Abstract
Lasers have come a long way in the management of benign prostatic hyperplasia. Over last nearly two decades, various different lasers have been utilized for prostatectomy. Neodymium: yttrium-aluminum-garnet laser that started this journey, is no longer used for prostatectomy. Holmium laser can achieve transurethral enucleation of the prostatic adenoma producing a fossa that can be compared with the fossa after Freyer's prostatectomy. Green light laser has a short learning curve, is nearly blood-less with good immediate results. Thulium laser is a faster cutting laser while diode laser is a portable laser device. Often laser prostatectomy is considered as a replacement for the standard transurethral resection of prostate (TURP). To be comparable, laser should reduce or avoid the immediate and long-term complications of TURP, especially bleeding and need for blood transfusion. It should also be safe in the ever increasing patient population on antiplatelet and anticoagulant drugs. We need to take stock of the situation and identify, which among the present day lasers has stood the test of time. A review of the literature was performed to see if any of these lasers could be called the “best laser for prostatectomy in 2013.”
Keywords: Benign prostatic hyperplasia, holmium laser enucleation of prostate, laser, photoselective vaporization of the prostate, prostate, thulium
INTRODUCTION
Laser for the treatment of benign prostatic hyperplasia (BPH) has always raised the interest and curiosity of urologists as well as patients. The name “laser” implies modernity and success in the patient's mind. The journey that started with the coagulative necrosis of prostatic adenoma caused by neodymium: yttrium-aluminum-garnet (Nd: YAG) laser has reached a stage where endoscopic “enucleation” could be performed by holmium laser. A number of lasers such as holmium, thulium, green light and diode lasers claim to be the new “gold standard” against the existing standard transurethral resection of prostate (TURP). Irrespective of the gold standard tag, the rapid technological advances have assured that lasers will play an increasing role in the management of BPH.
In this article, we review the literature to define the present status of various lasers and get a clearer view of the indications for this type of treatment and indeed, of its limitations. We also assess how they compare with TURP and to other lasers in various randomized control trials. Wherever possible, randomized controlled trials (RCT) were included in the study, if good RCT were not available then case studies and reports were considered.
TURP: The gold standard
TURP has been the standard mode of treatment of BPH for over eight decades now. The results of TURP have been acceptably good and hence it is considered a gold standard in management of BPH. Why are we then looking for alternatives to TURP? The reason is that over years we have realized shortcomings of this “gold standard” management.
One of the most important concerns for TURP has been intra-operative bleeding and the need for blood transfusion.[1] This risk is higher in patients on anticoagulants and anti-platelet agents. TURP is a difficult procedure to master and has a significant learning curve. The procedure is more difficult in patients with a large prostatic adenoma. Large glands more than 80 g may need two stages of resection. Intravasation of hypotonic fluid and risk of TUR syndrome is high in large prostates. Another energy source like an intracorporeal lithotripsy devise or a urethrotome is needed for associated problems like vesical calculi or urethral stricture. The question we need to answer is; can the present day lasers overcome these shortcomings?
Lasers for prostatectomy
Over the last two decades, many different lasers have been used to treat the enlarged prostate. They can be broadly classified in ablating lasers and cutting lasers. Nd: YAG Laser and potassium-titanyl-phosphate (KTP) Laser are the ablating lasers while holmium: yttrium-aluminum-garnet (Ho: YAG) laser, thulium laser and diode laser are the cutting lasers.
Choosing the “best laser”
To choose the “best laser”, a review of the literature was performed (Medline-PubMed) using the search terms prostatectomy, transurethral, TURP, learning curve, complications, holmium, thulium, diode laser, Nd: YAG laser, KTP laser, photoselective vaporization of the prostate (PVP) laser, solid state laser, results and cost effectiveness. Lasers for prostatectomy were analyzed to assess the immediate and long-term results. These results were compared with TURP in RCTs. The role of lasers was also studied in difficult situations such as large prostatic adenoma, patients with bleeding tendencies and patients, who had associated vesical calculi and stricture urethra. We also tried to look at the studies that compared different laser. Finally, effect of laser prostatectomy on sexual function and their cost effectiveness was examined.
Prostatectomy with Nd: YAG laser
Nd: YAG laser is a continuous wave laser with a wavelength of 1064 nm. Its active medium consists of neodymium atoms in an yttrium-aluminum-garnet rod. This laser energy is poorly absorbed by water and body pigments and has significant depth of penetration. The laser causes thermal coagulation of the surface tissue and of areas just under the surface. Subsequently, the coagulated tissue sloughs over the next few weeks. It may take up to 3 months to achieve complete healing.
Nd: YAG laser was applied to prostatic treatment through procedures like visual laser ablation of prostate (V-LAP) or by transurethral ultrasound-guided laser-induced prostatectomy (TULIP) device. The initial reports by Costello, Kabalin and Norris,[2,3,4,5] which appeared in early 90's had shown good promise. V-LAP was an easy procedure[6] that could be performed rapidly. The procedure was blood less and needed a very short hospital stay.[7] The unpredictable result of V-LAP was a huge problem. There was a long period of irritative symptoms post-operatively. Some patients needed prolonged catheterization.[8] There was a higher incidence of post-operative infections. The post-operative complications of V-LAP far outweighed the advantage of the ease of procedure. Nd: YAG laser has been totally given-up for prostatectomy in present practice.
