Abstract
Purpose
To compare the success rates, complications, and visual outcomes between silicone Ahmed glaucoma valve (AGV) implantation with 96 mm2 (FP8) or 184 mm2 (FP7) surface areas.
Methods
This study is a retrospective review of the records from 132 adult patients (134 eyes) that underwent silicone AGV implant surgery. Among them, the outcomes of 24 eyes from 24 patients with refractory glaucoma who underwent FP8 AGV implantation were compared with 76 eyes from 76 patients who underwent FP7 AGV implantation. Preoperative and postoperative data, including intraocular pressure (IOP), visual acuity, number of medications, and complications were compared between the 2 groups.
Results
There were no significant differences in baseline characteristics between the 2 groups (p > 0.05). The postoperative visual acuity of the patients in the FP8 group was better than that of the patients in the FP7 group in some early postoperative periods (p < 0.05); however, after 10 postoperative months, visual acuity was not significantly different through the 3-year follow-up period (p > 0.05). Postoperative IOP was not significantly different between the 2 groups (p > 0.05) except for IOP on postoperative day 1 (11.42 mmHg for the FP7 group and 7.42 mmHg for the FP8 group; p = 0.031). There was no statistical difference in success rates, final IOP, number of medications, or complication rates between the 2 groups (p > 0.05).
Conclusions
The FP7 and FP8 AGV implants showed no difference in terms of vision preservation, IOP reduction, and number of glaucoma medications required.
Keywords: Filtering surgery, Glaucoma drainage implants
Glaucoma is a leading cause of irreversible blindness worldwide [1]. For the surgical treatment of glaucoma, filtering surgery, such as trabeculectomy, is performed as a standard procedure. However, in cases of intractable glaucoma, including neovascular glaucoma, uveitic glaucoma, aphakic or intraocular lens glaucoma, and glaucoma after penetrating keratoplasty, it has been reported that the success rate of trabeculectomy is low [2-6]. An aqueous outflow device was first used to treat intractable glaucoma by Zorab in 1912 [7]. Since then, various aqueous outflow devices have been developed for intraocular pressure (IOP) reduction in glaucoma refractory to glaucoma filtering surgeries [8]. The Ahmed glaucoma valve (AGV; New World Medical Inc., Rancho Cucamonga, CA, USA) was introduced in 1993 as the first aqueous shunting device that has a unidirectional valve mechanism designed to prevent postoperative hypotony [9]. Currently, there are 2 types of AGVs that differ in their surface areas: 96 mm2 (FP8), which is generally used in children and 184 mm2 (FP7), which is generally used in adults. In the clinical setting, implantation of the FP7 AGV is challenging in adult eyes with conjunctival scarring or limited subconjunctival space owing to previous ocular surgeries, inflammatory ocular disorders, or small eyes. In these cases, the FP8 AGV is used instead of the FP7 AGV in adult eyes with glaucoma. Although silicone AGV is widely used, little is known about the differences in the efficacy and safety between the 2 models. If the FP7 and FP8 AGVs are similar in terms of efficacy and safety for treatment of adult glaucoma, using the FP8 AGV in adult eyes with insufficient conjunctival or subconjunctival condition could be a useful surgical option for IOP control. This study was performed to compare the postoperative outcomes between FP7 and FP8 AGV implants in adult eyes with glaucoma.
Materials and Methods
Participants
The study protocol was approved by the institutional review board of Kim's Eye Hospital, Seoul, Korea. All participants provided informed consent prior to enrollment and all procedures conformed to the guidelines of the Declaration of Helsinki. From June 2006 to July 2011, 134 eyes from 132 patients who underwent AGV implantation surgery at Kim's Eye Hospital were analyzed retrospectively. Each subject underwent a full ophthalmic examination, including visual acuity assessment, IOP assessment with a Goldmann applanation tonometer, anterior segment examination by slit-lamp biomicroscopy, fundus examination with a 90 diopter (D) lens, and 24-2 Swedish Interactive Threshold Algorithm standard automated visual fieldest (Humphrey Visual Field Analyzer; Carl Zeiss Meditec, Dublin, CA, USA) before surgery as well as 1 day, 1 month, 2-3 months, 4-6 months, 11-16 months, and 17-24 months after surgery. The number of eye drops used for IOP control was also recorded.
