Abstract
Introduction:
to report our experience with 41 patients treated by early endoscopic realignment of complete post-traumatic rupture urethra.
Materials and Methods:
The study includes patients presented to our institute, between May 2004 and April 2009, with post-traumatic complete posterior urethral disruption. Preoperative retrograde urethrography, voiding cystourethrography and abdominopelvic CT were performed to evaluate the urethral defect length, the bladder neck competence, the prostate position, and the extent of the pelvic hematoma. Within the first week after trauma, antegrade and retrograde urethroscopy were performed to identify both urethral ends and insert urethral catheter. Patients were followed up by pericatheter retrograde urethrogram monthly postoperatively till catheter removal on disappearance of extravasation. Retrograde urethrography, voiding cystourethrography and urethroscopy were performed 1 month after the removal of the catheter. Follow-up abdominal ultrasound and uroflowmetry monthly till 6 months, bimonthly till 1 year, and every 3 months thereafter were encouraged. Urinary continence and postoperative erectile dysfunction were assessed by direct patient interview.
Results:
Forty one patients in the age group 17-61 years (mean 37.9) were treated. Patients were followed up for
Conclusions:
Early endoscopic realignment for complete posterior urethral rupture is a feasible technique with no or minimal intraoperative complications. The technique is successful as the definitive line of therapy in reasonable number of patients and seems to render further future interventions for inevitable urethral stricture easier.
Keywords: Early, endoscopic realignment, post-traumatic, posterior urethra, urethral rupture
INTRODUCTION
Stricture of the male urethra continues to be a common and often challenging urological condition. The treatment of urethral stricture has evolved over the past few decades; however, the three most commonly used procedures (dilation, endoscopic urethrotomy, and urethroplasty) have changed very little over the past few decades.[1] Urethral rupture repair may be immediate (primary realignment or sutured end-to-end anastomosis within 2 days after the trauma), delayed (endoscopic realignment or surgical end-to-end anastomosis 2-14 days after injury), or late (any type of repair 3 months or more after trauma).[2] The best line of treatment of posterior urethral disruption secondary to blunt pelvic trauma remains controversial. Although some investigators recommended early realignment of urethral distraction injuries; these series are often relatively small and follow-up is relatively short.[3,4] Although classic reports recommend suprapubic cystostomy placement at the time of trauma with delayed urethral reconstruction 4 to 6 months after trauma through perineal approach, series that advocate primary realignment show a lower rate of urethroplasty as well as the formation of potentially less significant strictures than those treated with suprapubic cystostomy and late repair.[4] Many authors believe that subsequent open repair is simpler when realignment has been done.[4,5,6] The major advantages of primary endoscopic realignment are its minimal blood loss, shorter hospital stay, and potentially less stricture formation when compared with suprapubic cystotomy and delayed urethral reconstruction.[3] In this combined prospective and retrospective study, we report our experience with early endourologic urethral realignment to determine the success rate and complications of this procedure.
MATERIALS AND METHODS
This is a combined prospective and retrospective study that included all patients who had post-traumatic complete posterior urethral disruption secondary to blunt pelvic trauma. Patients having associated other organ injury mandating abdominal exposure were excluded as they always managed by open urethral realignment at laparotomy. Between May 2004 and April 2009, all patients presented to our center with history of recent blunt pelvic trauma associated with urethral injury (suspected in patients having acute retention of urine, blood at the external urethral meatus, high-riding prostate, perineal hematoma, or significant pubic rami fracture) underwent immediate retrograde urethrography (RU) to ensure complete urethral rupture (guaranteed by complete extravasation of contrast with no contrast reach the urinary bladder). Study scientific approval was obtained from the urology department scientific board and ethically approved by the ethics committee of the Faculty of Medicine (that conforms to the provisions of the Declaration of Helsinki). Informed written consents were obtained from all patients before intervention with guarantee of confidentiality.
