Abstract
Background
Hospital admissions over weekends have been associated with worse outcomes in different patient populations. The etiology of this difference in outcomes remains unclear; however different staffing patterns over weekends have been speculated to contribute. We evaluated outcomes in patients on maintenance dialysis admitted over weekends using a national database.
Study Design
Retrospective cohort study.
Setting & Participants
We included non-elective admissions of adult patients (≥18 years) on maintenance dialysis (n=3,278,572) identified using appropriate ICD-9-CM codes for years 2005-2009 using Nationwide Inpatient Sample database.
Predictor
Weekend vs weekday admission.
Outcomes
Primary outcome measure was all cause in-hospital mortality. Secondary outcomes included mortality by day three of admission, length of hospital stay, time to death and discharge disposition.
Measurements
We adjusted for patient and hospital characteristics, payer, year, comorbidities and primary discharge diagnosis common to maintenance dialysis patients.
Results
There were estimated 704,491 admissions over weekends vs 2,574,081 over weekdays. Unadjusted all cause in-hospital mortality was 40,666 (5.8%) for weekend admissions in comparison to 138,517 (5.4%) for weekday admissions (p<0.001). In multivariable model, patients admitted over weekends had higher all cause in-hospital mortality (OR, 1.06; 95% CI, 1.01-1.10) in comparison to those admitted over weekdays and higher mortality during first three days of admission (OR, 1.18; 95% CI, 1.10-1.26). Patients admitted over weekends were less likely to be discharged home, had longer hospital stay and shorter time to death compared to those admitted over weekdays on adjusted analysis.
Limitations
Use of ICD-9-CM codes to identify patients, defining weekend as midnight Friday to midnight Sunday.
Conclusions
Maintenance dialysis patients admitted over weekends have increased mortality rates and longer length of stay as compared to those admitted over weekdays. Further studies are needed to identify the reasons for worse outcomes for weekend admissions in this patient population.
Keywords: dialysis, admissions, mortality
A growing body of literature demonstrates unfavorable outcomes for weekend hospital admissions in comparison to weekdays. This phenomenon has been highlighted in several patient populations including those with myocardial infarction1, stroke2, intracerebral hemorrhage3, gastrointestinal bleeding4, pulmonary embolism5, ruptured abdominal aortic aneurysm5, acute epiglottitis5 and recently, acute kidney injury6. Though the etiology of this phenomenon remains elusive, potential explanations include differential staffing models with limited availability of clinician expertise, unmeasured differences in severity of illness and decreased accessibility to diagnostic and therapeutic procedures.
End-stage renal disease (ESRD) defined as kidney failure necessitating kidney replacement therapy, most often in the form of hemodialysis, is a growing epidemic in the United States. The current population wide prevalence is estimated to be 1,700 patients per million with a projection of over 700,000 prevalent patients by the year 20157. The US Renal Data System (USRDS) 2012 annual data reported that there were 340 new cases of ESRD per million population in 2010; ESRD constitutes a unique group of patients who are frequently hospitalized and the in-hospital mortality is on an average 6-8 times greater than in the general population (volume 2, chapters 1 and 5).8 Given their complex nature and propensity to develop volume and metabolic derangements, patients with ESRD, especially those on maintenance dialysis who need hospitalization, would likely require timely access to expert nephrology consultation and renal replacement therapy.
Worse outcomes for weekend admissions, though demonstrated for many timesensitive medical conditions, have not been studied among maintenance dialysis patients. Thus, we aimed to study if this phenomenon existed for hospital admissions of patients receiving maintenance dialysis. We used a large, nationally representative database (Nationwide Inpatient Sample [NIS] database) to describe the mortality differences and other associated outcomes between weekday and weekend admissions of patients on maintenance dialysis.
Methods
Study Design
We designed a retrospective, cohort study using the Healthcare Cost and Utilization Project - NIS, the largest all-payer inpatient care database publicly available in the United States. This is an administrative dataset created by the Agency for Healthcare Research and Quality and contains data from 20-percent stratified sample of U.S. community hospitals10. Each hospitalization is treated as an individual entry in the database and is coded with 1 principal diagnosis, up to 14 secondary diagnoses and 15 procedural diagnoses associated with that stay. NIS encompasses information on all patients regardless of payer, including private insurance and the uninsured. It also includes patient information regardless of type of hospital: teaching or non-teaching, rural or urban, large or small volume, and private or publicly owned. To facilitate the projection of national estimates, both hospital and discharge weights are provided, along with information necessary to calculate the variance of estimates.