The study included any patient who underwent AGV implantation surgery at Kim's Eye Hospital performed using the same technique by 1 of 2 glaucoma specialists (YHS and HKK) with a minimum of 6 months follow-up. The exclusion criteria were: patients' age less than 18 years or more than 80 years, AGV implanted in inferior quadrants, previous seton surgery or trabeculectomy in the operated eye, inflammatory or ocular surface disease with severe conjunctival scarring, history of retinal detachment surgery with scleral buckle or vitrectomy in the operated eye, and history of endophthalmitis in the operated eye. Among the 134 eyes from 132 patients, 44 eyes from 42 patients were excluded. For the remaining 90 eyes from 90 patients, diagnoses before surgery included: 50 eyes had neovascular glaucoma, 36 eyes had secondary open angle glaucoma, and 4 eyes had primary open angle glaucoma.
The AGV implantation selection was made by the surgeon based on conjunctival mobility and presence of previous surgical conjunctival scaring, limited subconjunctival space owing to previous ocular surgeries, scarred upper fornix, shallow fornix, and presence of small eyes. Eyes implanted with the FP7 and FP8 AGVs were assigned to the FP7 group and FP8 group, respectively.
Surgical procedures
The procedures were performed in a similar manner in all subjects regardless of implant size. The conjunctival incision was made 4 mm posterior to the limbus and, following dissection of the conjunctiva and tenon's capsule toward the fornix and limbus, bipolar cautery was performed. Mitomycin-C (0.02%) was applied with a large piece of soaked cellulose sponge under the conjunctival flap and over the episclera for 3 minutes followed by thorough irrigation of the area with a balanced salt solution. AGV priming was performed by gentle irrigation of the tube with a 27-gauge needle. The plate of the implant was then secured to the sclera 8 to 10 mm posterior to the surgical limbus using 2 interrupted 7-0 silk sutures. The tube was trimmed to an appropriate length with the bevel facing anteriorly and, after injection of methyl cellulose into the anterior chamber via a clear cornea stab incision, the tube was inserted into the anterior chamber through a corneoscleral track created using a 23-gauge needle. The tube was fixed to the episclera with a 10-0 nylon mattress suture. A quadrangular donor scleral patch graft (4 × 7 mm) was fashioned and secured over the exposed part of the tube using 10-0 nylon sutures. The conjunctiva and Tenon's capsule were repaired using 8-0 vicryl suture material in a running fashion. Dexamethasone (4 mg) and gentamycin (100 mg) were injected subconjunctivally upon procedure conclusion. The postoperative regimen included topical levofloxacin (0.5%) eye drops 4 times per day for 1 week and topical fluorometholone (0.1%) eye drops 4 times per day that was usually tapered over 6 to 8 weeks. Postoperative follow-up visits were scheduled for 1 day, 1 and 2 weeks, and 1, 3, 6, and 12 months after the procedure and every 6 months thereafter. Outcome measures of the study were compared at each time point.
Statistical analyses
Surgical success was defined as IOP maintained below 21 mmHg regardless of the number of IOP medications used during the final follow-up observation. The following observations made during follow-up were regarded as surgical failures: an IOP greater than 22 mmHg at 2 or more consecutive follow-up visits, an IOP less than 5 mmHg at 2 or more consecutive follow-up visits, additional glaucoma surgery was required, and loss of light perception [8,10,11].
