Abstract
Purpose
Hydroxyethyl starch (HES) is a synthetic colloid used widely for resuscitation despite the availability of safer, less costly fluids. Numerous HES reviews have been published that may have influenced clinicians’ practice. We have therefore examined the relationship between the methodological quality of published HES reviews, authors’ potential conflicts of interest (pCOI) and the recommendations made.
Methods
Systematic analysis of reviews on HES use.
Results
Between 1975 and 2010, 165 reviews were published containing recommendations for or against HES use. From the 1990s onwards, favorable reviews increased from two to eight per year and HES’s share of the artificial colloid market tripled from 20 to 60 %. Only 7 % (12/165) of these reviews of HES use contained meta-analyses; these 7 % had higher Overview Quality Assessment Questionnaire (OQAQ) scores [median (range) 6.5 (3–7)] than reviews without meta-analysis [2 (1–4); p < 0.001]. The rates of recommending against HES use are 83 % (10/12) in meta-analyses and 20 % (31/153) in reviews without meta-analysis (p < 0.0001). Fourteen authors published the majority (70/124) of positive reviews, and ten of these 14 had or have since developed a pCOI with various manufacturers of HES.
Conclusions
Low-quality HES reviews reached different conclusions than high-quality meta-analyses from independent entities, such as Cochrane Reviews. The majority of these low-quality positive HES reviews were written by a small group of authors, most of whom had or have since established ties to industry. The proliferation of positive HES reviews has been associated with increased utilization of an expensive therapy despite the lack of evidence for meaningful clinical benefit and increased risks. Clinicians need to be more informed that marketing efforts are potentially influencing scientific literature.
Keywords: Hydroxyethyl starch, Meta-analysis, pCOI
Introduction
Hydroxyethyl starch (HES) is one of the most commonly used non-crystalloid plasma expanders in hospitals worldwide, with regulatory approval in Europe, North and South America, and Asia [1–6]. For a half century, this artificial colloid has been used for multiple indications, including hypovolemia, perioperative fluid management, and trauma [7]. It was therefore surprising in a recent multi-center randomized controlled trial comparing HES to crystalloid therapy in septic patients that this starch significantly worsened renal dysfunction and, in high doses, survival [8].
Investigating these findings led to re-examination of the published literature reviewing the risks and benefits of HES. Two meta-analyses provided confirmatory evidence that HES administration for multiple indications was associated with renal failure [9, 10]. Other meta-analyses found that HES increased post-operative bleeding risks [11] and lacked meaningful benefit to support its use compared to safer, less costly crystalloids [12, 13]. In contrast, reviews without meta-analysis appeared to be numerous and supportive of HES [7, 14–19].
Medical reviews are an important component of a physician’s education [20], and they influence practice. However, their quality and validity are known to vary. The rationale for a meta-analysis is that potential bias has been reduced by a systematic identification, synthesis, and statistical aggregation of data from randomized controlled trials of an intervention according to a predetermined and explicit method [21, 22]. High-quality systematic reviews and meta-analyses in general rely on the most current published evidence [23]. However, for busy clinicians not familiar with this methodology, a meta-analysis may be time consuming to read and its results less easy to translate into practice than the more common “expert opinion” review format [24]. These non-systematic—or narrative—reviews frequently provide recommendations from experts in the field in a format expedient to read, but potentially lacking methodological rigor [25]. Such reviews may not present the best current evidence and thus may delay the identification of risks [26]. Despite these shortcomings, physicians are inclined to read less rigorous narrative reviews more often than the more rigorous systematic reviews and meta-analyses [20, 24].
In the study presented here, we investigated the potential reasons why HES use has become so widespread despite what appears to be objective data challenging its benefit and safety. We hypothesized this could be in part because literature addressing the use of HES has been dominated by the proliferation of lower quality reviews supporting its use compared to a relatively small volume of more rigorous meta-analyses that recommend against its use. To test this hypothesis, we performed a search for reviews addressing HES use published since its introduction into clinical practice 50 years ago. We categorized these reviews into those which included meta-analysis and those that did not, and then assessed the quality of these reviews using the Overview of Quality Assessment Questionnaire (OQAQ [27]). We also examined if the reviews provided a favorable or unfavorable recommendation regarding HES use and whether the authors had potential conflicts of interest (pCOI). The results of this study show that the low-quality HES reviews increased steadily in number over the last two decades, were generated by a small group of authors with ties to industry and made recommendations on HES use which were in direct conflict with those of high-quality meta-analysis.
