Abstract
Background/Context:
Antiplatelet drug resistance increases the risk of adverse events like stent thrombosis in acute coronary syndrome (ACS). Metabolic syndrome (MS) is a prothrombotic state and presence of MS further increases the risk of antiplatelet drug resistance.
Aims and Objectives:
We studied platelet aggregation characteristics in patients of ACS for aspirin or clopidogrel resistance. We studied the relation of drug resistance with blood markers like high sensitivity C-reactive protein (hsCRP). We also studied for any relation of drug resistance with presence of MS.
Materials and Methods:
We studied platelet aggregation characteristics by optical aggregometry using platelet-rich plasma (PRP) of patients. Collagen (2 μg/mL) and adenosine diphosphate (ADP; 10 μmol) were used. Greater than 50% aggregation in PRP of patients was taken as an evidence of drug resistance. Suitable blood tests were done including newer risk markers like hsCRP, apolipoprotein B, and fibrinogen.
Statistical test:
Statistical tests included Student's t-test and Kendall's rank correlation coefficient.
Results:
We had a total of 94 patients of ACS with 47 (50%) having MS. MS patients showed higher blood levels of hsCRP and fibrinogen. Twenty-eight (59.5%) patients with MS showed antiplatelet drug resistance compared to 12 patients without MS. Serum fibrinogen showed strongest correlation with drug resistance. HsCRP levels showed correlation with aspirin resistance (r = 0.53) only in the MS group.
Discussion and Conclusion:
We found significantly high prevalence of antiplatelet drug resistance. Aspirin and clopidogrel resistance was comparable. MS was a significant risk factor for drug resistance. The prothrombotic and proinflammatory markers showed strong correlation with drug resistance. A larger randomized trial is needed to better characterize this clinical problem.
Keywords: Aspirin resistance, clopidogrel resistance, fibrinogen, high sensitivity C-reactive protein, metabolic syndrome
INTRODUCTION
Metabolic syndrome (MS) consists of a combination of metabolic factors that gives rise to a proinflammatory and prothrombotic state and confers increased risk of cardiovascular (CV) mortality and morbidity. Besides the conventional markers like lipid profile, blood glucose and hypertension, some novel CV risk markers in MS have come up in recent years. These include angiotensin-converting enzyme (ACE), nitric oxide (NO), peroxisome proliferator-activated receptor (PPAR), soluble CD40 ligand (sCD40L), tumor necrosis factor (TNF), vascular cell adhesion molecule, high sensitivity C-reactive protein (hsCRP), apolipoprotein B, and fibrinogen.[1]
Light transmission aggregometry is the most widely used laboratory method to screen patients with suspected abnormalities of primary hemostasis due to inherited or acquired defects of platelet function.[2,3] It measures the increase in light transmission through platelet-rich plasma (PRP) that occurs when platelets are aggregated by an agonist. There are many preanalytical and analytical variables that affect the results of platelet aggregation in vitro. The failure of aspirin to prevent an arterial thrombotic event in vivo has been termed aspirin resistance. The failure of clopidogrel to prevent an arterial thrombotic event has been termed clopidogrel resistance. Aspirin resistance is prevalent in MS and is correlated with a number of variables. In the study by Goksel et al., this trend is clearly seen.[4] Current available data shows that about 4-30% of patients treated with conventional doses of clopidogrel do not display adequate antiplatelet response. Intrinsic mechanisms include genetic polymorphisms of the P2Y12 receptor and of the CYP3As, accrued release of adenosine diphosphate, or upregulation of other platelet activation pathways.[5]
Aspirin and clopidogrel are essential drugs in treatment of acute coronary syndrome (ACS). However, presence of resistance to their action is a practical problem that may cause increased risk of further vascular events. Thus, actual prevalence of antiplatelet drug resistance in the community must be known along with associated contributory factors like MS. This will help to decide on the dosing of these drugs or the use of alternative therapies to prevent further ACS in these patients.