Independent t-tests and chi-squared tests were performed to compare ocular and demographic variables between the 2 groups. To compare the success rate of surgery between the 2 groups, a log-rank (Mantel-Cox) test was performed. A p-valve of <0.05 was considered statistically significant. Statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 90 eyes (90 patients) were included in the study. Among them, 66 eyes underwent FP7 implant surgery, and 24 eyes underwent FP8 implant surgery. Table 1 summarizes the demographic and clinical characteristics of the study populations. The mean age was 57.6 ± 11.4 years for the FP7 group and 61.0 ± 9.9 years for the FP8 group (p = 0.199). Preoperative IOP was 41.9 ± 9.2 mmHg for the FP7 group and 39.0 ± 6.6 mmHg for the FP8 group (p = 0.105). There was no significant difference between the 2 groups in the following variables: sex, systemic disease distribution, glaucoma subtype, baseline visual acuity, number of preoperative antiglaucoma medications, previous ocular surgeries, laterality, and implantation site (p > 0.05) (Table 1).
Table 1.
Comparison of clinical characteristics between the FP7 and FP8 groups
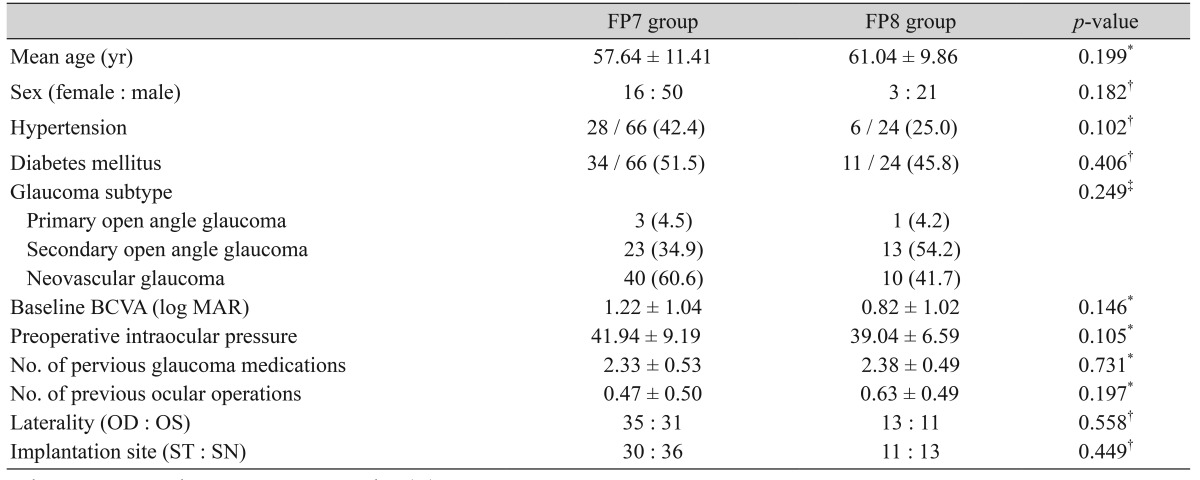
Values are presented as mean ± SD or number (%).
BCVA = best-corrected visual acuity; log MAR = logarithm of minimum angle of resolution; ST = superotemporal side; SN = superonasal side.
*Independent t-test; †Chi square test; ‡Fisher's exact test.
The mean follow-up period was 17.2 ± 9.1 months for the FP7 group and 20.3 ± 4.4 months for the FP8 group (p = 0.273). The postoperative visual acuity of the FP8 group was better than that in the FP7 group in some early postoperative periods (1 week, 2 to 3 months, and 7 to 10 months after the surgery; p < 0.05); however, after 10 postoperative months, there were no significant differences in visual acuity between the 2 groups through the 3-year follow-up (p > 0.05) (Table 2). Postoperative IOP was not significantly different between the 2 groups (p > 0.05) except for the IOP on postoperative day 1 (11.4 ± 8.4 mmHg for the FP7 group and 7.4 ± 3.9 mmHg for the FP8 group, p = 0.031) (Table 3). There were no statistically significant differences between the groups in terms of the number of glaucoma medications after surgery (Table 4).
Table 2.