NIS collects information on common demographic variables like age, race, and gender along with primary and secondary insurance, hospital level characteristics like teaching status, location (rural vs. urban), size of hospital and hospital region. Facilities are considered to be teaching hospitals if they have an American Medical Association approved residency program, or are a member of the Council of Teaching Hospitals, or have fulltime equivalent interns and residents to patient ratio of 0.25 or higher. Hospital location (rural/urban) and bed size are also defined. The bed size cutoff points are chosen so that approximately one-third of the hospitals in a given region, location, and teaching status combination would fall within each bed size category (into small, medium and large). From 2004 in NIS, the hospitals with a Core Based Statistical Area type of Metropolitan were categorized as urban, while hospitals with a Core Based Statistical Area type of Rural were categorized as rural. The data from the years 2005 to 2009 were used for this study.
Study Population
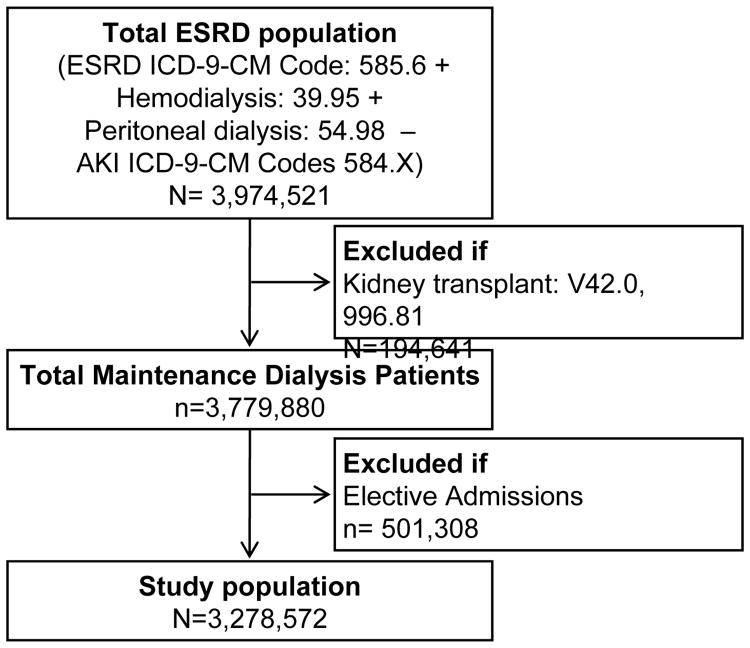
We included all admissions of adult patients (age ≥ 18 years) from the NIS database for the years 2005-2009 who were on maintenance dialysis. Maintenance dialysis status was defined as patients with an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for ESRD (585.6) or procedure code for hemodialysis (39.95) or peritoneal dialysis (54.98) but absence of ICD-9-CM code for acute kidney injury (584.X). ICD9-CM codes 584.X have >90% sensitivity and negative predictive value for acute kidney injury11. Elective admissions and patients who had undergone kidney transplantation were excluded from the study (Figure 1).
Fig 1. Selection of study population (Age ≥18 year). Estimates from weighted survey data.
Study Variables
In accordance with previous studies, we defined weekend admissions as those occurring after midnight on Friday through midnight on Sunday5,12-14. We used the Deyo's modification of Charlson's comorbidity index to identify the burden of comorbidity15. This index uses 17 comorbid conditions with differential weighting and the total scores range from 0 to 33, with higher scores representing greater comorbidity burden. In accordance with previous literature16 we excluded kidney disease when calculating the index as that was already included as patient characteristic. Using ICD-9-CM codes, we also examined primary discharge diagnosis common to maintenance dialysis patients (Table S1, available as online supplementary material). We used NIS variables to identify patient age, gender, race and primary payer. Age was divided into five groups: 18-34, 35-49, 50-64, 65-79, and ≥80 years. Discharges with missing data were excluded except for race, which was missing in approximately 20% of discharges. Missing race was included in primary analyses as a separate subgroup of race.
Outcomes
Our main outcome of interest was all cause in-hospital mortality. Additionally, we investigated length of hospital stay for survivors, time to death and discharge disposition. We also examined mortality by day 3 of admission as previous studies have reported much larger differences in short term mortality for weekend admissions in comparison to weekday admissions6. We also checked for interaction between year and weekend admissions to assess if there were any variations in mortality for weekend admissions by year. Subgroup analysis were performed to look at differences in adjusted odds of mortality for weekend admissions within subgroups of age (<65 or ≥65 years), gender, race (Caucasian vs. African American), primary payer (Medicare or Medicaid vs others), hospital bedsize, and hospital teaching status. The regression coefficients were compared using generalized Hausman test17,18.
Statistical Analysis
Stata IC 11.0 (StataCorp LP, College Station, TX) was used for all analyses. We used the weights provided with the NIS to generate national estimates of the number of admissions in each age group using the survey commands. Chi-square test was used to compare categorical variables between patients admitted on the weekend and those admitted on weekdays. Since length of stay of survivors and time to death were not normally distributed, t-test was performed on log transformed values.
