Abstract
Background/Aims
Left-sided diverticulitis is increasing in Japan, and many studies report that left-sided diverticulitis is more likely to be severe. Therefore, it is important to identify the features and risk factors for left-sided diverticulitis. We hypothesized that left-sided diverticulitis in Japan is related to obesity and conducted a study of the features and risk factors for this disorder in Japan.
Methods
Right-sided diverticulitis and left-sided diverticulitis patients (total of 215) were compared with respect to background, particularly obesity-related factors to identify risk factors for diverticulitis.
Results
There were 166 (77.2%) right-sided diverticulitis patients and 49 (22.8%) left-sided diverticulitis patients. The proportions of obese patients (body mass index ≥25 kg/m2, p=0.0349), viscerally obese patients (visceral fat area ≥100 cm2, p=0.0019), patients of mean age (p=0.0003), and elderly patients (age ≥65 years, p=0.0177) were significantly higher in the left-sided-diverticulitis group than in the right-sided-diverticulitis group. The proportion of viscerally obese patients was significantly higher in the left-sided-diverticulitis group than in the left-sided-diverticulosis group (p=0.0390).
Conclusions
This study showed that obesity, particularly visceral obesity, was a risk factor for left-sided diverticulitis in Japan.
Keywords: Diverticulitis, Epidemiology, Risk, Obesity
INTRODUCTION
Diverticular disease of the colon is common in both Western countries and Japan. In the past, colonic diverticulosis was rare in Japan; with detection rates as low as approximately 2% in 1960.1 However, the detection rate increased to approximately 20% in the 1980s and 1990s.2 Studies have reported that increasing rates of diverticulosis are caused by westernization of the diet.3,4 Generally, in Western countries diverticulosis is predominantly found on the left side (sigmoid colon, descending colon, and left portion of the transverse colon), but in Asia it is usually found on the right side (cecum, ascending colon, and right portion of the transverse colon).1,4 Right-sided diverticulosis (R-control) in Japan depends to a large extent on congenital factors.5 However, this trend has been changing and today, diverticulosis is increasing and spreading from right-sided to bilateral in Japan.2 Thus, there has been a relative increase in the number of patients with left-sided diverticulosis (L-control) in Japan. Ten to twenty-five percent of patients with known diverticulosis progress to diverticulitis.6 As a result, in Japan, contrary to Western countries, we must be aware of not only right-sided diverticulitis (RD), but also left-sided diverticulitis (LD). We make a clear distinction between RD and LD because the location of diverticulitis is important. Many studies have reported that LD is more likely to be severe, compared with RD.7-10 On the other hand, in Asia, conservative management with bowel rest and antibiotics is considered a safe and effective option for treating right-sided colonic diverticulitis.11,12 Therefore, the features and risk factors for LD need clarification. In Western countries, there are reports that obesity and diverticulitis are related13-20 and, in Western countries, LD occurs most frequently compared with a higher frequency of RD in Asia. Therefore, we hypothesized that obesity was a risk factor for developing LD in Japan. Usually, obesity refers to an excess of body fat, which can be divided into subcutaneous and visceral fat. Visceral fat is highlighted as a cause of metabolic complications such as hypertriglyceridemia, insulin resistance.21,22 Then, a lot of studies showed the relationship between visceral fat and colorectal disease. For example, some study showed the association between waist circumferences and large or advanced adenoma.23-25 In addition, one study showed a strong association between colorectal adenoma and visceral fat measured by computerized tomography scanning.26 Previous report showed that visceral fat which is estimated from waist circumference is influenced by age, gender, and racial.27 Therefore, computerized tomography scanning was useful to more accurately assess the visceral fat without influence of age, gender, and race.
In the field of acute colonic diverticulitis, one report showed the relationship between visceral obesity and development of diverticulitis.13 However, this report evaluated by means of indirect indicator such as waist-to-hip ratios or waist circumference and didn't directly measure visceral fat.13 Therefore, we measured visceral fat directly by abdominal computerized tomography scanning in order to more accurately assess it. Based on the results, we conducted a study about the relationship between obesity and development of LD in Japan.
