Abstract
Background/Aims
In South Korea, health check-ups are readily accessible to the public. We aimed to compare the prevalence of upper gastrointestinal (GI) and lower GI diseases in Korean Americans and native Koreans to determine differences and risk factors.
Methods
In total, 1,942 subjects who visited Gangnam Severance Hospital from July 2008 to November 2010 for a health check-up were enrolled. Basic characteristics and laboratory data for the subjects were collected. Esophagogastroduodenoscopy and colonoscopy were performed. In total, 940 Korean Americans (group 1) and 1,002 native Koreans (group 2) were enrolled.
Results
The overall prevalence of GI diseases for each group (group 1 vs group 2) were as follows: reflux esophagitis (RE) (9.65% vs 7.9%), gastric ulcer (2.8% vs 3.4%), duodenal ulcer (2.3% vs 3.6%), gastric cancer (0.4% vs 0.3%), colorectal polyp (35.9% vs 35.6%), colorectal cancer (0.5% vs 0.5%), and hemorrhoids (29.4% vs 21.3%). The prevalence of hemorrhoids was significantly higher in group 1 than in group 2 (p=0.001). In the multivariable analysis of group 1, male sex, age over 50 years, hypercholesterolemia and hypertriglyceridemia predicted colorectal polyps. Male sex and high fasting glucose levels were associated with RE.
Conclusions
Our study showed that the prevalence of GI diseases (except hemorrhoids) in Korean Americans was similar to that observed in native Koreans. Therefore, the Korean guidelines for upper and lower screening endoscopy may be applicable to Korean Americans.
Keywords: Korean Americans, Screening endoscopy
INTRODUCTION
In Korea, incidences of cancer have increased rapidly with more than 178,000 people reported to have been diagnosed with cancer in 2009.1,2 To achieve early cancer screening for all Koreans, the Korean government established National Cancer Screening Program (NCSP) in 1999. The NCSP supported representatives of academic societies and developed Korean guidelines for cancer screening including stomach and colorectal cancer.3 According to these guidelines, esophagogastroduodenoscopy or upper gastrointestinal (GI) series is recommended to the people over 40 years old every 2 years.3 For colorectal cancer screening, an annual fecal occult blood test is recommended for those 50 years and older.3 Colonoscopy or double-contrast barium enema is recommened if the fecal occult blood test is positive.3 Beside this NCSP, private regular health check-up programs designed to detect common cancer and chronic noncommunicable diseases are readily accessible to the public in South Korea. With support from the Korean government for medical tourism, a large number of foreigners including Korean Americans visit South Korea to check their health status. Korean Americans constitute the fifth largest Asian American group with a population of about 1.25 million.4 Approximately 80% of them are foreign born such as South Korea.4 Unfortunately, American physicians have been insufficiently screening for gastric cancer and Korean American physicians are also reluctant to recommend colorectal cancer screening to the Korean Americans because of a lack of research.5,6
We wondered whether Korean Americans have similar rate of GI diseases when compared to native Koreans and the Korean guidelines for screening gastric and colorectal cancer can be applicable to Korean Americans.
The aim of this study is to explore the prevalence of GI diseases by endoscopy and possible associated factors in Korean Americans and native Koreans.
MATERIALS AND METHODS
1. Study population and data collection
We performed a cross-sectional study of examinees who participated in a health check up at Gangnam Severance Hospital, Yonsei University College of Medicine from July 2008 to November 2010. We gathered information on 1,000 Korean Americans who voluntarily visited South Korea to have their overall health status assessed through the health check-up program. Korean Americans were defined as Korean immigrants to the United States including first-generation parents and their children regardless of their nationality. The length of residency in America was asked via e-mail questionnaire retrospectively (n=598). Then, we selected age-gender matched native Koreans living in South Korea who underwent the same health assessment at our center during the same period. Written informed consent was obtained from all subjects for the procedures. The study protocol was approved by the ethics committee in Health Promotion Center, Gangnam Severance Hospital.
The basic checkup program was comprised of laboratory blood tests and an esophagogastroduodenoscopy. Continuous variables included systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose, total cholesterol, high density lipoprotein (HDL), low density lipoprotein (LDL), and triglyceride (TG). About two-thirds of the subjects received an optional colonoscopy to screen for colorectal disease, regardless of the results from occult blood testing of stool samples. Four expert gastroenterologists with 2 to 6 years of experience performed the upper and lower endoscopies. In addition, data concerning age, gender, and body mass index (BMI) were also collected. We assessed the data for all subjects and compared Korean Americans and native Koreans.
