Abstract
Percutaneous renal access is a common procedure in urologic practice. The main indications are drainage of an obstructed and hydronephrotic kidney and antegrade renal access prior to percutaneous renal surgeries such as percutaneous nephrolithotomy (PCNL) and percutaneous endopyelotomy (EP). The contraindications for this technique are patients with history of allergy to topical or local anesthesia and patients with coagulopathy. The creation of a percutaneous tract into the renal collecting system is one of the important steps for percutaneous renal access. This step usually requires imaging.
The advantages and disadvantages of each modality of image guidance are controversial. We performed a structured review using the terms: Percutaneous nephrostomy, guidance, fluoroscopy, ultrasonography, computed tomography (CT) scan, and magnetic resonance imaging (MRI). The outcomes are discussed.
Keywords: Percutaneous nephrolithotomy, percutaneous renal surgery, radiation, urolithiasis
THE MODALITIES OF IMAGING
Ultrasonographic guidance
Real-time diagnostic ultrasonography (US) has been widely accepted as the imaging guidance for a dilated renal collecting system. The overall success rate is 88-99%. The complication rate is 4-8% and depends on the indications.[1,2,3] Ultrasound is radiation free, effective, and rapid, and is possible with a portable machine causing minimal complications in experienced hands.
The primary advantages of ultrasonographic guidance are as follows:
Minimizes radiation exposure for patients and operating personnel
Imaging of structures between skin and kidney; the depth of access needle and the anatomy around kidney can be evaluated by ultrasound. This technique can prevent adjacent and visceral organ injury
No need of contrast media, especially for patients with azotemia
Avoids intrarenal vascular injury (color Doppler ultrasound)
Overcomes the problem of unsuccessful retrograde ureteral catheterization that is required for contrast media injection in fluoroscopic guidance
Safe for patients, especially pregnant and pediatric patients
The procedure can be performed in supine position.
The disadvantages of ultrasonographic guidance are:
Sonographic identification of the needle needs operator skill but successful puncture of the collecting system can be confirmed by the appearance of urine following removal of the needle obturator
Technical difficulty in percutaneous access of non or mild hydronephrosis; this can be overcome by administration of diuretic which transiently dilates the calyces
Inability to clearly visualize and manipulate a guide wire following renal access.
The important anatomical landmarks during sonographic examination are renal capsule, renal cortex (low-level homogenous echoes), renal medulla (sonolucent structure), and hydronephrosis (hypoechoic cavity surrounded by a central echo complex).
Access under ultrasonographic guidance without a needle guide is an alternative technique useful in bedside, grossly hydronephrotic kidney but requires special training.[4]
During percutaneous nephrolithotomy (PCNL), renal access is usually achieved by fluoroscopy under combined fluoroscopic/ultrasound guidance. Hosseini and colleagues[5] performed ultrasound-guided PCNL in 47 patients of renal pelvic stone of size 24-46 mm with mild to moderate hydronephrosis. The success rate was 93.61%. All steps of PCNL including dilatation were performed under ultrasonographic guidance. The advantage of this technique is that it is an alternative method to fluoroscopy-guided PCNL without radiation exposure to the operator and patient. Ultrasound can be used for localization of renal stone, especially non-opaque stone. Basiri et al. presented the technique of totally US-guided PCNL in 30 patients under flank position. This technique provided satisfactory outcomes without any major complications.[6]
Gamal et al.[7] reported on the safety of solo US-guided PCNL in the treatment of single pelvic stone in moderately to severely dilated pelvicalyceal system in 34 patients. Renal access via middle calyx and tract dilatation step were performed under US guidance with a needle-guided system attached to the side wall of US probe. Perforation of pelvicalyceal system was found in two cases with successful management with DJ stent insertion for 4 weeks. Two patients had residual stones which needed shock wave lithotripsy, and both become stone free.