Holmium laser
The Ho: YAG laser was introduced for use in a number of urologic conditions. Initially, it was used as an adjunct to Nd: YAG laser in the treatment of BPH.[9] The Ho: YAG laser emits light at a frequency of 2100 nm. The energy is emitted in a series of rapid pulses over a few milliseconds. A flexible optical quartz fiber is required for the laser delivery. Holmium laser produces a cutting effect by vaporization of the tissue water; its hemostatic properties are less than those of the continuous wave lasers. For prostatectomy, ideally 100 W holmium laser energy is needed at 2 Joules with 50 Hz frequency. Prostatectomy is possible at lower power settings[10] of 60-80 W; however the lower power setting would increase the operative time.
Clinical results
Over last nearly two decades, multiple studies have documented the results of holmium laser enucleation of prostate (HoLEP). One of the first reports by Gilling et al.[11] in 1996 demonstrated very good results in 84 patients with a mean prostate volume was 50 mL followed over 4.3 months. The side-effects were minimal, with irritative symptoms and dysuria being negligible. The mean symptom score improved from 21.3 to 4.1 and the peak flow rates (PFR) increased from 7.5 mL/s to 19.3 mL/s.
These good results were substantiated in many prospective studies in multiple centers. Krambeck et al.[12] have recently published their experience of more than 1000 HoLEP procedures performed over 10 years from 1998 to 2009. Mean transrectal ultrasound (TRUS) prostate volume was 99.3 gm. Bladder stones were present in 50 patients while 12.1% had renal insufficiency. Significant improvement was documented over short-term, intermediate term and long-term follow-up with the mean symptom score was 8.7, 5.9 and 5.3 and peak urinary flow (PFR) was 17.9, 19.5 and 22.7 mL/s, respectively. They concluded that HoLEP is safe and effective for management of BPH. The complication rate is low and incontinence and the need for ancillary procedures is rare with durable long-term results.
Comparison to TURP
One of the first comparative trials was performed by Gilling et al.[13] in 1999. Patients were randomly assigned to TURP (59 patients) or HoL resection (61 patients) and were observed over 1 year. Both groups showed a significant improvement in symptoms scores and PFR. Complications were low and were equal in both groups. Prolonged catheterization was not required in either group.
The same group recently reported a 7 year follow-up of comparison of HoLEP and TURP.[14] Thirty-one of the initial 61 patients were available for follow-up at 7.6 years. There were no significant differences in any variable between the two groups. Of the assessable patients, none required re-operation for recurrent BPH in the HoLEP arm and three (of 17) required re-operation in the TURP arm. They concluded HoLEP is at least equivalent to TURP in the long-term with fewer re-operations being necessary.
A meta-analysis comparing HoLEP to TURP demonstrated similar improvement in both procedures.[15] There was no statistically significant difference between HoLEP and TURP in terms of Qmax at 6 and 12 months’ follow-up. HoLEP, however, showed several advantages over TURP like significantly less blood loss, a shorter catheterization time and a shorter hospital stay. TURP was associated with reduced operating time. The techniques were similar in terms of post-procedure urethral stricture, stress incontinence, transfusion requirement and rate of reintervention. HoLEP was found to be at least as safe as TURP in terms of adverse events.
One more recent study from Hamburg, Germany[16] compared HoLEP, TURP and simple prostatectomy for the resection speeds of the three procedures. Resection speed seems to be an objective criterion for comparing the efficacy of prostatic tissue removal. Resection speed and operative time for laser enucleation were statistically significantly faster than for TURP (0.61 vs. 0.51 gm/min and 62 vs. 73 min, P > 0.01) and similar to those of simple open prostatectomy (OP) (0.92 vs. 1.0 gm/min and 101 vs. 90 min, respectively, P ≥ 0.21). Based on resection speed, holmium laser enucleation of the prostate is faster than transurethral resection of the prostate and similar to simple OP.
HoLEP for large prostates
HoLEP has been used successfully for both small and large prostatic adenomas. The definition of a large prostate varies in different trials. Kuo et al.[17] assessed 108 patients with HoLEP for prostates weighing more than 75 g. They demonstrated that HoLEP can be performed on extremely large prostates with minimal risk or need for secondary interventions. Most patients were discharged home after an overnight stay. Postoperative decreases in prostate-specific antigen (PSA) and TRUS volumes supported the completeness of enucleation that could be achieved.
Kuntz et al.[18] reported 5-year follow-up results of a randomized clinical trial comparing HoLEP with open prostatectomy (OP) in 120 patients. They concluded that at 5 years post-surgery, the improvements in micturation obtained with HoLEP and OP were equally good. Mean American Urological Association (AUA)-SS was 3.0 in both groups (P = 0.98), mean Qmax was 24.4 mL/s in both groups (P = 0.97) and post-void residual urine volume was 11 mL in the HoLEP and 5 mL in the OP group (P = 0.25). Late complications consisted of urethral strictures and bladder-neck contractures; reoperation rates were 5% in the HoLEP and 6.7% in the OP group. As the reoperation rates were similarly low with as good the results, HoLEP seemed to be a true endourological alternative to OP.
