)
Missing data and multiple imputation
A total of 1,373,137 patients over 1999–2003 met the sample inclusion criteria (1,307,430 over 2004–2008). For 1999–2003, we excluded 108 of these patients due to missing or invalid disposition codes, and another 55,414 patients (4.0% of total) with unreported or unmatched zip codes. For 2004–2008, we excluded 69,581 patients for the preceding reasons, and another 9,401 patients for whom hospital costs were unavailable (due to missing or invalid charges or cost-to-charge ratios).
To prevent identification, some discharge records masked patient characteristics related to sample inclusion criteria or predicted mortality. Age, gender or admission quarter were masked for 80,307 patients with 1 of the 6 conditions studied over 1999–2003 (133,814 over 2004–2008). For each condition and analysis period, we created 10 independent data sets in which masked characteristics were imputed based on in-hospital death, Charlson-Deyo co-morbidity index, hospital ID, admission year, and (where available) age, gender and admission quarter.(22) Standard methods were used to combine analysis results across the imputed data sets.(23)
Role of the funding source
This research was sponsored by the National Institute of Aging and the Bing Center for Health Economics at the RAND Corporation. The design, conduct, analysis, interpretation, and presentation of the data are the sole responsibility of the investigators.
RESULTS
Table 1 reports summary statistics by condition for patients during 1999–2003 (2004–2008 data available in the Appendix). The number of patients was substantial, ranging from 98,208 (hip fracture) to 345,449 (pneumonia) patients. Average age ranged from 72.5y (AMI) to 81.4y (hip fracture). Observed mortality ranged from 2.97% for gastrointestinal hemorrhage, 10.25% for AMI, and 11.71% for stroke. About one out of ten patients were admitted to teaching hospitals and roughly 70% were treated at hospitals with greater than the median number of beds. Admissions were approximately evenly distributed between hospitals in Southern California and the rest of the state.
Table 1.
Summary statistics for patients admitted to California hospitals during 1999–2003, by presenting diagnosis
| AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia | |
|---|---|---|---|---|---|---|
| No. of patients | 184,691 | 335,278 | 189,614 | 164,483 | 98,208 | 345,449 |
| Observed inpatient mortality, % | 10.25 (30.33) | 4.77 (21.31) | 11.71 (32.15) | 3.23 (17.69) | 2.97 (16.97) | 7.91 (26.98) |
| Age (years) | 72.5 (12.5) | 74.7 (11.9) | 74.8 (11.7) | 72.7 (14.2) | 81.4 (4.9) | 73.5 (14.1) |
| Female, % | 41.4 (49.3) | 54.8 (49.8) | 56.3 (49.6) | 50.0 (50.0) | 74.8 (43.4) | 54.0 (49.8) |
| No. of Charlson-Deyo index co- morbidities | 2.2 (1.2) | 2.4 (1.1) | 2.2 (1.1) | 1.4 (1.2) | 1.0 (1.0) | 1.5 (1.1) |
| Medicare fee-for-service, % | 40.5 (49.1) | 55.3 (49.7) | 48.8 (50.0) | 47.0 (49.9) | 63.2 (48.2) | 52.9 (49.9) |
| Treated at teaching hospital,% | 10.3 (30.5) | 9.7 (29.6) | 11.5 (31.9) | 9.9 (29.9) | 7.7 (26.7) | 9.5 (29.3) |
| Treated in large hospital*, % | 79.3 (40.5) | 71.6 (45.1) | 72.8 (44.5) | 69.4 (46.1) | 69.0 (46.2) | 66.7 (47.1) |
| Treated in southern California, % | 56.4 (49.6) | 59.3 (49.1) | 56.7 (49.6) | 55.6 (49.7) | 55.4 (49.7) | 55.7 (49.7) |
| Zip code demographics | ||||||
| Median household income, $ | 49306 (18771) | 47290 (17992) | 49176 (19084) | 49025 (19056) | 50727 (19791) | 47450 (18160) |
| Below poverty line, % | 13.6 (8.4) | 14.8 (9.1) | 13.9 (8.7) | 13.9 (8.7) | 12.7 (7.9) | 14.5 (8.8) |
| Avg. Social security income, $ | 11252 (1323) | 11071 (1375) | 11217 (1382) | 11205 (1376) | 11485 (1317) | 11132 (1336) |
| Urban, % | 93.6 (16.9) | 94.6 (15.2) | 94.1 (16.3) | 93.9 (16.5) | 93.3 (16.9) | 93.4 (17.0) |
| Hispanic, % | 28.8 (21.2) | 31.4 (22.3) | 29.3 (21.9) | 29.3 (21.8) | 25.7 (20.0) | 30.0 (21.8) |
| Single, % | 44.9 (7.8) | 45.8 (7.7) | 45.4 (7.8) | 45.4 (7.9) | 44.9 (7.8) | 45.5 (7.8) |
| Less than high school, % | 22.6 (14.8) | 24.8 (15.7) | 23.2 (15.4) | 23.2 (15.3) | 20.3 (13.8) | 24.1 (15.2) |
| Employed, % | 56.8 (8.5) | 56.1 (8.4) | 56.7 (8.4) | 56.7 (8.5) | 57.1 (8.4) | 56.2 (8.5) |
| Zip code health characteristics among population 65 and older | ||||||
| Institutionalized, % | 3.3 (3.8) | 3.4 (3.9) | 3.4 (3.8) | 3.4 (3.9) | 3.7 (4.0) | 3.6 (4.0) |
| Physical disability, % | 29.2 (6.0) | 29.9 (6.0) | 29.2 (6.1) | 29.2 (6.1) | 28.4 (5.9) | 29.7 (6.0) |
| Mental disability, % | 12.6 (4.4) | 13.2 (4.6) | 12.7 (4.4) | 12.7 (4.4) | 12.1 (4.2) | 12.9 (4.4) |
| Sensory disability, % | 14.8 (3.4) | 15.0 (3.3) | 14.8 (3.4) | 14.8 (3.4) | 14.6 (3.3) | 15.0 (3.4) |
| Self-care disability, % | 10.2 (3.8) | 10.7 (4.0) | 10.3 (3.8) | 10.3 (3.8) | 9.9 (3.6) | 10.5 (3.8) |
| Home-bound disability (%) | 21.3 (5.6) | 22.2 (5.8) | 21.5 (5.7) | 21.5 (5.7) | 20.6 (5.4) | 21.8 (5.6) |
Notes: Based on California inpatient discharge records from the California Office of Statewide Health Planning and Development (OSHPD). Standard deviations are in parentheses. Age is based on discharges with exact (non-categorical) reporting.