High platelet reactivity in diabetic patients has been linked with a greater risk of adverse outcomes.[6] Potentially, increased doses of clopidogrel or aspirin, more potent agents such as prasugrel, or novel agents in development may be of incremental benefit.
We therefore undertook this study in a sample eastern Indian population to find the prevalence of aspirin/clopidogrel resistance in ACS patients. We also studied whether this drug resistance is commoner in patients with MS, a well-known vascular risk factor.
MATERIALS AND METHODS
This was an observational, cross-sectional, hospital-based, case control study conducted in a tertiary care center of eastern India from 1st April 2009 to 30th March 2011. Indoor and outdoor patients of Departments of Medicine and Cardiology were included after proper screening. ACS was diagnosed by records of echocardiography/ECG [electrocardiography]/angiography/isotope scan as available. We included patients of ACS who were receiving dual antiplatelet therapy of aspirin (150 mg/day) and clopidogrel (75 mg/day). Patients with renal or hepatic impairment, HIV infection, steroid intake, malabsorption, and malignancy were excluded. All blood tests were done at least 6 weeks after the acute event to avoid the acute phase changes in blood parameters like fibrinogen. All the patients were first clinically examined, followed by laboratory tests like blood glucose, lipid profile, hsCRP, fibrinogen, and apolipoprotein B (Beckman Coulter Synchron CX5 pro, USA). Normal values considered (according to literature of kit):
hsCRP: <1, low risk; 1-3, moderate risk; >3 mg/L, high coronary artery disease (CAD) risk
Apolipoprotein B: 0.52-1.63 g/L
Fibrinogen: 175-380 mg/dL.
Platelet aggregation study was done for each patient by optical aggregometry with adenosine diphosphate (ADP) and collagen in chronolog aggregometer 530™. All patients were asked to avoid foods like garlic or turmeric, which can affect platelet aggregation, at least for 3 days prior to the test. The reagents (supplied by same company) used were ADP (10 μmol) and collagen (2 μg/mL). ADP was used for testing clopidogrel resistance and collagen was used for aspirin resistance in PRP of the patient, obtained by centrifugation of citrated (1:9) blood at 1260-1300 rpm. For all patients, spontaneous platelet aggregation of PRP was also tested. All measurements were done at 37%C. Three minutes of aggregation characteristics have been used for each sample. More than 50% aggregation of a sample on addition of reagent is taken as platelet resistance. Results of platelet aggregation study are expressed dichotomously, that is, resistant vs no resistance. The patients were separated into two groups for subsequent analysis: Those with MS and those without. MS was diagnosed by standard criteria.[7]
The data was first arranged in Microsoft Excel worksheet. It was then analyzed using standard free online statistical software like Medcalc (version 11.3.6) and GraphPad. Discreet variables are expressed in percentages; continuous variables are expressed as mean ± standard deviation (SD). Pearson correlation coefficient is used to find correlation between continuous variables. For nonparametric variables, Kendall's rank correlation coefficient is used. The P < 0.05 are considered significant.
RESULTS
There were a total of 94 patients of ACS in our study. Of them, 47 had MS (group A) and remaining 47 had no MS (group B). As Table 1 shows, the groups were comparable with respect to demographical variables like age and gender. Sixty-six percent (n = 31) of patients with MS had BMI above 25, while 61.7% of group B had high BMI. This shows the generally high prevalence of obesity in our sample population, most of whom (n = 72; 76.6%) were urban. Smoking as a risk factor was more prevalent than alcohol intake (56.4 vs 18%).
Table 1.