MATERIALS AND METHODS
1. Patients
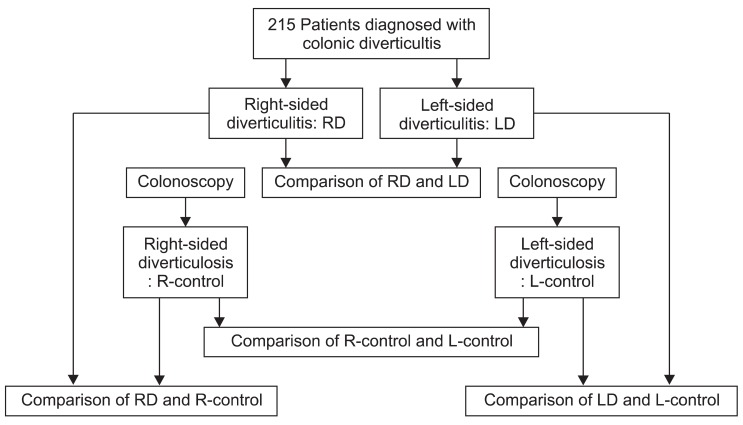
The study design was a multicenter retrospective and matched case-control study, conducted in five centers (Yokohama City University Hospital, Machida Municipal Hospital, Chigasaki Municipal Hospital, Yokosuka City Hospital, and Tokyo Metropolitan Hiroo General Hospital). The flow diagram of this study is shown in Fig. 1. The subjects were consecutive Japanese patients diagnosed with colonic diverticulitis between October 2006 and October 2011 at each center. Diagnosis of acute diverticulitis was made based on the following criteria: acute abdominal pain localized to the right/left side of the abdomen, increased serum inflammatory parameters (leukocytes, C-reactive protein) and/or fever, and computed tomography (CT) findings (localized colonic diverticular wall thickening and/or infiltration of pericolonic fat with no evidence of enlarged appendix). Patients were confirmed the presence of a colonic diverticulum by colonoscopy after treatment or previous colonoscopic examination. Patients who couldn't confirm the presence of colonic diverticulum by colonoscopy or patients who didn't undergo colonoscopy were excluded. Patients with a history of colonic resection, steroid therapy, nonsteroidal anti-inflammatory drug use, cancer, or inflammatory bowel disease were excluded from this study. The study was conducted with the approval of the Ethics Committee of Yokohama City University.
Fig. 1.
Flow diagram of this study.
2. Data collection
A standardized sheet was used to collect data, including location of diverticulitis, age, gender, body mass index (BMI), blood lipid profile (total cholesterol, TC; low density lipoprotein, LDL; triglyceride, TG), alcohol habits, and smoking habits. Abdominal CT data were used to measure visceral and subcutaneous fat. Visceral fat area (VFA) and subcutaneous fat area (SFA) were measured by Fat Scan V5.0 (East Japan Institute of Technology Co., Ltd., Ibaraki, Japan) at the level of the umbilicus. Adipose tissue was determined by setting the attenuation level from -190 to -30 Hounsfield units. VFA and SFA were determined separately using a trace function, which manually defined the boundary between the visceral and subcutaneous fat using a cursor.28
3. Control group
We conducted a matched case-control study to analyze the features and risk factors for diverticulitis. For each side of diverticulitis, a patient with multiple R-control or L-control with no history of colonic diverticulitis was selected as a control subject based on colonoscopy findings, exactly matched for age and gender. The reasons for colonoscopy were: diarrhea, constipation, abdominal pain, and a family history of colonic cancer. Records were reviewed and data collected as described.
4. Definition of obesity
Patients were classified as obese or viscerally obese using both BMI and VFA criteria. BMI was calculated, and obese patients were defined as those with a BMI ≥25 kg/m2 in accordance with the criteria of the Japan Society for the Study of Obesity.29 Additionally, we defined visceral obesity as VFA ≥100 cm2 in accordance with the criteria of the Japan Society for the Study of Obesity.29 This threshold value has been previously proven to be associated with elevated cardiovascular risk and with a substantial deterioration of metabolic variables predictive of metabolic syndrome.30
5. Statistical analysis
Statistical analysis was performed using Excel-Toukei 2010 software for Windows (Social Survey Research Information Co., Ltd., Tokyo, Japan). The Student t-test, Welch t-test, and Mann-Whitney U test were used to assess significant differences between the RD and LD groups, and LD and control groups. A p<0.05 was considered statistically significant.
RESULTS
1. Background of the subjects
A total of 215 patients were enrolled in this study (137 male [63.7%] and 78 female [36.3%]). The mean age was 46.2 years. The clinical characteristics of the patients with RD (n=166, 77.2%) and LD (n=49, 22.8%) are shown in Table 1. The mean age of LD patients was older than that of RD patients (52.9 years vs 44.2 years, p<0.001). The ratio of aged patients (age ≥65 years) (9.6% vs 22.4%, p<0.05) was significantly greater in the LD group compared with the RD group. Sex ratio (p=0.7933) revealed no significant difference between the two groups. Table 2 shows the characteristics of the patients with R-control and the patients with L-control.
Table 1.