We examined factors associated with in-hospital mortality by multivariable logistic regression. Univariable logistic regression was used to identify risk factor variables associated with in-hospital mortality. All variables that were significant at P < 0.10 were included in the final multivariable model. To control for the variability by year, we used year as a predictor in regression models. We checked variables for multicollinearity using tolerance and variance inflation factor. For the variables used in the final model, both the tolerance and variation inflation factor were very close to unity. Similarly for factors associated with length of stay of survivors and time to death, univariable and multivariable linear regressions were performed.
We examined for interactions between weekend admissions and cardiovascular diseases2,19-22, GI bleed12, hospital bedsize6 or teaching status23 as has been suggested in literature. Significant interaction terms were included in the appropriate final multivariable models. For all cause in-hospital mortality, we found significant interaction between weekend admission and primary discharge diagnosis of cardiovascular disease and weekend admission and teaching status of the hospital, which were both included in the final regression model. Similarly for length of stay of survivors, significant interaction with weekend admissions was found only with hospital bedsize.
We performed five sensitivity analyses to further evaluate the robustness of our results. To account for the multiple admissions of same patients (readmissions), we identified hospital records with similar age, sex, race, primary payer, hospital identification code and year of admission as done previously in literature24. For the first sensitivity analysis, we included all unique observations along with one of each duplicate observations randomly selected from the database. For the second sensitivity analysis we included all unique observations along with one of each duplicate observations admitted in the first month for that duplicate observation. Similarly for the third sensitivity analysis we included all unique observations along with one of each duplicate observations admitted in the last month for that duplicate observation. We finally did another sensitivity analysis including only unique observations and excluding any duplicate observations (Table S2). As race was missing for approximately 20% of observations, we performed another sensitivity analysis excluding race.
Results
Patient Characteristics
Using the NIS database, during the 5-year timeframe of our study (2005-2009), there were an estimated 3,278,572 (95% CI, 3,104,322-3,452,822) discharges on maintenance dialysis. Of those, an estimated 704,491 (95% CI: 654,945-754,038) were admitted over weekends. The baseline characteristics of patients in terms of age, sex, other demographics, co-morbidities and hospital characteristics are shown in Table 1. Patients admitted over weekends were more likely to be between the ages of 18-49 or ≥80 years, African Americans, and admitted less often to teaching hospitals. Primary discharge diagnosis common to maintenance dialysis patients included any infections or access complication, cardiovascular disease (including heart failure, acute coronary syndrome, atrial fibrillation/flutter and stroke), GI bleed and others (including hypertensive emergency and hyperkalemia).
Table 1. Demographic characteristics of ESRD patients admitted on weekdays and weekends*.
| Weekday (n=2,574,081) | Weekend (n=704,491) | P | |
|---|---|---|---|
| Age category | <0.001 | ||
| 18-34 y | 139051 (5.4) | 41305 (5.9) | |
| 35-49 y | 408790 (15.9) | 117972 (16.7) | |
| 50-64 y | 808058 (31.4) | 219483 (31.2) | |
| 65-79 y | 866877 (33.7) | 228843 (32.5) | |
| ≥80 y | 351305 (13.6) | 96888 (13.7) | |
| Female sex | 1268024 (49.3) | 348257 (49.4) | 0.3 |
| Race | <0.001 | ||
| White | 867833 (33.7) | 233832 (33.2) | |
| Black | 690299 (26.8) | 194938 (27.7) | |
| Hispanic | 337249 (13.1) | 86022 (12.2) | |
| Asian | 75329 (2.9) | 19943 (2.8) | |
| Native American | 22156 (0.9) | 6069 (0.9) | |
| Other | 53438 (2.1) | 14066 (2.0) | |
| Missing | 527777 (20.5) | 149621 (21.2) | |
| Primary Payer | 0.1 | ||
| Medicare | 1940761 (75.4) | 534299 (75.8) | |
| Medicaid | 280050 (10.9) | 76904 (10.9) | |
| Private | 276324 (10.7) | 73988 (10.5) | |
| Self-Pay | 37014 (1.4) | 9814 (1.4) | |
| Other | 32947(1.3) | 8253 (1.2) | |
| No charge | 6985 (0.3) | 1233 (0.2) | |
| Teaching hospital | 1301103 (50.5) | 351635 (49.9) | 0.03 |
| Urban location | 2402097 (93.3) | 655243 (93.0) | 0.02 |
| Bed Size | 0.2 | ||
| Small | 199708 (7.8) | 53047 (7.5) | |
| Medium | 578979 (22.5) | 159982 (22.7) | |
| Large | 1795394 (69.7) | 491462 (69.8) | |
| Region of Hospital | <0.001 | ||
| North East | 496719 (19.3) | 131712 (18.7) | |
| Mid-West | 530372 (20.6) | 150656 (21.4) | |
| South | 1023834 (39.8) | 285473 (40.5) | |
| West | 523156 (20.3) | 136650 (19.4) | |
| Modified Charlson's index | 0.7 | ||
| 0 | 617536 (24.0) | 169078 (24.0) | |
| 1-3 | 1711192 (66.5) | 467995 (66.4) | |
| 4-6 | 190991 (7.4) | 52179 (7.4) | |
| ≥7 | 54362 (2.1) | 15239 (2.2) | |
| Common primary discharge diagnosis | |||
| Infections & access issues | 498484 (19.4) | 141469 (20.1) | <0.001 |
| Cardiovascular diseases | 362142 (14.1) | 111178 (15.8) | <0.001 |
| Gastrointestinal bleed | 36223 (1.4) | 10864 (1.5) | <0.001 |
| Other | 78771 (3.1) | 22786 (3.2) | 0.05 |
Note: Values are given as number (percentage).