2. Definitions and assessment of variables
Reflux esophagitis (RE) was graded according to the Los Angeles classification system, and those of grades A to D were included in this study.7 Minimal changes such as erythema or blurring of the Z-line, were excluded because of low interobserver agreement.8 Gastric and duodenal ulcers were diagnosed endoscopically. Superficial gastritis or erosions were excluded. For gastric ulcers, multiple biopsy specimens were obtained to rule out malignancy. Based on colonoscopic findings, pathologically confirmed colorectal polyps, and malignancy were assessed. Benign nonneoplastic polyps such as hyperplastic and inflammatory polyps were excluded. Hemorrhoids included both internal and external types. Age was stratified into two groups, as <50 or ≥50 years. BMI was calculated from weight and height, and those with a BMI over 25 kg/m2 was defined obesity. High blood pressure was diagnosed if SBP ≥140 mm Hg or DBP ≥90 mm Hg. Lipid profiles were classified as high or low according to normal laboratory value as below, high cholesterol (total choletesterol level ≥240 mg/dL), high LDL (≥160 mg/dL), low HDL (<40 mg/dL), and high TG (≥200 mg/dL).
3. Statistical analysis
We compared the prevalences of diseases and categorical variables using chi-square test between Korean Americans and native Koreans. In each group, a multivariable logistic regression model was used to assess factors associated with each of the diseases. A p<0.05 was considered statistically significant. All statistical analyses were performed with the use of the SAS statistical software package version 9.2 (SAS Inc., Cary, NC, USA).
RESULTS
1. Patient characteristics and laboratory results
During the study period, 1,000 Korean Americans visited our center for a health check-up and 1,002 native Koreans were selected as age-gender matched controls. Among them, 60 Korean Americans were excluded because they did not undergo an upper endoscopy. Finally, a total of 1,942 subjects were enrolled and about two-thirds of them (n=1,305) underwent colonoscopy. The mean age of the Korean Americans was 53.5±8.5 and the male to female ratio was 45.6:54.4. Mean duration of residency in America was 24.3±9.6 years among those who answered the e-mail questionnaire (n=146/598; recovery rate, 24.4%). The mean BMI of the Korean Americans was 23.3±3.2 kg/m2. The proportions of the older age group (≥50 years), subjects with obesity, high fasting glucose level, high cholesterol, high LDL, and high TG were not significantly different between two groups (Table 1). High blood pressure is more frequent in Korean Americans (p=0.011) but low HDL was more prevalent in native Koreans (p=0.045).
Table 1.
Characteristics of Korean Americans and Native Koreans
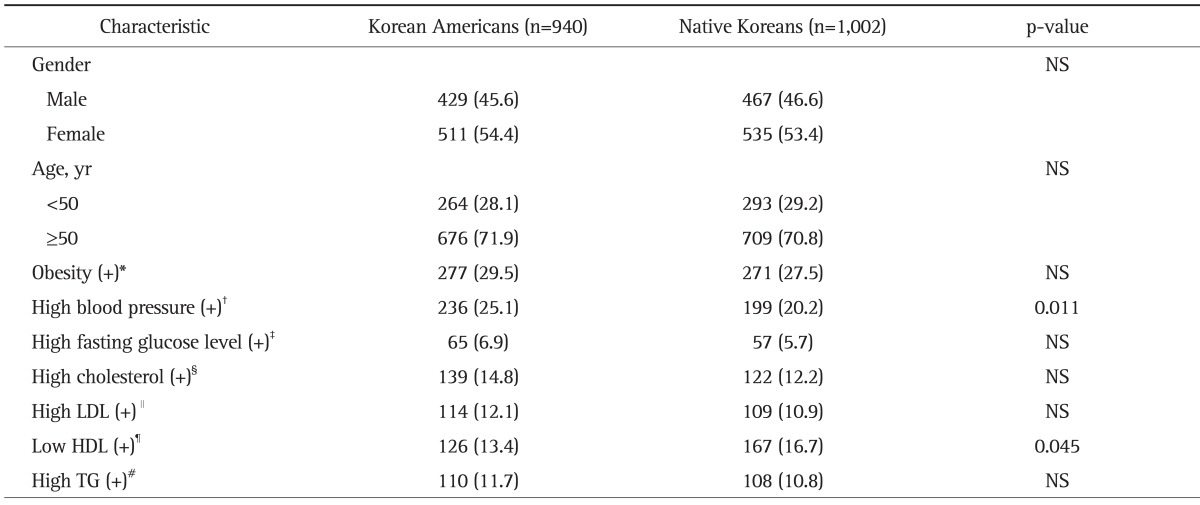
Data are presented as number (%).
NS, not significant.
*Body mass index >25 kg/m2; †Systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg; ‡Fasting blood glucose level ≥126 mg/dL; §Total cholesterol level ≥240 mg/dL; ∥Low density lipoprotein (LDL) level ≥160 mg/dL; ¶High density lipoprotein (HDL) level ≤40 mg/dL; #Triglyceride (TG) level ≥200 mg/dL.