Demographic characteristics of the patients
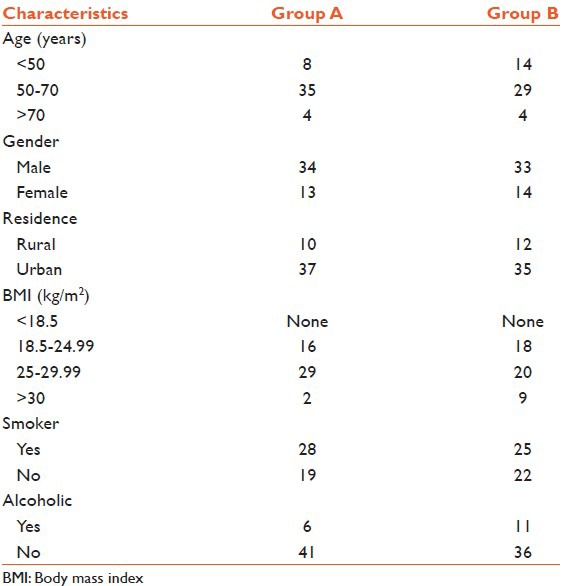
Table 2 shows the different parametric study parameters in the two groups. Those in the MS group had significantly higher blood hsCRP and fibrinogen levels. They also had higher waist circumference and triglyceride levels and lower high density lipoprotein (HDL) levels. The paradox of higher blood pressure in group B can be explained by the fact that patients with MS are more likely to receive different antihypertensives.
Table 2.
Comparison of different study parameters in two groups with statistical significance level using unpaired student’s t-test
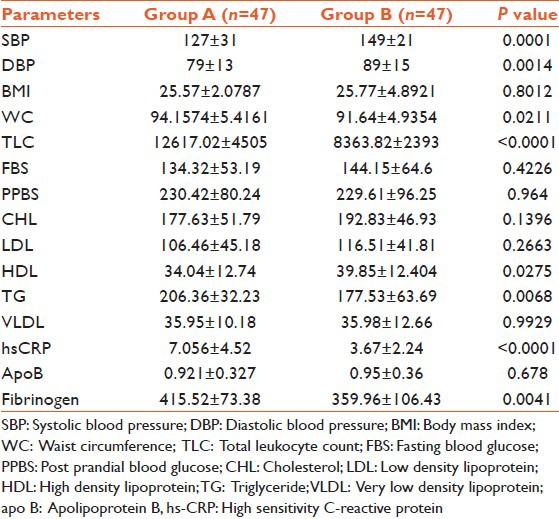
In group A, 40 (85%) patients had hsCRP levels above 3 mg/L; while in group B, 24 (51%) patients had this high level of hsCRP.
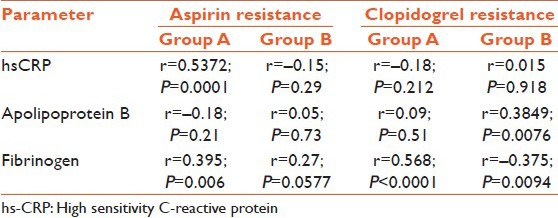
Figure 1 shows the number of aspirin and clopidogrel resistant cases in the two groups. The number of aspirin and clopidogrel resistant cases were comparable (21 vs 19). We did not find any case of dual drug resistance. In total there were 28 cases of antiplatelet drug resistance in group A and 12 such cases in group B (P = 0.0016 by Chi-square test, two-tailed). Thus, patients with MS had significantly higher incidence of antiplatelet drug resistance. There was no gender difference in drug resistance patterns. Table 3 shows the correlation of antiplatelet resistance with newer CV risk factors (by Kendall's rank correlation coefficient). It is seen that serum fibrinogen levels showed the strongest correlation with presence of antiplatelet drug resistance in both groups. Serum hsCRP levels showed strong correlation (r = 0.53) with aspirin resistance in group A. Thus, these newer risk markers have some correlation with resistance to antiplatelet drugs.
Figure 1.