Estimates from weighted survey data; χ2 test used for comparison
ESRD, end-stage renal disease
Mortality
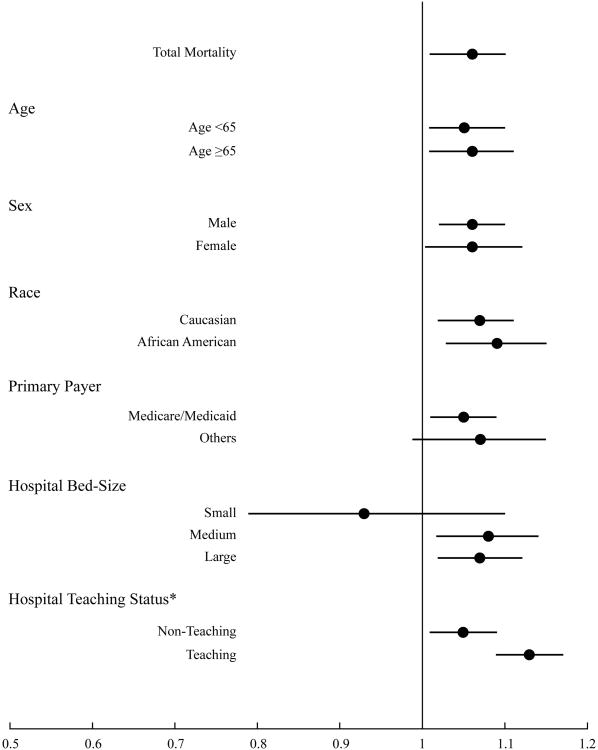
The unadjusted all cause in-hospital mortality was 5.4% for dialysis patients admitted during the weekdays in comparison to 5.8% for weekend admissions (Table 2). Even after adjusting relevant covariates, weekend admissions were associated with a 6% higher odds of death compared to those who were admitted during the weekdays (OR, 1.06; 95% CI, 1.01-1.10) (Fig 2) (Table 3). The unadjusted mortality by day three day of admission was similarly higher on weekends (5.4% vs. 4.5%; p<0.001) when compared to weekdays. After adjusting for relevant covariates, dialysis patients admitted over the weekends had an 18% higher odds of death by day three of admission than those who were admitted on weekdays (OR, 1.18; 95% CI, 1.10-1.26).
Table 2. Comparison of outcomes of ESRD patients admitted on weekdays versus weekends.
| Outcome** | Weekday (n*=2,574,081) | Weekend (n*=704,491) | P |
|---|---|---|---|
| All-cause in-hospital mortality* | 138517 (5.4) | 40666 (5.8) | <0.001 |
| Discharge disposition of survivors* | |||
| Home | 1433718 (55.7) | 386622 (54.9) | <0.001 |
| Other hospital | 66955 (2.6) | 18137 (2.5) | 0.6 |
| Skilled Nursing Facility | 553060 (21.5) | 154724 (22.0) | <0.001 |
| Home care | 335127 (13.0) | 89561 (12.7) | 0.006 |
| Against medical advice | 44758 (1.7) | 14345 (2.0) | <0.001 |
| Unknown | 1946 (0.1) | 436 (0.1) | 0.1 |
| LOS of survivors (d) | 4 [2-8] | 4 [3-8] | 0.001 |
| Time to death (d) | 6 [2-14] | 6 [2-13] | <0.001 |
Estimates from weighted survey data; χ2test used for comparison
Note: Values are given as number (percentage), except LOS and time to death, which are given as median [interquartile range] from non-survey weighted data, t-test on log-transformed values using survey weighted data used for comparison.
Primary and secondary.
ESRD, end-stage renal disease; LOS, length of stay
Fig 2.