Clinical Characteristics of Patients with Right-Sided Diverticulitis and Left-Sided Diverticulitis
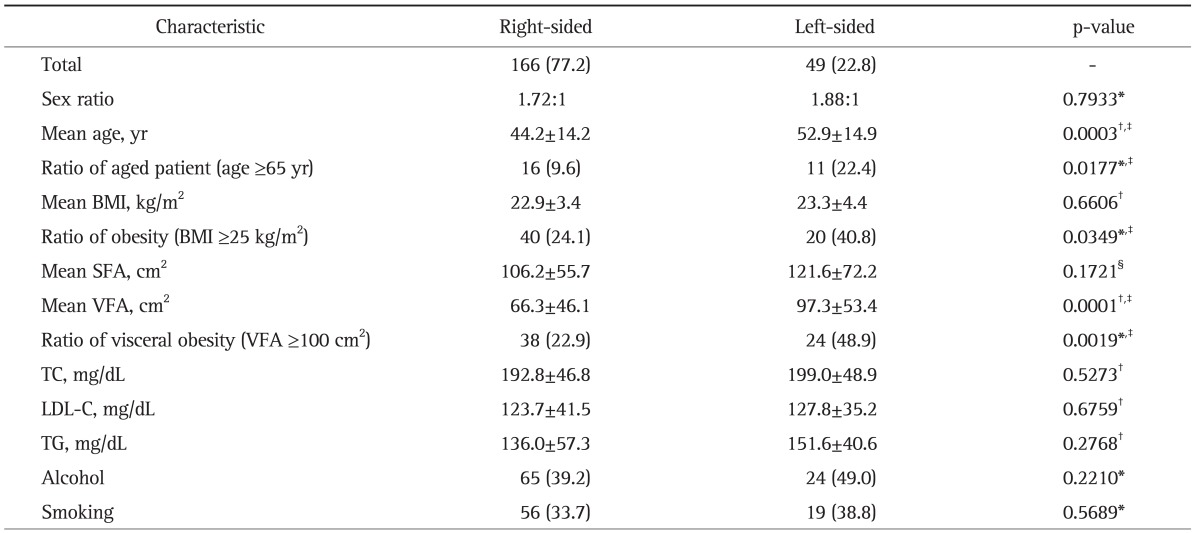
Data are presented as number (%) or mean±SD.
BMI, body mass index; SFA, subcutaneous fat area; VFA, visceral fat area; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; TG, triglycerides.
*Mann-Whitney U test; †Student t-test; ‡p<0.05; §Welch t-test.
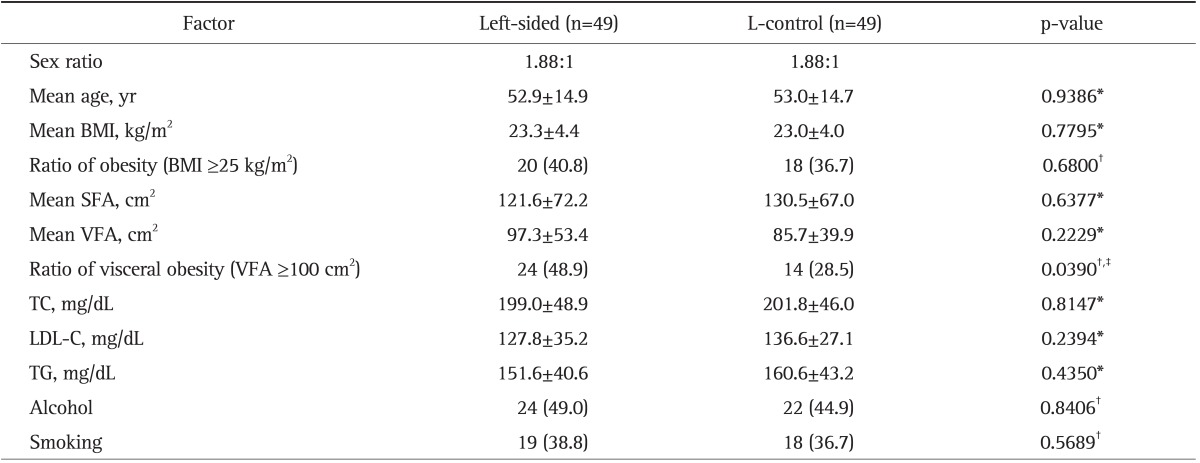
Table 2.