2. Prevalence of GI diseases
There were no significant differences between Korean Americans and native Koreans in regard to the prevalences the prevalence of RE, gastric ulcer, duodenal ulcer, gastric cancer, colorectal polyps, and colorectal cancer (Table 2). However, the prevalence of hemorrhoids was higher in Korean Americans (29.4% vs 21.3%, p=0.001). In females, RE (5.7% vs 3.0%, p=0.032) and hemorrhoids (33.0% vs 23.1%, p=0.004) were more prevalent in Korean Americans than native Koreans.
Table 2.
Prevalence of Gastrointestinal Diseases in Korean Americans and Native Koreans
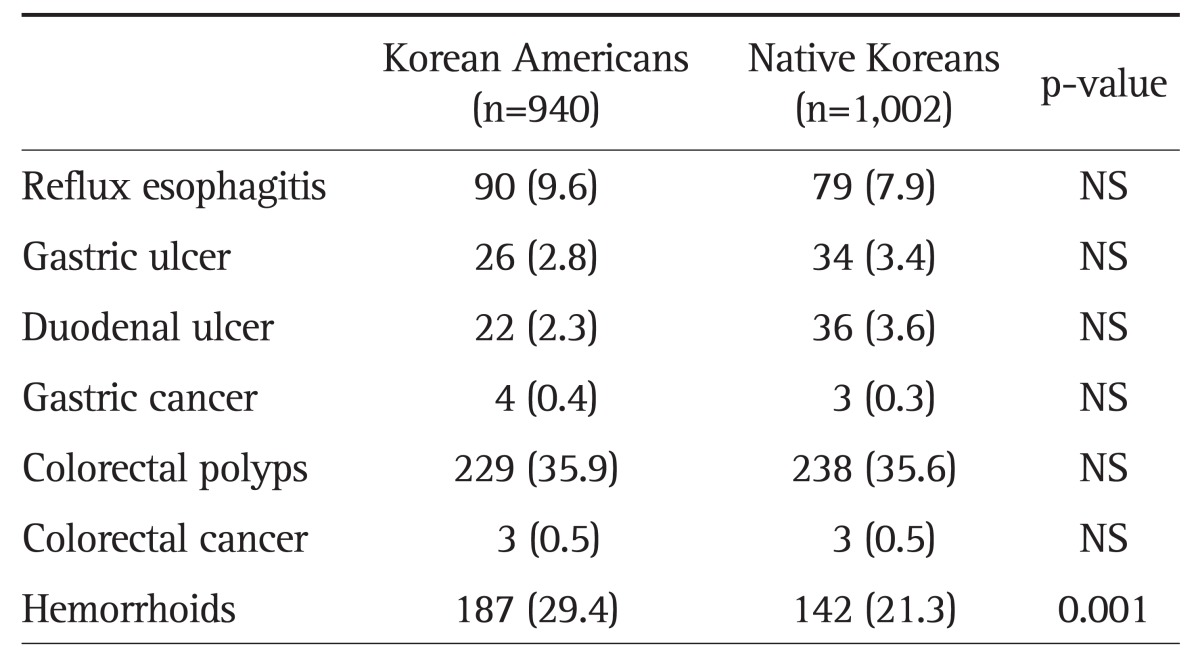
Data are presented as number (%).
NS, not significant.
3. Univariate and multivariate analysis for the associated factors in Korean Americans and native Koreans
1) Colorectal polyps
In the univariate analysis, significant predictive factors for colon polyps in Korean Americans were male gender, age over 50 years, high cholesterol and high TG while those in native Koreans were male gender, age over 50 years, obesity, low HDL, and high TG (Table 3). In the multivariable analysis, the same predictive factors in univariate analysis were still significant in Korean Americans: male gender (odds ratio [OR], 1.54; 95% confidence interval [CI], 1.12 to 2.14), age over 50 years (OR, 1.65; 95% CI, 1.14 to 2.39), high cholesterol (OR, 1.72; 95% CI, 1.11 to 2.64), and high TG (OR, 1.86; 95% CI, 1.14 to 3.04). In native Koreans, only male gender (OR, 1.78; 95% CI, 1.28 to 2.48), age over 50 years (OR, 1.91; 95% CI, 1.32 to 2.75), and high TG (OR, 1.72; 95% CI, 1.02 to 2.91) were independent predictors (Table 4).
Table 3.