A recent study assessed 57 patients who underwent HoLEP for prostates more than 175 g (range 175-391 cc).[19] Pre-operative mean PSA level was 14.6 ng/mL, mean IPSS score was 19.0 and mean PFR was 8.2 mL/s. Mean hospital stay was 26 h and post-operative catheterization was 18.5 h (range 6-96 h). All patients were able to void after catheter removal. Mean enucleated tissue weight was 176.4 g (range 48-532.2 g). At 6-month follow-up, IPSS score was 6.5, mean PSA level was 0.78 ng/mL and PFR was 18.5. During the follow-up period, no patient needed catheterization or had persistent incontinence. Even in this sub-group of very large prostate glands, HoLEP provided a satisfactory outcome with low morbidity. Krambeck et al. proposed HoLEP as the only endoscopic technique that allowed for tissue removal comparable with that of OP for such patients.
HoLEP in patients with bleeding tendency
Elzayat et al. from McGill University School of Medicine, Montreal, reported a total of 83 patients who underwent HoLEP and were on chronic oral anticoagulant therapy[20] or had bleeding disorders. The procedure could be performed without increased risk of major operative or post-operative complications or thromboembolic events. The study concluded that HoLEP was safe and effective therapeutic modality in patients on anticoagulation with symptomatic BPH refractory to medical therapy.
HoLEP: Learning curve
Steep learning curve has been a major issue of debate for HoLEP. This is often considered a reason for the slow adoption of this technique by urologists. Shah et al.[21] studied this issue and showed that HoLEP could be learnt by an experienced endourologist in about 50 cases. They divided their initial 162 patients in three groups and compared the results in these groups. Holmium laser prostate enucleation was successfully completed in 93.82% of patients. Eight patients required conversion to TURP. Enucleation and morcellation efficiency was 0.49 g/min and 2.75 g/min, respectively. Enucleation efficiency attained a plateau after 50 cases. Post-operative outcome was comparable in the 3 patient groups. There was a higher incidence of capsular perforation and stenotic urethral complications in the initial group.
Furthermore Elzayat and Elhilali[22] showed that the results of HoLEP even in the initial learning curve are good and acceptable. The mean PFR increased from 6.3 mL/s to 16.2 mL/s and mean PVR decreased from 232 mL to 41.2 mL (P > 0.0001). Mean IPSS improved from 17.3 to 5.6 (P > 0.0001). Bladder-neck contracture and urethral stricture developed in 0.8% and 1.7% of patients, respectively.
Photoselective KTP laser
PVP is performed using a high power 80-W or 120-W KTP laser (Greenlight PV Laser System). The KTP laser uses a KTP crystal to double the frequency of an Nd: YAG laser and produces a 532-nm wavelength. This provides an intermediate level of coagulation and vaporization. The depth of tissue penetration is only half the depth that of the Nd: YAG laser. However, the consequent higher energy per unit tissue volume produced may increase tissue vaporization and desiccation. KTP laser energy is delivered by a side-firing fiber.
PVP: Results
There is ample literature supporting good results with PVP laser prostatectomy both in immediate and long-term follow-up. Araki et al.[23] reported a 1 year follow up of 160 patients. The mean prostate volume was 72.3 cm3 and the mean PSA level of 2.2 ng/mL. Mean laser time and energy usage were 33.4 min and 99.0 kJ respectively. All were out-patient procedures with 60% patients catheter-free at discharge. Catheter for 1 week was needed in 17.5% patients.
Fu et al.[24] reported 42 patients where KTP prostatectomy was performed for patients who presented with retention of urine. All patients voided post-operatively with mean catheter duration was 5.6 days. There was a significant subjective improvement of symptoms and objective improvement in urinary flow rates at 12 months. Two patients had recurrent urinary retention during the follow-up. There were no intraoperative or post-operative adverse events.
Sulser et al.[25] described their experience with PVP in 65 patients. The mean operating time was 57 min. All patients were catheter free within 1 month with good short-term results.
PVP for patients with bleeding tendency
One of the major advantages of KTP laser is the blood less nature of this technology.[26] PVP laser vaporization was performed successfully in 66 patients with high cardiopulmonary risk, having presented with an American Society of Anesthesiology score of 3 or greater.[27] In addition, 29 patients were being treated with ongoing oral anticoagulant therapy or had a severe bleeding disorder. No major complication occurred intra-operatively or postoperatively and no blood transfusion was required. Post-operatively, 77% patients did not require irrigation. Average catheterization time was 1.8 ± 1.4 days. Two patients required reoperation due to recurrent urinary retention. Many other authors[28,29] have proposed PVP as a treatment option in men who are at high risk for clinically significant bleeding.
PVP for large prostate
Rajbabu et al.[30] from London have reported PVP for prostates more than 100 g size. Their report has been encouraging in the short and medium term. The good results could be achieved with a procedure time of 81.6 min (39-150), the mean energy used was 278 kJ (176-443) and the mean duration of catheterization was 23 h (0-72). The IPSS and QoL scores showed improvements and there was a statistically significant reduction in PSA level and prostate volume after PVP. There was no major complication and no patient had transurethral resection syndrome or needed a blood transfusion. The authors have presented PVP as a potential viable alternative to OP. Similar good results are reported in a study by Tugcu et al. from Turkey[31] where green light laser was used for 100 patients with prostate more than 70 g. The procedure is found to be virtually bloodless, safe and effective for surgical treatment of large volume prostates.
PVP: Other aspects
The aspect of learning curve of PVP has not been studied in the literature. The reason probably is that PVP is an easy procedure to master.