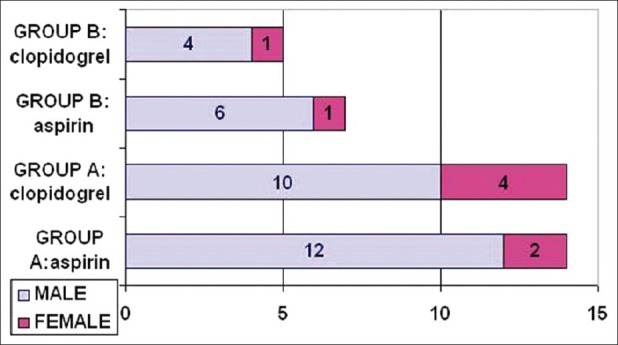
Resistance to antiplatelet drugs in the groups based on presence or absence of metabolic syndrome
Table 3.
Relation of platelet resistance with hsCRP, apolipoprotein B, and fibrinogen
DISCUSSION
In our cross-sectional study, we found significantly high levels of antiplatelet drug resistance in the patients with MS. However, even in ACS patients without MS, this drug resistance was present in significant number. We detected resistance to both aspirin and clopidogrel. MS patients in general had higher blood hsCRP and fibrinogen levels. The drug resistance showed correlation with hsCRP and fibrinogen.
MS is associated with higher proinflammatory and prothrombotic markers.[8] The levels of these markers also show positive correlation with different components of MS like waist circumference and body fat mass.[8] Thus, MS can be considered a proinflammatory state with release of different cytokines from adipose tissue.[9] As such, high hsCRP is associated with adverse CV outcome.[10] However, in MS patients, this risk is even more. In our patients with ACS, 64 (68%) had hsCRP levels above 3 mg/L; but 85% of the MS group had high hsCRP levels.
Aspirin resistance is a serious therapeutic problem. In different studies, 8-45% of the study population has been found to be aspirin resistant.[11] However, biochemical in vitro study results may not match with in vivo pharmacokinetics.[12] Various theories have been put forward to explain aspirin resistance like non-thromboxane mediated platelet activation, genetic polymorphism, or hyperlipidemia-induced increased sensitivity to collagen.[12] In these patients, probably higher dose of the drug is needed for therapeutic benefit. In our study, we found aspirin resistance in 21 (22%) of our patients; but 29.8% of patients with MS had this drug resistance as compared to 14.9% in the other group [vide Figure 1]. In a study from Turkey, they have found 22% prevalence of aspirin resistance in MS patients.[4] This aspirin resistance in that study was linked to high hsCRP levels. In our study too, we found significant correlation of aspirin resistance with hsCRP (r = 0.53; P = 0.0001) in group A patients.
Clopidogrel resistance is comparatively less studied. When ADP induced platelet aggregation >50% in blood of clopidogrel treated patients is taken as the definition of clopidogrel resistance, up to 40% of patients in different studies have been found to be resistant.[13] Clopidogrel resistance can give rise to clinical events like post percutaneous coronary intervention (PCI) stent thrombosis.[13] However, whether using higher dose of the drug can overcome this resistance is still debated.[14] In our study, we found clopidogrel resistance in 19 cases (20.2%). Of this 19, 14 (73.6%) had MS. MS, or diabetes in particular is known to cause reduced response to antiplatelet drugs.[15] This may be partly explained by alteration of the P2Y12-dependent pathway of platelet reactivity in these patients.[15]
Platelets in diabetic patients are hyperactive due to increased expression of surface adhesion molecules and receptors, and also disturbances in calcium homeostasis and prostaglandin pathways.[16] Another potential mechanism may be oxidative stress, which increases isoprostane production from arachidonic acid and thus increases the thromboxane pathway activation.[17] Platelet aggregation studies are finding their way in major guidelines too. In ACC guidelines on PCI, platelet aggregation studies are recommended if chance of clopidogrel resistance in deemed high.[18] Another guideline on antiplatelet drug usage for primary prevention of CV events in diabetes mentions that aspirin resistance is a possibility, but at this time, there is insufficient evidence to recommend increasing dose of aspirin in diabetics.[19] Current European guidelines on ACS also recommends platelet aggregation study for clopidogrel use if indicated (level IIb). Similarly, prasugrel is a newer antiplatelet drug which is thought to be better than clopidogrel in certain circumstances and may overcome resistance.