Avoiding injury to the vascular network in the kidney is very important for safe surgery. Doppler ultrasound can demonstrate the intrarenal arteries, helping operators avoid injury. Doppler ultrasound can display renal artery/vein, including arcuate artery and peripheral cortical arteries. Tzeng et al.[8] reported on a randomized study comparing B-mode ultrasound and color Doppler ultrasound in percutaneous renal access. Blood loss, determined as change in hemoglobin level, in B-mode ultrasound and color Doppler ultrasound was 2.34 ± 0.43 g/dl and 1.50 ± 0.61 g/dl, respectively (P > 0.001). Rate of blood transfusion was 6% in B-mode group and 2% in color Doppler ultrasound group (P > 0.001). This study demonstrated color Doppler ultrasound to be more accurate and safer with less blood loss, compared to B-mode ultrasound. The advantage of color Doppler ultrasound was further confirmed by a comparative study in mini-invasive percutaneous nephrolithotomy (m-PCNL). Compared with the B-mode ultrasound group, hemorrhagic complications and blood transfusion rate were significantly less in color Doppler ultrasound group where no major hemorrhagic complications occurred. The incidence of patients requiring blood transfusion, renal arteriovenous fistula and hemorrhage requiring embolization were 2.6, 1.1%, and 1.1%, respectively. The technique of renal access using color Doppler ultrasound is thus very important, especially in patients with a solitary kidney.[9]
The advancements in ultrasound technology, 3-D ultrasound (3 DUS) and 4-D ultrasound (4DUS) can be used in clinical practice at the patient's bedside. John et al. compared 2D and 4D guidance for renal access. There was no significant difference in the puncture time (1.8 min for 2 DUS and 2 min for 4 DUS) and no difference in the quality of puncture. 4 DUS had a higher difficulty rating compared to 2 DUS. This advanced technique needs more investigation to prove its efficacy for this indication.[10]
Fluoroscopy
The high-quality of current C-arm fluoroscopic equipment and the familiarity among urologists of fluoroscopic imaging has led to its preferred use in percutaneous renal access, particularly in the operating room. Surgeons prefer fluoroscopy for guidance due to the clear visibility of the needle and guide wire. For percutaneous renal surgeries such as PCNL or endopyelotomy, fluoroscopic monitoring is very important for the entire procedure during renal access, guide wire manipulation, tract dilatation, residual stone evaluation, and post-procedural nephrostogram.
The advantages of fluoroscopic guidance are:
Its familiarity to most urologists
Its ability to visualize radiopaque calculi
Iodinated contrast media can be used to aid in stone localization
Demonstrates anatomical details.
Radiation safety is one of the major concerns during PCNL under fluoroscopic guidance. The maximum yearly whole-body exposure to radiation recommended by the National Council on Radiation Protection is 5 rem.[11] The radiation dose exposure depends on time, distance, and shielding. The fluoroscopic time should be as minimal as possible. Fluoroscopic screening time (FST) during PCNL is the main factor in radiation exposure. During fluoroscopic guidance in PCNL, the maximum radiation exposure is to the surgeon, especially to the legs and least to the eye, followed by the assistant and nurse.[12] Tepeler et al.[13] reported that large stone and multiple accesses are factors that can affect the FST during PCNL. FST is not affected by body mass index (BMI), stone configuration, degree of hydronephrosis, site of access, and history of open nephrolithotomy. In patients with large stones requiring multiple accesses, the procedure should be performed by experienced surgeons to diminish radiation exposure. Radiation dose reduction can be achieved by directing the fluoroscopy beam from under the table. The surgeon should wear a lead apron, thyroid shields, lead-impregnated glasses, and lead gloves. Young children are more radiosensitive and radiation exposure has been linked to malignancies, including thyroid cancer and leukemia. Radiation exposure should be minimized in this specific group of patients.
