Abstract
Regarding that the breast cancer is the most prevalent disease among women, paclitaxel, an anti-cancer drug, could be used in treatment of this disease. As paclitaxel has adverse effects, it was used of nanoliposome drug delivery technology in order to reduce adverse effects and improve drug efficacy. Certain ratios of phosphatidylcholine, cholesterol and paclitaxel were synthesized to prepare nanoliposomal paclitaxel. Using Zeta sizer device, the mean diameter of nanoliposomal paclitaxel was obtained 421.4 nm and its encapsulation efficiency was 91.3 %. By dialysis, drug release in nanoliposome paclitaxel formulation within 28 h was studied which was 5.53 %. This study showed that cytotoxicity effect of nanoliposomal paclitaxel is more than that of the standard form.
Keywords: Breast cancer, Nano drug delivery, Paclitaxel, Nanoliposome
Introduction
Breast cancer is the most common cancer among women worldwide [1]. Annually one million cases of breast cancer are diagnosed around the world [2]. Breast cancer can be treated through chemotherapy; radiation and surgery [3]. Paclitaxel is of taxanes family that is used in the treatment of breast cancer. This drug is used in the treatment of ovarian, breast, non-small cell lung, and head and neck cancer [4–6]. Paclitaxel drug with therapeutic effects in patients can cause side effects [7]. Injected carriers in nano scale are utilized to cross biological barriers, protect drug and release the optimize dosage of the drug [8]. Liposome is one of these carriers.
Liposomes are all phospholipid vesicles composed of one or more layers which are concentric aqueous chambers [9, 10]. Liposomes protect the drug against degradation and patients against side effects [11].
The aim of this study was to investigate the effect of improving drug efficacy and reducing its side effects using nanoliposomal paclitaxel.
Materials and Methods
Phosphatidylcholine, cholesterol, paclitaxel and MTT solution (0.5 mg/ml) were purchased from Sigma Chemical Co., USA. Ethanol and isopropanol and RPMI 1640 medium were purchased from Merch Co. and Invitrogen Co., respectively. MCF-7 cells were obtained from the Pasteur Institute Cell Bank of Iran.
Preparation of Nanoliposome and Drug Encapsulation
Phosphatidylcholine and cholesterol (15 to 1 ratio) was dissolved in 120 ml of 98 % ethanol (room temperature, 300 rpm) to obtain a transparent and yellow suspension. Then 13 mg of paclitaxel was added and mixed with a magnetic stirrer (ambient temperature, 30 min, 300 rpm). The solvent phase was evaporated by rotary evaporator (50 °C, 100 rpm) (Heidolph Co., Germany) and the resulted gelos was dissolved in 13 ml of physiological serum. Then the obtained formulation was sonicated for 5 min (Bandelin Sonorex Digitec, 60 Hz).
Size Determination of Nanoliposomes
The mean diameter of the liposomes was determined using Zeta sizer device (Malvern Instruments Ltd.).
Encapsulation Efficiency
To evaluate the percentage of encapsulated drug, 2 ml (2 mg) of the formulation of liposomal paclitaxel was centrifuged at speed 13,000 rpm for 30 min at 4 °C. Then using a spectrophotometer (Model UV-1601PC company SHIMADZU), supernatant absorbance was removed at the wavelength of 227 nm. Then using the following Formula, encapsulation efficiency was calculated.
 |
1 |
In order to plot the standard curve, the serial concentrations of the standard paclitaxel were prepared and their light absorbance was measured using a spectrophotometer at 227 nm wavelength.
Drug Release Examination
To study the release pattern of liposomal paclitaxel, 1 ml of the liposomal drug formulation was poured in the dialysis bag and placed in 100 ml phosphate buffered saline (PBS) pH 7.4 and then put on magnetic stirrer (28 h at 37 °C). To assess the pattern of drug release at various times, 1 ml of PBS buffer was removed and replaced with a 1 ml of fresh phosphate buffer. The light absorbance of the samples was measured at 227 nm wavelength at different times and then the concentration of the free drug in each period was calculated using the standard curve. Finally, the drug release profile versus time was plotted.
Toxicological Effects of Drugs
After culturing the cell line MCF-7, 100 μl of a suspension containing 10,000 cells was decanted in a 96 well plates at temperature of 37 °C and was incubated under CO2 5 %. After 24 h, the cell supernatant was removed and various concentrations of the nanoliposomal paclitaxel formulation and the control were poured on cells. Then they were incubated for 24 h at above conditions. After the supernatant was removed, 100 μl of a solution of MTT (0.5 mg/ml) was added and after 3 h incubation, the purple color (the Formazan formation) was solved in living cells in 100 μl of isopropanol. Light absorbance at 570 nm wavelength was measured (Spectrophotometer Power Eave XS) and IC50 was calculated using the pharm program.