Clinical Characteristics of Patients with Right-Sided Diverticulosis (R-Control) and Left-Sided Diverticulosis (L-Control)
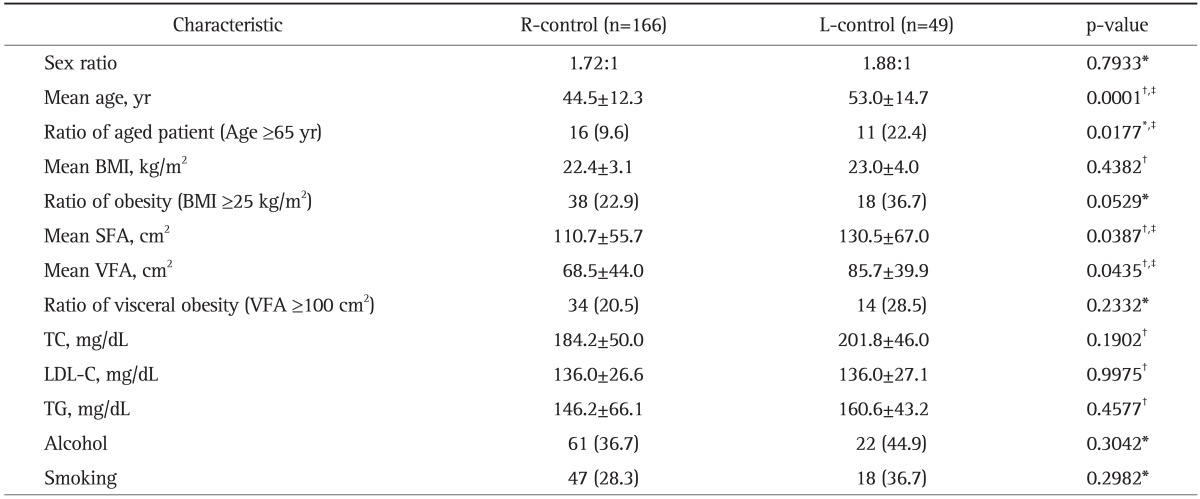
Data are presented as mean±SD or number (%).
BMI, body mass index; SFA, subcutaneous fat area; VFA, visceral fat area; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; TG, triglycerides.
*Mann-Whitney U test; †Student t-test; ‡p<0.05.
2. Comparison of right-sided and LD
Table 1 shows the characteristics of the RD and LD groups for obesity-related factors. Mean BMI (p=0.6606), mean SFA (p=0.1721), TC (p=0.5273), LDL (p=0.6759), TG (p=0.2768), alcohol habits (p=0.2210), and smoking habits (p=0.5689) were not significantly different between the two groups. Mean VFA (66.3±46.1 cm2 vs 97.3±53.4 cm2, p<0.001), the ratio of obesity (BMI ≥25 kg/m2) (24.1% vs. 40.8%, p<0.05) and the ratio of visceral obesity (VFA ≥100 cm2) (22.9% vs. 48.9%, p<0.001) were significantly greater in the LD group than in the RD group.
3. Comparison of R-control and L-control
Table 2 shows the characteristics of the R-control and L-control groups for obesity-related factors. Mean BMI (p=0.4382), the ratio of obesity (BMI ≥25 kg/m2) (p=0.0529) and the ratio of visceral obesity (VFA ≥100 cm2) (p=0.2332), TC (p=0.1902), LDL (p=0.9975), TG (p=0.4577), alcohol habits (p=0.3042), and smoking habits (p=0.2982) revealed no significant differences between the two groups. Mean VFA (68.5±44.0 cm2 vs 85.7±39.9 cm2, p<0.05), and mean SFA (110.7±55.7 cm2 vs 130.5±67.0 cm2, p<0.05) were significantly greater in the L-control group than in the R-control group.
4. Comparison of right-side diverticulitis and R-control
Table 3 shows the obesity-related factors for the RD and R-control groups. Mean BMI (p=0.3020), the ratio of obesity (BMI ≥25 kg/m2) (p=0.7960), mean SFA (p=0.4557), mean VFA (p=0.6607), the ratio of visceral obesity (VFA ≥100 cm2) (p=0.5956), TC (p=0.3917), LDL (p=0.1898), TG (p=0.6373), alcohol habits (p=0.6515), and smoking habits (p=0.2864) were not significantly different between the two groups.
Table 3.