Comparison of visual acuity between the FP7 and FP8 groups (logarithm of minimum angle of resolution, mean ± standard deviation)
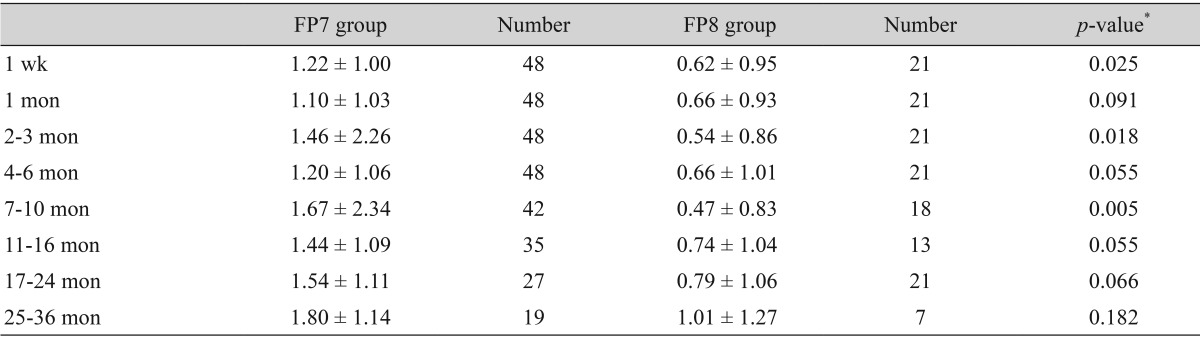
*Independent t-test.
Table 3.
Comparison of postoperative intraocular pressure between the FP7 and FP8 groups (mmHg, mean ± standard deviation)
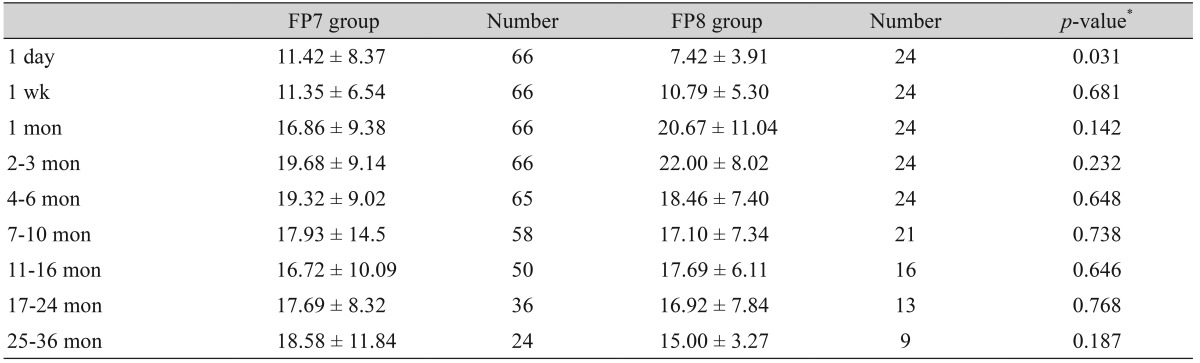
*Independent t-test.
Table 4.
Comparison of the number of postoperative glaucoma medications between the FP7 and FP8 groups (mean ± standard deviation)
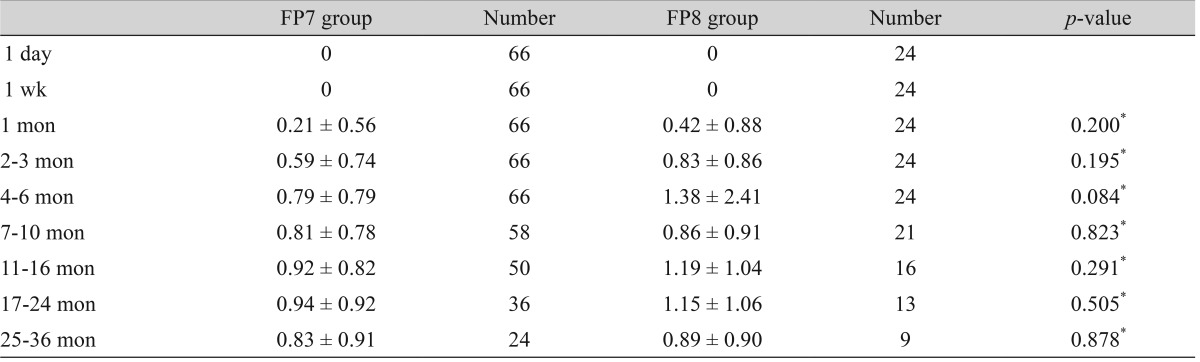
*Independent t-test.