Results
Size Determination of Nanoliposomes
The mean diameter of nanoliposomal Paclitaxel was obtained 421.4 nm.
Encapsulation Efficiency
Encapsulation efficiency (EE %) of the formulation were determined 91.3 % according to the Formula 1.
Evaluation of Drug Release
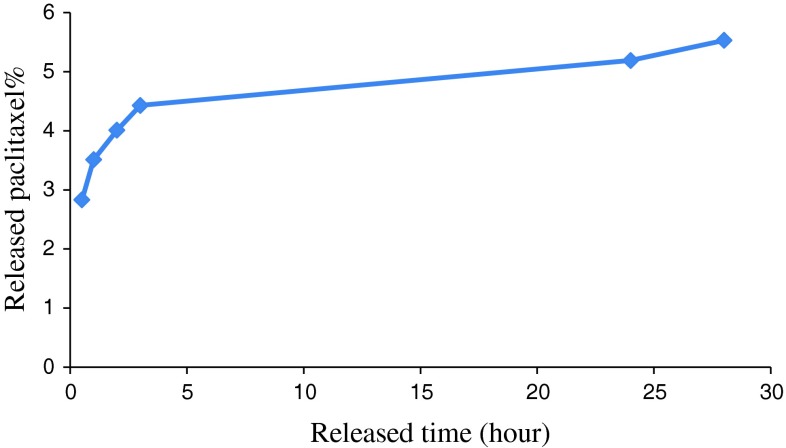
Paclitaxel released from the nanoliposomal paclitaxel formulation in PBS buffer was calculated during time intervals of 30 min, 1 h, 2, 3, 24, and 28 h using the standard curve of paclitaxel (Fig. 1). The following chart is based on the drug release pattern. This chart shows the maximum amount of drug released from liposomes within 28 h, about 5.53 %.
Fig. 1.
Paclitaxel release from formulations liposomal paclitaxel in PBS buffer
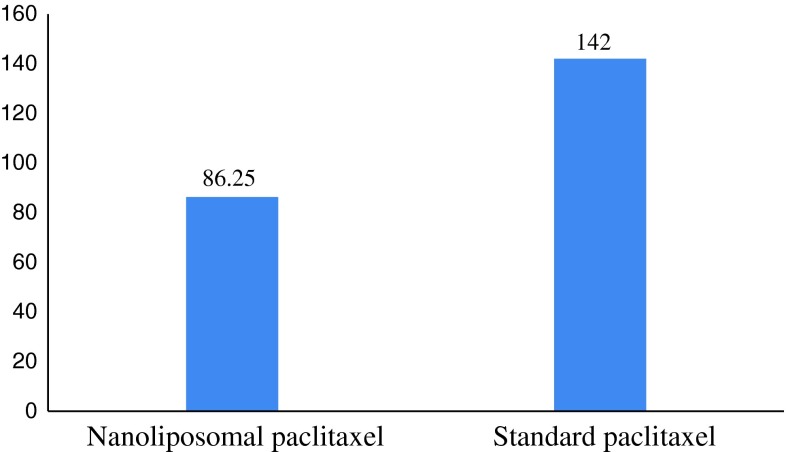
Investigation of Drug Cytotoxicity
Cytotoxicity of the drug in different concentrations was evaluated based on MTT method. The results are given in Fig. 2.
Fig. 2.
The values of IC50 (μl/ml) for two formulations nanoliposomal paclitaxel and standard paclitaxel
Discussion
Drug delivery is one of the main challenges facing biotech [11]. It has been proven that nanocarriers have the ability to deliver drugs to the targeted cells. Liposome is one of lipid nanocarriers. Liposomes protect the drug against degradation and the patient against side effects of encapsulated drug [8].
In 2005, Chen et al. [12] investigated the effect of adriamycin encapsulated in the liposome prescribed for spreaded models of the breast cancer by different ways. The results indicate a high percentage of adriamycin encapsulated in liposome absorbance by tumor cells and the results showed the increment of toxicity of the drug. In 2007, Giotta et al. [13] studied the doxorubicin drug encapsulated in the liposome in cyclophosphamide combination as the first-line treatment of breast cancer. Results of the survey indicated an increase in cytotoxic drug encapsulated in liposomes compared to free form of doxorubicin.