Initial management consisted of ultrasound-guided suprapubic cystostomy to relief retention of urine. Detailed history taking regarding voiding dysfunction and potency pattern before trauma was obtained. Digital rectal examination was performed to evaluate the anal sphincter tone and the distance to the prostate. As soon as the patients’ general conditions allow, voiding cystourethrography (VCUG) and abdominopelvic CT were performed to evaluate the bladder neck competence, the position of the prostate, and the extent of the pelvic hematoma, respectively. The length of the urethral defect was determined by concomitantly evaluating both RU and VCUG. All patients underwent primary endoscopic realignment within the first week.
The procedure
Primary endoscopic realignment was performed within the first week after trauma as soon as the general condition of the patient allowed. With the patient in the lithotomy position and under general anesthesia, a guide wire was passed through the suprapubic cystostomy to the urinary bladder. The suprapubic tract was dilated up to 24 Fr (French) using Amplatz dilators. The Amplatz sheath was inserted to pass the flexible cystoscope to visualize the bladder, bladder neck, and posterior urethra down to the rupture site. Simultaneously, retrograde urethroscopy-using rigid or flexible cystoscope or preferably short semirigid ureteroscope-was performed to visualize the anterior urethra up to the rupture site. In 36 patients, both antegrade and retrograde endoscopies met in the pelvic hematoma and the antegrade cystoscope guided the retrograde one to pass to the urinary bladder; a guide wire was passed through the retrograde endoscope to reach the urinary bladder. In five patients, a ureteral stent or guide wire was passed through the antegrade cystoscope and pushed down to the rupture site, grasped by the retrograde endoscope and pulled out through the external urethral meatus. A 16 Fr siliconized Foley's catheter was passed over the guide wire to the urinary bladder and left in place till absorption of the pelvic hematoma to guide both urethral ends to heal together. Suprapubic tube was left in every patient as safeguard if the urethral catheter is obstructed. Twice daily irrigation of the urethral catheters and intermittent closure and opening of the catheters every 4 to 6 hours to avoid catheter blockade and bladder defunctionalization, respectively, were encouraged in all patients. Urine acidification using daily vitamin C was encouraged to minimize catheters’ encrustation.
Patient monitoring
Pericatheter retrograde urethrogram was performed every month after the procedure to assess urethral healing. Catheters were removed when extravasation of the contrast disappeared. Patients were monitored by proper history taking for any difficulty or weak stream, RU, and urethroscopy 1 month after catheters’ removal. Ultrasound evaluation of postvoiding residual urine and uroflowmetry were done monthly till 6 months postoperatively and bimonthly thereafter till 1 year. Increasing postvoiding residual urine and/or decreasing flow rate suspect the development of stricture urethra and mandate RU. Passable urethral stricture after realignment was treated with internal urethrotomy with regular urethral dilation. Open urethroplasty was performed in cases of complete urethral obstruction after the procedure. Urinary continence and postoperative erectile function were assessed by direct patient interview. Follow-up visits every 3 months were advised for all patients after the first year.