The renal collecting system can be opacified with contrast following cystoscopic retrograde ureteral catheter placement or by injection of intravenous contrast material. During this procedure, injecting the collecting system with contrast can cause pyelotubular and pyelovenous backflow. The two methods of percutaneous renal access under fluoroscopic guidance are “triangulation” and “eye of the needle” (Bull's eye) techniques. The choice of the technique depends on the experience of the operator. There was no difference in fluoroscopic time, operative time, hospital stay, complication rate, and success rate between both groups (patients in the “eye of the needle” group had higher complication and more blood loss than patients in the “triangulation” group).[2]
A novel digital technology fluoroscopy system with three-dimensional (3D) reconstruction for renal access has been attempted in a pig model. The advantages of the system are determination of the volume of kidney and renal calyx anatomy for delineation of the target calyx.[14]
The ideal imaging guidance for renal access may be a combination of initial ultrasonography followed by fluoroscopy for control of catheter and guide wire manipulation.[15]
CT, MRI and robotic-assisted percutaneous guidance
Computed tomography (CT) guidance is another alterative for management of complex cases. This imaging guidance is essential in patients with specific medical conditions such as morbid obesity, splenomegaly, hepatomegaly, severe skeletal anomalies like scoliosis or kyphosis, or who have had previous major intra-abdominal surgery, and in patients with minimal or no dilatation of renal pelvis.[16,17]
Cross-sectional imaging is needed to facilitate safe access in cases with difficult access to the collecting system, which is usually needed in patients with retrorenal colon, spinal dysraphism, ileal conduits, nephrolithiasis in the presence of angiomyolipomas, and in morbidly obese patients with malrotated kidney. Chalasani et al. studied the position of colon in the prone position by CT Kidney-Ureter-Bladder (KUB) in 134 patients. The prevalence of retrorenal colon in men was 13.6% on the right and 11.9% on the left, and in women was 13.4% on the right and 26.2% on the left. They suggested preoperative imaging for patients at higher risk of retrorenal colon who should have alternative technique in renal access such as ultrasound and CT guidance.[18] The technique for CT guidance for percutaneous access is similar to the technique of CT-guided drainage procedure in patients with urinoma drainage or other perinephric abnormalities.
MRI guidance has the advantage of no radiation exposure.[19] However, the use of MRI for renal access is limited and development of new technology of MR scanners with faster scanning and better physical access to patients may increase its utility.
Clinical application of robotic-assisted percutaneous guidance system is limited due to its complicated technology. The depth and angulation of the percutaneous access tract to the collecting system are controlled on fluoroscopic or CT-based data. Proper needle position can be enhanced by standard C-arm fluoroscopy unit with visible laser guidance systems.
Endoscopic guidance
Ureteroscopic equipment, including flexible scopes are now widely available permitting retrograde intra-renal surgery (RIRS). Retrograde nephrostomy by Lawson's procedure was reported in 1980. Using the same principle, flexible ureteroscopy-assisted retrograde nephrostomy is a new option for renal access in a non-dilated collecting system.[20] The advantages of this technique are continuous visualization of all steps of PCNL by renal access through Amplatz sheath placement, less radiation exposure, less bleeding, and being a shorter procedure especially in patients with non-dilated collecting systems. Grasso et al.[21] performed flexible ureteroscopy for assisting renal access in seven patients in minimally dilated collecting systems, obese patients, those in whom prior attempts of percutaneous access had failed and in patients who had calyceal diverticular calculi. The desired calyx can be selected under direct vision. The renal access is achieved under fluoroscopic guidance, but the tip of the needle is visualized and monitored by fluoroscopy and endoscopy. The guide wire can be placed through-and-through, allowing safe PCNL.
Bader et al.[22] described the experience of “all-seeing needle” as an optical puncture system in PCNL procedure for optimal renal access. The micro-optics of 0.9 mm and 0.6 mm diameter with integrated light lead was inserted through the working channel of an access needle of size 4.85 Fr outside diameter, which was connected to an irrigation system for better intraoperative view. The punctured calyces and calculi in all 15 patients could be visualized prior to placement of guide wire and tract dilatation. This technique can improve the safety of renal access.
Chen et al.[3] reported a new device called 'sonic flashlight’ to visualize and guide the needle during renal access. This novel technique is a real-time tomographic reflection which generates a virtual anatomically scaled image. The demonstration of sonographic image appears from the tip of the transducer. This technique can facilitate safe renal access for complicated cases.
EFFECT OF PATIENT POSITION AND SITE OF ACCESS ON RENAL ACCESS GUIDANCE
The ideal patient position for optimal renal access is still controversial. PCNL can be done in prone, prone-flexed, supine, supine oblique, and split-leg modified lateral positions.[15,23,24,25,26] The advantages of the prone position are significantly shorter nephrostomy tract length and potentially greater access sites. Simultaneous antegrade and retrograde upper urinary tract access is the advantage of supine and lateral positions, but renal access in these positions is usually achieved under ultrasonographic guidance. Percutaneous upper pole renal access including supracostal access is usually performed under fluoroscopic guidance as the technique requires coordination with anesthesiologists.[15] Hoznek et al.[27] reported PCNL in supine position under fluoroscopy guidance in patients who had unsuccessful renal access under ultrasonic guidance. A successful puncture was achieved in the first attempt in 7 of 10 patients without any complications. Fluoroscopic guidance is also useful in the supine position for an urologist who is not familiar with ultrasonic guidance.