We also found serum fibrinogen levels correlating with antiplatelet drug resistance in our patients. MS is a prothrombotic state with inhibition of antifibrinolytic pathway.[20] Serum fibrinogen level is a marker of this procoagulant state. This can explain the correlation of fibrinogen with antiplatelet drug resistance [Table 3]. In a study from China, they found that high fibrinogen levels have an odds ratio (OR) of 2.973 in predicting aspirin resistance in regression analysis.[21]
In our study, patients with no MS also showed presence of drug resistance. Twelve patients (25.5%) of group B in our study showed resistance to any one antiplatelet drug [Figure 1]. This shows high prevalence of this resistance in the Indian population. In a study from Vellore, India they have found 38% prevalence of resistance to aspirin in patients with CVD.[22] In another study from Lucknow, they have found 12.7% of ACS patients showing less response to clopidogrel.[23] Thus, even in patients without MS, this resistance is a clinical problem.
Our study is limited by the small number of patients and lack of follow-up. Whether this laboratory drug resistance translates into actual increase in clinical events is not studied here. A larger multicentric trial is needed to actually find the clinical implication of this finding and to decide the need for increased dose of these drugs in our patients.
ACKNOWLEDGEMENT
The Principal, MSVP and Dean, student affairs of this medical College for allowing us to conduct the study and also for encouragement.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Koh KK, Han SH, Quon MJ. Inflammatory markers and the metabolic syndrome: Insights from therapeutic interventions. J Am Coll Cardiol. 2005;46:1978–85. doi: 10.1016/j.jacc.2005.06.082. [DOI] [PubMed] [Google Scholar]
- 2.Dacie JV, Lewis SM, Pitney WR, Brozovic M. Quantitative assay of coagulation factors. In: Dacie JV, Lewis SM, editors. Practical Haematology. 6th Ed. Edinburgh: Churchill Livingstone; 1984. pp. 248–58. [Google Scholar]
- 3.Cattaneo M. Inherited platelet-based bleeding disorders. J Thromb Haemost. 2003;1:1628–36. doi: 10.1046/j.1538-7836.2003.00266.x. [DOI] [PubMed] [Google Scholar]
- 4.Kahraman G, Sahin T, Kilic T, Baytugan NZ, Agacdiken A, Ural E, et al. The frequency of aspirin resistance and its risk factors in patients with metabolic syndrome. Int J Cardiol. 2007;115:391–6. doi: 10.1016/j.ijcard.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen TA, Diodati JG, Pharand C. Resistance to clopidogrel: A review of the evidence. J Am Coll Cardiol. 2005;45:1157–64. doi: 10.1016/j.jacc.2005.01.034. [DOI] [PubMed] [Google Scholar]
- 6.Angiolillo DJ, Bernardo E, Sabate M, Jimenez-Quevedo P, Costa MA, Palazuelos J, et al. Impact of platelet reactivity on cardiovascular outcomes in patients with type 2 diabetes mellitus and coronary artery disease. J Am Coll Cardiol. 2007;50:1541–7. doi: 10.1016/j.jacc.2007.05.049. [DOI] [PubMed] [Google Scholar]
- 7.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 8.Mauras N, Delgiorno C, Kollman C, Bird K, Morgan M, Sweeten S, et al. Obesity without established comorbidities of the metabolic syndrome is associated with a proinflammatory and prothrombotic state, even before the onset of puberty in children. J Clin Endocrinol Metab. 2010;95:1060–8. doi: 10.1210/jc.2009-1887. [DOI] [PubMed] [Google Scholar]