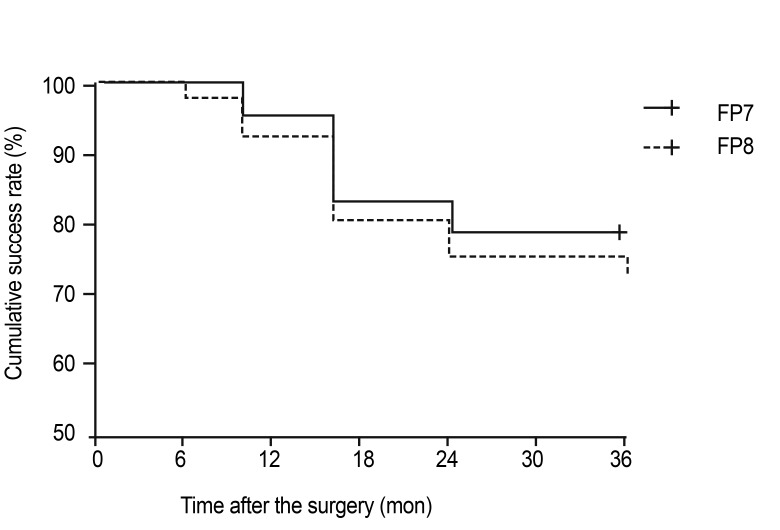
In this study, surgical success was considered as IOP maintained at less than 21 mmHg regardless of the medication used, no additional glaucoma surgery required, non-occurrence of light sense loss, and no consecutive follow-up visits with low IOP. Therefore, the cumulative success rate according to the log-rank test for Kaplan-Meier survival analysis was 79.2% for the FP8 group and 72.7% for the FP7 group at the 3-year follow-up (p = 0.535) (Fig. 1). The main reasons for failure were not significantly different between the 2 groups (Table 5).
Fig. 1.
Kaplan-Meier survival curves illustrating the cumulative success rates of both Ahmed glaucoma valve implantation groups. The final success rate 3 years after the operation was 72.7% for the FP7 group and 79.2% for the FP8 group (p = 0.535, log-rank test).
Table 5.
Distribution of the main reason for failure in the FP7 (n = 66) and FP8 (n = 24) groups
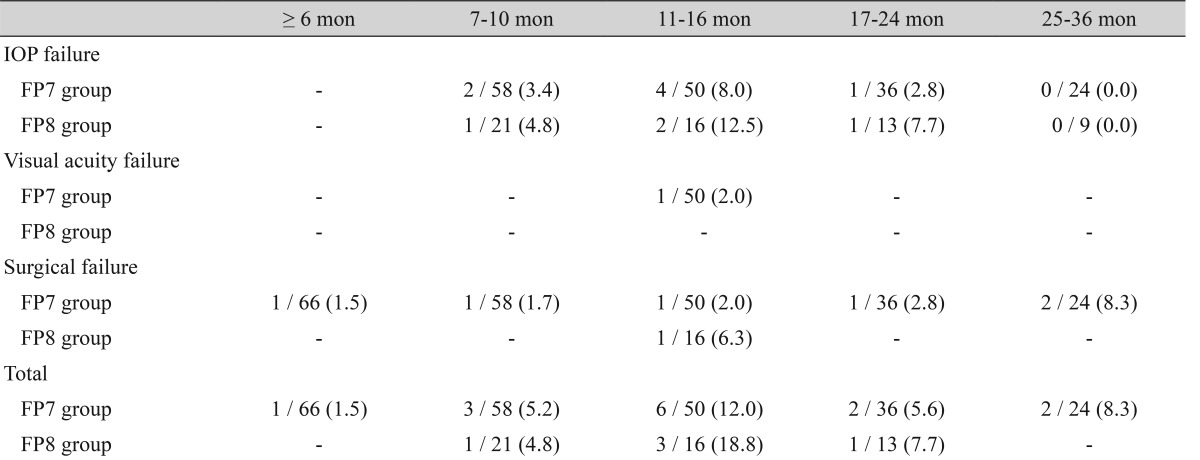
Values are presented as number (%).
