Abstract
Individuals in substance use disorder (SUD) treatment have shown high levels of difficulty with emotion regulation, as well as a high prevalence of reported trauma and symptoms of post-traumatic stress (PTS). Dissociation from the body is a common clinical experience among women with a history of sexual trauma. Research has shown promising effects of mind-body approaches in SUD treatment, as well as the importance of emotional regulation in conceptual models of psychopathology. The current study examines the mediating role of bodily dissociation and emotion regulation on PTS symptoms in a sample of women enrolled in substance use disorder treatment. Results indicate that bodily dissociation and emotion regulation had significant direct effects on PTS symptoms from baseline to a 6-month follow-up, and that bodily dissociation also may indirectly operate to reduce PTS symptoms through its effect on emotion regulation difficulties. These results suggest the importance of addressing bodily dissociation and emotion regulation difficulties in women’s substance use disorder treatment.
Keywords: substance disorder treatment, women, dissociation, emotion regulation, post traumatic stress
Introduction
Emotion regulation difficulties are typically high in post traumatic stress disorder (PTSD),1 characterized by high intensity emotional reaction, low stress tolerance, experiential avoidance, and lack of control.2,3 PTSD can impair development of sense of self, lead to decreased belief in control over one’s body, and result in maladaptive coping strategies such as dissociation.4–6 The rates of PTSD among substance users are high and range from 25%–47%7,8 and, among individuals in treatment, there is a gender difference in type of trauma, with women reporting significantly more interpersonal violence compared to men. The emergence of mind-body approaches in substance use treatment,9 in combination with the inclusion of emotional regulation in conceptual models of psychopathology, has led to increased interest in the role of emotional regulation in the treatment of problematic substance use.10 Mind-body therapies, in general, address the relationships among somato-emotional awareness, coping, and emotional regulation and teach integrative strategies that may help individuals react more effectively to stress and negative emotions.11–13
Clinical studies have shown that for individuals in substance abuse treatment, emotion regulation difficulties as measured by the Difficulties in Emotional Regulation Scale (DERS)14 are significantly higher compared to community controls.15,16 Due to the high prevalence of PTSD and reported trauma among individuals seeking treatment for a substance use disorder (SUD), recent studies have examined the PTSD-SUD relation to emotional regulation difficulties. Among young people17 and adults18 with co-morbid PTSD and SUD, studies show higher rates of substance use in emotionally negative situations compared to individuals with SUD only. In addition, emotion-focused coping was found to mediate the relationship between PTSD symptom severity and negative situational use in young adults.17 Studies of individuals engaged in substance abuse treatment show a significant association between emotion regulation difficulties (as measured by the DERS) and PTSD symptoms.19,20
Recent theoretical models21,22 suggest the underlying role of interoception, defined as awareness of inner body sensations,23,24 for regulation among individuals that abuse alcohol and drugs. There is preliminary evidence that women with PTSD show a failure to activate neural circuitry to modulate interoceptive responses compared to non-traumatized healthy women.25 A lack of sensory and emotional awareness and related regulatory processes are common among women with a history of interpersonal trauma.1,4,6 In addition, PTSD severity may be related to the degree of peritraumatic dissociation (dissociation that occurs during the traumatic event(s)).26,27 Bodily dissociation, a sense of separation from and lack of awareness of bodily sensations, is an aspect of dissociative experience.28 Among individuals with PTSD, bodily dissociation can be an avoidant/protective strategy to cope with sensory and emotional stressors,4,29 and can interfere with the ability to engage in interoceptive awareness in clinical treatment of PTSD.30,31 While few studies have examined the role of dissociation improvement in trauma treatment, the results of these studies suggest that there is a mediating role of dissociation on psychological health and regulation indicators among women in recovery from childhood sexual abuse. For example, one study demonstrated the association between improved dissociation and psychological health and body awareness/connection (the antithesis of bodily dissociation) at treatment intervals across time among women receiving body therapy during their treatment for childhood sexual abuse,29 while another showed significantly improved emotion regulation among individuals in treatment for childhood sexual abuse that received adjunctive sensory integration therapy that targeted bodily dissociation and no improvement among the controls who did not.32 A third study demonstrated that improved dissociation promoted cognitive and affective processing in PTSD treatment.33
Although the role of bodily dissociation and emotion regulation are theoretically mediators of post traumatic stress (PTS) symptoms for individuals in substance use disorder treatment, this has yet to be examined empirically. The current study explored these posited roles of bodily dissociation and emotion regulation difficulties as potential mediators between baseline PTS and later PTS symptoms among women in substance abuse treatment, including the direct effect of bodily dissociation on emotional regulation as suggested in the above research. The data came from a prior study of Mindful Awareness in Body-oriented Therapy (MABT), a mind-body intervention designed to teach interoceptive skills for self-care, for women in substance use disorder treatment.34 Mediation of PTSD symptoms by bodily dissociation and emotion regulation As the development and implementation of mind-body treatment approaches for SUDs continues to grow, it is critical that we understand more about the potential role of bodily dissociation and emotion regulation difficulties on PTS.