Large hospital was defined as having greater than the median number of hospital beds as reported in 2001 financial reports to OSHPD. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
Table 2 presents hospital spending by quintile. During 1999–2003, hospital spending on patients admitted to the bottom quintile of hospitals averaged $25,568 (in 2001 dollars) over the final two years of life, compared to $58,635 for those admitted to the top quintile. For 2004–2008, Table 2 presents median spending in each hospital spending quintile, by disease. Spending was calculated among patients who died while hospitalized. Median spending in the first quintile of hospitals ranged from $4,555 (stroke) to $7,982 (hip fracture). Median spending in the top quintile ranged from $13,945 (stroke) to $28,546 (hip fracture). Because 2004–2008 hospital spending levels were not directly comparable to 1999–2003 levels – since hospital spending in 2004–2008 was computed for the terminal hospital stay of decedents, rather than all hospital stays over the final two years of life – we divided hospitals into spending quintiles when analyzing the association between inpatient mortality and hospital spending.
Table 2.
Hospital spending by quintile, 208 California hospitals in 1999–2003 and 2004–2008
| Quintile | 1999- 2003
|
2004–2008
|
|||||
|---|---|---|---|---|---|---|---|
| AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia | ||
| 1 | $25,658 | $5,168 | $5,090 | $4,555 | $4,859 | $7,982 | $5,556 |
| 2 | $30,844 | $7,107 | $7,174 | $6,306 | $7,627 | $12,215 | $7,878 |
| 3 | $36,288 | $9,985 | $9,097 | $7,638 | $9,431 | $14,739 | $9,815 |
| 4 | $43,228 | $13,346 | $11,383 | $9,388 | $12,374 | $18,962 | $12,437 |
| 5 | $58,635 | $21,072 | $18,984 | $13,945 | $21,762 | $28,546 | $20,789 |
Notes: Hospital spending is in 2001 dollars. Spending during 1999–2003 was derived from the most recent Dartmouth Atlas, which does not break down spending by disease. Hospital spending during 2004–2008 was calculated using the terminal hospital stays of patients admitted between 2004 and 2008. Hospital spending levels from 2004–2008 are not directly comparable to 1999–2003 levels because hospital spending in 2004–2008 is computed from the terminal hospital stay of patients, rather than all hospital stays over the final two years of life. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
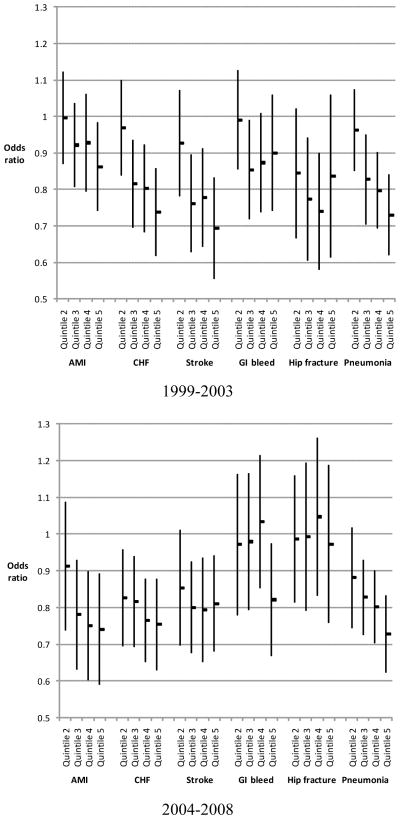
Table 3 presents the risk-adjusted odds-ratio (OR) of inpatient mortality by hospital spending quintile for each medical condition (OR measured relative to the bottom quintile of hospital spending). The OR was adjusted for predicted patient mortality and a set of patient and hospital/region factors. The top and bottom panels display ORs for 1999–2003 and 2004–2008, respectively. Figure 1 in the Appendix depicts these results graphically.
Table 3.