IOP = intraocular pressure.
Discussion
It has been hypothesized that glaucoma drainage implants with large plates produces an increased surface area of encapsulation and a higher degree of IOP reduction [12]. In a prospective randomized clinical trial comparing single-plate and double-plate Molteno implants, Heuer et al. [13] found a higher success rate and greater IOP reduction with the double-plate implants than with single-plate implants, presumably because of the large surface area of the double-plate implants. On the contrary, Seah et al. [14] reported no significant difference in success rates, final IOP, number of medications, and rates of complications between the 250 and 350 mm2 Baerveldt glaucoma implants (BGIs). In another prospective study comparing the 350 and 500 mm2 BGIs, Lloyd et al. [15] reported that there was no difference in success rates and visual outcomes between the different implant sizes. Britt et al. [16] also reported that the 500 mm2 BGI was not superior to the 350 mm2 BGI for IOP control. These results are in agreement with the present study results: no differences were found in vision preservation, IOP reduction, or decrease in number of glaucoma medications between the FP7 and FP8 AGV implants in adult eyes with glaucoma. Thus far, this is the only study comparing the surgical outcomes between FP7 and FP8 AGV implants in adult eyes.
Similar surgical outcomes between the FP7 and FP8 groups imply that the plate area may not be the major factor in determining surgical success, and it is likely that there is a maximal surface area beyond which there is minimal improvement in IOP control [17]. Kang and Kee [18] argued that there is an upper limit of the increase in the surface area at which the implants cease to have a beneficial effect on IOP, and it is inferred that the effect of IOP decrease does not depend on the area of filter cloth beyond a certain size. This phenomenon may be at least partly responsible for the lack of superior IOP reduction of the FP7 AGV implants compared to the FP8 AGV implants. Another possible explanation is the surgeon's perceived a priori likelihood of failure or complications, because the choice of implant is to some extent influenced by the severity of the glaucoma [14]. It is difficult to compare surgical success rates from different studies because of differences in study design, populations studied, types of implants used, and lengths of follow-up periods. Variable success rates of AGV implantation have been reported and range between 64.5% and 95.0%, with follow-up periods of 6 to 24 months [19,20]. A success rate of 80% was obtained by Hu et al. [6] with FP7 after a follow-up of 6 months and 78% was reported by Coleman et al. [9], with FP7 after a follow-up of 12 months. In addition, a success rate of 96% was obtained with the FP7 implant after a follow-up of 12 months [11]. These results are similar to the results Ishida et al. [21] reported: a 94.2% success rate with FP7 implant at 12 months. In 40 eyes from 40 patients with different types of refractory glaucoma, a 92.5% success rate was reported with both FP7 and FP8 after a follow-up period of 6 months [22]. Unfortunately, this study did not report separate success rates between FP7 and FP8 groups. Although materials vary, a 53.8% success rate was reported with the 96 mm2 AGV (model S3, New World Medical Inc.) and a 92.3% success rate was reported with the 184 mm2 AGV (model S3, New World Medical Inc.) after a follow-up period of 10 months [23].