Odds ratio and 95% confidence intervals for all-cause inpatient mortality associated with weekend admissions (vs. weekday admissions) in different subgroups. *OR of all-cause inpatient mortality are significantly different within subgroups of hospitals by teaching status using generalized Hausman Test (p=0.006)
Table 3. Multivariable regression for mortality with weekend as predictor variable, controlling for other covariates.
| Variables | OR (95% CI) | P |
|---|---|---|
| Weekend | 1.06 (1.01-1.10) | 0.009 |
| Age category | <0.001 | |
| 18-34 y | 1.00 (reference) | |
| 35-49 y | 1.66 (1.51-1.82) | |
| 50-64 y | 2.75 (2.51-3.01) | |
| 65-79 y | 4.34 (3.97-4.76) | |
| ≥80 y | 6.24 (5.69-6.85) | |
| Sex | <0.001 | |
| Male | 1.00 (reference) | |
| Female | 0.93 (0.91-0.95) | |
| Race | <0.001 | |
| Caucasian | 1.00 (reference) | |
| African American | 0.80 (0.77-0.83) | |
| Hispanic | 0.76 (0.72-0.79) | |
| Asian or Pacific Islander | 0.85 (0.78-0.92) | |
| Native American | 0.81 (0.68-0.95) | |
| Other | 0.90 (0.83-0.97) | |
| Missing | 0.93 (0.88-0.98) | |
| Primary Payer | <0.001 | |
| Medicare | 1.00 (reference) | |
| Medicaid | 1.02 (0.96-1.08) | |
| Private | 1.18 (1.12-1.24) | |
| Self-Pay | 1.44 (1.25-1.64) | |
| No Charge | 0.71 (0.29-1.73) | |
| Other | 1.51 (1.28-1.77) | |
| Modified Charlson's Index | <0.001 | |
| 0 | 1.00 (reference) | |
| 1-3 | 0.95 (0.92-0.98) | |
| 4-6 | 1.46 (1.39-1.54) | |
| ≥7 | 2.33 (2.18-2.50) | |
| Hospital Teaching Status | ||
| Non-Teaching | 1.00 (reference) | 0.7 |
| Teaching | 1.01 (0.96-1.06) | |
| Bed Size | 0.2 | |
| Small | 1.00 (reference) | |
| Medium | 0.92 (0.85-1.00) | |
| Large | 0.93 (0.86-1.01) | |
| Region of Hospital | <0.001 | |
| North East | 1.00 (reference) | |
| Mid-West | 0.82 (0.77-0.88) | |
| South | 0.96 (0.90-1.03) | |
| West | 0.98 (0.92-1.05) | |
| Year | 0.98 (0.97-0.99) | <0.001 |
| Primary diagnosis | ||
| Infections & access issues | 2.00 (1.94-2.07) | <0.001 |
| Cardiovascular diseases | 1.05 (1.01-1.10) | 0.02 |
| Gastrointestinal bleed | 0.80 (0.72-0.90) | <0.001 |
| Other | 0.34 (0.29-0.38) | <0.001 |
| Interactions with weekend admission | ||
| Cardiovascular diseases | 0.93 (0.86-0.99) | 0.03 |
| Hospital Teaching Status | 1.08 (1.02-1.14) | 0.005 |
OR, odds ratio; CI, confidence interval;
We did not find any significant difference in adjusted odds of mortality for weekend admissions within subgroups of age (<65 or ≥65 years), gender, race (Caucasian vs. African American), primary payer (Medicare or Medicaid vs others), or hospital bedsize but the adjusted odds of mortality in weekend admissions was significantly higher in teaching hospitals in comparison to non-teaching hospitals (Fig 2). To assess if the relationship changes over time we also checked for interaction between year and weekend admissions, which was not significant.
Disposition and Length of Stay
The patients admitted over weekends were less likely to be discharged home and more likely to be transferred to skilled nursing facilities in comparison to those admitted over weekdays (p<0.001 for both) (Table 2). We also found that time to death was shorter and length of stay of survivors was longer for weekend admissions in comparison to weekday admissions (Table 2). Similarly in comparison to those admitted over weekdays, the adjusted time to death of patients admitted over weekends was 9% shorter (OR, 0.91; 95% CI, 0.89-0.94), and the adjusted length of hospital stay of survivors was 3% longer (OR, 1.03; 95% CI, 1.02-1.04).
Sensitivity Analyses
The sensitivity analyses performed excluding race suggested 6% higher odds of all-cause inpatient mortality (OR, 1.06; 95% CI, 1.01-1.10) for weekend admissions in comparison to weekday admissions. Similarly it showed that weekend admissions were associated with increased adjusted mortality by third day of admission (OR, 1.17; 95% CI, 1.10-1.25), longer length of stay (OR, 1.03; 95% CI, 1.02-1.04) and shorter time to death (OR, 0.92; 95% CI, 0.89-0.94) in comparison to weekday admissions. These results are similar to the results of the primary analysis that included race. Similarly the other four sensitivity analyses showed similar trends as the primary analysis even after accounting for duplicate observations in different manners. (Table S2)
Discussion
Using a nationally representative dataset, we have demonstrated that patients on maintenance dialysis who are admitted over weekends have higher all-cause inpatient mortality in comparison to those admitted over weekends. This effect was present independent of patient demographics, insurance status, co-morbidities, admission diagnosis, and hospital characteristics such as size, location, geographical region and teaching status. We also found that although the adjusted length of hospital stay was not different between the two groups, the patients admitted over weekends did have a shorter time to death by almost a day. To make the weekend and weekday population as homogenous as possible, elective admissions were excluded as these are usually restricted to weekdays. Similarly primary discharge diagnosis common to maintenance dialysis patients like infections, dialysis access problems, cardiovascular diseases (including heart failure, acute coronary syndrome, atrial fibrillation/flutter and stroke), GI bleeding and others (including hypertensive emergency and hyperkalemia) were also adjusted for.