Risk-adjusted odds-ratio of inpatient mortality by hospital spending quintile for six major medical conditions, 1999–2003 and 2004–2008
| Quintile of hospital spending | AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia |
|---|---|---|---|---|---|---|
| 1999–2003 | ||||||
|
| ||||||
| 2 | 0.996 [0.870–1.122] | 0.969 [0.838–1.099] | 0.927 [0.782–1.071] | 0.990 [0.855–1.125] | 0.844 [0.667–1.022] | 0.962 [0.850–1.075] |
| 3 | 0.921 [0.806–1.037] | 0.816 [0.695–0.936] | 0.761 [0.628–0.895] | 0.854 [0.719–0.989] | 0.773 [0.605–0.941] | 0.827 [0.704–0.951] |
| 4 | 0.928 [0.794–1.062] | 0.802 [0.682–0.922] | 0.777 [0.642–0.912] | 0.873 [0.738–1.009] | 0.740 [0.581–0.898] | 0.797 [0.693–0.901] |
| 5 | 0.862 [0.742–0.983] | 0.737 [0.617–0.857] | 0.693 [0.555–0.831] | 0.900 [0.742–1.058] | 0.836 [0.613–1.058] | 0.729 [0.619–0.840] |
| 2004–2008 | ||||||
|
| ||||||
| 2 | 0.912 [0.738–1.086] | 0.827 [0.696–0.958] | 0.854 [0.697–1.011] | 0.972 [0.780–1.163] | 0.987 [0.813–1.160] | 0.881 [0.745–1.018] |
| 3 | 0.781 [0.632–0.929] | 0.816 [0.694–0.939] | 0.800 [0.676–0.925] | 0.979 [0.794–1.165] | 0.992 [0.791–1.194] | 0.828 [0.726–0.929] |
| 4 | 0.750 [0.602–0.898] | 0.766 [0.653–0.878] | 0.793 [0.651–0.935] | 1.034 [0.854–1.214] | 1.047 [0.833–1.261] | 0.802 [0.703–0.900] |
| 5 | 0.741 [0.590–0.891] | 0.755 [0.630–0.879] | 0.811 [0.680–0.942] | 0.821 [0.668–0.975] | 0.973 [0.758–1.188] | 0.729 [0.624–0.834] |
Notes: Odds ratios of inpatient mortality for a given hospital spending quintile are calculated with respect to the lowest quintile. 95% confidence interval in brackets. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
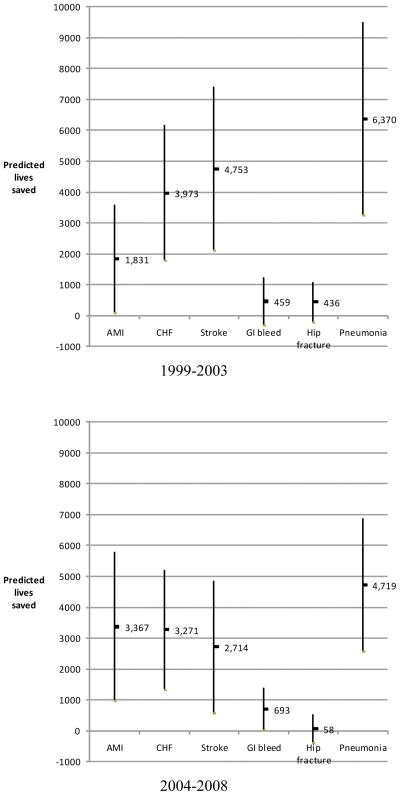
Figure 1. Predicted lives saved if all patients were treated in hospitals in the top spending quintile vs. the bottom spending quintile.
Notes: Vertical bars represent 95% confidence intervals around the predicted lives saved (boxes). Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
In both 1999–2003 and 2004–2008, adjusted inpatient mortality was negatively associated with hospital spending for all six diagnoses. During 1999–2003, patients admitted with AMI in the fifth quintile of Dartmouth hospital spending had lower mortality than those admitted to hospitals in the first quintile (OR of inpatient mortality 0.862, 95% CI 0.742–0.983). Increases in hospital spending from one quintile to the next tended to be associated with subsequent reductions in mortality among patients admitted for AMI. For patients admitted in 1999–2003 with primary diagnoses of CHF, stroke, gastrointestinal hemorrhage, hip fracture, or pneumonia, those admitted to hospitals in the fifth quintile of spending were less likely to die inpatient compared to patients in the first quintile (ORs ranging from 0.693 to 0.900). With the exception of gastrointestinal hemorrhage and hip fracture, these associations were statistically significant at the p < 0.05 level. A similar pattern held during 2004–2008, with patients in the fifth quintile of disease-specific hospital spending also less likely to die than those in the lowest quintile (ORs across diseases ranging from 0.729 to 0.973). Among these, only hip fracture was not statistically significant at p < 0.05. For both 1999–2003 and 2004–2008, increases in hospital spending across quintiles were generally associated with reductions in inpatient mortality (Table 3 and Appendix Figure 1).
Figure 1 shows the predicted number of inpatient lives that would be saved if all patients admitted to our sample of hospitals had been admitted to the top-spending quintile of hospitals rather than to the lowest. For patients presenting with AMI, 1,831 lives might have been saved over the five-year period 1999–2003, a 9% reduction in mortality; for AMI patients over 2004–2008, we estimate the number of potential lives saved to be 3,367, a 19% reduction. For CHF, stroke, and pneumonia, the predicted number of lives saved was similar to AMI, on the order of 2,500 to 6,500 lives during both 1999–2003 and 2004–2008. For patients admitted with gastrointestinal hemorrhage and hip fracture during 1999–2003, our model predicted that approximately 500 lives might have been saved, respectively, if all patients with these diseases had been admitted to the top quintile of hospital spending compared with the bottom.