Falahatkor et al.[28] compared PCNL in supine position under ultrasonographic guidance and fluoroscopic guidance. No significant difference in mean operative time, stone-free rate, hospital stay, and complication was found between both groups. More patients in the ultrasonic guidance group needed blood transfusion (3 patients: 1 patient). The advantages of this technique are less radiation exposure to the operator and staff personnel, identification of the anatomy between skin and kidney, making the operator feel more comfortable during operation without lead shied apron, and avoidance of contrast media administration.
The advantages of total ultrasound guidance in supine position have also been reported. Zhou et al. performed this technique in 92 m-PCNL patients, with 82.6% of total stone clearance and 1 patient requiring blood transfusion.[29] Basiri et al. reported ultrasound guidance in supine position in 19 patients, with a total stone-free rate of 84% without visceral injury.[30]
COMPARATIVE DATA
Various studies comparing the two common guidance systems are listed in Table 1. Basiri et al. compared ultrasonographic-guided access for PCNL in prone position in 50 patients with conventional fluoroscopic-guided access in another 50 patients. After successful access under ultrasonography guidance, the site of puncture was controlled using fluoroscopy. The mean age and sex ratios were not different in both groups. Time for access was significantly longer in the ultrasonographic-guided patients, but their duration of radiation exposure was lower. The authors concluded that PCNL under ultrasonographic guidance is an acceptable alternative to fluoroscopy and reduces radiation hazards.[31]
Table 1.
Studies comparing ultrasound and fluoroscopy guided access in PCNL
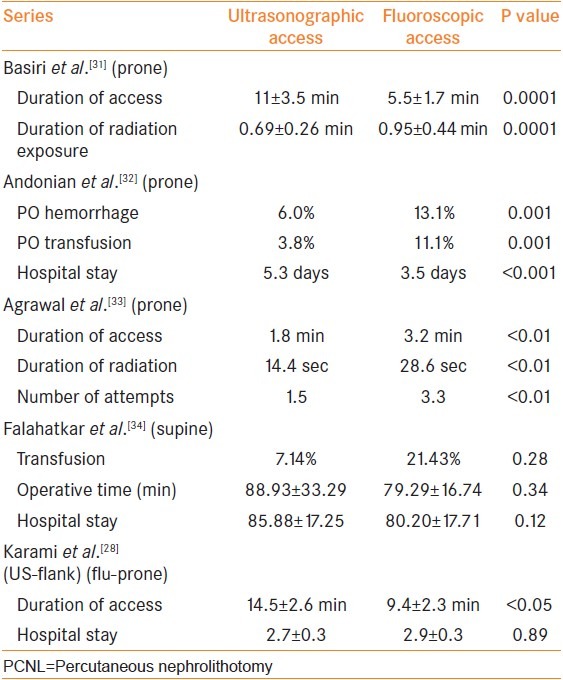
The international Clinical Research Office of the Endourological Society (CROES) analyzed the perioperative outcomes of PCNL using different imaging modalities such as ultrasound or fluoroscopic guidance. For renal access, 453 matched samples of both groups were compared with respect to frequency and pattern of Clavien complications and success rate. The stone-free rate was not different between both groups, but longer hospital stay was found in the ultrasound group (5.3 days compared to 3.5 days in the fluoroscopy group, P > 0.001). Postoperative blood transfusion was significantly higher in the fluoroscopy group (11.1% compared to 3.8% in the ultrasound group, P = 0.001). Larger size of access sheath was used in the fluoroscopy group (average 29.5 F compared to 22.6 F in the ultrasound group), which might be related with the higher incidence of hemorrhage.[32]
Agarwal et al. compared the safety and efficacy of US-guided renal access with fluoroscopy-guided renal access. The mean time to successful puncture, duration of radiation exposure, and mean number of attempts for successful puncture were higher in the fluoroscopy group. The radiation exposure and mean time of tract formation were 82 sec and 7.4 min, respectively, in the fluoroscopy group and 58 sec and 4.8 min, respectively, in the ultrasound group (P > 0.01). No significant difference was found in the successful access rate, stone-free rate, hospital stay, and incidence of hemorrhage requiring transfusion between both the groups.[33]
