Abstract
Patient: Male, 0
Final Diagnosis: Bland-White-Garland syndrome
Symptoms: Cardiomegaly, feeding problems
Medication: —
Clinical Procedure: Reimplantation of the left coronary artery to the aorta
Specialty: Pediatrics and Neonatology
Objective:
Rare disease
Background:
Bland-White-Garland syndrome (BWGS) is a very rare disease characterized by anomalous origin of the left coronary artery from the pulmonary trunk (ALCAPA). WBGS affects 1 in every 300 000 live births. Children typically present with dyspnea, pallor, and failure to thrive. Without surgical repair, most of these children die during the first months of life.
Case Report:
This case report describes 3-month-old boy admitted to the hospital because of feeding problems. The boy was born at term, with birth weight 3200 g, and was 10 points in Apgar score. He was breast-fed from birth. From the seventh week of age, his mother observed his increasing difficulties with feeding. Physical examination revealed pale skin, diminished heart sounds, tachycardia, cardiomegaly, and hepatomegaly. Results of urine and blood tests and ultrasonography of the central nervous system and abdomen were normal. The chest radiography showed cardiomegaly and electrocardiogram revealed anterolateral myocardial infarction. On echocardiography, an anomalous left coronary artery arising from the pulmonary artery was found. The life-saving treatment of choice was immediate surgical reimplantation of the left coronary artery to the aorta.
Conclusions:
Children with congenital heart disease are often prone to malnutrition, but in rare cases failure to thrive and breast-feeding problems can be the first symptoms of life-threatening diseases like myocardial infarction secondary to Bland-White-Garland syndrome (BWGS).
Keywords: Bland-White-Garland syndrome, ALCAPA failure to thrive, myocardial infarction, infant
Background
Failure to thrive and difficulties in breast-feeding are some of the most common problems in everyday pediatric practice. Differential diagnosis includes many infant and maternal causes, mostly influencing the lactation process [1]. Breast-feeding problems can be associated with the simplest problems, like inappropriate feeding. But, rarely, failure to thrive in breast-feeding infants is considered an indication for hospitalization and, even more unusually, an indication for emergency treatment [2,3]. The health care professional should take a full medical history, including history of pregnancy, infections, diet, and psychosocial state, and perform a full physical examination [4], because BWGS is a life-threatening clinical syndrome that must be included in the differential diagnosis.
Case Report
A 3-month-old boy was admitted to our hospital because of poor weight gain while breast-feeding. The boy was born at term, with birth weight 3200 g, and was 10 points in Apgar score. He was breast-fed from birth. His body weight was 4500 g (+1300 g) after 6 weeks. However, from the seventh week of age, his mother observed that he had increasing difficulties with sucking. She had an appointment in the breast-feeding clinic and she was consulted, but without any improvement in feeding. On the day of admission the boy was in good general condition. However, on physical examination there were several abnormalities noted: pale skin, diminished heart sounds, tachycardia (HR was 124 beats per minute), and signs of cardiomegaly and hepatomegaly. Results of laboratory tests, including complete blood count and tests of liver, kidney and thyroid function, as well as urinalysis, were all normal. Because of signs of cardiomegaly, ECG and chest X-ray were ordered. The ECG showed signs of anterolateral myocardial infarction (Figure 1), thus alerting clinicians that this was a very serious situation. Emergency 2D ECG was performed, which showed dilated cardiomyopathy with severe systolic dysfunction, EF 22%, and severe mitral insufficiency. The cardiologist was able to visualize a 2.8-mm–wide right coronary artery, but the most striking finding was the anomalous origin of the left coronary artery from the pulmonary trunk (Figure 2). Based on this echocardiographic examination, Bland-White-Garland syndrome was diagnosed. On the chest X-ray, severe cardiomegaly (CTR 0.75) was seen (Figure 3). Immediate cardiac surgery was arranged and successfully performed. This patient survived myocardial infarction in his seventh week of life.
Figure 1.
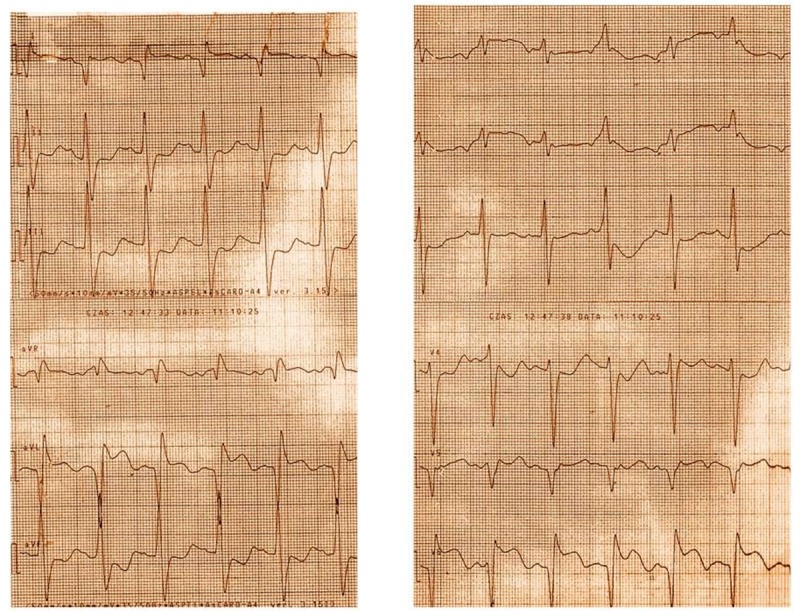
ECG: Deep Q waves and T waves inversions in leads I, avL and deep Q waves with ST elevation in the left precordial leads (V5–V6). Signs of anterolateral myocardial infarction.