Methods
Sample
The current study was based on analyses of the full sample of adult women enrolled in a prior treatment study for alcohol and other drug use disorders. The sample was comprised of 52 women engaged in a women-only intensive SUD treatment program at a private non-profit agency. The prior study involved assessments at 4 time points and these were used in this analysis: baseline, 3, 6 and 9 months. In the prior study, participants were randomly assigned to receive MABT plus usual care or usual care only after the baseline assessment. Usual care involved inpatient residential care for 3 weeks followed by intensive outpatient treatment for approximately 16 weeks. The recruitment, assessment procedures, further details regarding usual care and MABT intervention, and randomized-controlled trial results are detailed in a prior publication.34
Participants ranged in age from 18 to 58 (M = 38.83, SD = 11.4). They identified as white (not Hispanic, 94.2%), mixed race (3.8%), or Asian (1.9%). All participants had entered SUD treatment voluntarily (versus mandated). The majority were unemployed (63.5%), with annual income ranging from 0–$210,000 and a median household income of $55,000. All participants were high school graduates or had acquired certificates of high school equivalency. Alcohol was the primary substance of abuse (67.3%), followed by opiates or other analgesics (17.3%). Approximately 33% of the sample reported polysubstance abuse. Approximately 65% of participants reported sexual and/or physical trauma in either childhood or as an adult; these individuals met screening criteria for PTSD. Participants were fluent in English. Excluded were those with current psychosis, dementia, imminent suicide risk, or inability to attend MABT sessions.
Measures
All measures administered were self-report, collected via paper-and-pencil at 4 assessment time points across the 9-month study period (baseline, 3, 6 and 9 months). The Bodily Dissociation (BD) scale, a subscale of the Scale of Body Connection,35 was used to assess bodily dissociation. BD assesses separation from body, including emotional disconnection (eg, difficulty attending to emotion). It is a Likert type scale; a lower score indicates less bodily dissociation; Cronbach’s alpha for DB with this sample was 0.74. The Difficulties in Emotion Regulation Scale (DERS)14 is a Likert-type scale assessing 5 different subfactors of emotion regulation; a lower score indicates fewer difficulties in emotion regulation. To reduce subject burden, the DERS was shortened and select subscales of the DERS were used: Impulse Control Difficulties, Limited Access to Emotion Regulation Strategies, and Lack of Emotional Clarity. DERS subscales were summed together and the reliability of the DERS summed scales was 0.78. PTS symptoms were assessed using the Modified PTSD Symptom Scale (MPSS),36 a Likert-type scale; a lower score indicates fewer PTS symptoms. The items are clustered into reexperiencing, avoidance, and arousal symptoms in accordance with the Diagnostic and Statistical Manual of Mental Disorders, 4th edition diagnostic criteria for PTSD,37 and it has demonstrated good internal consistency.38,39 Cronbach’s alpha for the MPSS was 0.95.