Karami et al. reported the use of ultrasound guidance for PCNL in the flank position with a high success rate and limited complications. However, the time for access was longer for ultrasound guidance (14.5 ± 2.6 min in ultrasound group and 9.4 ± 2.3 min in fluoroscopy group, P > 0.05).[34]
Falahatkar et al. reported the advantages of totally ultrasound guided PCNL in 14 patients compared to fluoroscopic-guided supine PCNL in 14 patients as being elimination of X-ray exposure, avoidance of contrast media administration, decrease of energy expenditure, and demonstration of anatomy between skin and kidney. The mean operative time, stone-free rate, hospital stay, transfusion rate, and postoperative complications were not different between the two groups.[28]
CONCLUSIONS
Each percutaneous renal guidance techniques has its advantages and disadvantages and no single technique is ideal in all circumstances. The two most commonly used modalities are ultrasonography and fluoroscopy. Color Doppler ultrasound, an addition to B-mode ultrasound guidance, can help avoid vascular injury, resulting in decreased intraoperative and postoperative hemorrhage. CT guidance is only used for access in complicated cases. MRI and robotic-assisted guidance are in their infancy and need more research. Endoscopic guide can improve the safety of renal access, but the cost, and experience of the operators need to be considered.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Juul N, Nielsen V, Torp-Peterson S. Percutaneous balloon catheter nephrostomy guided by ultrasound. Results of a new technique. Scand J Urol nephrol. 1985;19:291–4. doi: 10.3109/00365598509180272. [DOI] [PubMed] [Google Scholar]
- 2.Tepeler A, Armaðan A, Akman T, Polat EC, Ersöz C, Topaktaþ R, et al. Impact of percutaneous renal access technique on outcomes of percutaneous nephrolithotomy. J Endourol. 2012;26:828–33. doi: 10.1089/end.2011.0563. [DOI] [PubMed] [Google Scholar]
- 3.Chen ML, Shukla G, Jackman SV, Tsao AK, Smaldone MC, Ost MC, et al. Real-time tomographic reflection in facilitating percutaneous access to the renal collecting system. J Endourol. 2011;25:743–5. doi: 10.1089/end.2010.0375. [DOI] [PubMed] [Google Scholar]
- 4.Desai M. Ultrasonography-guided punctures with and without puncture guide. J Endourol. 2009;23:1641–3. doi: 10.1089/end.2009.1530. [DOI] [PubMed] [Google Scholar]
- 5.Hosseini MM, Hassanpour A, Farzan R, Yousefi A, Afrasiabi MA. Ultrasonography-guided percutaneous nephrolithotomy. J Endourol. 2009;23:603–7. doi: 10.1089/end.2007.0213. [DOI] [PubMed] [Google Scholar]
- 6.Basiri A, Ziaee SA, Nasseh H, Kamranmanesh M, Masoudy P, Heidary F, et al. Totally ultrasonography-guided percutaneous nephrolithotomy in the flank position. J Endourol. 2008;22:1453–7. doi: 10.1089/end.2007.0391. [DOI] [PubMed] [Google Scholar]
- 7.Gamal WM, Hussein M, Aldahshoury M, Hammady A, Osman M, Moursy E, et al. Solo ultrasonography-guided percutanous nephrolithotomy for single stone pelvis. J Endourol. 2011;25:593–6. doi: 10.1089/end.2010.0558. [DOI] [PubMed] [Google Scholar]
- 8.Tzeng BC, Wang CJ, Huang SW, Chang CH. Dopper ultrasound-guided percutaneous nephrolithotomy: A prospective randomized study. Urology. 2011;78:535–9. doi: 10.1016/j.urology.2010.12.037. [DOI] [PubMed] [Google Scholar]