Effect of hospital size and geography
We also examined how hospital size and geography affected the estimated relationship between hospital spending and inpatient mortality during 1999–2003 (Table 4). For each disease and sub-group comparison (e.g. Southern vs. rest of California), we report the OR of inpatient mortality among patients admitted to hospitals in the fifth spending quintile versus the first. The association between hospital spending and inpatient mortality did not vary statistically significantly by geography or hospital size. For example, the OR of inpatient mortality for patients admitted with CHF to hospitals in the fifth quintile of spending (relative to the first quintile) was 0.854 (95% CI 0.597–1.111) in Southern California, versus 0.797 (95% CI 0.645–0.950) in the rest of the state (p-value 0.707). Similar results held for the other diseases considered. The OR of inpatient CHF mortality among hospitals in the fifth quintile of spending (relative to the first) was 0.764 (95% CI 0.599 – 0.928) for the largest 50% of hospitals, versus 0.789 (95% CI 0.640 – 0.938) for the bottom 50% (p- value 0.794).
Table 4.
Impact of geography and hospital size on the association between hospital spending and inpatient mortality, 1999–2003
| Odds ratio of inpatient mortality between highest and lowest quintile of hospital spending [95% Confidence Interval] | ||||||
|---|---|---|---|---|---|---|
| AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia | |
| Region | ||||||
| Southern California | 0.979 [0.619–1.339] | 0.854 [0.597–1.111] | 0.793 [0.512–1.074] | 0.809 [0.555–1.063] | 0.927 [0.612–1.243] | 0.738 [0.556–0.919] |
| Rest of California | 0.821 [0.701–0.941] | 0.797 [0.645–0.950] | 0.831 [0.696–0.966] | 1.035 [0.841–1.230] | 0.966 [0.697–1.236] | 0.818 [0.674–0.961] |
| p-value | 0.390 | 0.707 | 0.806 | 0.177 | 0.847 | 0.503 |
| Hospital size | ||||||
| Larger than median hospital | 0.863 [0.701–1.026] | 0.764 [0.599–0.928] | 0.698 [0.507–0.890] | 0.964 [0.765–1.164] | 0.778 [0.454–1.101] | 0.725 [0.577–0.874] |
| Smaller than median hospital | 0.955 [0.737–1.173] | 0.789 [0.640–0.938] | 0.757 [0.570–0.945] | 0.887 [0.594–1.180] | 1.007 [0.677–1.338] | 0.775 [0.596–0.955] |
| p-value | 0.479 | 0.794 | 0.634 | 0.660 | 0.291 | 0.646 |
Notes: Table examines whether geography and hospital size modify the association between hospital spending and inpatient mortality. Odds ratios for geography and hospital size compare inpatient mortality spending between the highest and lowest quintile of hospital spending; e.g. odds ratio < 1 implies adjusted inpatient mortality was lower in hospitals in the top spending quintile compared to the lowest. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
Sensitivity analysis
Results were similar when we used (a) a surrogate measure of hospital spending; (b) linear and quadratic specifications of hospital spending; and (c) indicator variables for hospital regions. In terms of confounding, the true OR of inpatient mortality with respect to the top spending quintile would become statistically indistinguishable from one for AMI patients over 1999–2003, if there were an unmeasured binary variable with an OR of inpatient mortality of 0.85, a 20% probability of occurring at a hospital in the top spending quintile, and a 10% probability of occurring at a bottom-quintile hospital. For pneumonia patients, the true OR would be significantly less than one even with a 100% probability of the binary variable occurring at top-spending hospitals.
DISCUSSION
We examined the association between hospital spending and inpatient mortality in 208 California hospitals. We found that greater hospital spending was associated with lower inpatient mortality for a variety of major acute medical conditions. Our findings suggest that while greater overall medical spending in the U.S. is not associated with better quality of care or better health outcomes(1, 2, 10), specific types of medical spending – e.g., acute-care hospital spending – may be efficacious. Our results, along with prior studies(8, 24), highlight that intensive spending in hospitals may be associated with lower mortality despite bearing no or even negative relationship to standard measures of process quality (e.g. aspirin use at admission for patients presenting with acute myocardial infarction).(14, 25) Reported process measures may simply do a poor job of explaining variation in hospital mortality.(26, 27)
While our analysis demonstrates that intensive spending by hospitals is associated with lower mortality, it does not identify the specific costly interventions that high-spending hospitals undertake to achieve this mortality benefit. Prior work suggests that patients at moderate and high risk of dying have lower mortality when admitted to hospitals in which larger fractions of patients spend time in the ICU, undergo mechanical ventilation, or receive dialysis.(8) These interventions likely only proxy for the additional costly diagnostic work-up and management that higher spending hospitals may do. For the admitting diagnoses we consider, these additional interventions may include early and more frequent coronary revascularization for AMIs and upper and lower endoscopies for gastrointestinal hemorrhages.