Obesity-Related Factors of Patients with Right-Sided Diverticulitis and Right-Sided Diverticulosis (R-Control)
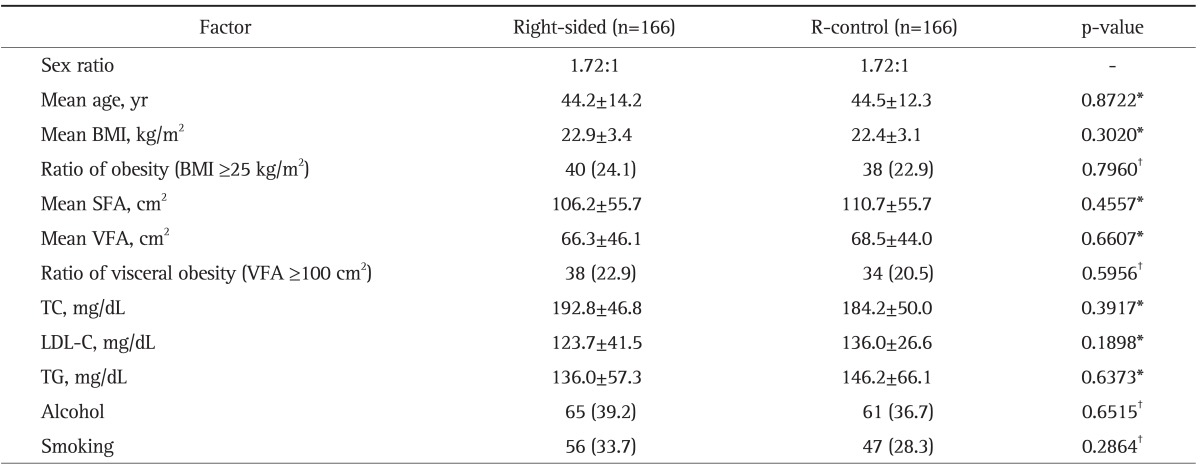
Data are presented as mean±SD or number (%).
BMI, body mass index; SFA, subcutaneous fat area; VFA, visceral fat area; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; TG, triglycerides.
*Student t-test; †Mann-Whitney U test.
5. Comparison of left-side diverticulitis and L-control
Table 4 shows the obesity-related factors of the LD and L-control groups. Mean BMI (p=0.7795), the ratio of obesity (BMI ≥25 kg/m2) (p=0.6800), mean SFA (p=0.6377), mean VFA (p=0.2229), TC (p=0.8147), LDL (p=0.2394), TG (p=0.4350), alcohol habits (p=0.8406), and smoking habits (p=0.5689) showed no significant differences between the two groups. The ratio of visceral obesity (VFA ≥100 cm2; 48.9% vs 28.5%, p<0.05) was significantly greater in the LD group compared with the L-control group.
Table 4.
Obesity-Related Factors of Patients with Left-Sided Diverticulitis and Left-Sided Diverticulosis (L-Control)
Data are presented as mean±SD or number (%).
BMI, body mass index; SFA, subcutaneous fat area; VFA, visceral fat area; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; TG, triglycerides.
*Student t-test; †Mann-Whitney U test; ‡p<0.05.
DISCUSSION
This study showed that visceral obesity was a risk factor for LD. However, a similar trend was not seen for RD. There are many reports showing a relationship between visceral obesity and gastroenterological disease.31-33 The most critical link between visceral fat and these diseases is chronic inflammation. Adipose tissue secretes a number of cytokines, such as tumor necrosis factor-a and interleukin-6 known to participate in local and generalized inflammation.34 Therefore, visceral fat may enhance or precipitate the inflammatory process in diverticulitis. Inflammation related to visceral obesity may be more likely to occur on the left rather than the right side due to greater bacterial numbers.35 However, the precise mechanism is still unclear and is an area for future research.
The ratio of visceral obesity (VFA ≥100 cm2) was significantly greater in the LD group than in the L-control group. On the other hand, the ratio of BMI ≥25 kg/m2 revealed no significant difference between the two groups. BMI has been used as one of the most reliable anthropometric indices of obesity and is simple to calculate. However, even though BMI is a readily available objective measurement, it is not a reliable method of measuring fat, particularly visceral fat.36,37 This study also showed that the ratio of aged patients (age ≥65 years) and mean age were significantly greater in the LD group compared with the RD group. This result may have been influenced by the fact that L-control increases with age in Japan.2 In addition, our data showed that VFA was significantly higher in the L-control groups than the R-control groups suggesting that visceral fat may be related to not only the development of LD but also to the development of L-control.
This study also showed that 22.4% of patients with LD were aged patients (age ≥65 years). Japan is an aging society with the highest proportion of over 65-year-old in the world; 22.1% in 2008. The aging rate will continue to rise in the future with the numbers of aged LD patients in Japan expected to increase as well.38 Previous studies reported a high mortality rate in aged patients with diverticulitis.39,40 Therefore, LD prevention in aged patients is important. This study showed a relationship between visceral obesity and LD. Therefore, reducing visceral fat may prevent the development of LD. A limitation of this study is that colonoscopy cannot detect diverticulosis any better than a barium enema. Additionally, the size of the study population was small, and even though it was a multicenter study, the results do not represent the entire Japanese population. Larger scale studies are needed.