Methods
Search methods
Hydroxyethyl starch fluid therapy reviews were identified by literature searches of electronic databases using the terms “hydroxyethyl starch” and “reviews” in MEDLINE via OVID and PubMed, Web of Science, EMBASE, and CENTRAL (The Cochrane Library, http://www.thecochranelibrary.com) (1960 through to 31 May 2010). The initial search strategy was designed for MEDLINE-Ovid (Appendix 1) and adapted to the other databases, CENTRAL was searched by using the terms “hydroxyethyl starch” and “reviews”. The search covers the period from 1962 when HES was first introduced for clinical use until June 2010.
Inclusion and exclusion criteria
We included meta-analyses and non-meta-analysis reviews which addressed widespread clinical uses of HES, including hypovolemia, hemodilution prior to surgery, anesthesia, critical care, sepsis, emergencies, hemorrhagic shock, burns, trauma, organ transplantation, head injury, stroke, and military and non-military prehospital fluid therapy. We did not consider reviews which addressed uncommon use indications, including hearing loss [28], eclampsia [29], central retinal vein occlusion [30], ovarian hyperstimulation syndrome [31], paracentesis [32], diabetic ketoacidosis [33], hemodilution in chronic obstructive pulmonary disorder [34], apheresis [35], blood component harvest [36], tissue and organ preservation [37, 38], and small volume resuscitation with hypertonic crystalloid/colloid solutions [39]. We included only records written in English, German, and French. Reviews which took part in a pro–con debate were omitted since their conclusions were determined a priori.
Data extraction
One reviewer scanned all titles and abstracts of the reports identified to produce a list of relevant reports to be retrieved in full. Two reviewers screened full texts, reached agreement on a final sample of relevant reviews, then independently abstracted data from the full text of the included studies and resolved disagreement by consensus. The data collection sheet was developed by consensus after an initial reading of a subset of the full texts. A third reviewer resolved disagreements.
Abstracted items
Quality assessment
Depending on whether a review contained a meta-analysis or not, it was classified as a review with or a review without meta-analysis. The quality of these reviews with and without a meta-analysis was assessed by the OQAQ, a validated index of the scientific quality of research overviews [27]. The OQAQ has been used previously to grade reviews in anesthesia and critical care medicine, the specialties that use HES most frequently [40, 41], and serves as a benchmark to evaluate other quality assessment tools [42]. Furthermore, a meta-analysis with a statistical analysis is not a required criterion for scoring. The OQAQ score provides an overall rating from 0 (low quality) to 7 (high quality) (see Appendix 2 for further details). Based on cutoffs previously set by others [40], a review reaching an overall score ≥5 was considered to be a high-quality review, whereas reviews with scores of <5 were categorized as low-quality reviews.
Categories of recommendation
Two reviewers independently graded each review to determine whether the review in question favored the use of HES or not. Statements from the summaries and conclusion sections of the reviews were given priority in evaluating the authors’ opinions about the use of HES. Each author’s exact wording was transcribed for each review. If such information could not be extracted from the summary or conclusion, recommendations about HES were then extracted from the review’s main text. Resulting statements were evaluated and similar statements grouped together to derive categories. Three categories were identified:
Favorable reviews (i.e., reviews that recommended HES use over other fluids) that either recommended HES without qualification or with some clinical qualifiers (i.e., to observe package insert dose limits or to use only HES solutions of a particular molecular weight). This category also included reviews which made no explicit recommendation but claimed that newer HES solutions were either safer and improved over older generation starches and that the reformulation made safety no longer a concern, or that risks associated with HES use were avoidable by taking precautionary measures, such as adequate hydration. Also included were recommendations which were broader in nature, such as favoring synthetic colloids but specifically also including HES (i.e., “gelatin or HES”).