Procedure
The consent forms, signed by all study participants, and study procedures were in accord with the Helskinki Declaration of 1975 and approved by the Institutional Review Board of the University of Washington. 61 participants were screened, 53 meet inclusion criteria and 52 completed baseline assessment and were included in this study sample. Participants were compensated with gift cards upon completion of each assessment.
Analytic plan
To test the general posited model, a path analysis approach with a maximum likelihood estimation was used to test the effect of bodily dissociation and emotion regulation difficulties on PTS symptoms involving assessments at baseline, 3 and 6 month follow-up and/or 9 month follow-up. Given the small N in this analysis, we were cautious regarding our ML estimation and the underlying multivariate normal assumptions. While the distribution of the variables were reasonably normal, which provides some assurance to the underlying assumptions, we also used OLS estimation and bootstrapped standard errors in separate analyses. The results of these alternative assessments of the model were consistent with the ML results provided. The only differences observed were actually in the assessments of the indirect path standard errors; our estimates using the delta method (shown) versus bootstrapped standard errors suggest the significant indirect paths pointed to below should be interpreted with some caution. All direct paths, however, were robust to method used.
Furthermore, we acknowledge the possible effects of having some members of the sample participating in additional treatment. To address the issue of this treatment condition, the analysis was run with and without the inclusion of the subset of individuals that completed the MABT intervention so that those included had no, or almost no (due to early relapse and study drop out) exposure to MABT. As an additional alternative, we simply included a MABT exposure covariate in the current model. There was little difference between the models with this sub- sample and the full sample or with the model including the covariate, thus we are reporting the results from the depicted model using the full sample to maximize the sample size available and to limit the number of parameters estimated. There was also little difference between the models using 6 or 9 months as the final assessment time point, and thus we are reporting the results of the model utilizing baseline, 3- and 6-month assessments.
Results
Descriptive statistics for variables included in analyses are shown in Table 1. No significant relationships were found between the outcome variable (PTS) and ethnic minority status in the sample. Correlations at baseline across measures of PTS, DERS and BD were all significant and of moderate magnitude between 0.41–0.45. The correlations among the temporal variables used in the model are provided in Table 2; all correlations were significant at 0.05 or less.
Table 1.
Means (SD) of primary variables.
| Baseline (n = 52) | 3 months (n = 35) | 6 months (n = 34) | |
|---|---|---|---|
| BD | 1.6 (0.65) | 1.2 (0.58) | 1.1 (0.52) |
| DERS† | 49.8 (14.8) | 34.9 (10.8) | 33.5 (11.5) |
| PTS | 56.1 (27.5) | 34.7 (25.9) | 27.1 (24.1) |
Note:
Includes impulse control difficulties, limited access to emotion regulation strategies, and lack of emotional clarity subscales.
Abbreviations: BD, Bodily Dissociation from the Scale of Body Connection; DERS, Difficulties in Emotional Regulation Scale; PTS, Post Traumatic Stress Scale symptoms from the Modified PTSD Symptom Scale.
Table 2.
Correlations among model variables.
| Correlations | ||||
|---|---|---|---|---|
|
|
||||
| DERS2 | DB2 | PTS3 | PTS1 | |
| DERS2 | 1.000 | |||
| DB2 | 0.568* | 1.000 | ||
| PTS3 | 0.616** | 0.288 | 1.000 | |
| PTS1 | 0.267# | 0.385* | 0.540** | 1.000 |
Notes:
P < 0.10;
P < 0.05;
P < 0.01.
