Abstract
Background:
Chronic periodontitis in amultifactorial inflammatory disease which is caused by various microorganisms. Many studies have found close association between chronic periodontitis and C-reactive protein (CRP). CRPis an inflammatory marker which increases in all inflammatory condition.
Aims and Objective:
The present clinical study was designed to show the effect of periodontal treatment on the CRP levels of gingival crevicular fluid and to determine the effect of nonsurgical therapy in minimizing the CRP levels in chronic generalized periodontitis.
Material and Method:
Gingival crevicular fluid was collected using a micro capillary pipette that was hand calibrated at every 1 mm till 10 mm, from selected sites in the subjects on the 1st, 14th and 45th days.
Results and Conclusion:
Decreased CRP levels of gingival crevicular fluid were observed at the end of the study. There was a 37% reduction in probing pocket depth and 45% gain in clinical attachment level and a reduction of about 57% after 14 days and 90% reduction of CRP levels in gingival crevicular fluid after 45 days. Thus, the results show that the presence of CRP level is more significant in gingival crevicular fluid and confirms the underlying inflammatory component of the disease activity in chronic periodontitis.
Keywords: C-reactive protein, GCF, periodontitis
INTRODUCTION
Periodontitis is considered as a multifactorial inflammatory disease. Recently, an old concept that states that periodontitis may have an etiological or modulation role in other systemic disease has surfaced. Among all the explanatory mechanisms, one is based around the concept of periodontitis having an effect by the dissemination of mediators such as C-reactive protein (CRP), interleukin-6 (IL) and tumor necrosis factor-α (TNF-α). This type of respond is activated either by the local infection by bacteria resulting in inflammatory damage of periodontal tissue or by the systemic spread of bacteria or their toxins and products during the course of periodontal disease. These bacterial pathogens, bacterial antigens, endotoxins and inflammatory cytokines like CRP, IL-1 and TNF-α contribute and modify the process of atherogenesis and thromboembolic events.[1]
The relation between vascular events and periodontal disease is further supported by evidence showing that oral bacteria can cause platelet aggregation and thromboembolic events by upregulating the expression of platelet aggregation-associated protein. It is also known that CRP induces monocytes/macrophages to produce tissue factors, which stimulate the coagulation pathway and increase blood coagulability. Hence, CRP levels in the gingival crevicular fluid may be a new way to assess cardiovascular disease risk due to periodontitis.
Elevated levels of CRP and decreased plasma adiponectin are associated with increased risk of atherosclerosis. As periodontal disease has been suggested to act as a risk factor for atherosclerosis, Iwamoto and Nishimura (2003) examined the effect of antimicrobial periodontal treatment on CRP, adiponectin and TNF-α levels. Periodontal treatment is effective in reducing CRP and TNF-α, while adiponectin does not appear to be influenced by periodontal treatment. Elevated levels of CRP and TNF-α may be associated with increased risk for further development of a thrombosclerosis in periodontitis patients.[2]
MATERIALS AND METHODS
One hundred and twenty (120) patients diagnosed with chronic generalized periodontitis having pocket depth ≥5 mm with radiographic evidence of bone loss were selected for the study. Inclusion criteria included the patients who were diagnosed with chronic generalized periodontitis having pocket depth ≥5 mm with radiographic evidence of bone loss and in the age group of 35-55 years. Care was also taken to include patients with no systemic disease, those who were nonsmokers and those with acceptable oral hygiene.
Exclusion criteria included those patients who had undergone oral prophylaxis or taken antibiotic 6 months prior to the study. Pregnant, nursing patient and patients with inability to comply with the follow-up visit were excluded from the study.
A written informed consent form explaining the nature of the study and lab investigation procedure was signed by the patient. Gingival crevicular fluid was collected using a micro capillary pipette that was hand calibrated at every 1 mm till 10 mm, from selected sites in the subjects on 0 day (prior to phase I therapy), 14th day and 45th day, and gingival index (Loe H and Sillness J), sulcus bleeding index (Mulheman), clinical probing pocket depth and clinical attachment loss were recorded in a prepared chart. On every recall visit, i.e., 14th day and 45th day, oral hygiene instructions were reinforced and gingival crevicular fluid was collected for estimation of CRP. Clinical parameters like gingival index, bleeding index, clinical probing pocket depth and clinical attachment loss were recorded.
Method of collection of gingival crevicular fluid
Patients selected were seated comfortably in the dental chair with proper illumination. Samples of gingival crevicular fluid were taken from the selected sites by placing calibrated volumetric micro capillary pipettes with 0-5 μL range (Sigma Chemical Company, St. Lowis, MO, USA) using the extracrevicular method.