Univariate Analysis of the Factors Associated with Colorectal Polyps and Reflux Esophagitis in Korean Americans and Native Koreans
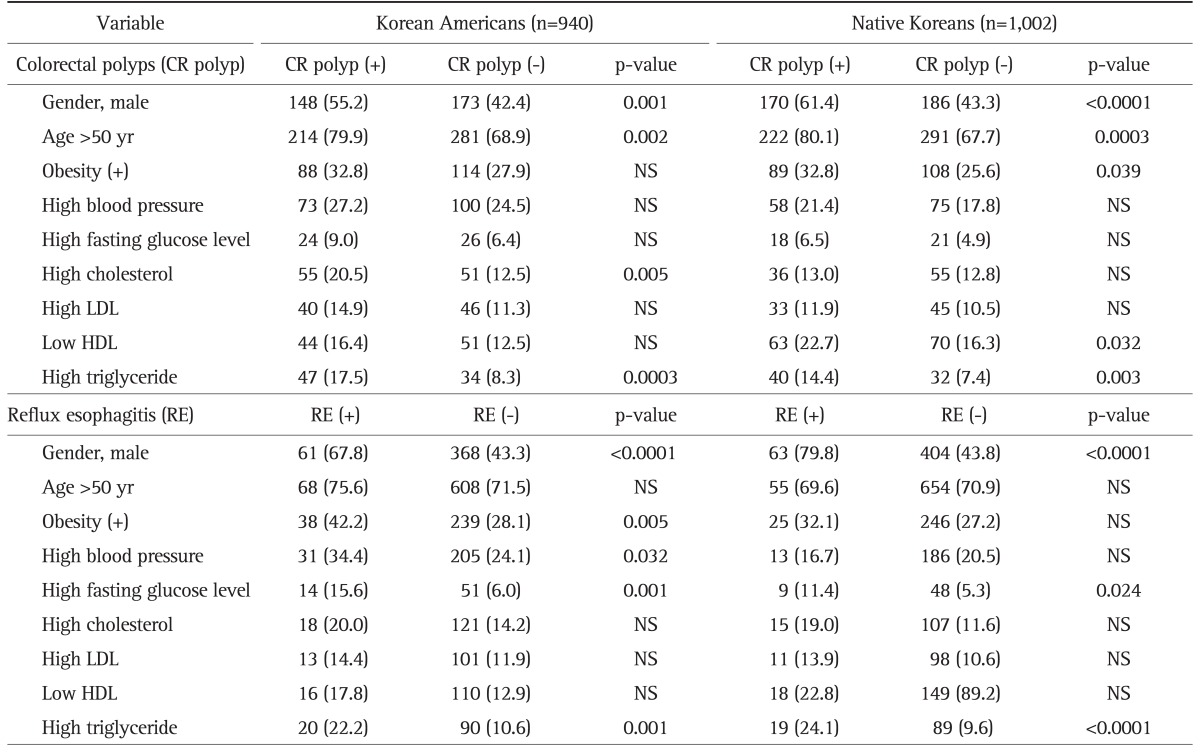
Data are presented as number (%).
NS, not significant; LDL, low density lipoprotein; HDL, high density lipoprotein.
Table 4.
Multivariable Analysis* of the Factors Associated with Colorectal Polyps and Reflux Esophagitis in Korean Americans and Native Koreans
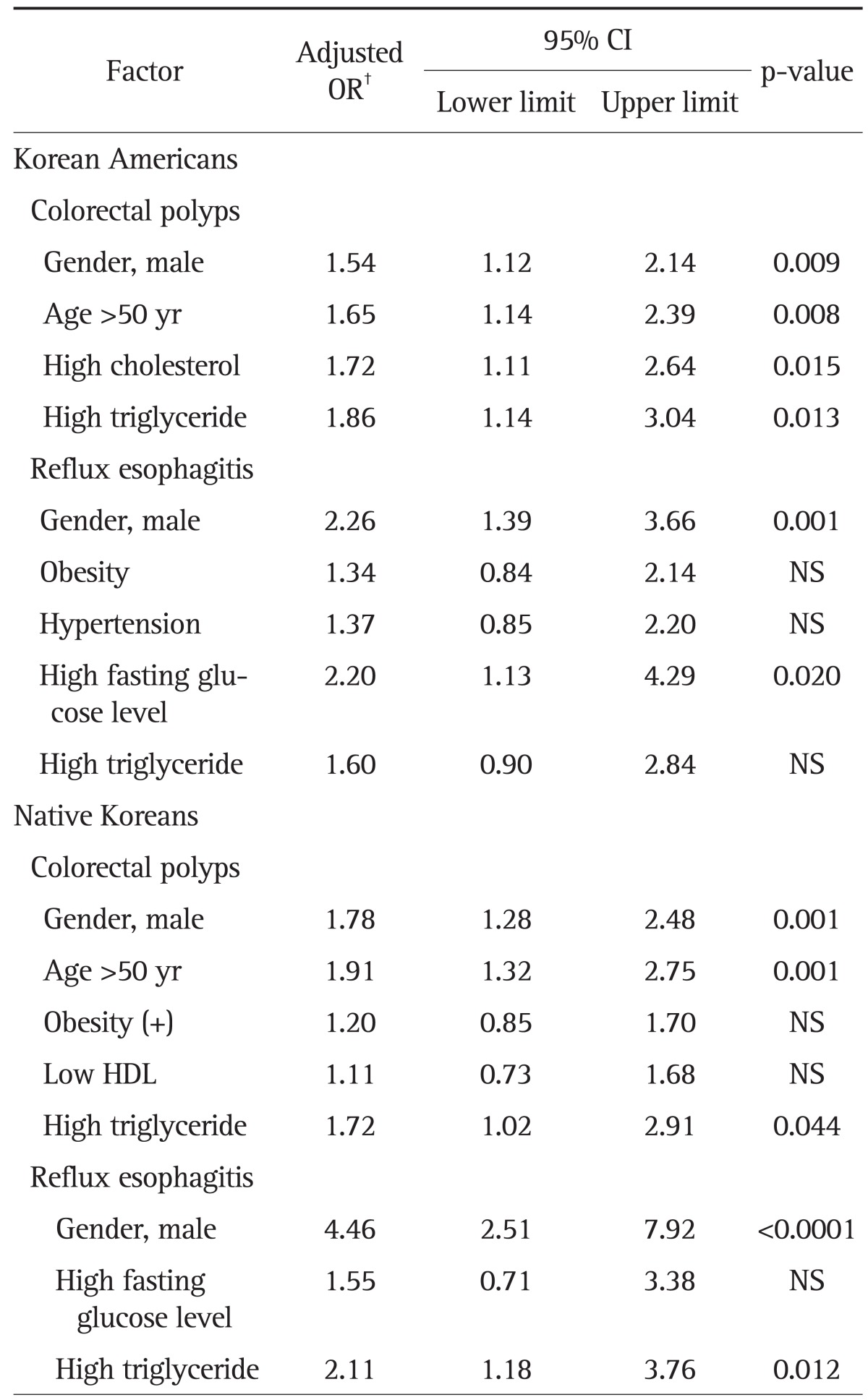
OR, odds ratio; CI, confidence interval; NS, not significant; HDL, high density lipoprotein.
*Logistic regression for multivariate analysis; †Adjusted for all variables in the table.
2) RE
In the univariate analysis, significant predictive factors for RE in Korean Americans were male gender, obesity, high blood pressure, high fasting glucose level, and high TG while those in native Koreans were male gender, high fasting glucose level, and high TG (Table 3). Multivariate analysis showed that independent predictors were male gender (OR, 2.26; 95% CI, 1.39 to 3.66), high fasting glucose level (OR, 2.20; 95% CI, 1.13 to 4.29) in Korean Americans and male gender (OR, 4.46; 95% CI, 2.51 to 7.92), and high TG (OR, 2.11; 95% CI, 1.18 to 3.76) in native Koreans (Table 4).
3) Other GI diseases: gastric ulcer, duodenal ulcer, gastric cancer, colorectal cancer, and hemorrhoids
In other diseases except for hemorrhoids, there was no independent predictor in multivariate analysis.
In Korean Americans with hemorrhoids, female gender (58.3% vs 49.1%, p=0.023) and obesity (37.3% vs 26.4%, p=0.004) were significant associated factors in the univariate analysis. Female gender (OR, 1.71; 95% CI, 1.22 to 2.40), and obesity (OR, 1.93; 95% CI, 1.35 to 2.76) were still independent predictors of hemorrhoids in the multivariable analysis. In native Koreans, none of the variables were associated with hemorrhoids in the univariate and multivariate analysis.
DISCUSSION