Previous studies have shown disparity in outcomes of patients admitted over weekends and weekdays1-6,12,13 however literature on outcomes of patients on maintenance dialysis admitted over weekends is sparse. A recent study compared outcomes of patients with acute kidney injury admitted over weekends and weekdays including patients needing dialysis,6 however none of these patients were on maintenance dialysis. Similarly, Bell et al 5 retrospectively examined 3.8 million acute care admissions in Canada and determined that weekends were associated with significantly higher mortality for 23 of 100 leading causes of death.25-27 In their study kidney failure was one of the 23 diagnoses, however the definition of kidney failure was unclear and patients included may have had acute kidney injury, chronic kidney disease or ESRD, as also speculated by other authors.28 Further, this subgroup had less than 3500 patients and mortality was adjusted for age, race, sex and Charlson's co-morbidity index but not for hospital characteristics, which has independent effects on patient outcomes6,29.
Patients receiving maintenance dialysis represent a unique population with high co-morbidities, high rates of hospitalizations and high mortality. Immune dysfunction has been well documented in these patients making them prone to poor outcomes30,31. In this study, we explored differences in outcomes of weekend vs weekday admissions, specifically for a much larger number of patients on maintenance dialysis and performed a more rigorous adjustment of our analysis. Additionally, we strengthened our model via sensitivity analysis and reached the same conclusions. Moreover, we found that the absolute risk increase for weekend admissions in comparison to weekday admissions was 0.4%, translating into one excess death for every 250 weekend admissions. If we take into account the rise in the number of patients needing maintenance dialysis and the high number of hospitalizations of this patient population, this finding assumes even greater clinical significance.
We further found that this disparity was even higher if we examined mortality by third day of admission (18% in comparison to 6% for total admission duration). This is in alignment with previous studies demonstrating much larger differences in short term mortality for weekend admissions in comparison to weekday admissions.5,32,6,33 Another important finding of our study is that the disparity in mortality for weekend admissions of maintenance dialysis patients did not differ within subgroups of age (<65 or ≥65 years), gender, race (Caucasian vs. African Americans) or hospital bed size. However weekend admissions to teaching hospitals had worse all-cause inpatient mortality in comparison to non teaching hospitals. Similar findings were reported by Cram et al23 using the 1998 California Office of Statewide Health Planning and Development Discharge Data File. They evaluated in-hospital mortality in patients admitted with 50 common diagnoses. Due to the availability during weekends of residents in training, one may expect more continuous patient care and thus better outcomes. In practice however, reduced staffing over weekends along with increased hand-offs and the need to cover more and unfamiliar patients in the hospital may contribute to this unexpected result.
The reasons for higher mortality for weekend admissions in maintenance dialysis population are not readily apparent from our analysis. Though there were some statistically significant differences in baseline characteristics of weekend and weekday admissions, even after adjusting for patient and hospital characteristics, co-morbidities, payer status, year and primary discharge diagnoses common to maintenance dialysis patients, higher mortality for weekend admissions persisted. There are some unique in-hospital circumstances which likely impact patients on maintenance dialysis more than other groups. The weekends usually have less available staff and resources and, depending on the structure of the hospital staff working over weekends, they may not be familiar with patients and may be less experienced. Decreased nurse staffing has been shown to be associated with worse outcomes.34,35 In addition, many long-term care facilities do not admit patients on weekends, thus stretching the already scant available resources over weekends in hospitals.
Although we have used a database with representative sample, our study has some limitations. We used ICD-9-CM codes for ESRD, dialysis, and acute kidney injury to identify our study population. While dialysis and acute kidney injury codes have been used previously, the ICD-9-CM codes for ESRD have not been validated.36 The same inclusion algorithm has however been used in the literature before16. Additionally, coding may vary amongst different hospitals and coding errors may have resulted in some degree of selection bias. However, we believe that such coding practices are unlikely to differ between weekdays and weekends. We classified weekend admissions as those occurring from midnight Friday to midnight Sunday. This does not take into account that health care services on Friday evenings, early mornings on Mondays and holidays are likely similar to those provided over weekends. We therefore may have underestimated the worse outcomes over weekends. Since maintenance dialysis facilities are open on Saturdays there may be a difference in outcomes of Saturday and Sunday admissions, however we were unable to differentiate between Saturday and Sunday admissions. Further, despite multivariable adjustment, we cannot exclude other unmeasured confounding factors that may have influenced our results. Additionally, we were not able to determine if the patients being admitted came from home or another health care facility. The database does not provide any unique patient identifiers, therefore, it is not possible to accurately distinguish readmissions of the same patient. However using patient characteristics, primary payer, hospital ID and year of admission we attempted to identify duplicate observations and performed four different sensitivity analyses based on the different ways of selecting unique observations with continued robustness of our results.