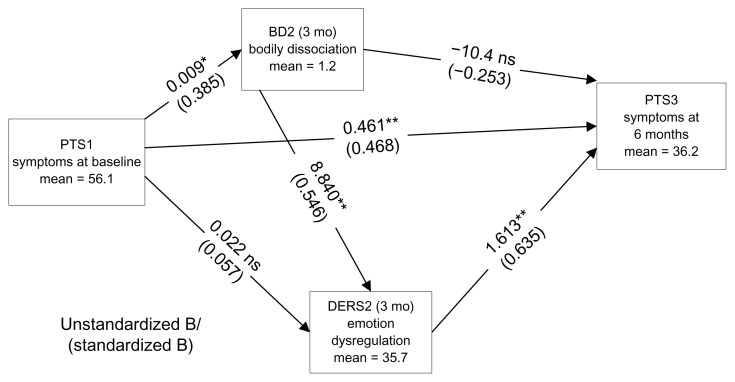
We estimated the model in Figure 1 with and without the direct effect of baseline PTS symptoms and the better of the 2 models included the direct effect of PTS symptoms at baseline to PTS symptoms at 6 months as shown. The model without the direct effect indicated poor fit using chi-square. The Comparative Fit Index (CFI) index and Root Mean Square Error of Approximation (RMSEA) and the subsequent addition of the direct effect provided a significant reduction in the chi-square (10.5 1/df P < 0.01) and had a smaller Bayesian Information Criterion (BIC) measure. The posited mediating variables of bodily dissociation at 3 months (BD2) and emotion regulation difficulties at 3 months (DERS2) both had effects on PTS symptoms at 6 months, controlling for baseline PTS. To understand the total effects of initial PTS symptoms on later PTS symptoms, we were interested in the indirect effects implied in the model of how PTS symptoms operate through both bodily dissociation and emotional regulation difficulties, as well as the direct effect observed (b = 0.461; standardized (std) B = 0.468; P < 0.01). The coefficients in Figure 1 for the relation of initial PTS symptoms to bodily dissociation and to emotion regulation difficulties showed direct effects to bodily dissociation, but not to emotional regulation difficulties; however, PTS symptoms were indirectly related to DERS2 though bodily dissociation (indirect effect = 0.082; P < 0.04). This route from baseline PTS to later PTS is complex, given that bodily dissociation was not directly related to 6-month PTS symptoms and was only indirectly related via emotional regulation difficulties (indirect effect = 14.3, std indirect effect = 0.347 P < 0.01), while emotional regulation difficulty was directly related to later PTS symptoms (b = 1.63, std B = 0.635 P < 0.01). Clearly the direct effect of PTS symptoms from baseline to 6 months (b = 0.461, std B = 0.468) is larger than its complex indirect route through bodily dissociation (BD2) to emotion regulation difficulties (DERS2) to PTS symptoms at 6 months (b = 0.132, std B = 0.134). The import of these indirect effects should be interpreted with some caution since its statistical significance varies with type of estimation procedure used for its standard error; the delta method standard errors (SEs) suggest significant indirect paths, while the bootstrap SEs are somewhat larger and not significant at the 0.05 level.
Figure 1.
Mediation model.
Notes: *≤0.05; **≤0.01.
Discussion
The results of this study support the posited partial mediation of PTS symptoms by bodily dissociation and emotion regulation difficulties. These sets of indirect effects are important in that the full indirect route of initial PTS symptoms to PTS symptoms at 6 months involves reductions in both bodily dissociation and emotion regulation difficulties and is a possible chain of PTS symptoms to BD2 to DERS2 to latter PTS symptoms.
These results are preliminary and reflect one possible model. While it is possible that alternative models may also fit the data, it is nonetheless useful for considering the potential roles of bodily dissociation and emotion regulation difficulties on PTS symptoms. The posited model is consistent with prior knowledge and conceptualization of how PTS influences bodily dissociation and emotional regulation, and how bodily dissociation may impact regulation. Clearly an alternative is to remove the path from BD to DERS, or perhaps even reverse this effect.