Our study showed that the prevalence of GI diseases including gastric cancer and colorectal neoplasms in Korean Americans were similar to those in native Koreans. We suggest that males aged over 50 years with high cholesterol or high TG in Korean Americans should be screened regularly with colonoscopy. The prevalence of colorectal polyps is known to be higher in Western people than in Asian people. The overall prevalence for all types of colorectal polyps in Western countries ranges from 29.4% to 58%.9-11 In Asia, two studies indicated prevalences of 16.3% and 18.5% for colonic polyps in asymptomatic subjects.12,13
We found that 35.9% of Korean Americans and 35.6% of native Koreans had colorectal polyps. This is higher than that from two preivous studies in other Asian population.12,13 A study by Chung et al. reported that 22.2% of asymptomatic Koreans aged 40 to 49 years and 32.8% aged 50 to 59 years had a colorectal neoplasm.14 In another small scale study by Kim et al.,15 32.3% of young (<50 years old) and 53.3% of old (≥50 years old) patients had colorectal polyps. The high prevalence reported in Korean studies can be partially explained by different exclusion criteria and study populations. In fact, we assessed all subjects that underwent a screening colonoscopy regardless of any colorectal symptoms or personal history of colorectal cancer. Second, ethnic factors may contribute to the high prevalence of colorectal polyps in Koreans. Although low prevalence of colorectal neoplasia in Asian patients especially Chinese has been reported, not all studies in Asian country have revealed the similar results. A study in Asian Americans of which 90% were Vietnamese and Chinese reported a 25.2% prevalence of colorectal neoplasia.16 The prevalence of colorectal neoplasm appeared to be higher in Japanese and Korean populations than in other six Asian populations including Chinese and Filipino.17 Asian migrants in America should consider possible ethnic differences in Asian people for colorectal cancer screening. Recently, Korean guidelines for postpolypectomy colonoscopy surveillance were published.18 The authors advised that asymptomatic persons over 50 aged who are concerned about colorectal cancer should receive screening colonoscopy as index. They also recommended 3 to 5 years of surveillance interval according to the result of index colonoscopy.18 We suggest that Korean Americans should follow these Korean guidelines.
