Abstract
A patient presented with multiple nodulo-ulcerative lesions over neck and chest. Lymphadenopathy and systemic involvement were absent. Patient was seronegative for HIV. There was no history of local injury and no history of travel. Histopathological findings were consistent with histoplasmosis. Diagnosis of primary cutaneous histoplasmosis was made. We highlight this case owing to its rare and atypical presentation, in an attempt to promote clinical and micro-pathological awareness regarding such occurrences.
Keywords: Micro-pathological awareness, nodulo-ulcerative lesions, primary cutaneous histoplasmosis
INTRODUCTION
Histoplasmosis classically presents as opportunistic mycosis caused by the intracellular dimorphic fungus Histoplasma capsulatum and is frequently associated with HIV infection and other immunocompromised states.[1] In India, histoplasmosis is prevalent in the Gangetic delta.[2] We report a rare case of cutaneous histoplasmosis in a HIV seronegative patient from West Bengal, India.
CASE REPORT
A 28-year-married female from Kolkata, presented at Dermatology outpatient department (OPD) of a hospital with history of nodulo-ulcerative lesions accompanied with extensive inflammation over left antero-lateral neck and chest for last 10 months. She was referred to the Department of Microbiology for further assessment. Close examination revealed pale white to pink nodules, painless papules, ulcerated plaques, and few crusted lesions [Figure 1]. Slight serous discharge was seen on the ulcerated lesions. Scarred and puckered areas of skin were visible amidst the lesions and also over neck and anterior shoulder.
Figure 1.

Pale white to pink nodules, papules, ulcerated plaques, and few crusted lesions over left antero-lateral neck and chest
There was neither any history of fever, nor travelling abroad or to other places in India. Patient did not delineate any past history of splinter injury or thorn prick. However, she gave a history of irregular treatment with antibiotics for last 3 months, for the same. On extensive discussion with the patient, we found that patient was carrying with herself a histopathological report by a private laboratory, mentioning the diagnosis as histoplasmosis. Also, the patient was taking oral itraconazole (past 1 week) and mentioned that lesions have started to heal after taking itraconazole. The anxious patient had somehow lost faith in ongoing treatment and attended our institution in search of alternative opinion and rapid recovery.
On examination, there was no lymphadenopathy and no hepatosplenomegaly. We did not find any other systemic manifestation. She was normoglycemic with a normal hemogram and renal biochemical parameters. Chest X-ray was normal. Patient was seronegative for HIV and, flow cytometry for CD4 count was within normal limit. For microbiological assessment, swabs and scrapings were taken from surface of lesion for staining and bacterial and fungal culture. Scrapings from the surface of the lesions were also sent for histopathological assessment. Though the bacterial and fungal cultures showed no growth, histopathological examination revealed Periodic acid-Schiff (PAS) positive multiple tiny intracellular round to oval yeast forms, few surrounded with halo; suggestive of histoplasmosis [Figure 2]. A diagnosis of primary cutaneous histoplasmosis (PCH) was made. Further the case was lost to follow-up.
Figure 2.
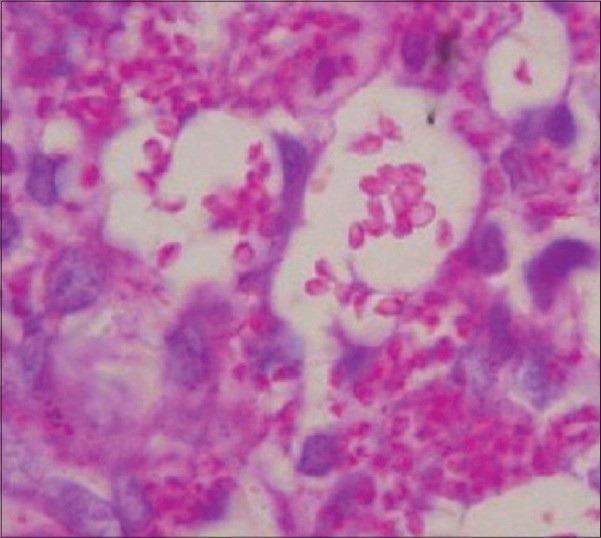
Multiple tiny intracellular round to oval yeast forms, few surrounded with halo in dermis, ×400 PAS stain
DISCUSSION
North-east India including West Bengal is endemic for histoplasmosis.[3] Three main clinical manifestations of histoplasmosis are pulmonary, progressive disseminated and chronic cavitory forms: all may be accompanied with skin lesions, or rarely, the disease manifests as PCH.[4] PCH in immunocompetent individuals itself is very rare, with hardly three case reports, and can present with nodules, ulcers and abscesses.[3,5]
Confirmation of etiology in our case is credited to histopathology and good response to the approved antifungal itraconazole. Absence of lymphadenopathy and hepatosplenomegaly, normoglycemic status, a normal hemogram and renal biochemical parameters and a normal chest X-ray, rule out systemic involvement. Puckering of skin amidst the area of involvement was probably due to healing of inflamed and ulcerated lesions following administration of itraconazole. Source and route of infection are undetermined in our case. The probable route of infection may be through direct inoculation of spores through skin with splinter injury or thorn pricks.[5]
Cutaneous presentation without any systemic involvement, florid inflammation and ulceration, normal CD4 count, HIV seronegative status of the patient and prompt response to appropriate treatment are the notable features of our case. The differential diagnosis of nodulo-ulcerative lesions should include skin and lymphocutaneous malignancies and other systemic mycoses.
CONCLUSION
Though histoplasmosis is reported to be endemic in West Bengal, there are no reports of primary cutaneous histoplasmosis accompanied with extensive inflammation in HIV seronegative individual from West Bengal, till date. In our case, early diagnosis and accurate treatment would have relieved the patient of morbid stress much earlier. Such cases with unusual clinical presentation may pose diagnostic challenge.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chande C, Menon S, Gohil A, Lilani S, Bade J, Mohammad S, Joshi A, et al. Cutaneous histoplasmosis in AIDS. Indian J Med Microbiol. 2010;28:404–6. doi: 10.4103/0255-0857.71850. [DOI] [PubMed] [Google Scholar]
- 2.Subramanian S, Abraham OC, Rupali P, Zachariah A, Mathews MS, Mathai D. Disseminated histoplasmosis. J Assoc Physicians India. 2005;53:185–9. [PubMed] [Google Scholar]
- 3.Nair SP, Vijayadharan M, Vincent M. Primaty cutaneous histoplasmosis. Indian J Dermatol Venereol Leprol. 2000;66:151–3. [PubMed] [Google Scholar]
- 4.Joshi SA, Kagal AS, Bharadwaj RS, Kulkarni SS, Jadhav MV. Disseminated histoplamosis. Indian J Med Microbiol. 2006;24:297–8. doi: 10.4103/0255-0857.29393. [DOI] [PubMed] [Google Scholar]
- 5.Vasudevan B, Ashish B, Amitabh S, Mohanty AP. Primary cutaneous histoplasmosis in a HIV-positive individual. J Glob Infect Dis. 2010;2:112–5. doi: 10.4103/0974-777X.62884. [DOI] [PMC free article] [PubMed] [Google Scholar]