Thus far, some studies showed the correlation between obesity and diverticulitis (Table 5).13,14,20,41 However, most studies were conducted in Western countries. In Asia, there are few reports that show the relationship between obesity and diverticulitis. Jeong et al.41 showed that visceral obesity was significantly associated with complications of diverticulitis such as perforation or abscess. On the other hand, our data showed that visceral obesity was a risk factor for development of diverticulitis for the first time in Asia. Then, as a review method, we used control patient for evaluation of obesity. The patients with diverticulosis but without diverticulitis were selected as a control. This review method is also novel.
Table 5.
Previous Major Reports That Showed the Correlation between Obesity and Diverticulitis
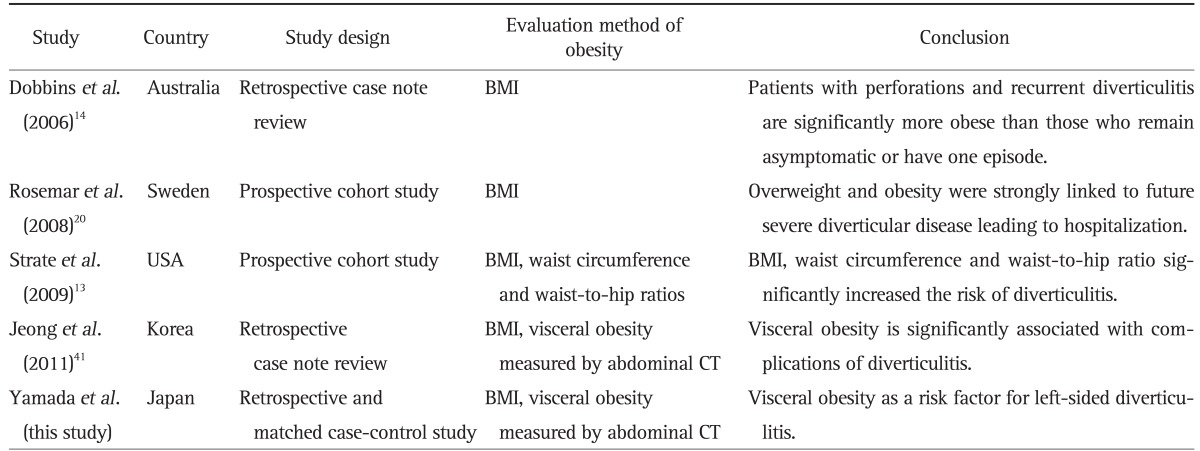
BMI, body mass index; CT, computed tomography.
In summary, our results suggest that visceral obesity is associated with an increased risk of LD and, therefore, reducing visceral fat has the potential to prevent LD. In Japan, severe cases were more frequent in the LD group compared with the RD group and the number of LD patients is expected to increase as the population ages. Clarifying the risk factors and features of LD is necessary to establish effective prevention and treatment programs.
ACKNOWLEDGEMENTS
The authors would like to thank the staff of the participating institutions for their support in recruiting eligible patients and also the patients who participated in this study.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Inoue M. The epidemiologic and clinical features of diverticular disease of the colon. J Jpn Soc Coloproctol. 1992;45:904–913. [Google Scholar]
- 2.Miura S, Kodaira S, Aoki H, Hosoda Y. Bilateral type diverticular disease of the colon. Int J Colorectal Dis. 1996;11:71–75. doi: 10.1007/BF00342463. [DOI] [PubMed] [Google Scholar]
- 3.Ohi G, Minowa K, Oyama T, et al. Changes in dietary fiber intake among Japanese in the 20th century: a relationship to the prevalence of diverticular disease. Am J Clin Nutr. 1983;38:115–121. doi: 10.1093/ajcn/38.1.115. [DOI] [PubMed] [Google Scholar]
- 4.Aldoori W, Ryan-Harshman M. Preventing diverticular disease. Review of recent evidence on high-fibre diets. Can Fam Physician. 2002;48:1632–1637. [PMC free article] [PubMed] [Google Scholar]
- 5.Nakaji S, Danjo K, Munakata A, et al. Comparison of etiology of right-sided diverticula in Japan with that of left-sided diverticula in the West. Int J Colorectal Dis. 2002;17:365–373. doi: 10.1007/s00384-002-0403-x. [DOI] [PubMed] [Google Scholar]
- 6.Parra-Blanco A. Colonic diverticular disease: pathophysiology and clinical picture. Digestion. 2006;73(Suppl 1):47–57. doi: 10.1159/000089779. [DOI] [PubMed] [Google Scholar]
- 7.Kim SH, Byun CG, Cha JW, Choi SH, Kho YT, Seo DY. Comparative study of the clinical features and treatment for right and left colonic diverticulitis. J Korean Soc Coloproctol. 2010;26:407–412. doi: 10.3393/jksc.2010.26.6.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim JH, Cheon JH, Park S, et al. Relationship between disease location and age, obesity, and complications in Korean patients with acute diverticulitis: a comparison of clinical patterns with those of Western populations. Hepatogastroenterology. 2008;55:983–986. [PubMed] [Google Scholar]
- 9.Choi KS, Byeon JS, Yoon SM, et al. Diverticulitis: focused on clinical course and relapse. Intest Res. 2008;6:37–44. [Google Scholar]