As reported in previous studies, male predominance was also observed in this study.12,14,16 Further study is needed to compare differences in colonic size, pathologic findings, anatomical locations as well as lifestyles between two groups.
Considering that the purpose of screening endoscopy is to detect early precancerous lesions in the healthy people, the prevalence of benign diseases in this study are additional findings.
Prevalence of RE is increasing in Korea. Studies in Korea have reported the prevalence of RE to range from 8.0% to 11.8% in symptomatic patients, and 3.19% to 9.7% in asymptomatic subjects.19-23 This proportion was lower than those reported in other Asian countries such as Japan (14% to 16%), China (20.8%), and Taiwan (12.0%).24-27 Although many risk factors for RE have been reported in Korean studies, including smoking, hiatal hernia, older aged females (≥65), and Helicobacter pylori eradication history, male gender was the only common independent factor reported in all studies.19,28,29 Interestingly, the OR for male gender was more than two-times as high in native Koreans than in Korean Americans. This can be explained by a higher prevalence of RE in female Korean Americans. In Japan, a high incidence of GERD was reported in elderly females because of kyphosis and osteoporosis related to hiatal hernia.25 Only high fasting glucose level was another predictor of RE in this study. However, this was inconsistent after adjustments in other previous studies.19 Further study is needed to clarify more details in related to reflux symptoms and other regarding risk factors of RE in Korean American.
Hemorrhoidal disease is a common benign anorectal disorder and can be troublesome during daily bowel movements. The prevalence of hemorrhoids have been reported in a wide range from 4.4% to 86%.30,31 We found that Korean Americans had a greater prevalence of hemorrhoids than native Koreans. Known risk factors for hemorrhoids are constipation, low physical activity, low fiber diet and high BMI.32-34 In the present study, female gender and obesity are predictors of hemorrhoids. The pathophysiology of hemorrhoids is related to the engorgement of vascular plexus.35 Persistent pressure to anal cushions by various condition such as pregnancy, increased intra-abdominal pressure, which can affect hemorrhoids.35 Prolonged straining during vaginal delivery possibly induces mechanical trauma in anal canal, which might be associated with persistent hemorrhoids.35 We cannot explain how obesity affect hemorrhoids, but associated factors can be explained by underlying pathophysiology of hemorrhoids. We suggest that obese Korean American women are vulnerable to hemorrhoids, and clinical education to prevent predisposing factors to hemorrhoids should be done.
There are limitations to our study. First, this is a cross-sectional study in a single health promotion center, which means both groups are not representative of each population. Therefore, we selected age and gender matched native Koreans to compare with Korean Americans to compensate selection bias. Because people in both groups have same purpose to find any diseases of their own, we could overcome detection bias. Secondly, we included all subjects that underwent upper and lower endoscopy regardless of symptoms or personal risks for each GI disease. The main purpose of this study was to compare the prevalence of common endoscopically diagnosed diseases between Korean Americans and native Koreans, symptoms and risk factors of each disease could not be excluded at the same time because of the possibility of small stratified sample size. Obtaining more data from multiple centers in Korea and United States, would possibly overcome this limitation and be more representative of Korean-populations in both countries. Finally, the lack of data for general characteristics of individuals such as smoking, alcohol intake, socioeconomic status, and current medication limited the analysis of their association with each of the diseases.
In conclusion, the prevalence of GI diseases in Korean Americans were similar with native Koreans. In Korean Americans, only hemorrhoids were more prevalent. Korean Americans who are predisposed to colorectal polyps should consider following the Korean guidelines of screening colonoscopy. This is the preliminary study to compare the common GI diseases between Korean Americans and native Koreans for the first time. Further studies to reveal different risk factors for each disease are needed.