Other processes may also be involved. For example, several mechanisms by which improved bodily dissociation may help increase emotion regulation skills in individuals with PTS symptoms may be implicated. PTSD is characterized by difficulty assessing the emotional environment and negotiating internal and external sensory and emotional cues to effectively process affective information.40 Improved bodily dissociation may facilitate emotion regulation in the face of PTS symptom triggers, such as escalating emotion or a challenging interpersonal or physical environment. There are 3 symptom clusters involved in PTSD: avoidance, the intrusive re-experiencing of trauma memories, and hyperarousal.37 Increased association with (vs. dissociation from) the body may facilitate the ability to be aware of and accept sensory experience (versus avoid), to recognize sensory cues that are associated with emotional escalation and thus break from automatic habitual dissociative processes (versus re-experience in response to triggers), and to engage in interoceptive processing of internal sensations (rather than become reactive, which may lead to heightened arousal). Thus, it is possible that improved bodily dissociation and associated interoceptive processing addresses regulation of core PTSD symptoms of avoidance, re-experiencing and hyperarousal. It is also possible that the role of bodily dissociation in treatment of PTSD symptoms is contingent on the experience of peritraumatic bodily dissociation, which one might expect in this female SUD population for whom the traumatic experiences were interpersonal and often involved sexual abuse as children and domestic violence as adults. The findings from this study provide beginning empirical support that bodily dissociation and emotion regulation difficulties may partially mediate PTS symptoms among a female SUD population.
There are several study limitations to consider. Our hypothesis was tested in a small sample, the participants likely had a higher socioeconomic status than typically seen across community clinics, and our study involved women only. However, the high level of trauma exposure and symptoms of post-traumatic stress among this study sample is typical of women in SUD treatment, suggesting the generalizabilty of these findings. Also, we used a set of DERS subscales rather than the full scale; DERS subscales have, however, been shown in other studies to be highly correlated.14,41
This study was not powered to test the posited model, and thus we are not fully able to assess the possible significant route of these various mediating relationships; the direct effects in the model hold but the indirect estimates significance is not consistent across the various estimators used. The basic results, however, do hold when accounting for the individuals exposed to additional treatment (MABT exposure).
In conclusion, the negative health consequences associated with post-traumatic stress among women with SUD highlight the need to better understand what treatments may be most effective and for whom. Despite the study limitations and many unanswered questions, these study results are an important first step, indicating the potential role of bodily dissociation and emotion regulation in treatment of PTS symptoms among women in SUD treatment. These study results also suggest the importance of treatments that teach somatic awareness and association for this population. We hope that these results will stimulate more research specific to the role of bodily dissociation, interoceptive awareness, and emotion regulation in trauma and substance use disorder treatment.
Footnotes
Author Contributions
Conceived and designed the experiments: CP. Analyzed the data: JH. Wrote the first draft of the manuscript: CP, JH. Contributed to the writing of the manuscript: CP, JH. Agree with manuscript results and conclusions: CP, JH. Jointly developed the structure and arguments for the paper: CP, JH. Made critical revisions and approved final version: CP, JH. All authors reviewed and approved of the final manuscript.
Competing Interests
Author(s) disclose no potential conflicts of interest.
Disclosures and Ethics
As a requirement of publication the authors have provided signed confirmation of their compliance with ethical and legal obligations including but not limited to compliance with ICMJE authorship and competing interests guidelines, that the article is neither under consideration for publication nor published elsewhere, of their compliance with legal and ethical guidelines concerning human and animal research participants (if applicable), and that permission has been obtained for reproduction of any copyrighted material. This article was subject to blind, independent, expert peer review. The reviewers reported no competing interests.
Funding
This study was partially funded by the National Institute of Drug Abuse (NIDA) at NIH (#R21 DA024771).