RESULTS
A total of 41 patients were included in this study. Their age range was 17-61 years (mean 37.9 years). They presented to the trauma unit of our institution. The mechanism of injury was motor vehicle accident in 29 patients (70.7%), fall from height in 7 patients (17.1%), train accident in 3 patients (7.3%), and farming tractor roll over in 2 patients (4.9%). All patients had pelvic fractures associated with blood drop at the external urethral meatus and acute urinary retention. The operative time ranged from 36 to 106 minutes (mean 54 minutes). No intraoperative complications were encountered and no patients required blood transfusion. Patients were discharged from the hospital 2 to 4 days postoperatively. In all patients, serial pericatheter retrograde urethrogram showed urethral extravasation of the contrast at 1 and 2 months [Figure 1]. At 3 months follow-up, no contrast extravasation was detected [Figure 2] and catheters were removed at that time. After removal of urethral catheters, patients were classified into three groups. Group I, 18 patients (43.9%) had no difficulty during voiding. All those patients had no or constantly minimal postvoiding residual urine (less than 50 cc) on abdominal ultrasound evaluation and reasonable uroflowmetry findings (Qmax more than 15 ml/second) detected through the follow-up period. RU revealed normal urethra [Figure 3] with no postvoiding residual urine [Figure 4]. Group II, 15 patients (36.6%) developed difficulty during voiding and RU revealed passable stricture [Figure 5] that were successfully managed by internal urethrotomy and regular urethral dilation. Group III, 8 patients (19.5%) developed retention of urine and suprapubic cystostomy was reinserted. Successful perineal urethroplasties were done later on for them. Urethroplasties were not difficult than usual. Operative time was (75-145 minutes, mean 108 minutes). Blood loss was estimated to be (500-800 cc). Three patients had stress urinary incontinence after endoscopic realignment. Normal erectile function was preserved in 28 patients (68.3%). No specific RU, VCUG, or abdominopelvic CT findings could be detected to influence operative results.
Figure 1.

Pericatheter ascending urethrography–2 months after early urethral alignment–showing contrast extravasation
Figure 2.
Pericatheter ascending urethrography–3 months after early urethral alignment–showing contrast reaching the bladder with no extravasation
Figure 3.

Retrograde urethrography–3 months after catheter removal–showing contrast agent reaching the bladder freely
Figure 4.

Voiding cystourethrography–3 months after catheter removal–showing minimal postvoiding residual urine
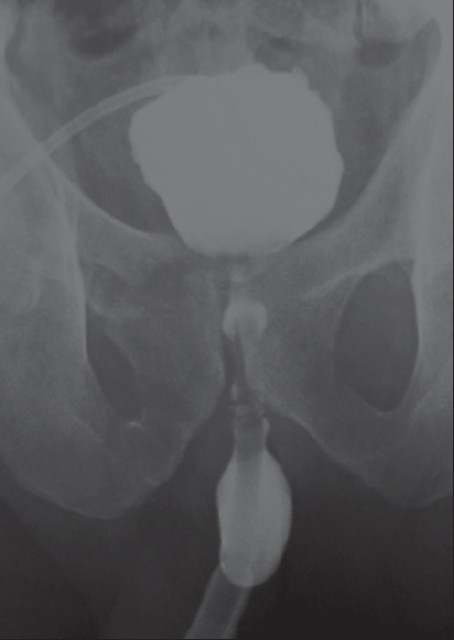
Figure 5.

Retrograde urethrography–2 months after catheter removal–showing urethral stricture after primary endoscopic alignment
DISCUSSION
Post–traumatic complete urethral disruption and its associated complications can be distressing to patients with pelvic fractures. The complications of urethral disruption including recurrent urethral stricture, impotence, and incontinence has a significant impact on the physical and emotional condition of those patients.[7] The goals of treatment of urethral disruption are achieving urethral continuity while minimizing the risk of complications. Treatment options of complete posterior urethral rupture include immediate primary realignment or end-to-end anastomosis within 2 days after the trauma, delayed endoscopic realignment or end-to-end anastomosis 2-14 days after injury, or late endoscopic or surgical repair 3 months or more after trauma.[2,8,9,10]
Before 1974, when Sachse[10] attempted the first endourologic repair of posterior urethral disruption using direct vision urethrotomy in a delayed fashion, suprapubic cystotomy and delayed repair was the procedure of choice for re-establishing urethral continuity.[3] Till now, some investigators consider suprapubic cystotomy and delayed urethroplasty the best treatment option.[11] Although suprapubic drainage with delayed repair has several advantages as avoidance of major operative procedure in acutely traumatized patients, decreasing the possibility of pelvic hematoma infection, and avoiding mobilization of the prostate and membranous urethra that might result in injury to penile nerve supply with consequential erectile dysfunction (ED), its drawbacks include the need for prolonged suprapubic drainage (3-6 months) and the inevitable urethral stricture that require one or more urethroplasties.[3]
Recent advances in endourologic instruments and techniques have led to early primary endoscopic realignment that is easy to perform and require minimal manipulations with comparable complications rate to that of delayed urethroplasty.[8,9] Some investigators consider that primary endoscopic urethral realignment may alleviate the need for open urethroplasty.[12,13] This is in agreement with our study, in which only eight patients (19.5%) required open urethroplasty.