ACKNOWLEDGEMENTS
The authors would like to thank Hyung-Gon Kim, Chief of the Health Promotion Center at Gangnam Severance Hospital for his assistance and support.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Park B, Choi KS, Lee YY, Jun JK, Seo HG. Cancer screening status in Korea, 2011: results from the Korean National Cancer Screening Survey. Asian Pac J Cancer Prev. 2012;13:1187–1191. doi: 10.7314/apjcp.2012.13.4.1187. [DOI] [PubMed] [Google Scholar]
- 2.Park B, Choi KS, Lee YY, Jun JK, Seo HG. Trends in Cancer Screening Rates among Korean Men and Women: results from the Korean National Cancer Screening Survey (KNCSS), 2004-2011. Cancer Res Treat. 2012;44:113–120. doi: 10.4143/crt.2012.44.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim Y, Jun JK, Choi KS, Lee HY, Park EC. Overview of the National Cancer screening programme and the cancer screening status in Korea. Asian Pac J Cancer Prev. 2011;12:725–730. [PubMed] [Google Scholar]
- 4.U.S. Census Bureau. The American Community-Asians: 2004. American Community Survey Reports [Internet] Washington, DC: U.S. Department of Commerce Economics and Statistics Administration; 2013. [cited 2012 Oct 30]. Available from: http://www.commerce.gov. [Google Scholar]
- 5.Jo AM, Maxwell AE, Rick AJ, Cha J, Bastani R. Why are Korean American physicians reluctant to recommend colorectal cancer screening to Korean American patients? Exploratory interview findings. J Immigr Minor Health. 2009;11:302–309. doi: 10.1007/s10903-008-9165-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Won CW, Hwang HS. U.S. geriatricians and gastric cancer screening in elderly Korean-American men: differences from Korean geriatricians. J Am Geriatr Soc. 2012;60:996–997. doi: 10.1111/j.1532-5415.2012.03947.x. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong D, Bennett JR, Blum AL, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996;111:85–92. doi: 10.1053/gast.1996.v111.pm8698230. [DOI] [PubMed] [Google Scholar]
- 8.Miwa H, Yokoyama T, Hori K, et al. Interobserver agreement in endoscopic evaluation of reflux esophagitis using a modified Los Angeles classification incorporating grades N and M: a validation study in a cohort of Japanese endoscopists. Dis Esophagus. 2008;21:355–363. doi: 10.1111/j.1442-2050.2007.00788.x. [DOI] [PubMed] [Google Scholar]
- 9.Rondagh EJ, Bouwens MW, Riedl RG, et al. Endoscopic appearance of proximal colorectal neoplasms and potential implications for colonoscopy in cancer prevention. Gastrointest Endosc. 2012;75:1218–1225. doi: 10.1016/j.gie.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Betés M, Muñoz-Navas MA, Duque JM, et al. Use of colonoscopy as a primary screening test for colorectal cancer in average risk people. Am J Gastroenterol. 2003;98:2648–2654. doi: 10.1111/j.1572-0241.2003.08771.x. [DOI] [PubMed] [Google Scholar]
- 11.Mehran A, Jaffe P, Efron J, Vernava A, Liberman A. Screening colonoscopy in the asymptomatic 50- to 59-year-old population. Surg Endosc. 2003;17:1974–1977. doi: 10.1007/s00464-003-8807-4. [DOI] [PubMed] [Google Scholar]
- 12.Liu HH, Wu MC, Peng Y, Wu MS. Prevalence of advanced colonic polyps in asymptomatic Chinese. World J Gastroenterol. 2005;11:4731–4734. doi: 10.3748/wjg.v11.i30.4731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Byeon JS, Yang SK, Kim TI, et al. Colorectal neoplasm in asymptomatic Asians: a prospective multinational multicenter colonoscopy survey. Gastrointest Endosc. 2007;65:1015–1022. doi: 10.1016/j.gie.2006.12.065. [DOI] [PubMed] [Google Scholar]
- 14.Chung SJ, Kim YS, Yang SY, et al. Prevalence and risk of colorectal adenoma in asymptomatic Koreans aged 40-49 years undergoing screening colonoscopy. J Gastroenterol Hepatol. 2010;25:519–525. doi: 10.1111/j.1440-1746.2009.06147.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim YG, Jang BI, Kim DH, et al. A matched case-control study using the propensity score on differences in the characteristics of colorectal polyps between younger and older Koreans: proximal shift in the distribution of colorectal polyps among older Koreans. Gut Liver. 2010;4:481–487. doi: 10.5009/gnl.2010.4.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lam KD, Garcia RT, Nguyen LH, et al. Prevalence of colorectal neoplasms in Asian Americans. Dig Dis Sci. 2009;54:160–167. doi: 10.1007/s10620-008-0499-0. [DOI] [PubMed] [Google Scholar]