Unfavorable reviews (i.e., reviews that recommended against HES use) that either explicitly stated not to use HES or to use other fluids instead due to increased harm or lack of beneficial outcomes data regarding HES. This category also included reviews which instead of a recommendation stated that the side effects were potentially detrimental, thereby indicating that HES should not be used.
Neutral reviews left the choice of fluid open for the reader to decide for themselves. Some of these reviews explicitly stated that no particular protein or non-protein colloid or crystalloid fluid could be recommended. Other reviews discussed the effects of HES and other fluids in such a way that the authors made it clear they wanted to abstain from indicating any preference or giving any recommendation.
Potential conflict of interest and HES market share
A “potential conflict of interest” was defined to be present if a financial relationship with a manufacturer of commercially available intravenous fluids was declared or if any other kind of support from such a manufacturer was stated. Potential conflicts of interest with companies not manufacturing commercially available fluids were disregarded.
“No conflict of interest” was defined to be present if support was declared from departmental, public, governmental, non-profit, or military organizations, provided the authors did not at the same time declare a financial relationship as defined above.
Not all journals required a declaration of conflict of interest at the time of publication of the HES review. Hence, regarding authors who had published more than two reviews, we searched the internet via Google Scholar for authors’ own statements of financial relationships with a fluid manufacturer. In addition, the market share of HES artificial colloids was determined for the years 1994, 2006 and 2008 from published sources and commercial market research reports [43, 44].
Statements in HES reviews on safety issues and costs
Statements made in any HES review on safety issues, such as the risks of HES causing coagulopathy, renal dysfunction, plasma accumulation, tissue deposition, pruritus, anaphylactoid reactions [45], and HES-associated excess mortality [9], were collected in the database, as well as any statements about the cost of HES compared to other fluids.
Hypothetical statements about HES benefits
We noted when reviews made the following statements:
Harmful effects are clinically manageable [46] or avoidable (e.g., by not exceeding daily dose limits [19], using newer types of HES [47] or providing “free water” [48]).