The gingival crevicular fluid sample was collected only from those teeth that had average pocket probing depth in each subject. Supragingival plaque obstructing access to the entrance of the crevice was carefully removed using a sterile periodontal probe.
These selected sites for gingival crevicular fluid sampling were isolated with cotton rolls and air dried using three-way syringes for 2 s. Calibrated glass micro pipettes (0.5 μL volume) were placed at the opening of the gingival crevice and fluid was collected for a period of 15-20 min. It was then transferred to a glass vial containing 100 μL of phosphate buffer (pH 7, 0.05 M) solution containing 0.1% w/v bovine serum albumin, and stored at −80°C until assay. The glass vial was immediately taken to the lab for analysis.
RESULTS
The aim of this research study is to stabilize the CRP as a gingival crevicular fluid biomarker. CRP levels in patients with periodontitis could prove valuable in identifying patients with enhanced disease susceptibility.
When gingival index was compared, it showed an improvement of 45% on the 14th day and 62% on the 45th day [Table 1]. Bleeding index showed an improvement of 53% and 66% on the 14th and 45th days, respectively [Table 2]. Probing depth decreased by 21% on the 14th day and 37% on the 45th day [Table 3]. Similarly, the clinical attachment level showed improvement of 27% and 45% on the 14th and 45th days, respectively [Table 4]. The mean score for CRP level at baseline was 6.345 ± 3.781, which reduced to 2.675 ± 1.528 at the end of the 14th day, and further reduced to 0.587 ± 0.082 z at the 45th day. On comparison from baseline to the 14th day, a mean change of 3.670 ± 1.253, with “t” value of 4.620 indicated a statistically highly significant reduction (P < 0.01). While comparing baseline from 14th day to 45th day, a mean change of 2.675 ± 0.728 was seen, with “t” value of 7.173, indicating a statistically highly significant reduction at the end of the 45th day (P < 0.01). From baseline to the 45th day, the mean change was 4.647 ± 0.887, with “t” value of 7.607, indicating a highly significant reduction (P < 0.01) [Table 5].
Table 1.
Mean gingival Index before and after treatment
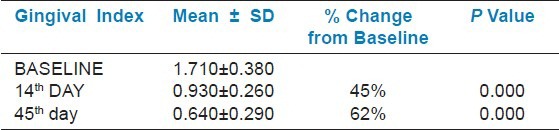
Table 2.
Mean Sulcus bleeding Index before and after treatment
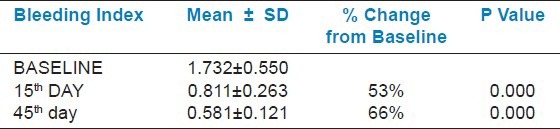
Table 3.
Mean Probing pocket depth level before and after treatment
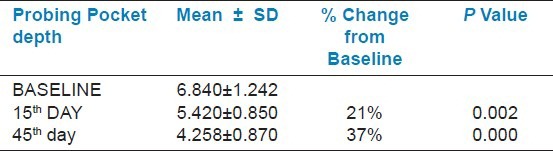
Table 4.
Mean Clinical attachment level before and after treatment
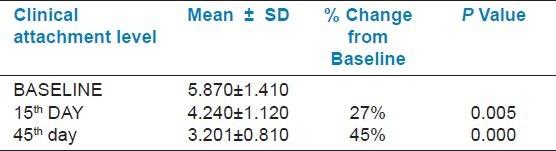
Table 5.
Mean C - reactive protein level before and after treatment
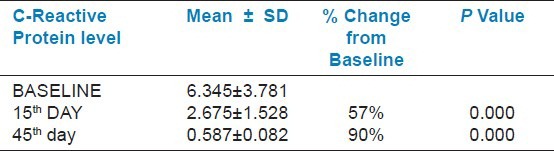
When we made a comparison between the CRP levels from baseline to the 14th day, the improvement was 57%, from baseline to the 45th day was 90% and from the 14th day to the 45th day was 100%.
DISCUSSION
Worldwide, studies show that periodontal disease is commonly spread everywhere but with varying degrees.[3] The present manpower and its efforts are unable to handle the situation in the right manner. Prevention of periodontal destruction rather than therapy should be the goal of dental professionals.