- 17.Leung WK, Ho KY, Kim WH, et al. Colorectal neoplasia in Asia: a multicenter colonoscopy survey in symptomatic patients. Gastrointest Endosc. 2006;64:751–759. doi: 10.1016/j.gie.2006.06.082. [DOI] [PubMed] [Google Scholar]
- 18.Yang DH, Hong SN, Kim YH, et al. Korean guidelines for postpolypectomy colonoscopy surveillance. Clin Endosc. 2012;45:44–61. doi: 10.5946/ce.2012.45.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim N, Lee SW, Cho SI, et al. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther. 2008;27:173–185. doi: 10.1111/j.1365-2036.2007.03561.x. [DOI] [PubMed] [Google Scholar]
- 20.Hwang JK, Kim J, Hong SG, et al. A prospective multicenter study on the prevalence and symptoms of erosive reflux esophagitis in secondary and tertiary hospitals in Korea. Korean J Gastroenterol. 2009;53:283–291. doi: 10.4166/kjg.2009.53.5.283. [DOI] [PubMed] [Google Scholar]
- 21.Yoo SS, Lee WH, Ha J, et al. The prevalence of esophageal disorders in the subjects examined for health screening. Korean J Gastroenterol. 2007;50:306–312. [PubMed] [Google Scholar]
- 22.Jeon SG, Rhee PL, Shin MH, et al. The prevalence and risk factors of reflux esophagitisin routine check-up subjects. Korean J Gastroenterol. 1998;32:701–708. [Google Scholar]
- 23.Lee JY, Hong WK, Sohn KM, et al. Prevalence and clinical characteristics of gastroesophageal reflux disease and reflux esophagitis in chuncheon city-Health care examination study. Korean J Med. 2008;74:385–390. [Google Scholar]
- 24.Okamoto K, Iwakiri R, Mori M, et al. Clinical symptoms in endoscopic reflux esophagitis: evaluation in 8031 adult subjects. Dig Dis Sci. 2003;48:2237–2241. doi: 10.1023/b:ddas.0000007857.15694.15. [DOI] [PubMed] [Google Scholar]
- 25.Fujimoto K. Review article: prevalence and epidemiology of gastro-oesophageal reflux disease in Japan. Aliment Pharmacol Ther. 2004;20(Suppl 8):5–8. doi: 10.1111/j.1365-2036.2004.02220.x. [DOI] [PubMed] [Google Scholar]
- 26.Du J, Liu J, Zhang H, Yu CH, Li YM. Risk factors for gastroesophageal reflux disease, reflux esophagitis and non-erosive reflux disease among Chinese patients undergoing upper gastrointestinal endoscopic examination. World J Gastroenterol. 2007;13:6009–6015. doi: 10.3748/wjg.v13.45.6009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang FW, Tu MS, Chuang HY, Yu HC, Cheng LC, Hsu PI. Erosive esophagitis in asymptomatic subjects: risk factors. Dig Dis Sci. 2010;55:1320–1324. doi: 10.1007/s10620-009-0888-z. [DOI] [PubMed] [Google Scholar]
- 28.Nam SY, Choi IJ, Ryu KH, Kim BC, Kim CG, Nam BH. Effect of Helicobacter pylori infection and its eradication on reflux esophagitis and reflux symptoms. Am J Gastroenterol. 2010;105:2153–2162. doi: 10.1038/ajg.2010.251. [DOI] [PubMed] [Google Scholar]
- 29.Cho JH, Kim HM, Ko GJ, et al. Old age and male sex are associated with increased risk of asymptomatic erosive esophagitis: analysis of data from local health examinations by the Korean National Health Insurance Corporation. J Gastroenterol Hepatol. 2011;26:1034–1038. doi: 10.1111/j.1440-1746.2011.06686.x. [DOI] [PubMed] [Google Scholar]
- 30.Haas PA, Haas GP, Schmaltz S, Fox TA., Jr The prevalence of hemorrhoids. Dis Colon Rectum. 1983;26:435–439. doi: 10.1007/BF02556521. [DOI] [PubMed] [Google Scholar]
- 31.Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology. 1990;98:380–386. doi: 10.1016/0016-5085(90)90828-o. [DOI] [PubMed] [Google Scholar]
- 32.Riss S, Weiser FA, Schwameis K, et al. The prevalence of hemorrhoids in adults. Int J Colorectal Dis. 2012;27:215–220. doi: 10.1007/s00384-011-1316-3. [DOI] [PubMed] [Google Scholar]
- 33.Riss S, Weiser FA, Schwameis K, Mittlbck M, Stift A. Haemorrhoids, constipation and faecal incontinence: is there any relationship? Colorectal Dis. 2011;13:e227–e233. doi: 10.1111/j.1463-1318.2011.02632.x. [DOI] [PubMed] [Google Scholar]
- 34.Lohsiriwat V. Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol. 2012;18:2009–2017. doi: 10.3748/wjg.v18.i17.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Avsar AF, Keskin HL. Haemorrhoids during pregnancy. J Obstet Gynaecol. 2010;30:231–237. doi: 10.3109/01443610903439242. [DOI] [PubMed] [Google Scholar]