- 10.Lee HC, Jeon SW, Kim SY, et al. Clinical characteristics of right versus left colonic diverticulitis. Korean J Med. 2008;75:533–538. [Google Scholar]
- 11.Kim MR, Kye BH, Kim HJ, Cho HM, Oh ST, Kim JG. Treatment of right colonic diverticulitis: the role of nonoperative treatment. J Korean Soc Coloproctol. 2010;26:402–406. doi: 10.3393/jksc.2010.26.6.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matsushima K. Management of right-sided diverticulitis: a retrospective review from a hospital in Japan. Surg Today. 2010;40:321–325. doi: 10.1007/s00595-008-4055-5. [DOI] [PubMed] [Google Scholar]
- 13.Strate LL, Liu YL, Aldoori WH, Syngal S, Giovannucci EL. Obesity increases the risks of diverticulitis and diverticular bleeding. Gastroenterology. 2009;136:115–122. doi: 10.1053/j.gastro.2008.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dobbins C, Defontgalland D, Duthie G, Wattchow DA. The relationship of obesity to the complications of diverticular disease. Colorectal Dis. 2006;8:37–40. doi: 10.1111/j.1463-1318.2005.00847.x. [DOI] [PubMed] [Google Scholar]
- 15.Konvolinka CW. Acute diverticulitis under age forty. Am J Surg. 1994;167:562–565. doi: 10.1016/0002-9610(94)90098-1. [DOI] [PubMed] [Google Scholar]
- 16.Mader TJ. Acute diverticulitis in young adults. J Emerg Med. 1994;12:779–782. doi: 10.1016/0736-4679(94)90483-9. [DOI] [PubMed] [Google Scholar]
- 17.Schauer PR, Ramos R, Ghiatas AA, Sirinek KR. Virulent diverticular disease in young obese men. Am J Surg. 1992;164:443–446. doi: 10.1016/s0002-9610(05)81177-8. [DOI] [PubMed] [Google Scholar]
- 18.Schweitzer J, Casillas RA, Collins JC. Acute diverticulitis in the young adult is not "virulent". Am Surg. 2002;68:1044–1047. [PubMed] [Google Scholar]
- 19.Zaidi E, Daly B. CT and clinical features of acute diverticulitis in an urban U.S. population: rising frequency in young, obese adults. AJR Am J Roentgenol. 2006;187:689–694. doi: 10.2214/AJR.05.0033. [DOI] [PubMed] [Google Scholar]
- 20.Rosemar A, Angerås U, Rosengren A. Body mass index and diverticular disease: a 28-year follow-up study in men. Dis Colon Rectum. 2008;51:450–455. doi: 10.1007/s10350-007-9172-5. [DOI] [PubMed] [Google Scholar]
- 21.Arner P. Differences in lipolysis between human subcutaneous and omental adipose tissues. Ann Med. 1995;27:435–438. doi: 10.3109/07853899709002451. [DOI] [PubMed] [Google Scholar]
- 22.Dusserre E, Moulin P, Vidal H. Differences in mRNA expression of the proteins secreted by the adipocytes in human subcutaneous and visceral adipose tissues. Biochim Biophys Acta. 2000;1500:88–96. doi: 10.1016/s0925-4439(99)00091-5. [DOI] [PubMed] [Google Scholar]
- 23.Giovannucci E, Ascherio A, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Intern Med. 1995;122:327–334. doi: 10.7326/0003-4819-122-5-199503010-00002. [DOI] [PubMed] [Google Scholar]
- 24.Giovannucci E, Colditz GA, Stampfer MJ, Willett WC. Physical activity, obesity, and risk of colorectal adenoma in women (United States) Cancer Causes Control. 1996;7:253–263. doi: 10.1007/BF00051301. [DOI] [PubMed] [Google Scholar]
- 25.Shinchi K, Kono S, Honjo S, et al. Obesity and adenomatous polyps of the sigmoid colon. Jpn J Cancer Res. 1994;85:479–484. doi: 10.1111/j.1349-7006.1994.tb02383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Otake S, Takeda H, Suzuki Y, et al. Association of visceral fat accumulation and plasma adiponectin with colorectal adenoma: evidence for participation of insulin resistance. Clin Cancer Res. 2005;11:3642–3646. doi: 10.1158/1078-0432.CCR-04-1868. [DOI] [PubMed] [Google Scholar]