In this study, the influence of the nanoliposomal paclitaxel formulation on breast cancer cell line was studied which shows that a significant amount of drug efficiency encapsulation is located inside the vesicles and this can be largely controlled by the ratio of phospholipid, cholesterol, drugs and methods (the reverse-phase evaporation). The study of nanoliposomal drug release pattern indicates that the drug release is relatively slow and as expected, using liposomes as a drug delivery factor has a significant role in slowing the drug release. This is because it takes more time for the drug to pass through the layers of phospholipid layers of the liposome.
The comparison between toxicological effects of the nanoliposomal paclitaxel formulation with standard paclitaxel indicates the more effect of nanoliposomal paclitaxel formulation in destroying cancer cells. To justify this it can be said that the nanoliposomal paclitaxel formulation because of owing phospholipid structures similar to the bilayer structure of MCF-7 cell membranes could better interact with these cells and by welding them together and release the drug directly into the target cell cause the death increment of these cells.
References
- 1.Warner E. Clinical practice breast-cancer screening. N Engl J Med. 2011;365:1025–1032. doi: 10.1056/NEJMcp1101540. [DOI] [PubMed] [Google Scholar]
- 2.Anders CK, Carey LA. Biology, metastatic patterns, and treatment of patients with triple-negative breast cancer. Clin Breast Cancer. 2009;9:73–81. doi: 10.3816/CBC.2009.s.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo J, Bourre L, Soden DM, O’Sullivan GC, O’Driscoll C. Can non-viral technologies knockdown the barriers to siRNA delivery and achieve the next generation of cancer therapeutics? Biotechnol Adv. 2011;29:402–417. doi: 10.1016/j.biotechadv.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Rowinsky EK, Donehower RC. Paclitaxel (Taxol) N Engl J Med. 1995;332:1004–1014. doi: 10.1056/NEJM199504133321507. [DOI] [PubMed] [Google Scholar]
- 5.Rowinsky EK, Onetto N, Canetta RM, Arbuck SG. Taxol: the first of the taxanes, an important new class of antitumor agents. Semin Oncol. 1992;19:646–662. [PubMed] [Google Scholar]
- 6.Greco FA. Paclitaxel-based combination chemotherapy in advanced non-small cell lung cancer. Lung Cancer. 2001;34:53–56. doi: 10.1016/S0169-5002(01)00393-2. [DOI] [PubMed] [Google Scholar]
- 7.Dorr RT. Pharmacology and toxicology of cremophor el diluent. Ann Pharmacother. 1994;28:11–14. doi: 10.1177/10600280940280S503. [DOI] [PubMed] [Google Scholar]
- 8.Costantino L, Boraschi D. Is there a clinical future for polymeric nanoparticles as brain-targeting drug delivery agents? Drug Discov Today. 2012;17:367–378. doi: 10.1016/j.drudis.2011.10.028. [DOI] [PubMed] [Google Scholar]
- 9.Maurer N, Fenske DB, Cullis PR. Developments in liposomal drug delivery systems. Expert Opin Biol Ther. 2001;1:923–947. doi: 10.1517/14712598.1.6.923. [DOI] [PubMed] [Google Scholar]
- 10.Latif N, Bachhawat BK. Liposomes in immunology. J Biosci. 1984;6:491–502. doi: 10.1007/BF02703901. [DOI] [Google Scholar]
- 11.Georgens C, Weyermann J, Zimmer A. Recombinant virus like particles as drug delivery system. Curr Pharm Biotechnol. 2005;6:49–55. doi: 10.2174/1389201053167202. [DOI] [PubMed] [Google Scholar]
- 12.Chen JH, Ling R, Yao Q, Li Y, Chen T, Wang Z, et al. Effect of small-sized liposomal adriamycin administered by various routes on a metastatic breast cancer model. Endocr Relat Cancer. 2005;12:93–100. doi: 10.1677/erc.1.00871. [DOI] [PubMed] [Google Scholar]
- 13.Giotta F, Lorusso V, Maiello E, Filippelli G, Valerio MR, Caruso M, et al. Liposomal-encapsulated doxorubicin plus cyclophosphamide as first-line therapy in metastatic breast cancer: a phase ii multicentric study. Ann Oncol. 2007;18:66–69. doi: 10.1093/annonc/mdm228. [DOI] [PubMed] [Google Scholar]