One often quoted drawback of PVP is that no tissue is available for histopathology after prostatectomy. In today's time, when pre-operative cancer detection by PSA and transrectal ultrasonography is easy, this may not be of much significance. To answer this question, the Mayo Clinic group[32] analyzed the incidental cancer prostates (PCa) diagnosed during 240 cases of HoLEP who had a normal PSA level pre-operatively. The database consisted of 240 consecutive patients, aged 52-90 years with prostate sizes from 25 cm3 to 375 cm3. A total of 28 patients were identified with incidental PCa (14 cT1a and 14 cT1b). The incidental PCa detection rate was 11.7%. Of these, 3 patients (10.7%) with cT1b required additional treatment as a result of PSA progression. Even this, low rate might be significant as these patients would otherwise go untreated. The impact on disease-specific survival and progression requires a longer follow-up. The incidental PCa detection rate of 11.7% shows the potential benefit of pathological analysis.
PVP is a prostate specific laser that cannot be used for other urologic indications such as stones and strictures.
Thulium laser
Thulium laser is a continuous wave laser (in contrast to pulsed holmium laser) that has a wave-length similar to holmium laser. The continuous wave pattern helps producing clean and faster cuts during the prostatectomy. Thulium laser has good hemostatic properties. Many techniques for thulium laser prostatectomy have been described like ablation, resection and enucleation.
Bach et al.[33] from Hamburg, Germany analyzed the initial results of 88 patients where thulium laser vapo-enucleation (ThuLEP) was performed. Prostatic volume was 61.3 ± 24.0 cc, OR-time was 72 min ± 26.6 and laser-time was 32.4 ± 10.1 min. Total laser energy used was 123.7 ± 40.6 k. Foley catheter-time was 2.1 ± 1.06 days on average. The voiding parameters improved significantly with a smooth post-operative period. Early complications were minimal with 27% of patients experiencing short-term dysuria. Overall satisfactory results were documented and ThuLEP was found to be safe and effective modality for management of BPH. The same group compared ThuLEP by 70 W and 120 W[34] and found that 120 W enhances the effectiveness of ThuLEP with regard to the percentage of resected tissue and the enucleation/operation efficiency. When comparing 120 W and 200 W units in 28 patients with 60-70 g prostate, they found equivalent safe and efficacious clinical outcomes with both units at 12-month follow-up.[35] There were no differences in mean operative (69.21 vs. 78.67 min), laser (45.43 vs. 48.58 min), morcellation (16.52 vs. 20.48 min) and catheter (2.2 vs. 2.1 d) time between the devices.
Large prostates more than 80 g can be safely treated with a manageable risk of complications by ThuLEP.[36] Minor risk of urinary infection, stress urinary incontinence and dysuria are the only noticeable problems.
Zhang et al.[37] compared ThuLEP with HoLEP in 131 patients. ThuLEP required a longer operation time (72.4 vs. 61.5 min, P = 0.034) but resulted in less blood loss than HoLEP (130.0 vs. 166.6 mL, P = 0.045). The catheterization time was comparable. At 18 months, the lower urinary tract symptom indexes were improved significantly in both groups compared with the baseline values.
The learning curve of Thulium laser enucleation has not been adequately reported in the literature. A recent study by Netsch et al.[38] demonstrated that with proper mentoring, vapo-enucleation can be performed with reasonable efficiency even in the early learning curve. A resident without experience in transurethral prostate surgery could perform this procedure efficiently in 8-16 cases.
The same group has studied the safety of Thulium laser in 56 patients with high cardiopulmonary risk of which 32 were on oral anti-coagulants.[39] Vapo-enucleation could be safely performed in this high risk group; although, 4 patients needed second look procedure and transfusions for significant bleeding. Thulium laser has also been used for indications such as stricture urethra and tumors of bladder and prostate. It has hemostatic roles in open surgery, gynecology and gastroenterology. It also may have a potential role in laparoscopy, bronchoscopy and general surgery.
Diode laser
Diode laser system has a wavelength of 980 nm. It offers a high simultaneous absorption in water and hemoglobin and is postulated to combine high tissue ablative properties with good hemostasis. The high gain of the diode laser allows the more efficient use of the photons that are generated; hence, the available diode laser units are small and portable and special connections are not required.
An initial study of ten patients who underwent diode laser vaporization of the prostate showed encouraging results at 1 year follow-up.[40]A Spanish study[41] reported enucleation of prostate by diode laser in 17 patients. The mean prostate volume was 61.26 cc. The improvement in the IPSS (22.3 ± 4.1 vs. 7.1 ± 1.06) and in the Qmax (7.14 ± 2.6 vs. 21.4 ± 3.6) was sustainable. The mean loss of hemoglobin was 2.1 g/dl. There were no major consequences or complications. Patients needed a short catheter placement and had good immediate post-operative improvement.
Erectile dysfunction after various laser treatments
Erectile and ejaculatory dysfunction is a common problem and shows the expected increasing trends with ageing. Erectile function reduces after TURP in nearly quarter of the patients.[42] Ejaculatory dysfunction in form of retrograde ejaculation is more common.