Joshipura et al.[4] in their prospective cohort study showed that tooth loss may be associated with an increased risk of chronic heart disease, primarily among those with a positive periodontal disease history; diet was only a small mediator of this association. Recent studies have also shown that chronic periodontal disease may be a risk factor for heart disease,[5] renal disease, diabetes mellitus, respiratory disease, low birth weight and preterm delivery, and these are also related with altered levels of CRP. Poor oral hygiene and periodontal or periapical infections may induce bacteremia even in the absence of dental procedures. Bacteremia may also result in activation of the hepatic acute response (acute phase response). This response includes elevation of fibrinogen, CRP, heptoglobin, α1 -antitrypsin and other components of acute phase response. There are now considerable data indicating that periodontal infections result in activation of the acute phase response and elevation of certain serum markers.[6] Ridker et al.[7] mentioned that mild elevations in CRP placed an individual at risk for both myocardial infarction and peripheral artery disease. The rapid rise of CRP in serum following exposure to IL-1, which is a potent bone resorber, is found in gingival crevicular fluid. Mergerhagen in 1984 found elevated CRP levels in inflamed periodontal tissues of chronic heart disease patients.
Thus, the primary aim of this study was to quantitatively estimate the CRP level in gingival crevicular fluid samples and the effect of nonsurgical therapy on CRP levels in patients with chronic periodontitis. The gingival index and bleeding index of the experimental period, i.e., on days 0, 14 and 45, were recorded and compared. Results showed a highly significant change with regard to improvement in the gingival inflammation and reduced bleeding on probing from the baseline when compared with the 14th day and the 45th day. However, change was less significant between the 14th day and the 45th day. The definite reductions exhibited could be due to regular follow-up visits and reinforcement of oral hygiene instruction followed by the patient throughout the study period. These results could be correlated with similar findings observed by various other studies.[8,9]
Gains in clinical attachment levels and reduction in pocket probing depth are the most common parameters used to measure clinical improvement. There was a significant decrease in the clinical attachment loss between baseline and 45th day, which was found to be 45%. Statistically significant reduction in the probing pocket depth was also observed at the end of the 45th day, which was 37%. These findings are in agreement with other studies by Persson et al.[10] and Adonogianaki et al.[8]
The primary thrust of this study was to evaluate CRP in gingival crevicular fluid, which is a potential indicator of disease activity. The mean score in this study for CRP level at baseline was 6.235 ± 3.781, which reduced to 2.675 ± 1.528 at the end of the 14th day, and further reduced to 0.587 ± 0.082 at the 45th day. On comparison from baseline to the 14th day, a mean change of 3.670 ± 1.253 with “t” value of 4.820 indicated a highly statistically significant reduction (P < 0.01). While comparing baseline from the 14th day to the 45th day, a mean change of 2.088 ± 0.352 was seen with “t” value of 7.673, indicating a statistically highly significant reduction at the end of the 45th day (P < 0.01). From baseline to the 45th day, the mean change was 4.647 ± 0.887 with “t” value of 7.607, indicating a highly significant reduction (P < 0.01).
The improvement from baseline to the 14th day was 65% and from baseline to the 45th day was 100%. This can be attributed to the fact that CRPs are produced in inflammatory conditions[7,11,12,13] and, once the inflammation subsides due to treatment (scaling and root planning), the CRP levels decrease. Present studies have demonstrated that the extent of increase in CRP levels in periodontitis patient depends on the severity of disease and that the elevation of CRP is associated with the presence of periodontopathic bacteria.[14] It should be noted that CRP levels of patients tended to be higher at baseline and declined at reassessment, suggesting that destructive periodontal diseases are treatable and that it may be possible to lower the CRP value through effective management of destructive periodontal disease.[15] It has been suggested that inflammation status, as assessed by CRP concentration, modifies the vascular protective effects.[16] CRP is an acute phase protein released by hepatocytes in response to increases in circulating inflammatory cytokines. CRP also serves as an activator of the complement system, an immunological cascade that assists the innate immune system by marking and destroying nonself antigens. Activation of complement is thought to contribute to the perpetuation of the inflammatory response, and is implicated in neurodegenerative processes.[17]