In the present study, the success rates were 79.2% for the FP8 group and 72.7% for the FP7 group at the 3-year follow-up, which are comparable with the success rates of other studies. In adult eyes, FP7 AGV implantation is preferred. However, in conditions with conjunctival scarring or limited subconjunctival space, FP7 AGV implantation is challenging. In addition, an oversized implant can result in various complications, including implant exposure, extrusion, discomfort, and motility defects [19]. Given that FP7 and FP8 AGV implants did not show differences in surgical outcomes, we suggest that FP8 implantation may be a useful surgical option for IOP control in adult eyes with insufficient conjunctival or subconjunctival areas. This option may be especially useful for special circumstances in Asian eyes since small globes are common in this population [24].
To compare surgical outcomes between FP7 and FP8 AGV implants, randomization of subjects who underwent AGV implantation may be ideal. However, in the present study, the type of AGV was chosen per the surgeon's clinical judgment without randomization. Therefore, the possibility of selection bias remains. Other limitations include a relatively small sample size and limited follow-up period. Long-term, prospective, randomized, patient-, and investigator-masked studies are needed to confirm the results of this study.
In conclusion, FP7 and FP8 AGV implants showed no difference in terms of preservation of vision, IOP reduction, or decrease in the number of required glaucoma medications. The FP8 AGV implant appears to be a viable option for the management of refractory glaucoma in adult eyes with conjunctival scarring or limited subconjunctival space owing to the previous ocular surgeries, inflammatory ocular disorders, or small eyes.
Acknowledgements
This study was supported by Kim's Eye Hospital Research Center.
Footnotes
This work has been presented in part as a poster at the 2012 Joint Meeting of the Asia-Pacific Academy of Ophthalmology and European Society of Ophthalmology (Busan, Korea).
No potential conflict of interest relevant to this article was reported.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen RC, Bellows AR, Hutchinson BT, Murphy SD. Filtration surgery in the treatment of neovascular glaucoma. Ophthalmology. 1982;89:1181–1187. doi: 10.1016/s0161-6420(82)34672-2. [DOI] [PubMed] [Google Scholar]
- 3.Heuer DK, Gressel MG, Parrish RK, 2nd, et al. Trabeculectomy in aphakic eyes. Ophthalmology. 1984;91:1045–1051. doi: 10.1016/s0161-6420(84)34196-3. [DOI] [PubMed] [Google Scholar]
- 4.Syed HM, Law SK, Nam SH, et al. Baerveldt-350 implant versus Ahmed valve for refractory glaucoma: a case-controlled comparison. J Glaucoma. 2004;13:38–45. doi: 10.1097/00061198-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Taglia DP, Perkins TW, Gangnon R, et al. Comparison of the Ahmed glaucoma valve, the Krupin eye valve with disk, and the double-plate Molteno implant. J Glaucoma. 2002;11:347–353. doi: 10.1097/00061198-200208000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Hu CH, Lee YG, Hong YJ. Ahmed glaucoma valve implant in refractory glaucoma. J Korean Ophthalmol Soc. 1997;38:259–266. [Google Scholar]
- 7.Zorab A. The reduction of tension in chronic glaucoma. Ophthalmoscope. 1912;10:258–261. [Google Scholar]
- 8.Souza C, Tran DH, Loman J, et al. Long-term outcomes of Ahmed glaucoma valve implantation in refractory glaucomas. Am J Ophthalmol. 2007;144:893–900. doi: 10.1016/j.ajo.2007.07.035. [DOI] [PubMed] [Google Scholar]