- 9.Lu MH, Pu XY, Gao X, Zhou XF, Qiu JG, Si-Tu J. A comparative study of clinical value of single B-mode ultrasound guidance and B-mode combined with color doppler ultrasound guidance in mini-invasive percutaneous nephrolithotomy to decrease hemorrhagic complications. Urology. 2010;76:815–20. doi: 10.1016/j.urology.2009.08.091. [DOI] [PubMed] [Google Scholar]
- 10.John BS, Rowland D, Ratnam L, Walkden M, Nayak S, Patel U, et al. Percutaneous renal intervention: Comparison of 2-D and time-resolved 3-D (4-D) ultrasound for minimal calcyceal dilation using an ultrasound phantom and fluoroscopic control. Ultrasound Med Biol. 2008;34:1765–9. doi: 10.1016/j.ultrasmedbio.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Safak M, Olgar T, Bor D, Berkmen G, Gogus C, et al. Radiation doses of patients and urologists during percutaneous nephrolithotomy. J Radiol Prol. 2009;29:409–15. doi: 10.1088/0952-4746/29/3/005. [DOI] [PubMed] [Google Scholar]
- 12.Majidpour HS. Risk of radiation exposure during PCNL. Urol J. 2010;7:87–9. [PubMed] [Google Scholar]
- 13.Tepeler A, Binbay M, Yuruk E, Sari E, Kaba M, Muslumanoglu AY, et al. Factors affecting the fluoroscopic screening time during percutaneous nephrolithotomy. J Endourol. 2009;23:1825–9. doi: 10.1089/end.2009.0256. [DOI] [PubMed] [Google Scholar]
- 14.Soria F, Delgado MI, Sánchez FM, Allona A, Jiménez Cruz JF, Morell E, et al. Effectiveness of three-dimensional fluoroscopy in percutaneous nephrostomy: An animal model study. Urology. 2009;73:649–52. doi: 10.1016/j.urology.2008.09.063. [DOI] [PubMed] [Google Scholar]
- 15.Lojanapiwat B, Prasopsuk S. Upper-pole access for percutaneous nephrolithotomy: Comparison of supracostal and infracostal approaches. J Endourol. 2006;20:491–4. doi: 10.1089/end.2006.20.491. [DOI] [PubMed] [Google Scholar]
- 16.Duty B, Waingankar N, Okhunov Z, Ben Levi E, Smith A, Okeke Z. Anatomical variation between the prone, supine, and supine oblique positions on computed tomography: Implications for percutaneous nephrolithotomy access. Urology. 2012;79:67–71. doi: 10.1016/j.urology.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Egilmez H, Oztoprak I, Atalar M, Cetin A, Gumus C, Gultekin Y, et al. The place of computed tomography as a guidance modality in percutaneous nephrostomy: Analysis of a 10-year single-center experience. Acta Radiol. 2007;48:806–13. doi: 10.1080/02841850701416528. [DOI] [PubMed] [Google Scholar]
- 18.Chalasani V, Bissoon D, Bhuvanagir AK, Mizzi A, Dunn IB. Should PCNL patients have a CT in the prone position preoperatively? Can J Urol. 2010;17:5082–6. [PubMed] [Google Scholar]
- 19.Kariniemi J, Sequeiros RB, Ojala R, Tervonen O. MRI-guided percutaneous nephrostomy: A feasibility study. Eur Radiol. 2009;19:1296–301. doi: 10.1007/s00330-008-1235-z. [DOI] [PubMed] [Google Scholar]
- 20.Spirnak JP, Resnick MI. Retrograde percutaneous stone removal using modified Lawson technique. Urology. 1987;30:551–3. doi: 10.1016/0090-4295(87)90434-1. [DOI] [PubMed] [Google Scholar]
- 21.Grasso M, Lang G, Taylor FC. Flexible ureteroscopically assisted percutaneous renal access. Tech Urol. 1995;1:39–43. [PubMed] [Google Scholar]
- 22.Bader MJ, Gratzke C, Seitz M, Sharma R, Stief CG, Desai M. The “all-seeing needle”: Initial results of an optical puncture system confirming access in percutaneous nephrolithotomy. Eur Urol. 2011;59:1054–9. doi: 10.1016/j.eururo.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 23.Kawahara T, Ito H, Terao H, Yoshida M, Ogawa T, Uemura H, et al. Ureteroscopy assisted retrograde nephrostomy: A new technique for percutaneous nephrolithotomy (PCNL) BJU Int. 2012;110:588–90. doi: 10.1111/j.1464-410X.2011.10795.x. [DOI] [PubMed] [Google Scholar]