References
- 1.van der Kolk BA, Pelcovitz D, Roth S, Mandel FS, McFarlane A, Herman JL. Dissociation, somatization, and affect dysregulation: the complexity of adaptation of trauma. Am J Psychiatry. 1996;153(Suppl 7):83–93. doi: 10.1176/ajp.153.7.83. [DOI] [PubMed] [Google Scholar]
- 2.Eftekhari A, Zoellner LA, Vigil SA. Patterns of emotion regulation and psychopathology. Anxiety Stress Coping. 2009;22(5):571–86. doi: 10.1080/10615800802179860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore SA, Zoellner LA, Mollenholt N. Are expressive suppression and cognitive reappraisal associated with stress-related symptoms? Behav Res Ther. 2008;46(9):993–1000. doi: 10.1016/j.brat.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herman J. Trauma and Recovery: The Aftermath of Violence—From Domestic Abuse to Political Terror. New York: HarperCollins; 1997. [Google Scholar]
- 5.Veysey B, Clark C. Introduction. Alcoholism Treatment Quarterly. 2005;22(3):1–18. [Google Scholar]
- 6.Briere J, Runtz M. Childhood sexual abuse—long-term sequelae and implications for psychological-assessment. Journal of Interpersonal Violence. 1993;8(3):312–30. [Google Scholar]
- 7.Driessen M, Schulte S, Luedecke C, et al. TRAUMAB-Study Group. Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multi-center study. Alcohol Clin Exp Res. 2008;32(3):481–8. doi: 10.1111/j.1530-0277.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- 8.Lubman DI, Allen NB, Rogers N, Cementon E, Bonomo Y. The impact of co-occurring mood and anxiety disorders among substance-abusing youth. J Affect Disord. 2007;103(1–3):105–12. doi: 10.1016/j.jad.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Zgierska A, Marcus MT. Mindfulness-based therapies for substance use disorders: part 2. Subst Abus. 2010;31(2):77–8. doi: 10.1080/08897071003641248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Breslin KT, Reed MR, Malone SB. An holistic approach to substance abuse treatment. J Psychoactive Drugs. 2003;35(2):247–51. doi: 10.1080/02791072.2003.10400006. [DOI] [PubMed] [Google Scholar]
- 12.Kosakoski J. Massage: Hands down, a treatment for addiction. Counselor: The Magazine for Addiction Professionals. 2003;4:36–8. [Google Scholar]
- 13.Wesa KM, Culliton P. Recommendations and guidelines regarding the preferred research protocol for investigating the impact of an optimal healing environment on patients with substance abuse. J Altern Complement Med. 2004;10(Suppl 1):S193–9. doi: 10.1089/1075553042245755. [DOI] [PubMed] [Google Scholar]
- 14.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- 15.Fox HC, Axelrod SR, Paliwal P, Sleeper J, Sinha R. Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug Alcohol Depend. 2007;89(2–3):298–301. doi: 10.1016/j.drugalcdep.2006.12.026. [DOI] [PubMed] [Google Scholar]
- 16.Fox HC, Hong KA, Sinha R. Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addict Behav. 2008;33(2):388–94. doi: 10.1016/j.addbeh.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Staiger PK, Melville F, Hides L, Kambouropoulos N, Lubman DI. Can emotion-focused coping help explain the link between posttraumatic stress disorder severity and triggers for substance use in young adults? J Subst Abuse Treat. 2009;36(2):220–6. doi: 10.1016/j.jsat.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 18.Waldrop AE, Back SE, Verduin ML, Brady KT. Triggers for cocaine and alcohol use in the presence and absence of posttraumatic stress disorder. Addict Behav. 2007;32(3):634–9. doi: 10.1016/j.addbeh.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 19.McDermott MJ, Tull MT, Gratz KL, Daughters SB, Lejuez CW. The role of anxiety sensitivity and difficulties in emotion regulation in posttraumatic stress disorder among crack/cocaine dependent patients in residential substance abuse treatment. J Anxiety Disord. 2009;23(5):591–9. doi: 10.1016/j.janxdis.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bornovalova MA, Ouimette P, Crawford AV, Levy R. Testing gender effects on the mechanisms explaining the association between post-traumatic stress symptoms and substance use frequency. Addict Behav. 