Newer HES solutions are likely to be safer than older solutions [7].
Additional purported beneficial properties beyond the plasma expansion effect may exist [i.e., anti-inflammatory effect [49], “sealing” of capillary leaks [15, 50], improved microcirculation or tissue oxygenation or rheology [49], prevention of hyperchloremic acidosis by choosing “balanced” HES (i.e., HES in a saline-reduced solvent [51])]. These statements have not been shown to be associated with improved clinically relevant outcomes in randomized controlled trials [52].
Statistical analysis
The number of reviews that met each of the criteria was determined and tabulated. Fisher’s exact test was used to compare the proportions of binary outcomes between the two groups. The OQAQ scores and numbers of reviews were compared between two groups using Wilcoxon rank-sum tests. The Spearman correlation was used to assess the increase in the number of HES reviews over time. All data analyses were conducted using SAS ver. 9.2 (SAS Institute, Cary, NC).
Results
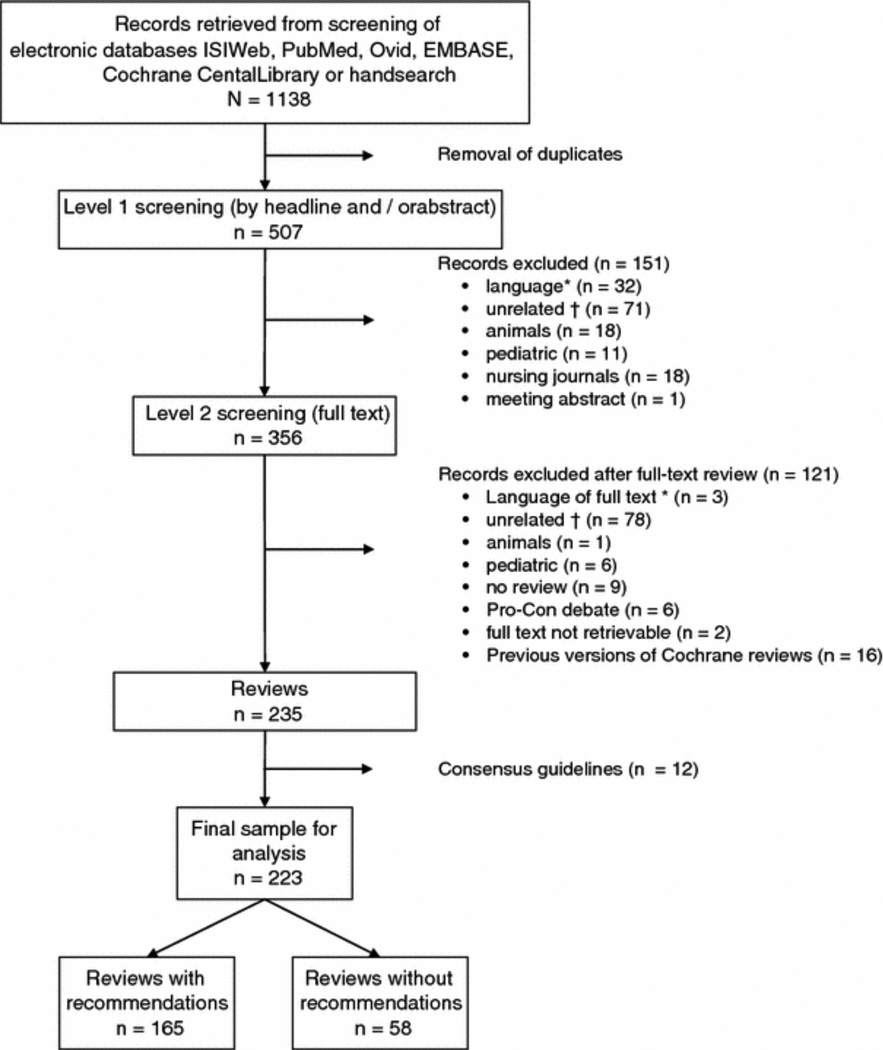
Search
Our searches resulted in a total of 1,138 citations. After screening abstracts and titles of papers and removing duplicates, 356 citations remained. Subsequent examination of the full-text publications led to exclusion of another 121 citations (for details, see Fig. 1). Twelve of the remaining citations were then excluded because they were Consensus Guidelines [53–64]. The final sample for analysis included 223 HES reviews published between 1975 and June 2010 (see full reference list in the Electronic Supplementary Material (ESM)).
Fig. 1.
Study flow. *Excluded languages: Japanese, Russian, Serbocroatian, Polish, Danish, Swedish, Spanish, Portuguese, Chinese, Lithuanian, Czech, Italian. †Unrelated conditions: ovarian hyperstimulation syndrome, retinal vein occlusion, small-volume resuscitation, idiopathic sensorineural hearing loss, eclampsia, diabetic ketoacidosis, chronic obstructive lung disease, polymer science, pharmacokinetics, apheresis, cell harvest, blood component harvest and organ preservation
Characteristics of reviews
Categories of recommendation
Of the 223 HES reviews in our analysis, 165 made a recommendation favorable or unfavorable, and 58 reviews were neutral with respect to their assessment of HES. Only those reviews with a recommendation (165) were included in our analyses because the 58 neutral HES reviews are uninformative regarding our aim of determining reasons why reviews supported or did not support HES use. Of the 165 reviews with recommendations, 124 were favorable and 41 were unfavorable reviews.