- 9.Sutherland JP, McKinley B, Eckel RH. The metabolic syndrome and inflammation. Metab Syndr Relat Disord. 2004;2:82–104. doi: 10.1089/met.2004.2.82. [DOI] [PubMed] [Google Scholar]
- 10.Wiwanitkit V. hs-CRP as a predictive factor for cardiac outcome. Ann Card Anaesth. 2010;13:74. doi: 10.4103/0971-9784.58844. [DOI] [PubMed] [Google Scholar]
- 11.Macchi L, Sorel N, Christiaens L. Aspirin resistance: Definations, mechanisms, prevalence, and clinical significance. Curr Pharm Des. 2006;12:251–8. doi: 10.2174/138161206775193064. [DOI] [PubMed] [Google Scholar]
- 12.Kour D, Tandon VR, Kapoor B, Mahajan A, Parihar A, Smotra S. Aspirin Resistance. JK Sci. 2006;8:116–7. [Google Scholar]
- 13.Vlachojannis GJ, Dimitropoulos G, Alexopoulos D. Clopidogrel resistance: Current aspects and future directions. Hellenic J Cardiol. 2011;52:236–45. [PubMed] [Google Scholar]
- 14.Wiviott SD, Trenk D, Frelinger AL, O’Donoghue M, Neumann FJ, Michelson AD, et al. PRINCIPLE-TIMI 44 Investigators. Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: The Prasugrel in comparison to clopidogrel for inhibition of platelet activation and aggregation-thrombolysis in myocardial infarction 44 trial. Circulation. 2007;116:2923–32. doi: 10.1161/CIRCULATIONAHA.107.740324. [DOI] [PubMed] [Google Scholar]
- 15.Scheen AJ, Legrand D. Aspirin and clopidogrel resistance in patients with diabetes mellitus. Eur Heart J. 2006;27:2900. doi: 10.1093/eurheartj/ehl295. [DOI] [PubMed] [Google Scholar]
- 16.Natarajan A, Zaman AG, Marshall SM. Platelet hyperactivity in type 2 diabetes: Role of antiplatelet agents. Diab Vasc Dis Res. 2008;5:138–44. doi: 10.3132/dvdr.2008.023. [DOI] [PubMed] [Google Scholar]
- 17.Anfossi G, Trovati M. Pathophysiology of platelet resistance to anti-aggregating agents in insulin resistance and type 2 diabetes: Implications for anti-aggregating therapy. Cardiovasc Hematol Agents Med Chem. 2006;4:111–28. doi: 10.2174/187152506776369908. [DOI] [PubMed] [Google Scholar]
- 18.Smith SC, Jr, Feldman TE, Hirshfeld JW, Jr, Jacobs AK, Kern MJ, King SB, 3rd, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention) Circulation. 2006;113:e166–286. doi: 10.1161/CIRCULATIONAHA.106.173220. [DOI] [PubMed] [Google Scholar]
- 19.Pignone M, Alberts MJ, Colwell JA, Cushman M, Inzucchi SE, Mukherjee D, et al. American Diabetes Association; American Heart Association; American College of Cardiology Foundation. Aspirin for primary prevention of cardiovascular events in people with diabetes: A position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation. Diabetes Care. 2010;33:1395–402. doi: 10.2337/dc10-0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nieuwdorp M, Stroes ES, Meijers JC, Büller H. Hypercoagulability in the metabolic syndrome. Curr Opin Pharmacol. 2005;5:155–9. doi: 10.1016/j.coph.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Liu Z, Yu Y, Mao Y, Wang X, Wang J, Huo Y. Profile and prevalence of aspirin resistance in patients with metabolic syndrome. J Geriatr Cardiol. 2008;5:7–10. [Google Scholar]
- 22.Thomson VS, John B, George P, Joseph G, Jose J. Aspirin resistance in Indian patients with coronary artery disease and cardiovascular events. J Postgrad Med. 2009;55:252–6. doi: 10.4103/0022-3859.58927. [DOI] [PubMed] [Google Scholar]
- 23.Kumar S, Saran RK, Puri A, Gupta N, Sethi R, Surin WR, et al. Profile and prevalence of clopidogrel resistance in patients of acute coronary syndrome. Indian Heart J. 2007;59:152–6. [PubMed] [Google Scholar]