Our study has additional limitations. Although we measured hospital spending among patients at the end of life, adjusted for patient co-morbidities, and accounted for patient zip-code socio-demographics, hard-to-measure aspects of health are still a concern.(7) Patients admitted to higher-spending hospitals may be healthier than predicted, either because of where those hospitals are located or because higher-spending hospitals have lower thresholds for hospital admission. Both of these would bias us towards finding an association between higher hospital spending and lower inpatient mortality. While for diagnoses such as CHF and pneumonia, higher-spending hospitals may less discriminately admit patients to the hospital instead of managing these illnesses on an outpatient basis, acute events such as stroke and AMI would presumably be less affected. We find equally strong relationships between hospital spending and mortality across the range of disease acuity we consider.
An additional bias arises if higher-spending hospitals diagnose more conditions, or simply attach more diagnoses to discharge records.(19) Adjusting for the number of diagnoses at discharge would bias us towards finding a negative association between hospital spending and inpatient mortality. Our results were unchanged, however, when the number of co-morbidities was excluded from the analysis. Despite the potential biases in favor a negative association between spending and mortality, it is important to recognize that higher-spending hospitals may also spend more because their patients are sicker than our mortality risk adjustments would predict. In this case, we would understate the efficacy of hospital spending.
Our findings should be interpreted with caution. Higher hospital spending on these six major medical conditions may not produce better health outcomes outside of California, although we know of no reason to doubt it. Furthermore, hospital spending would not necessarily be cost effective, because alternative interventions might enhance population health at lower cost. The cost effectiveness of hospital spending depends on its impact on inpatient and post-discharge mortality, the latter of which we were unable to assess with our data. Hence, important questions about the efficacy and value of hospital care remain to be asked and answered.
Acknowledgments
Funding support: Dr. Romley received support from 1R03AG031990-A1. Dr. Goldman was supported by the Roybal Center for Health Policy Simulation (P30AG024968)
Role of the sponsor: The design, conduct, analysis, interpretation, and presentation of the data are the responsibility of the investigators, with no involvement from the funding source.
Appendix Figure 1.
Risk-adjusted odds-ratio of inpatient mortality by hospital spending quintile for six major medical conditions, 1999–2003 and 2004–2008
Notes: Odds ratios of inpatient mortality for a given hospital spending quintile are calculated with respect to the lowest quintile. Vertical bars represent 95% confidence intervals around the predicted lives saved (boxes).Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
Appendix Table 1.
Summary statistics for patients admitted to California hospitals during 2004–2008, by presenting diagnosis
| AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia | |
|---|---|---|---|---|---|---|
| No. of patients | 169,537 | 324,371 | 172,471 | 170,301 | 88,154 | 302,795 |
| Observed inpatient mortality, % | 8.25 (27.52) | 3.88 (19.32) | 11.43 (31.82) | 2.70 (16.20) | 2.83 (16.58) | 5.46 (22.73) |
| Age (years) | 72.0 (12.9) | 74.1 (12.9) | 74.0 (12.6) | 71.9 (14.6) | 81.6 (5.0) | 73.2 (14.3) |
| Female, % | 40.8 (49.1) | 52.2 (50.0) | 54.2 (49.8) | 50.3 (50.0) | 73.7 (44.1) | 53.3 (49.9) |
| No. of Charlson-Deyo index co- morbidities | 2.4 (1.3) | 2.6 (1.2) | 2.3 (1.2) | 1.6 (1.3) | 1.1 (1.1) | 1.6 (1.2) |
| Medicare fee-for-service, % | 41.7 (49.3) | 58.1 (49.3) | 50.6 (50.0) | 49.9 (50.0) | 68.5 (46.5) | 56.9 (49.5) |
| Treated at teaching hospital,% | 10.1 (30.1) | 10.1 (30.1) | 12.9 (33.5) | 9.6 (29.4) | 7.8 (26.9) | 9.3 (29.0) |
| Treated in large hospital*, % | 78.2 (41.3) | 71.0 (45.4) | 73.8 (44.0) | 68.9 (46.3) | 68.1 (46.6) | 65.6 (47.5) |
| Treated in southern California, % | 55.8 (49.7) | 58.9 (49.2) | 56.9 (49.5) | 55.9 (49.7) | 55.3 (49.7) | 55.1 (49.7) |