The avulsed prostatic urethra is frequently displaced and misaligned with respect to the distal urethra. This eventually results in non-anatomic location that may complicate reconstruction.[9] In our study, we found that placing a urethral catheter across the urethral rupture site-without traction-prevents urethral nonalignment and corrects bladder displacement as the hematoma is absorbed where complete disappearance of extravasation is often associated with urethral alignment and restoring normal bladder position (comparing Figure 1 to Figures 2, 3 and 5. This is in agreement with Porter et al.,[7] who considered that this technique allows urethral realignment without disturbing the pelvic hematoma and the urethral catheter acts as a guide that allows the cut ends of the urethra to come together as the hematoma is reabsorbed.
The urethral catheter is left indwelling for 3 months until complete urethral healing. This time is the optimum time for complete healing of the urethra. Serial pericatheter ascending urethrogram was performed every month after the procedure. Extravasation of contrast was detected in the early films [Figure 1]. However, this extravasation disappeared completely 3 months after the procedure [Figure 2]. The catheter should be left in situ without traction to avoid damage of the continence mechanism of the bladder neck. This is important because the bladder neck constitutes the main sphincter mechanism after trauma.
Our results reported that primary endoscopic realignment was successful in 43.9% of patients with no need for further intervention. The need for additional procedures occurred in 56.1% of cases. These results are slightly less satisfactory than those achieved by Moudouni et al.,[3] who reported the need for additional endoscopic procedure in 41% of their patients. This difference might result from the inclusion of patients having partial (22.2% of cases) rather than complete urethral disruption in the other study.
In the current study, 36.6% of patients-who developed passable stricture-were all managed by internal urethrotomy and regular urethral dilatation. This is compatible with Tazi et al.,[14] who concluded that urethral strictures developed after primary endoscopic realignment are short and accessible to an endoscopic urethrotomy.
In our study, eight patients (19.5%) developed urethral stricture with retention of urine after removal of the urethral catheter. They required perineal urethroplasty to manage their stricture. This result was comparable with that of Goel et al.,[15] who reported that 23% of their cases required open surgery after endoscopic treatment. This slight difference may be attributed to the fibrosis and scar formation caused by later intervention in the other study (3-6 months). In agreement with Mouraviev et al.,[4] it is noted that urethroplasty after failure of endoscopic realignment is simple and easy to perform. This might result from the proper urethral alignment, the short distance between the distal and proximal ends of the urethra and the minimal periurethral fibrosis.
Some investigators reported no significant difference in both impotence and incontinence rates in patients treated with primary realignment versus those with delayed urethroplasty.[9,16] In our study, only 3 patients had stress urinary incontinence and 13 patients had ED postoperatively. From history taking, four patients had ED before trauma hence only nine patients (22%) had trauma-related ED. However, it was difficult to attribute this ED to the trauma itself or the endoscopic treatment. Nine patients had successful treatment with vasoactive therapy.