SUMMARY AND CONCLUSIONS
CRP level is more significant in gingival crevicular fluid and confirms the underlying inflammatory component of the disease activity in chronic periodontitis. Nonsurgical periodontal treatment was effective in reducing the levels of CRP in gingival crevicular fluid, and this study data support the hypothesis that levels of gingival crevicular fluid biomarkers specific for three aspects of periodontitis – degree of inflammation, collagen degradation and bone turnover – correlate with the clinical features of periodontal disease, and suggest that elevated gingival crevicular fluid levels of CRP are candidate biomarkers of periodontal disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.D’Aiuto F, Ready D, Tonetti MS. Periodontal disease and C-reactive protein-associated cardiovascular risk. J Periodontal Res. 2004;39:236–41. doi: 10.1111/j.1600-0765.2004.00731.x. [DOI] [PubMed] [Google Scholar]
- 2.Iwamoto Y, Nishimura F, Soga Y, Takeuchi K, Kurihara M, Takashiba S, et al. Antimicrobial periodontal treatment decreases serum C-reactive protein, tumor necrosis factor-alpha, but not adiponectin levels in patients with chronic periodontitis. J Periodontol. 2003;74:1231–6. doi: 10.1902/jop.2003.74.8.1231. [DOI] [PubMed] [Google Scholar]
- 3.Polson AM, Goodson JM. Periodontal diagnosis. Current status and future needs. J Periodontol. 1985;56:25–34. doi: 10.1902/jop.1985.56.1.25. [DOI] [PubMed] [Google Scholar]
- 4.Joshipura KJ, Rimm EB, Douglass CW, Trichopoulos D, Ascherio A, Willett WC. Poor oral health and coronary heart disease. J Dent Res. 1996;75:1631–6. doi: 10.1177/00220345960750090301. [DOI] [PubMed] [Google Scholar]
- 5.Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher S. Periodontal disease and cardiovascular disease. J Periodontol. 1996;67:1123–37. doi: 10.1902/jop.1996.67.10s.1123. [DOI] [PubMed] [Google Scholar]
- 6.Herzberg MC, Weyer MW. Dental plaque, platelets, and cardiovascular diseases. Ann Periodontol. 1998;3:151–60. doi: 10.1902/annals.1998.3.1.151. [DOI] [PubMed] [Google Scholar]
- 7.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–9. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 8.Adonogianaki E, Moughal NA, Mooney J, Stirrups DR, Kinane DF. Acute-phase proteins in gingival crevicular fluid during experimentally induced gingivitis. J Periodontal Res. 1994;29:196–202. doi: 10.1111/j.1600-0765.1994.tb01213.x. [DOI] [PubMed] [Google Scholar]
- 9.Adonogianaki E, Mooney J, Kinane DF. Detection of stable and active periodontitis sites by clinical assessment and gingival crevicular acute-phase protein levels. J Periodontal Res. 1996;31:135–43. doi: 10.1111/j.1600-0765.1996.tb00475.x. [DOI] [PubMed] [Google Scholar]
- 10.Persson GR, Pettersson T, Ohlsson O, Renvert S. High-sensitivity serum C-reactive protein levels in subjects with or without myocardial infarction or periodontitis. J Clin Periodontol. 2005;32:219–24. doi: 10.1111/j.1600-051X.2005.00648.x. [DOI] [PubMed] [Google Scholar]
- 11.Ebersole JL, Cappelli D. Acute-phase reactants and inflammatory. Periodontology. 2000;2000(23):19–49. doi: 10.1034/j.1600-0757.2000.2230103.x. [DOI] [PubMed] [Google Scholar]
- 12.Noack B, Genco RJ, Trevisan M, Grossi S, Zambon JJ, De Nardin E. Periodontal infections contribute to elevated systemic C-reactive protein level. J Periodontol. 2001;72:1221–7. doi: 10.1902/jop.2000.72.9.1221. [DOI] [PubMed] [Google Scholar]
- 13.De Nardin E. The role of inflammatory and immunological mediators in periodontitis and cardiovascular disease. Ann Periodontol. 2001;6:30–40. doi: 10.1902/annals.2001.6.1.30. [DOI] [PubMed] [Google Scholar]
- 14.Yamazaki K, Honda T, Oda T, Ueki-Maruyama K, Nakajima T, Yoshie H, et al. Effect of periodontal treatment on the C-reactive protein and proinflammatory cytokine levels in Japanese periodontitis patients. J Periodontal Res. 2005;40:53–8. doi: 10.1111/j.1600-0765.2004.00772.x. [DOI] [PubMed] [Google Scholar]
- 15.Craig RG, Yip JK, So MK, Boylan RJ, Socransky SS, Haffajee AD. Relationship of destructive periodontal disease to the acute-phase response. J Periodontol. 2003;74:1007–16. doi: 10.1902/jop.2003.74.7.1007. [DOI] [PubMed] [Google Scholar]
- 16.Jonathan E, Derrick B, Emma L, Sarah P, John D, Jane A, et al. C-reactive protein concentration and the vascular benefits of statin therapy: An analysis of 20,536 patients in the Heart Protection Study. Lancet. 2011;377:469–76. doi: 10.1016/S0140-6736(10)62174-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eagan DE, Gonzales MM, Tarumi T, Tanaka H, Stautberg S, Haley AP. Serum C-reactive protein relates to increased cerebral myoinositol levels in middle-aged adults. Cardiovasc Psychiatry Neurol. 2012;1:1–9. doi: 10.1155/2012/120540. [DOI] [PMC free article] [PubMed] [Google Scholar]