HoLEP, PVP and ThuLEP did not appear to affect the erectile function although the ejaculatory loss was as frequent as in TURP.[43,44,45,46,47] Briganti et al.[43] compared erectile dysfunction in HoLEP and TURP in 120 patients. A total of 32 patients (53.3%) in HoLEP and 31 (51.6%) in TURP group reported various degrees of erectile dysfunction before surgery according to the Erectile function domain of International index of erectile function IIEF-EF. Differences between preoperative and postoperative orgasmic domain scores in each group were significant (P > 0.001). A slight but not significant increase in the mean IIEF-EF domain score was reported in each group at postoperative assessments without any difference between the 2 surgical approaches. According to general assessment question analysis the prevalence of subjectively reported postoperative retrograde ejaculation was significantly higher than at baseline assessment in the 2 groups with no differences between the 2 surgical procedures.
A systematic review of RCT[42] showed that laser surgeries for BPH have comparable effects to those of TURP on the erectile function. Collectively, less than 15.4% or 15.2% of patients will have either decrease or increase, respectively, of erectile function after laser procedures, although both are not statistically significant.
Cost-effectiveness of various lasers
Cost-effectiveness has always been an important consideration for choosing the treatment modality. The total cost to the patient would be calculated by the establishment cost and per-patient disposable cost. The saving on reduced hospitalization, nursing care, complications and treatment of complications and also on the reduced work hour loss would favorably impact the calculations. The implications of these factors would also vary at various geographical places.
One of the initial studies performed by Fraundorfer et al.[48] found HoLEP to be more cost effective than TURP over 1 year follow-up. They calculated that a minimum of 93 cases per year are required to recover the capital and service costs of the holmium laser. A similar study carried out at Turkey concluded that laser prostatectomy is more costly than TURP.[49] For large prostate glands, HoLEP when compared with OP led to a significant net saving to the hospital.[50]
A study from Cleveland clinic comparing cost-effectiveness of PVP and TURP concluded that the estimated cost was lower for PVP than for any other procedural option studied.[51] Study from Newcastle[52] had a totally opposing view where the authors concluded that HoLEP is cost-effective in their practice while PVP was unlikely to be cost-effective. They argued against unrestricted use of PVP until further evidence of effectiveness and cost reduction was obtained.
In our circumstances, laser prostatectomy is more costly when compared with TURP. All three lasers have a nearly similar initial investment but PVP has the highest disposables cost.
Laser: Which to choose?
Nd: YAG laser is outdated in today's time.
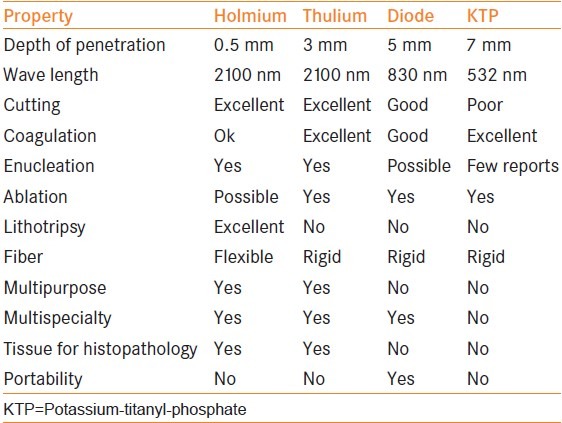
The physics of the four lasers, holmium, thulium, diode and KTP are compared in Table 1. Interestingly there are no good quality long term follow-up randomized controlled studies in recent literature comparing various lasers for prostatectomy.
Table 1.
Comparison of lasers
The good and sustained results of holmium laser enucleation for prostatectomy are very well studied in multiple RCT's. HoLEP is the only laser treatment for BPH with level 1 evidence and endorsement in both the AUA and European Association of Urology guidelines. van Rij and Gilling,[53] in a recent review article has proposed HoLEP to be the “New Gold-Standard” in 2013.
The limitations of holmium laser may be a longer learning curve and a comparatively sub-optimal hemostasis. The distinct advantages are it is multi-utility and multispecialty use. It is an excellent intra-corporeal lithotripsy device and the disposables cost is least among the three lasers.
PVP is a prostate specific laser with documented good results and brilliant hemostasis. Lack of tissue for histopathology is a theoretical disadvantage. Initial installation cost and disposables cost is the highest. Additional low power holmium laser would be needed for intra-corporeal lithotripsy. The distinct advantages are nearly bloodless procedure, need for a small size urethral catheter for a short duration and ease of the procedure.
Thulium laser has very good cutting and coagulating properties. The procedure is easier and faster than HoLEP. The installation and disposable cost is higher than holmium laser, but less than PVP. Additional low power holmium laser would be needed for intra-corporeal lithotripsy.
CONCLUSION
The use of the laser to treat symptomatic BPH has evolved from the relatively cumbersome TULIP technique to other methods that require smaller pieces of equipment. Newer lasers such as Holmium, PVP and Thulium have achieved post-operative results and quality-of-life improvement as good as TURP. The difficulties in treating large prostates have been overcome. The complications and problems such as prolonged catheterization, infections and urethral strictures, have been lowered considerably. The ever increasing population of patients on oral anticoagulants can be treated safely by these lasers. Cost-effectiveness still remains a question in urologists’ minds.