- 24.Honey RJ, Wiesenthal JD, Ghiculete D, Pace S, Ray AA, Pace KT. Comparison of supracostal versus infracostal percutaneous nephrolithotomy using the novel prone-flexed patients position. J Endourol. 2011;25:947–54. doi: 10.1089/end.2010.0705. [DOI] [PubMed] [Google Scholar]
- 25.Moraitis K, Philippou P, El-Husseiny T, Wazait H, Masood J, Buchholz N. Simultaneous antegrade/retrograde upper urinary tract access: Bart's modified lateral position for complex upper tract endourologic pathologic features. Urology. 2012;79:287–92. doi: 10.1016/j.urology.2011.08.023. [DOI] [PubMed] [Google Scholar]
- 26.Lezrek M, Ammani A, Bazine K, Assebane M, Kasmaoui H, Qarro A, et al. The split-leg modified lateral position for percutaneous renal surgery and optimal retrograde access to the upper urinary tract. Urology. 2011;78:217–20. doi: 10.1016/j.urology.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 27.Hoznek A, Ouzaid I, Gettman M, Rode J, De La Taille A, Salomon L, et al. Fluorosopy-guided renal access in supine percutaneous nephrolithotomy. Urology. 2011;78:221–4. doi: 10.1016/j.urology.2011.02.058. [DOI] [PubMed] [Google Scholar]
- 28.Falahatkar S, Neiroomand H, Enshaei A, Kazemzadeh M, Allahkhah A, Jalili MF. Totally ultrasound versus fluoroscopically guided complete supine percutaneous nephrolithotripsy: A first report. J Endourol. 2010;24:1421–6. doi: 10.1089/end.2009.0407. [DOI] [PubMed] [Google Scholar]
- 29.Zhou X, Gao X, Wen J, Xiao C. Clinical value of minimally invasive percutaneous nephrolithotomy in the supine position under the guidance of real-time ultrasound: Report of 92 cases. Urol Res. 2008;36:111–4. doi: 10.1007/s00240-008-0134-8. [DOI] [PubMed] [Google Scholar]
- 30.Basiri A, Ziaee AM, Kianian HR, Mehrabi S, Karami H, Moghaddam SM. Ultrasonographic versus fluoroscopic access for percutaneous nephrolithotomy: A randomized clinical trial. J Endourol. 2008;22:281–4. doi: 10.1089/end.2007.0141. [DOI] [PubMed] [Google Scholar]
- 31.Basiri A, Mohammadi Sichani M, Hosseini SR, Moradi Vadjargah A, Shakhssalim N, Kashi AH, et al. X-ray-free percutaneous nephrolithotomy in supine position with ultrasound guidance. World J Urol. 2010;28:239–44. doi: 10.1007/s00345-009-0451-8. [DOI] [PubMed] [Google Scholar]
- 32.Andonian S, Scoffone CM, Louie MK, Gross AJ, Grabe M, Daels FP, et al. Does Imaging Modality Used for Percutaneous Renal Access Make a Difference. A Matched Case Analysis? J Endourol. 2013;27:24–8. doi: 10.1089/end.2012.0347. [DOI] [PubMed] [Google Scholar]
- 33.Agarwal M, Agrawal MS, Jaiswal A, Kumar D, Yadav H, Lavania P. Safety and efficacy of ultrasonography as an adjunct to fluoroscopy for renal access in percutaneous nephrolithotomy (PCNL) BJU Int. 2011;108:1346–9. doi: 10.1111/j.1464-410X.2010.10002.x. [DOI] [PubMed] [Google Scholar]
- 34.Karami H, Rezaei A, Mohammadhosseini M, Javanmard B, Mazloomfard M, Lotfi B. Ultrasonography-guided percutaneous nephrolithotomy in the flank position versus fluoroscopy-guided percutaneous nephrolithotomy in the prone position: A comparative study. J Endourol. 2010;24:1357–61. doi: 10.1089/end.2009.0099. [DOI] [PubMed] [Google Scholar]