| Zip code demographics | ||||||
| Median household income, $ | 49183 (18809) | 47040 (18063) | 49072 (19085) | 48790 (18919) | 51077 (19963) | 47594 (18324) |
| Below poverty line, % | 13.8 (8.6) | 15.1 (9.2) | 14.1 (8.8) | 14.2 (8.8) | 12.6 (7.9) | 14.6 (8.9) |
| Avg. Social security income, $ | 11227 (1339) | 11028 (1386) | 11193 (1387) | 11178 (1376) | 11491 (1334) | 11130 (1347) |
| Urban, % | 93.0 (17.7) | 94.4 (15.4) | 93.8 (16.4) | 93.6 (16.6) | 93.0 (17.2) | 93.2 (17.0) |
| Hispanic, % | 29.0 (21.3) | 32.0 (22.5) | 29.8 (22.1) | 29.9 (22.0) | 25.7 (20.3) | 30.2 (21.7) |
| Single, % | 44.5 (7.7) | 45.6 (7.7) | 45.1 (7.8) | 45.1 (7.8) | 44.5 (7.9) | 45.1 (7.8) |
| Less than high school, % | 22.9 (15.0) | 25.3 (16.0) | 23.5 (15.6) | 23.6 (15.5) | 20.3 (14.0) | 24.2 (15.3) |
| Employed, % | 56.7 (8.7) | 55.9 (8.5) | 56.6 (8.4) | 56.5 (8.5) | 57.2 (8.5) | 56.2 (8.5) |
| Zip code health characteristics among population 65 and older | ||||||
| Institutionalized, % | 3.3 (3.9) | 3.4 (3.9) | 3.3 (3.9) | 3.4 (4.0) | 3.6 (4.0) | 3.5 (4.0) |
| Physical disability, % | 29.2 (6.1) | 29.9 (6.1) | 29.2 (6.1) | 29.3 (6.1) | 28.2 (6.0) | 29.6 (6.1) |
| Mental disability, % | 12.6 (4.4) | 13.2 (4.6) | 12.7 (4.4) | 12.7 (4.4) | 12.0 (4.2) | 12.8 (4.4) |
| Sensory disability, % | 14.8 (3.5) | 15.0 (3.4) | 14.8 (3.4) | 14.8 (3.4) | 14.5 (3.4) | 15.0 (3.5) |
| Self-care disability, % | 10.2 (3.8) | 10.7 (4.0) | 10.3 (3.8) | 10.3 (3.8) | 9.8 (3.6) | 10.4 (3.8) |
| Home-bound disability (%) | 21.3 (5.7) | 22.2 (5.8) | 21.5 (5.7) | 21.5 (5.7) | 20.4 (5.5) | 21.7 (5.7) |
Notes: Based on California inpatient discharge records from the California Office of Statewide Health Planning and Development (OSHPD). Standard deviations are in parentheses. Age is based on discharges with exact (non-categorical) reporting.
Large hospital was defined as having greater than the median number of hospital beds as reported in 2001 financial reports to OSHPD. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
Appendix Table 2.
Risk-adjusted odds-ratio of inpatient mortality by quintile of Hospital Care Intensity index for six major medical conditions, 1999–2003
| Quintile of hospital spending | AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia |
|---|---|---|---|---|---|---|
| 2 | 0.964 [0.855–1.074] | 1.014 [0.862–1.166] | 1.054 [0.905–1.203] | 1.046 [0.900–1.193] | 1.173 [0.946–1.400] | 1.053 [0.924–1.182] |
| 3 | 0.942 [0.844–1.040] | 0.893 [0.765–1.022] | 0.851 [0.736–0.966] | 0.953 [0.814–1.091] | 0.937 [0.787–1.087] | 0.900 [0.793–1.008] |
| 4 | 0.933 [0.839–1.026] | 0.836 [0.722–0.949] | 0.760 [0.657–0.863] | 0.903 [0.759–1.046] | 0.816 [0.658–0.974] | 0.877 [0.782–0.972] |
| 5 | 0.906 [0.788–1.024] | 0.754 [0.640–0.868] | 0.671 [0.569–0.773] | 0.926 [0.775–1.078] | 0.849 [0.670–1.029] | 0.762 [0.675–0.849] |
Notes: Table examines the association between inpatient mortality and a surrogate measure of spending, the Hospital Care Intensity index produced by the Dartmouth Atlas. Results shown here can be compared to the top panel in Table 3. 95% confidence interval in brackets. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
Appendix Table 3.
Predicted lives saved if all patients were treated in hospitals in the top spending quintile vs. the bottom spending quintile, by specification of hospital spending, 1999–2003
| Specification of hospital spending | AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia |
|---|---|---|---|---|---|---|
| Quintile | 1,831 | 3,973 | 4,753 | 459 | 436 | 6,370 |
| Linear | 6,627 | 3,080 | 5,565 | 1,762 | 751 | 5,824 |
Notes: Table provides a specification check on spending. The first row of results shows predicted lives saved when spending is divided into quintiles; the second row shows results when spending enters the model linearly. Linear term was always statistically significant; in quadratic specification (not reported), the square of spending was significant for only one condition (hip fracture). For the purpose of prediction, bottom quintile spending in the linear specification was defined to equal mean spending in the bottom quintile; high spending was defined similarly. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
Appendix Table 4.