In summary, this study, which included a representative sample of non-elective inpatient admissions, provides evidence of worse outcomes for maintenance dialysis patients who were admitted over weekends. Future studies are needed to explore the reasons that might explain such findings and consider strategies to strengthen staffing and resources over weekends that might improve the quality of health care delivery for maintenance dialysis patients.
Supplementary Material
Table S1: ICD-9-CM codes for primary discharge diagnosis.
Table S2: Sensitivity analyses and effect on various outcomes.
Note: The supplementary material accompanying this article (doi:_______) is available at www.ajkd.org
Acknowledgments
Support: This publication was made possible by grant RR024990 (SDN) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. JDS is supported by the NIH/National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK085185) and investigator-initiated grant support from The PhRMA Foundation, Genzyme, and Roche Organ Transplant Research Foundation. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NCRR or NIH.
Footnotes
Financial Disclosure: The authors declare that they have no other relevant financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005 Aug 17;294(7):803–812. doi: 10.1001/jama.294.7.803. [DOI] [PubMed] [Google Scholar]
- 2.Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. 2007 Apr;38(4):1211–1215. doi: 10.1161/01.STR.0000259622.78616.ea. [DOI] [PubMed] [Google Scholar]
- 3.Crowley RW, Yeoh HK, Stukenborg GJ, Medel R, Kassell NF, Dumont AS. Influence of weekend hospital admission on short-term mortality after intracerebral hemorrhage. Stroke. 2009 Jul;40(7):2387–2392. doi: 10.1161/STROKEAHA.108.546572. [DOI] [PubMed] [Google Scholar]
- 4.Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2009 Mar;7(3):303–310. doi: 10.1016/j.cgh.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 5.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001 Aug 30;345(9):663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 6.James MT, Wald R, Bell CM, et al. Weekend hospital admission, acute kidney injury, and mortality. J Am Soc Nephrol. 2010 May;21(5):845–851. doi: 10.1681/ASN.2009070682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilbertson DT, Liu J, Xue JL, et al. Projecting the number of patients with end-stage renal disease in the United States to the year 2015. J Am Soc Nephrol. 2005 Dec;16(12):3736–3741. doi: 10.1681/ASN.2005010112. [DOI] [PubMed] [Google Scholar]
- 8.Collins AJ, Foley RN, Herzog C, et al. US Renal Data System 2012 annual data report. Am J Kidney Dis. 2013;61(1) 1:e1–e480. doi: 10.1053/j.ajkd.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 10.Introduction to the HCUP Nationwide Inpatient Sample. [Accessed Jan 5, 2013];2010 http://www.hcup-us.ahrq.gov/db/nation/nis/NISIntroduction2010.pdf.
- 11.Waikar SS, Wald R, Chertow GM, et al. Validity of International Classification of Diseases, Ninth Revision, Clinical Modification Codes for Acute Renal Failure. J Am Soc Nephrol Jun. 2006;17(6):1688–1694. doi: 10.1681/ASN.2006010073. [DOI] [PubMed] [Google Scholar]
- 12.Ananthakrishnan AN, McGinley EL, Saeian K. Outcomes of weekend admissions for upper gastrointestinal hemorrhage: a nationwide analysis. Clin Gastroenterol Hepatol. 2009 Mar;17(3):296–302e291. doi: 10.1016/j.cgh.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 13.Aujesky D, Jimenez D, Mor MK, Geng M, Fine MJ, Ibrahim SA. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009 Feb 24;119(7):962–968. doi: 10.1161/CIRCULATIONAHA.108.824292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crowley RW, Yeoh HK, Stukenborg GJ, Ionescu AA, Kassell NF, Dumont AS. Influence of weekend versus weekday hospital admission on mortality following subarachnoid hemorrhage. Clinical article. J Neurosurg. 2009 Jul;111(1):60–66. doi: 10.3171/2008.11.JNS081038. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992 Jun;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 16.Kumar G, Sakhuja A, Taneja A, et al. Pulmonary Embolism in Patients with CKD and ESRD. Clin J Am Soc Nephrol. 2012 Jul 26; doi: 10.2215/CJN.00250112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Survey Data Reference Manual Release 11. Stata Press; 2009. svy postestimation — Postestimation tools for svy; pp. 101–105. [Google Scholar]