- 27.Carroll JF, Chiapa AL, Rodriquez M, et al. Visceral fat, waist circumference, and BMI: impact of race/ethnicity. Obesity (Silver Spring) 2008;16:600–607. doi: 10.1038/oby.2007.92. [DOI] [PubMed] [Google Scholar]
- 28.Yoshizumi T, Nakamura T, Yamane M, et al. Abdominal fat: standardized technique for measurement at CT. Radiology. 1999;211:283–286. doi: 10.1148/radiology.211.1.r99ap15283. [DOI] [PubMed] [Google Scholar]
- 29.Examination Committee of Criteria for 'Obesity Disease' in Japan; Japan Society for the Study of Obesity. New criteria for 'obesity disease' in Japan. Circ J. 2002;66:987–992. doi: 10.1253/circj.66.987. [DOI] [PubMed] [Google Scholar]
- 30.Hiuge-Shimizu A, Kishida K, Funahashi T, et al. Coexistence of visceral fat and multiple risk factor accumulations is strongly associated with coronary artery disease in Japanese (the VACATION-J study) J Atheroscler Thromb. 2012;19:657–663. doi: 10.5551/jat.13037. [DOI] [PubMed] [Google Scholar]
- 31.Erarslan E, Turkay C, Koktener A, Koca C, Uz B, Bavbek N. Association of visceral fat accumulation and adiponectin levels with colorectal neoplasia. Dig Dis Sci. 2009;54:862–868. doi: 10.1007/s10620-008-0440-6. [DOI] [PubMed] [Google Scholar]
- 32.Oh TH, Byeon JS, Myung SJ, et al. Visceral obesity as a risk factor for colorectal neoplasm. J Gastroenterol Hepatol. 2008;23:411–417. doi: 10.1111/j.1440-1746.2007.05125.x. [DOI] [PubMed] [Google Scholar]
- 33.Nam SY, Choi IJ, Ryu KH, Park BJ, Kim HB, Nam BH. Abdominal visceral adipose tissue volume is associated with increased risk of erosive esophagitis in men and women. Gastroenterology. 2010;139:1902–1911. doi: 10.1053/j.gastro.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 34.Watanabe S, Hojo M, Nagahara A. Metabolic syndrome and gastrointestinal diseases. J Gastroenterol. 2007;42:267–274. doi: 10.1007/s00535-007-2033-0. [DOI] [PubMed] [Google Scholar]
- 35.Rambaud JC. Bacterial ecology of the digestive tract and defense of the body. Ann Gastroenterol Hepatol (Paris) 1992;28:263–266. [PubMed] [Google Scholar]
- 36.Camhi SM, Bray GA, Bouchard C, et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity (Silver Spring) 2011;19:402–408. doi: 10.1038/oby.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kok P, Seidell JC, Meinders AE. The value and limitations of the body mass index (BMI) in the assessment of the health risks of overweight and obesity. Ned Tijdschr Geneeskd. 2004;148:2379–2382. [PubMed] [Google Scholar]
- 38.Arai H. Geriatrics in the most aged country, Japan. Arch Gerontol Geriatr. 2009;49(Suppl 2):S1–S2. doi: 10.1016/S0167-4943(09)00302-1. [DOI] [PubMed] [Google Scholar]
- 39.Pessaux P, Muscari F, Ouellet JF, et al. Risk factors for mortality and morbidity after elective sigmoid resection for diverticulitis: prospective multicenter multivariate analysis of 582 patients. World J Surg. 2004;28:92–96. doi: 10.1007/s00268-003-7146-x. [DOI] [PubMed] [Google Scholar]
- 40.Morris CR, Harvey IM, Stebbings WS, Hart AR. Incidence of perforated diverticulitis and risk factors for death in a UK population. Br J Surg. 2008;95:876–881. doi: 10.1002/bjs.6226. [DOI] [PubMed] [Google Scholar]
- 41.Jeong JH, Lee HL, Kim JO, et al. Correlation between complicated diverticulitis and visceral fat. J Korean Med Sci. 2011;26:1339–1343. doi: 10.3346/jkms.2011.26.10.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]