Risk-adjusted odds-ratio of inpatient mortality by hospital spending quintile for six major medical conditions, according to inclusion of indicator variables for hospital regions in addition to baseline factors, 1999–2003
| Quintile of hospital spending | AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia |
|---|---|---|---|---|---|---|
| Baseline factors only | ||||||
| 2 | 0.996 [0.870–1.122] | 0.969 [0.838–1.099] | 0.927 [0.782–1.071] | 0.990 [0.855–1.125] | 0.844 [0.667–1.022] | 0.962 [0.850–1.075] |
| 3 | 0.921 [0.806–1.037] | 0.816 [0.695–0.936] | 0.761 [0.628–0.895] | 0.854 [0.719–0.989] | 0.773 [0.605–0.941] | 0.827 [0.704–0.951] |
| 4 | 0.928 [0.794–1.062] | 0.802 [0.682–0.922] | 0.777 [0.642–0.912] | 0.873 [0.738–1.009] | 0.740 [0.581–0.898] | 0.797 [0.693–0.901] |
| 5 | 0.862 [0.742–0.983] | 0.737 [0.617–0.857] | 0.693 [0.555–0.831] | 0.900 [0.742–1.058] | 0.836 [0.613–1.058] | 0.729 [0.619–0.840] |
| Including indicator variables for hospital regions | ||||||
| 2 | 1.042 [0.913–1.171] | 1.010 [0.880–1.140] | 0.912 [0.783–1.041] | 1.003 [0.859–1.147] | 0.860 [0.682–1.038] | 0.958 [0.837–1.078] |
| 3 | 0.984 [0.833–1.135] | 0.903 [0.765–1.040] | 0.798 [0.669–0.927] | 0.929 [0.764–1.093] | 0.809 [0.609–1.008] | 0.853 [0.726–0.980] |
| 4 | 0.991 [0.830–1.152] | 0.880 [0.735–1.025] | 0.811 [0.668–0.955] | 0.911 [0.752–1.070] | 0.762 [0.579–0.946] | 0.823 [0.702–0.943] |
| 5 | 0.927 [0.772–1.083] | 0.804 [0.662–0.946] | 0.741 [0.604–0.878] | 0.942 [0.762–1.121] | 0.810 [0.586–1.034] | 0.745 [0.624–0.865] |
Notes: This table explores whether including indicators for hospital referral region impact the estimated association between hospital spending and inpatient mortality. The top panel reports odds ratios of inpatient mortality from the baseline specification which adjusts for predicted mortality and a set of patient and hospital/region factors. The bottom panel reports odds ratios when indicators for hospital referral region are included as well. Hospital regions were defined by Dartmouth hospital referral regions. 95% confidence interval in brackets. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
Appendix Table 5.
Risk-adjusted odds-ratio of inpatient mortality by hospital spending quintile for six major medical conditions, according to inclusion of number of Charlson-Deyo co-morbidities, 1999–2003
| Quintile of hospital spending | AMI | CHF | Stroke | GI bleed | Hip fracture | Pneumonia |
|---|---|---|---|---|---|---|
| Baseline | ||||||
| 2 | 0.996 [0.870–1.122] | 0.969 [0.838–1.099] | 0.927 [0.782–1.071] | 0.990 [0.855–1.125] | 0.844 [0.667–1.022] | 0.962 [0.850–1.075] |
| 3 | 0.921 [0.806–1.037] | 0.816 [0.695–0.936] | 0.761 [0.628–0.895] | 0.854 [0.719–0.989] | 0.773 [0.605–0.941] | 0.827 [0.704–0.951] |
| 4 | 0.928 [0.794–1.062] | 0.802 [0.682–0.922] | 0.777 [0.642–0.912] | 0.873 [0.738–1.009] | 0.740 [0.581–0.898] | 0.797 [0.693–0.901] |
| 5 | 0.862 [0.742–0.983] | 0.737 [0.617–0.857] | 0.693 [0.555–0.831] | 0.900 [0.742–1.058] | 0.836 [0.613–1.058] | 0.729 [0.619–0.840] |
| Excluding number of Charlson-Deyo co-morbidities | ||||||
| 2 | 0.992 [0.864–1.119] | 0.973 [0.841–1.105] | 0.924 [0.779–1.069] | 0.979 [0.847–1.110] | 0.819 [0.654–0.984] | 0.961 [0.851–1.072] |
| 3 | 0.920 [0.805–1.035] | 0.825 [0.703–0.946] | 0.759 [0.626–0.893] | 0.857 [0.723–0.991] | 0.767 [0.604–0.929] | 0.828 [0.705–0.951] |
| 4 | 0.925 [0.792–1.059] | 0.810 [0.689–0.930] | 0.776 [0.641–0.911] | 0.873 [0.740–1.007] | 0.728 [0.578–0.877] | 0.800 [0.696–0.903] |
| 5 | 0.860 [0.739–0.981] | 0.747 [0.625–0.868] | 0.693 [0.554–0.832] | 0.908 [0.752–1.064] | 0.836 [0.608–1.064] | 0.731 [0.621–0.842] |
Notes: Table examines whether including the number of Charlson-Deyo co-morbidities impacts the estimated association between hospital spending and inpatient mortality. The top panel reports odds ratios of inpatient mortality from the baseline specification which adjusts for predicted mortality and a set of patient and hospital/region factors. The bottom panel reports odds ratios when the number of Charlson-Deyo co-morbidities is excluded. 95% confidence interval in brackets. Abbreviations: Acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal hemorrhage (GI bleed).
Footnotes
Author Contributions:
Study concept and design: John Romley, Anupam B. Jena, Dana Goldman
Acquisition of data: John Romley, Anupam B. Jena, Dana Goldman
Analysis and interpretation of data: John Romley, Anupam B. Jena, Dana Goldman
Drafting of manuscript: John Romley, Anupam B. Jena, Dana Goldman
Critical revision of the manuscript for important intellectual content: John Romley, Anupam B. Jena, Dana Goldman
Reproducible research statement: Statistical code: Available from Dr. Romley (romley@rand.org). Data set: Public-use discharge databases available from the California Office of Statewide Health Planning and Development.
Potential Conflicts of Interest: None disclosed.
Contributor Information
John A. Romley, Email: romley@sppd.usc.edu.