The question about the “best laser” still remains un-answered. Long-term data from multicenter groups would be needed to give this answer.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Fitzpatrick JM. Minimally invasive and endoscopic management of benign prostatic hyperplasia. In: Wein AJ, Kavoussi LR, Partin AW, Novick AC, Peters CA, editors. Campbell Walsh Urology. 10th ed. Philadelphia: Elsevier Saunders; 2012. pp. 2655–94. [Google Scholar]
- 2.Costello AJ. Laser prostatectomy. Med J Aust. 1992;157:504. doi: 10.5694/j.1326-5377.1992.tb137337.x. [DOI] [PubMed] [Google Scholar]
- 3.Kabalin JN. Laser prostatectomy performed with a right angle firing neodymium: YAG laser fiber at 40 watts power setting. J Urol. 1993;150:95–9. doi: 10.1016/s0022-5347(17)35407-1. [DOI] [PubMed] [Google Scholar]
- 4.Norris JP, Norris DM, Lee RD, Rubenstein MA. Visual laser ablation of the prostate: Clinical experience in 108 patients. J Urol. 1993;150:1612–4. doi: 10.1016/s0022-5347(17)35857-3. [DOI] [PubMed] [Google Scholar]
- 5.Kabalin JN. Laser prostatectomy - What we have accomplished and future directions. J Urol. 1995;154:2093–5. doi: 10.1016/s0022-5347(01)66703-x. [DOI] [PubMed] [Google Scholar]
- 6.Anson K, Nawrocki J, Buckley J, Fowler C, Kirby R, Lawrence W, et al. A multicenter, randomized, prospective study of endoscopic laser ablation versus transurethral resection of the prostate. Urology. 1995;46:305–10. doi: 10.1016/S0090-4295(99)80211-8. [DOI] [PubMed] [Google Scholar]
- 7.Cowles RS, 3rd, Kabalin JN, Childs S, Lepor H, Dixon C, Stein B, et al. A prospective randomized comparison of transurethral resection to visual laser ablation of the prostate for the treatment of benign prostatic hyperplasia. Urology. 1995;46:155–60. doi: 10.1016/s0090-4295(99)80185-x. [DOI] [PubMed] [Google Scholar]
- 8.Keoghane SR, Lawrence KC, Gray AM, Doll HA, Hancock AM, Turner K, et al. A double-blind randomized controlled trial and economic evaluation of transurethral resection vs contact laser vaporization for benign prostatic enlargement: A 3-year follow-up. BJU Int. 2000;85:74–8. doi: 10.1046/j.1464-410x.2000.00407.x. [DOI] [PubMed] [Google Scholar]
- 9.Gilling PJ, Cass CB, Malcolm AR, Fraundorfer MR. Combination holmium and Nd: YAG laser ablation of the prostate: Initial clinical experience. J Endourol. 1995;9:151–3. doi: 10.1089/end.1995.9.151. [DOI] [PubMed] [Google Scholar]
- 10.Kelly DC, Das A. Holmium laser enucleation of the prostate technique for benign prostatic hyperplasia. Can J Urol. 2012;19:6131–4. [PubMed] [Google Scholar]
- 11.Gilling PJ, Cass CB, Cresswell MD, Fraundorfer MR. Holmium laser resection of the prostate: Preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology. 1996;47:48–51. doi: 10.1016/s0090-4295(99)80381-1. [DOI] [PubMed] [Google Scholar]
- 12.Krambeck AE, Handa SE, Lingeman JE. Experience with more than 1,000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urol. 2010;183:1105–9. doi: 10.1016/j.juro.2009.11.034. [DOI] [PubMed] [Google Scholar]
- 13.Gilling PJ, Mackey M, Cresswell M, Kennett K, Kabalin JN, Fraundorfer MR. Holmium laser versus transurethral resection of the prostate: A randomized prospective trial with 1-year followup. J Urol. 1999;162:1640–4. [PubMed] [Google Scholar]
- 14.Gilling PJ, Wilson LC, King CJ, Westenberg AM, Frampton CM, Fraundorfer MR. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: Results at 7 years. BJU Int. 2012;109:408–11. doi: 10.1111/j.1464-410X.2011.10359.x. [DOI] [PubMed] [Google Scholar]
- 15.Tan A, Liao C, Mo Z, Cao Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg. 2007;94:1201–8. doi: 10.1002/bjs.5916. [DOI] [PubMed] [Google Scholar]
- 16.Ahyai SA, Chun FK, Lehrich K, Dahlem R, Zacharias MS, Fisch MM, et al. Transurethral holmium laser enucleation versus transurethral resection of the prostate and simple open prostatectomy - Which procedure is faster? J Urol. 2012;187:1608–13. doi: 10.1016/j.juro.2011.12.107. [DOI] [PubMed] [Google Scholar]
- 17.Kuo RL, Kim SC, Lingeman JE, Paterson RF, Watkins SL, Simmons GR, et al. Holmium laser enucleation of prostate (HoLEP): The Methodist Hospital experience with greater than 75 gram enucleations. J Urol. 2003;170:149–52. doi: 10.1097/01.ju.0000070686.56806.a1. [DOI] [PubMed] [Google Scholar]
- 18.Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008;53:160–6. doi: 10.1016/j.eururo.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 19.Krambeck AE, Handa SE, Lingeman JE. Holmium laser enucleation of the prostate for prostates larger than 175 grams. J Endourol. 2010;24:433–7. doi: 10.1089/end.2009.0147. [DOI] [PubMed] [Google Scholar]