2009;34(8):685–92. doi: 10.1016/j.addbeh.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paulus MP. Neural basis of reward and craving—a homeostatic point of view. Dialogues Clin Neurosci. 2007;9(4):379–87. doi: 10.31887/DCNS.2007.9.4/mpaulus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldstein RZ, Craig AD, Bechara A, et al. The neurocircuitry of impaired insight in drug addiction. Trends Cogn Sci (Regul Ed) 2009;13(9):372–80. doi: 10.1016/j.tics.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3(8):655–66. doi: 10.1038/nrn894. [DOI] [PubMed] [Google Scholar]
- 24.Craig AD. How do you feel—now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10(1):59–70. doi: 10.1038/nrn2555. [DOI] [PubMed] [Google Scholar]
- 25.Simmons AN, Paulus MP, Thorp SR, Matthews SC, Norman SB, Stein MB. Functional activation and neural networks in women with posttraumatic stress disorder related to intimate partner violence. Biol Psychiatry. 2008;64(8):681–90. doi: 10.1016/j.biopsych.2008.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- 27.Gershuny BS, Cloitre M, Otto MW. Peritraumatic dissociation and PTSD severity: do event-related fears about death and control mediate their relation? Behav Res Ther. 2003;41(2):157–66. doi: 10.1016/s0005-7967(01)00134-6. [DOI] [PubMed] [Google Scholar]
- 28.Sadock BJ, Sadock VA. Kaplan & Sadock’s Comprehensive Textbook of Psychiatry. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 29.Price C. Dissociation reduction in body therapy during sexual abuse recovery. Complement Ther Clin Pract. 2007;13(2):116–28. doi: 10.1016/j.ctcp.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Timms R, Connors P. Embodying Healing: Integrating Bodywork and Psychtherapy in recovery from Childhood Sexual Abuse. Orwell, VT: Safer Society Press; 1992. [Google Scholar]
- 31.Ogden P, Minton K. Sensorimotor psychotherapy: one method for processing traumatic memory. Traumatology. 2000;6:149–73. [Google Scholar]
- 32.Kaiser E, Gillette C, Spinazzola J. A controlled pilot-outcome study of sensory integration (SI) in the treatment of complex adaptation to traumatic stress. Journal of Aggression, Maltreatment & Trauma. 2010;19:699–720. [Google Scholar]
- 33.Cloitre M, Petkova E, Wang J, Lu Lassell F. An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depress Anxiety. 2012;29(8):709–17. doi: 10.1002/da.21920. [DOI] [PubMed] [Google Scholar]
- 34.Price CJ, Wells EA, Donovan DM, Rue T. Mindful awareness in body-oriented therapy as an adjunct to women’s substance use disorder treatment: a pilot feasibility study. J Subst Abuse Treat. 2012;43(1):94–107. doi: 10.1016/j.jsat.2011.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Price CJ, Thompson EA. Measuring dimensions of body connection: body awareness and bodily dissociation. J Altern Complement Med. 2007;13(9):945–53. doi: 10.1089/acm.2007.0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Falsetti S, Resnick H, Resick P, Kilpatrick D. The modified ptsd symptom scale: a brief self-report measure of posttraumatic stress disorder. The Behavior Therapist. 1993;16:161–2. [Google Scholar]
- 37.American Psychiatric Association. Diagnostic and Statistical Manual of mental Disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 38.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34(8):669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 39.Coffey SF, Dansky BS, Falsetti SA, Saladin ME, Brady KT. Screening for PTSD in a substance abuse sample: psychometric properties of a modified version of the PTSD Symptom Scale Self-Report. Posttraumatic stress disorder. J Trauma Stress. 1998;11(2):393–9. doi: 10.1023/A:1024467507565. [DOI] [PubMed] [Google Scholar]
- 40.Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61(3):201–16. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- 41.Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and post-traumatic stress symptoms. Behav Ther. 2007;38(3):303–13. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]