- 9.Coleman AL, Hill R, Wilson MR, et al. Initial clinical experience with the Ahmed glaucoma valve implant. Am J Ophthalmol. 1995;120:23–31. doi: 10.1016/s0002-9394(14)73755-9. [DOI] [PubMed] [Google Scholar]
- 10.Kaya M, Ozbek Z, Yaman A, Durak I. Long-term success of ahmed glaucoma valve in refractory glaucoma. Int J Ophthalmol. 2012;5:108–112. doi: 10.3980/j.issn.2222-3959.2012.01.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hinkle DM, Zurakowski D, Ayyala RS. A comparison of the polypropylene plate Ahmed glaucoma valve to the silicone plate Ahmed glaucoma flexible valve. Eur J Ophthalmol. 2007;17:696–701. doi: 10.1177/112067210701700502. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz KS, Lee RK, Gedde SJ. Glaucoma drainage implants: a critical comparison of types. Curr Opin Ophthalmol. 2006;17:181–189. doi: 10.1097/01.icu.0000193080.55240.7e. [DOI] [PubMed] [Google Scholar]
- 13.Heuer DK, Lloyd MA, Abrams DA, et al. Which is better? One or two? A randomized clinical trial of single-plate versus double-plate Molteno implantation for glaucomas in aphakia and pseudophakia. Ophthalmology. 1992;99:1512–1519. doi: 10.1016/s0161-6420(92)31772-5. [DOI] [PubMed] [Google Scholar]
- 14.Seah SK, Gazzard G, Aung T. Intermediate-term outcome of Baerveldt glaucoma implants in Asian eyes. Ophthalmology. 2003;110:888–894. doi: 10.1016/S0161-6420(03)00088-5. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd MA, Baerveldt G, Fellenbaum PS, et al. Intermediate-term results of a randomized clinical trial of the 350- versus the 500-mm2 Baerveldt implant. Ophthalmology. 1994;101:1456–1463. doi: 10.1016/s0161-6420(94)31152-3. [DOI] [PubMed] [Google Scholar]
- 16.Britt MT, LaBree LD, Lloyd MA, et al. Randomized clinical trial of the 350-mm2 versus the 500-mm2 Baerveldt implant: longer term results: is bigger better? Ophthalmology. 1999;106:2312–2318. doi: 10.1016/S0161-6420(99)90532-8. [DOI] [PubMed] [Google Scholar]
- 17.Hong CH, Arosemena A, Zurakowski D, Ayyala RS. Glaucoma drainage devices: a systematic literature review and current controversies. Surv Ophthalmol. 2005;50:48–60. doi: 10.1016/j.survophthal.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 18.Kang SH, Kee C. The effectiveness of surface area extension with pericardial membrane in Ahmed glaucoma valve implant surgery. J Korean Ophthalmol Soc. 2002;43:2196–2201. [Google Scholar]
- 19.Smith SL, Starita RJ, Fellman RL, Lynn JR. Early clinical experience with the Baerveldt 350-mm2 glaucoma implant and associated extraocular muscle imbalance. Ophthalmology. 1993;100:914–918. doi: 10.1016/s0161-6420(93)31554-x. [DOI] [PubMed] [Google Scholar]
- 20.Kook MS, Jeon SK, Kim MJ, Yoon YH. Combined pars plana vitrectomy and Ahmed implantation for refractory glaucoma. J Korean Ophthalmol Soc. 1998;39:559–565. [Google Scholar]
- 21.Ishida K, Netland PA, Costa VP, et al. Comparison of polypropylene and silicone Ahmed glaucoma valves. Ophthalmology. 2006;113:1320–1326. doi: 10.1016/j.ophtha.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 22.Mokbel TH, Khalaf MA, El-Khouly SE, El-Metwally NO. Flexible Ahmed valve for selected cases of refractory glaucoma. Eur J Ophthalmol. 2012;22:83–89. doi: 10.5301/ejo.5000003. [DOI] [PubMed] [Google Scholar]
- 23.Oh SJ, Kim IS, Hong YJ, et al. Comparison of short-term surgical outcomes of Ahmed glaucoma valve implant between 96 mm2 and 184 mm2 of the surface area. J Korean Ophthalmol Soc. 2004;45:1872–1879. [Google Scholar]
- 24.Law RW, Li RT, Lai JS, et al. Modification of an adult-sized Ahmed glaucoma valve for a small globe. Jpn J Ophthalmol. 2006;50:67–68. doi: 10.1007/s10384-005-0265-1. [DOI] [PubMed] [Google Scholar]