- 20.Elzayat E, Habib E, Elhilali M. Holmium laser enucleation of the prostate in patients on anticoagulant therapy or with bleeding disorders. J Urol. 2006;175:1428–32. doi: 10.1016/S0022-5347(05)00645-2. [DOI] [PubMed] [Google Scholar]
- 21.Shah HN, Mahajan AP, Sodha HS, Hegde S, Mohile PD, Bansal MB. Prospective evaluation of the learning curve for holmium laser enucleation of the prostate. J Urol. 2007;177:1468–74. doi: 10.1016/j.juro.2006.11.091. [DOI] [PubMed] [Google Scholar]
- 22.Elzayat EA, Elhilali MM. Holmium laser enucleation of the prostate (HoLEP): Long-term results, reoperation rate, and possible impact of the learning curve. Eur Urol. 2007;52:1465–71. doi: 10.1016/j.eururo.2007.04.074. [DOI] [PubMed] [Google Scholar]
- 23.Araki M, Lam PN, Wong C. High-power potassium-titanyl-phosphate laser photoselective vaporization prostatectomy for symptomatic benign prostatic hyperplasia. J Endourol. 2008;22:1311–4. doi: 10.1089/end.2008.0140. [DOI] [PubMed] [Google Scholar]
- 24.Fu WJ, Gao JP, Hong BF, Yang Y, Cai W, Zhang L. Photoselective laser vaporization prostatectomy for acute urinary retention in China. J Endourol. 2008;22:539–43. doi: 10.1089/end.2007.0045. [DOI] [PubMed] [Google Scholar]
- 25.Sulser T, Reich O, Wyler S, Ruszat R, Casella R, Hofstetter A, et al. Photoselective KTP laser vaporization of the prostate: First experiences with 65 procedures. J Endourol. 2004;18:976–81. doi: 10.1089/end.2004.18.976. [DOI] [PubMed] [Google Scholar]
- 26.Alivizatos G, Skolarikos A. Greenlight laser in benign prostatic hyperplasia: Turning green into gold. Curr Opin Urol. 2008;18:46–9. doi: 10.1097/MOU.0b013e3282f0d63b. [DOI] [PubMed] [Google Scholar]
- 27.Reich O, Bachmann A, Siebels M, Hofstetter A, Stief CG, Sulser T. High power (80 W) potassium-titanyl-phosphate laser vaporization of the prostate in 66 high risk patients. J Urol. 2005;173:158–60. doi: 10.1097/01.ju.0000146631.14200.d4. [DOI] [PubMed] [Google Scholar]
- 28.Sandhu JS, Ng CK, Gonzalez RR, Kaplan SA, Te AE. Photoselective laser vaporization prostatectomy in men receiving anticoagulants. J Endourol. 2005;19:1196–8. doi: 10.1089/end.2005.19.1196. [DOI] [PubMed] [Google Scholar]
- 29.Yuan J, Wang H, Wu G, Liu H, Zhang Y, Yang L. High-power (80 W) potassium titanyl phosphate laser prostatectomy in 128 high-risk patients. Postgrad Med J. 2008;84:46–9. doi: 10.1136/pgmj.2007.062711. [DOI] [PubMed] [Google Scholar]
- 30.Rajbabu K, Chandrasekara SK, Barber NJ, Walsh K, Muir GH. Photoselective vaporization of the prostate with the potassium-titanyl-phosphate laser in men with prostates of <100 mL. BJU Int. 2007;100:593–8. doi: 10.1111/j.1464-410X.2007.06985.x. [DOI] [PubMed] [Google Scholar]
- 31.Tugcu V, Tasci AI, Sahin S, Ordekci Y, Karakas OF, Zorluoglu F. Outcomes of 80 W KTP laser vaporization of the large prostate. Urol Int. 2007;79:316–20. doi: 10.1159/000109716. [DOI] [PubMed] [Google Scholar]
- 32.Nunez R, Hurd KJ, Noble BN, Castle EP, Andrews PE, Humphreys MR. Incidental prostate cancer revisited: Early outcomes after holmium laser enucleation of the prostate. Int J Urol. 2011;18:543–7. doi: 10.1111/j.1442-2042.2011.02776.x. [DOI] [PubMed] [Google Scholar]
- 33.Bach T, Netsch C, Haecker A, Michel MS, Herrmann TR, Gross AJ. Thulium: YAG laser enucleation (VapoEnucleation) of the prostate: Safety and durability during intermediate-term follow-up. World J Urol. 2010;28:39–43. doi: 10.1007/s00345-009-0461-6. [DOI] [PubMed] [Google Scholar]
- 34.Netsch C, Bach T, Herrmann TR, Gross AJ. Thulium: YAG VapoEnucleation of the prostate in large glands: A prospective comparison using 70-and 120-W 2-μm lasers. Asian J Androl. 2012;14:325–9. doi: 10.1038/aja.2011.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Netsch C, Bach T, Pohlmann L, Herrmann T, Gross AJ. Comparison of 120-200 W 2 μm thulium: Yttrium-aluminum-garnet vapoenucleation of the prostate. J Endourol. 2012;26:224–9. doi: 10.1089/end.2011.0173. [DOI] [PubMed] [Google Scholar]
- 36.Bach T, Netsch C, Pohlmann L, Herrmann TR, Gross AJ. Thulium: YAG vapoenucleation in large volume prostates. J Urol. 2011;186:2323–7. doi: 10.1016/j.juro.2011.07.073. [DOI] [PubMed] [Google Scholar]
- 37.Zhang F, Shao Q, Herrmann TR, Tian Y, Zhang Y. Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology. 2012;79:869–74. doi: 10.1016/j.urology.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 38.Netsch C, Bach T, Herrmann TR, Neubauer O, Gross AJ. Evaluation of the learning curve for Thulium VapoEnucleation of the prostate (ThuVEP) using a mentor-based approach. World J Urol. 2012 doi: 10.1007/s00345-012-0894-1. Epub DOI: 101007/s00345-012-0894-1, accessed August 8, 2013. [DOI] [PubMed] [Google Scholar]