Figure 2.
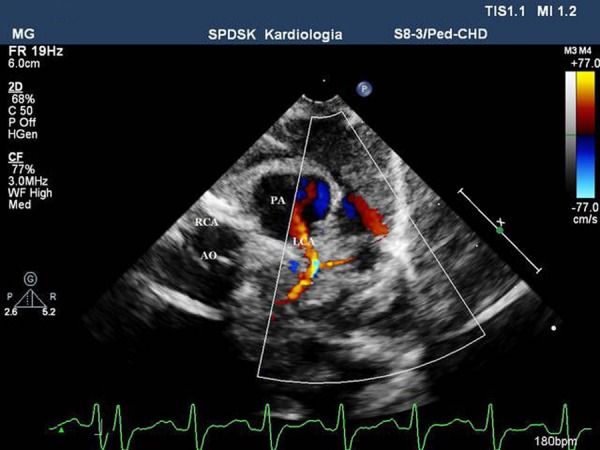
2D-ECHO. Parasternal short axis view at the level of the great vessels. Anomalous left coronary artery originating from the pulmonary trunk.
Figure 3.

Chest X-ray showing significant cardiomegaly.
Discussion
Bland-White-Garland syndrome is a very rare congenital anomaly, present in 1 out of 300 000 neonates [5]. In the described infant, the onset of the disease was typical for the syndrome. From the seventh week of life, after pulmonary arterial pressure had decreased, this child demonstrated irritability and distress after feeding and had angina-like spells. These were caused by the coronary steal from the left coronary artery into the pulmonary trunk, which resulted in diminished perfusion of the left ventricular muscle, extensive myocardial ischemia, seen as dilated left ventricle with severely diminished ejection fraction on 2D-Echo, and finally, myocardial infarction. The prognosis of this syndrome depends on early diagnosis and successful cardiac surgery. Without diagnosis and treatment, the natural course of the disease is devastating and most untreated children die in the first year of life because of massive myocardial injury and following end-stage heart failure [6,7]. With appropriate diagnosis and emergency cardiac surgery, they have a much better chance to survive. The preferred method is a direct reimplantation of the left coronary artery to the aorta [8].
Conclusions
Children with congenital heart disease are prone to malnutrition [9]. Failure to thrive, growth failure, and problems with breast-feeding can be the first symptoms of life-threatening disease such Bland-White-Garland syndrome.
References:
- 1.Emond A, Drewett R, Blair P, Emmett P. Postnatal factors associated with failure to thrive in term infants in the Avon Longitudinal Study of parents and Children. Arch Dis Child. 2007;92(2):115–19. doi: 10.1136/adc.2005.091496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sachs M, Dykes F, Carter B. Weight monitoring of breastfed babies in the United Kingdom – interpreting, explaining and intervening. Matern Child Nutr. 2006;2(1):3–18. doi: 10.1111/j.1740-8709.2006.00019.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tyler M, Hellings P. Feeding methods and rehospitalization in newborns less than 1 month of age. J Obstet Gynecol Neonatal Nurs. 2005;34(1):70–79. doi: 10.1177/0884217504272813. [DOI] [PubMed] [Google Scholar]
- 4.Kitsantas P, Pawloski LR. Maternal obesity, health status during pregnancy, and breastfeeding initiation and duration. J Matern Fetal Neonatal Med. 2010;23(2):135–41. doi: 10.3109/14767050903118270. [DOI] [PubMed] [Google Scholar]
- 5.Cowles RA, Berdon WE. Bland-White-Garland syndrome of anomalous left coronary artery arising from the pulmonary artery (ALCAPA): a historical review. Pediatr Radiol. 2007;37(9):890–95. doi: 10.1007/s00247-007-0544-8. [DOI] [PubMed] [Google Scholar]
- 6.Barbetakis N, Efstathiou A, Efstathiou N, et al. A long-term survivor of Bland-White-Garland syndrome with systemic collateral supply: a case report and review of the literature. BMC Surg. 2005;15(5):23. doi: 10.1186/1471-2482-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dymnicka S, Tomaszewski M, Aleszewicz J, Bielińska B. Myocardial infarction in children. Pol Tyg Lek. 1995;50:58–61. [PubMed] [Google Scholar]
- 8.Varan B, Tokel K, Yilmaz G. Malnutrition and growth failure in cyanotic and acyanotic congenital heart disease with or without pulmonary hypertension. Arch Dis Child. 1999;81(1):49–52. doi: 10.1136/adc.81.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arce Casas A, Concheiro Guisan A, Cambra Lasaosa FJ, et al. Coronary ischemia secondary to congenital anomaly of the left coronary artery. An Pediatr (Barc) 2003;58(1):71–73. doi: 10.1016/s1695-4033(03)77996-x. [DOI] [PubMed] [Google Scholar]