Anupam B. Jena, Email: jena.anupam@mgh.harvard.edu.
Dana P. Goldman, Email: dana.goldman@usc.edu.
References
- 1.Wennberg J, Cooper M. The Dartmouth atlas of health care. The Center for the Evaluative Clinical Sciences, Dartmouth Medical School, American Hospital Publishing; 1996. pp. 15–20. [Google Scholar]
- 2.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Annals of Internal Medicine. 2003;138(4):273. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 3.Fisher ES. Medical Care--Is More Always Better? New England Journal of Medicine. 2003;349(17):1665. doi: 10.1056/NEJMe038149. [DOI] [PubMed] [Google Scholar]
- 4.Bach PB. Reply to “Looking Back, Moving Forward”. N Engl J Med. 2010;362(7):574. doi: 10.1056/NEJMp1000448. [DOI] [PubMed] [Google Scholar]
- 5.Skinner J, Staiger D, Fisher ES. Looking Back, Moving Forward. N Engl J Med. 2010;362(7):569-a–74. doi: 10.1056/NEJMp1000448. [DOI] [PubMed] [Google Scholar]
- 6.Bach P. A Map to Bad Policy--Hospital Efficiency Measures in the Dartmouth Atlas. New England Journal of Medicine. 2010;362(7):569. doi: 10.1056/NEJMp0909947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.!!! INVALID CITATION !!!
- 8.Barnato AE, Chang CC, Farrell MH, Lave JR, Roberts MS, Angus DC. Is survival better at hospitals with higher “end-of-life” treatment intensity? Med Care. 48(2):125–32. doi: 10.1097/MLR.0b013e3181c161e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Quality and Research. Guide to Inpatient Quality Indicators. 2008. [Google Scholar]
- 10.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder E. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Annals of Internal Medicine. 2003;138(4):288. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 11.Wennberg J, Fisher E, Goodman D, Skinner J. Tracking the Care of Patients with Severe Chronic Illness-The Dartmouth Atlas of Health Care. 2008 [PubMed] [Google Scholar]
- 12.Wennberg JE, Fisher ES, Stukel TA, Sharp SM. Use Of Medicare Claims Data To Monitor Provider-Specific Performance Among Patients With Severe Chronic Illness. Health Aff. 2004 doi: 10.1377/hlthaff.var.5. hlthaff.var.5. [DOI] [PubMed] [Google Scholar]
- 13.Skinner J, Chandra A, Goodman D, Fisher ES. The elusive connection between health care spending and quality. Health Affairs. 2009;28(1):w119. doi: 10.1377/hlthaff.28.1.w119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yasaitis L, Fisher ES, Skinner JS, Chandra A. Hospital Quality And Intensity Of Spending: Is There An Association? Health Affairs. 2009;28(4):w566. doi: 10.1377/hlthaff.28.4.w566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Hospital Association. Annual Survey. Chicago, IL: Health Forum, LLC; 2001. [Google Scholar]
- 16.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 17.Chandra A, Staiger DO. Productivity Spillovers in Health Care: Evidence from the Treatment of Heart Attacks. Journal of Political Economy. 2007;115(1):103–40. doi: 10.1086/512249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinstein M, Skinner J. Comparative Effectiveness and Health Care Spending-- Implications for Reform. New England Journal of Medicine. 2010 doi: 10.1056/NEJMsb0911104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song Y, Skinner J, Bynum J, Sutherland J, Wennberg JE, Fisher ES. Regional variations in diagnostic practices. N Engl J Med. 363(1):45–53. doi: 10.1056/NEJMsa0910881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652– 9. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 21.Lin DY, Psaty BM, Kronmal RA. Assessing the Sensitivity of Regression Results to Unmeasured Confounders in Observational Studies. Biometrics. 1998;54(3):948–63. [PubMed] [Google Scholar]
- 22.van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Statistics in Medicine. 1999;18(6):681–94. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 23.Rubin DB. Multiple imputation for nonresponse in surveys. Hoboken, N.J: Wiley-Interscience; 2004. [Google Scholar]
- 24.Ong MK, Mangione CM, Romano PS, Zhou Q, Auerbach AD, Chun A, et al. Looking Forward, Looking Back: Assessing Variations in Hospital Resource Use and Outcomes for Elderly Patients With Heart Failure. Circulation: Cardiovascular Quality and Outcomes. 2009 doi: 10.1161/CIRCOUTCOMES.108.825612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wennberg JE, Fisher ES, Baker L, Sharp SM, Bronner KK. Evaluating the efficiency of California providers in caring for patients with chronic illnesses. Health Affairs. 2005;24(4):256–64. doi: 10.1377/hlthaff.w5.526. [DOI] [PubMed] [Google Scholar]
- 26.Bradley EH, Herrin J, Elbel B, McNamara RL, Magid DJ, Nallamothu BK, et al. Hospital quality for acute myocardial infarction: correlation among process measures and relationship with short-term mortality. JAMA. 2006;296(1):72. doi: 10.1001/jama.296.1.72. [DOI] [PubMed] [Google Scholar]
- 27.Werner RM, Bradlow ET. Relationship between Medicare’s hospital compare performance measures and mortality rates. JAMA. 2006;296(22):2694. doi: 10.1001/jama.296.22.2694. [DOI] [PubMed] [Google Scholar]