- 39.Netsch C, Stoehrer M, Brüning M, Gabuev A, Bach T, Herrmann TR, et al. Safety and effectiveness of Thulium VapoEnucleation of the prostate (ThuVEP) in patients on anticoagulant therapy. World J Urol. 2013 doi: 10.1007/s00345-013-1093-4. Epub DOI: 101007/s00345-013-1093-4, accessed August 8, 2013. [DOI] [PubMed] [Google Scholar]
- 40.Seitz M, Sroka R, Gratzke C, Schlenker B, Steinbrecher V, Khoder W, et al. The diode laser: A novel side-firing approach for laser vaporisation of the human prostate - Immediate efficacy and 1-year follow-up. Eur Urol. 2007;52:1717–22. doi: 10.1016/j.eururo.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 41.Buisan O, Saladie JM, Ruiz JM, Bernal S, Bayona S, Ibarz L. Diode laser enucleation of the prostate (Dilep): Technique and initial results. Actas Urol Esp. 2011;35:37–41. doi: 10.1016/j.acuro.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 42.Arai Y, Aoki Y, Okubo K, Maeda H, Terada N, Matsuta Y, et al. Impact of interventional therapy for benign prostatic hyperplasia on quality of life and sexual function: A prospective study. J Urol. 2000;164:1206–11. [PubMed] [Google Scholar]
- 43.Briganti A, Naspro R, Gallina A, Salonia A, Vavassori I, Hurle R, et al. Impact on sexual function of holmium laser enucleation versus transurethral resection of the prostate: Results of a prospective, 2-center, randomized trial. J Urol. 2006;175:1817–21. doi: 10.1016/S0022-5347(05)00983-3. [DOI] [PubMed] [Google Scholar]
- 44.Frieben RW, Lin HC, Hinh PP, Berardinelli F, Canfield SE, Wang R. The impact of minimally invasive surgeries for the treatment of symptomatic benign prostatic hyperplasia on male sexual function: A systematic review. Asian J Androl. 2010;12:500–8. doi: 10.1038/aja.2010.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bruyère F, Puichaud A, Pereira H, Faivre d’Arcier B, Rouanet A, Floc’h AP, et al. Influence of photoselective vaporization of the prostate on sexual function: Results of a prospective analysis of 149 patients with long-term follow-up. Eur Urol. 2010;58:207–11. doi: 10.1016/j.eururo.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 46.Kavoussi PK, Hermans MR. Maintenance of erectile function after photoselective vaporization of the prostate for obstructive benign prostatic hyperplasia. J Sex Med. 2008;5:2669–71. doi: 10.1111/j.1743-6109.2008.00978.x. [DOI] [PubMed] [Google Scholar]
- 47.Luo GH, Sun ZL, Xia SJ. Influences of erectile functions in benign prostatic hyperplasia patients by two micro (thulium) laser resection of prostate-tangerine technique. Zhonghua Yi Xue Za Zhi. 2011;91:2243–6. [PubMed] [Google Scholar]
- 48.Fraundorfer MR, Gilling PJ, Kennett KM, Dunton NG. Holmium laser resection of the prostate is more cost effective than transurethral resection of the prostate: Results of a randomized prospective study. Urology. 2001;57:454–8. doi: 10.1016/s0090-4295(00)00987-0. [DOI] [PubMed] [Google Scholar]
- 49.Agirbas I, Tatar M, Kisa A. Benign prostatic hyperplasia: Cost and effectiveness of three alternative surgical treatment methods used in a Turkish hospital. J Med Syst. 2005;29:487–92. doi: 10.1007/s10916-005-6105-5. [DOI] [PubMed] [Google Scholar]
- 50.Salonia A, Suardi N, Naspro R, Mazzoccoli B, Zanni G, Gallina A, et al. Holmium laser enucleation versus open prostatectomy for benign prostatic hyperplasia: An inpatient cost analysis. Urology. 2006;68:302–6. doi: 10.1016/j.urology.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 51.Stovsky MD, Griffiths RI, Duff SB. A clinical outcomes and cost analysis comparing photoselective vaporization of the prostate to alternative minimally invasive therapies and transurethral prostate resection for the treatment of benign prostatic hyperplasia. J Urol. 2006;176:1500–6. doi: 10.1016/j.juro.2006.06.064. [DOI] [PubMed] [Google Scholar]
- 52.Armstrong N, Vale L, Deverill M, Nabi G, McClinton S, N’Dow J, et al. Surgical treatments for men with benign prostatic enlargement: Cost effectiveness study. BMJ. 2009;338:b1288. doi: 10.1136/bmj.b1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van Rij S, Gilling PJ. In 2013, holmium laser enucleation of the prostate (HoLEP) may be the new ‘gold standard’. Curr Urol Rep. 2012;13:427–32. doi: 10.1007/s11934-012-0279-4. [DOI] [PubMed] [Google Scholar]