CONCLUSIONS
Early endoscopic realignment for complete posterior urethral rupture is a feasible technique with no or minimal intraoperative complications. The technique is successful as the definitive line of therapy in reasonable number of patients and seems to render further future interventions for inevitable urethral stricture easier. However, larger number of patients and longer follow-up period are required to exactly evaluate the advantages of this technique.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zehri A, Ather M, Afshan Q. Predictors of recurrence of urethral stricture disease following optical urethrotomy. Int J Surg. 2009;7:361–4. doi: 10.1016/j.ijsu.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 2.Nerli R, Koura A, Ravish I, Amarkhed S, Prabha V, Alur S. Posterior urethral injury in male children: long-term follow up. J Ped Urol. 2008;4:154–9. doi: 10.1016/j.jpurol.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Moudouni S, Patard J, manunta A, Guiraud P, Lobel B, Guille F. Early endoscopic realignment of post-traumatic posterior urethral disruption. Urology. 2001;57:628–32. doi: 10.1016/s0090-4295(00)01068-2. [DOI] [PubMed] [Google Scholar]
- 4.Mouraviev VB, Coburn M, Santucci RA. The treatment of posterior urethral disruption associated with pelvic fractures: Comparative experience of early realignment versus delayed urethroplasty. J Urol. 2005;173:873–6. doi: 10.1097/01.ju.0000152145.33215.36. [DOI] [PubMed] [Google Scholar]
- 5.Gheiler E, Frontera J. Immediate primary realignment of prostatomembranous urethral disruptions using endourologic techniques. Urology. 1997;49:596–9. doi: 10.1016/s0090-4295(97)80002-7. [DOI] [PubMed] [Google Scholar]
- 6.Ku J, Kim M, Jeon Y, Lee N, Park Y. Management of bulbous urethral disruption by blunt external trauma: The sooner, the better? Urology. 2002;60:579–83. doi: 10.1016/s0090-4295(02)01834-4. [DOI] [PubMed] [Google Scholar]
- 7.Porter J, Takayama T, Defalco A. Traumatic posterior posterior urethral injury and early realignment using magnetic urethral catheters. J Urol. 1997;158:425–30. [PubMed] [Google Scholar]
- 8.Yasuda K, Yamanishi T, Isaka S, Okano T, Masai M, Shimazaki J. Endoscopic re-establishment of membranous urethral disruption. J Urol. 1991;145:977–9. doi: 10.1016/s0022-5347(17)38505-1. [DOI] [PubMed] [Google Scholar]
- 9.Follis H, Kock M, Mcdougal W. Immediate management of prostatomembranous urethral disruptions. J Urol. 1992;147:1259–62. doi: 10.1016/s0022-5347(17)37534-1. [DOI] [PubMed] [Google Scholar]
- 10.Sachse H. Treatment of urethral stricture: Transurethral slit in view using sharp section. Fortschr Med. 1974;92:12–5. [PubMed] [Google Scholar]
- 11.Philipraj SJ. Delayed repair is the ideal management for posterior urethral injuries-For the motion. Indian J Urol. 2010;26:305–9. doi: 10.4103/0970-1591.65414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jepson B, Boulier J, Moore R, Parra R. Traumatic posterior urethral injury and early primary endoscopic realignment: Evaluation of long-term follow-up. Urology. 1999;53:1205–10. doi: 10.1016/s0090-4295(99)00003-5. [DOI] [PubMed] [Google Scholar]
- 13.Ikuerowo SO, Omisanjio OA, Esho JO, Balogun BO, Akinola RA. Combined antegrade and retrograde endoscopic realignment of traumatic urethral disruption. Internet J Urol. 2010;7:1. [Google Scholar]
- 14.Tazi H, Ouali M, Lrhorfi MH, Moudouni S, Tazi K, Lakrissa A. Endoscopic realignment for post-traumatic rupture of posterior urethra. Prog Urol. 2003;13:1345–50. [PubMed] [Google Scholar]
- 15.Goel M, Kumar M, Kapoor P. Endoscopic management of traumatic posterior urethral stricture: Early results and follow up. J Urol. 1997;157:95–7. [PubMed] [Google Scholar]
- 16.Husmann DA, Wilson WT, Boone TB, Allen TD. Prostatomembranous urethral disruption: Managed by suprapubic cystostomy and delayed urethroplasty. J Urol. 1990;144:76–8. doi: 10.1016/s0022-5347(17)39371-0. [DOI] [PubMed] [Google Scholar]