- 18.Kim HM, Eisenberg D, Ganoczy D, et al. Examining the relationship between clinical monitoring and suicide risk among patients with depression: matched case-control study and instrumental variable approaches. Health Serv Res. 2010 Oct;45(5 Pt 1):1205–1226. doi: 10.1111/j.1475-6773.2010.01132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gallerani M, Boari B, Manfredini F, Mari E, Maraldi C, Manfredini R. Weekend versus weekday hospital admissions for acute heart failure. Int J Cardiol. 2011 Feb 3;146(3):444–447. doi: 10.1016/j.ijcard.2010.10.113. [DOI] [PubMed] [Google Scholar]
- 20.Horwich TB, Hernandez AF, Liang L, et al. Weekend hospital admission and discharge for heart failure: association with quality of care and clinical outcomes. Am Heart J. 2009 Sep;158(3):451–458. doi: 10.1016/j.ahj.2009.06.025. [DOI] [PubMed] [Google Scholar]
- 21.Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007 Mar 15;356(11):1099–1109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 22.Deshmukh A, Pant S, Kumar G, Bursac Z, Paydak H, Mehta JL. Comparison of outcomes of weekend versus weekday admissions for atrial fibrillation. Am J Cardiol. 2012 Jul 15;110(2):208–211. doi: 10.1016/j.amjcard.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 23.Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004 Aug 1;117(3):151–157. doi: 10.1016/j.amjmed.2004.02.035. [DOI] [PubMed] [Google Scholar]
- 24.Chung L, Krishnan E, Chakravarty EF. Hospitalizations and mortality in systemic sclerosis: results from the Nationwide Inpatient Sample. Rheumatology (Oxford) 2007 Dec;46(12):1808–1813. doi: 10.1093/rheumatology/kem273. [DOI] [PubMed] [Google Scholar]
- 25.Ensminger SA, Morales IJ, Peters SG, et al. The hospital mortality of patients admitted to the ICU on weekends. Chest. 2004 Oct;126(4):1292–1298. doi: 10.1378/chest.126.4.1292. [DOI] [PubMed] [Google Scholar]
- 26.Laupland KB, Shahpori R, Kirkpatrick AW, Stelfox HT. Hospital mortality among adults admitted to and discharged from intensive care on weekends and evenings. J Crit Care. 2008 Sep;23(3):317–324. doi: 10.1016/j.jcrc.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 27.Barnett MJ, Kaboli PJ, Sirio CA, Rosenthal GE. Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002 Jun;40(6):530–539. doi: 10.1097/00005650-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Halm EA, Chassin MR. Why do hospital death rates vary? N Engl J Med. 2001 Aug 30;345(9):692–694. doi: 10.1056/NEJM200108303450911. [DOI] [PubMed] [Google Scholar]
- 29.Ananthakrishnan AN, McGinley EL, Saeian K. Higher hospital volume is associated with lower mortality in acute nonvariceal upper-GI hemorrhage. Gastrointest Endosc. 2009 Sep;70(3):422–432. doi: 10.1016/j.gie.2008.12.061. [DOI] [PubMed] [Google Scholar]
- 30.Hauser AB, Stinghen AE, Kato S, et al. Characteristics and causes of immune dysfunction related to uremia and dialysis. Perit Dial Int. 2008 Jun;28(3):S183–187. [PubMed] [Google Scholar]
- 31.Kato S, Chmielewski M, Honda H, et al. Aspects of immune dysfunction in end-stage renal disease. Clin J Am Soc Nephrol. 2008 Sep;3(5):1526–1533. doi: 10.2215/CJN.00950208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marco J, Barba R, Plaza S, Losa JE, Canora J, Zapatero A. Analysis of the mortality of patients admitted to internal medicine wards over the weekend. Am J Med Qual. 2010 Jul-Aug;25(4):312–318. doi: 10.1177/1062860610366031. [DOI] [PubMed] [Google Scholar]
- 33.Barba R, Losa JE, Velasco M, Guijarro C, Garcia de Casasola G, Zapatero A. Mortality among adult patients admitted to the hospital on weekends. Eur J Intern Med. 2006 Aug;17(5):322–324. doi: 10.1016/j.ejim.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002 May 30;346(22):1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 35.Sasichay-Akkadechanunt T, Scalzi CC, Jawad AF. The relationship between nurse staffing and patient outcomes. J Nurs Adm. 2003 Sep;33(9):478–485. doi: 10.1097/00005110-200309000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Parikh DS, Swaminathan M, Archer LE, et al. Perioperative outcomes among patients with end-stage renal disease following coronary artery bypass surgery in the USA. Nephrol Dial Transplant. 2010 Jul;25(7):2275–2283. doi: 10.1093/ndt/gfp781. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: ICD-9-CM codes for primary discharge diagnosis.
Table S2: Sensitivity analyses and effect on various outcomes.
Note: The supplementary material accompanying this article (doi:_______) is available at www.ajkd.org