Factors associated with HES recommendation
Quality assessment
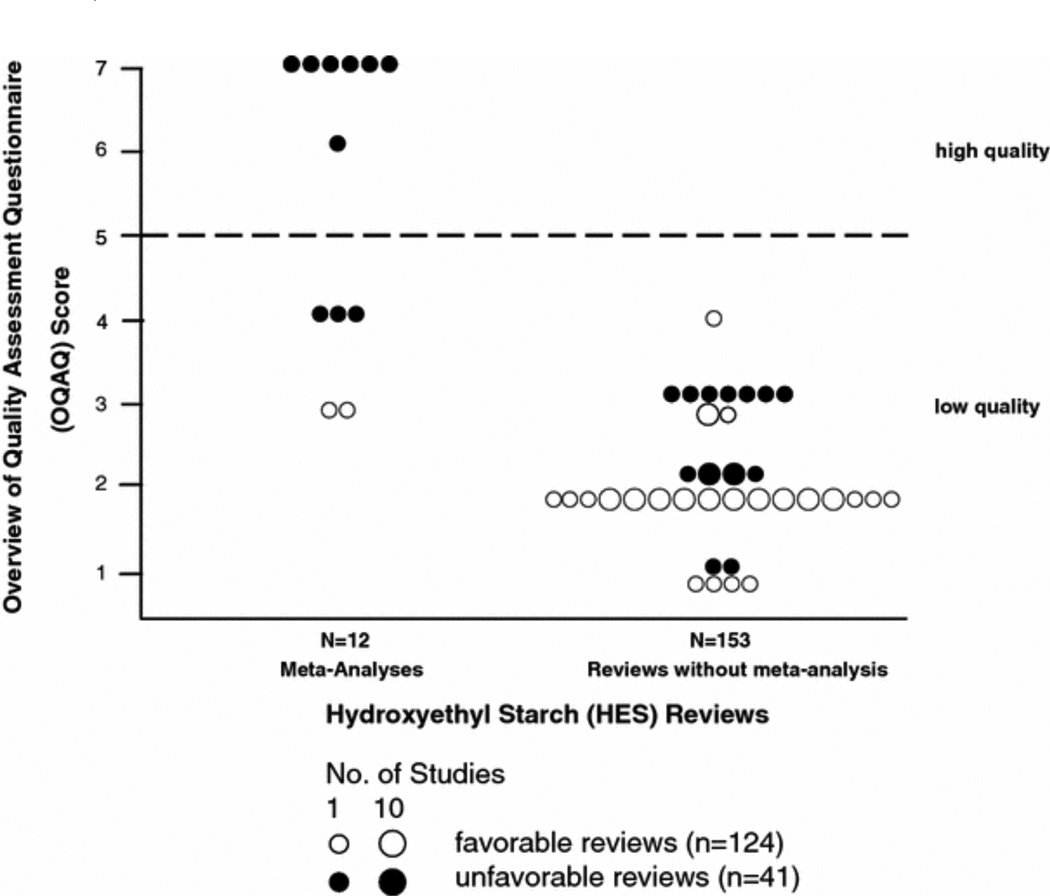
Among the reviews with a recommendation (n = 165), the meta-analyses (n = 12) had a significantly higher OQAQ score than reviews without a meta-analysis (n = 153) [median (range) 6.5 (3–7) vs. 2 (1–4), respectively; p < 0.0001]. Approximately 60 % of meta-analyses met the criteria (OQAQ score ≥5) for high-quality reviews, while none of the reviews without a meta-analysis met the criteria for high quality (7/12 vs. 0/153, respectively; p < 0.0001). Of the 12 meta-analyses, ten made an unfavorable recommendation on HES use and had a higher OQAQ score than those meta-analyses which made an unfavorable recommendation (2/12) [median (range) of 7 (4–7) vs. 3 (3–3); p = 0.02] (Fig. 2). Of note, all seven reviews that met the prospective criteria for being high-quality (OQAQ score ≥5) were meta-analyses and uniformly had an unfavorable view of HES (7/7) (see ESM for references of included reviews).
Fig. 2.
Quality assessment of hydroxyethyl starch (HES) reviews by OQAQ score. Reviews with an overall Overview of Quality Assessment Questionnaire (OQAQ) score of ≥5 are regarded as having minor or minimal flaws, i.e., being of high quality. HES meta-analyses achieved significantly higher OQAQ scores [n = 12; median (range) 6.5 (3–7)] than HES reviews without a meta-analysis [n = 153; 2 (1–4); p < 0.0001]. Meta-analyses that were not in favor of HES use achieved significantly higher OQAQ scores [n = 10, 7 (4–7)] than favorable meta-analyses [n = 2, 3 (3–3); n = 0.02]
Reviews with or without meta-analysis
Forty-one reviews had an unfavorable view of HES, of which 25 % (10/41) were meta-analyses, and approximately 75 % (31/41) were low-quality reviews without a meta-analysis. In comparison, 124 reviews had a favorable view of HES, of which <2 % (2/124) were meta-analyses, and all 124 favorable reviews were of low quality (Fig. 2).
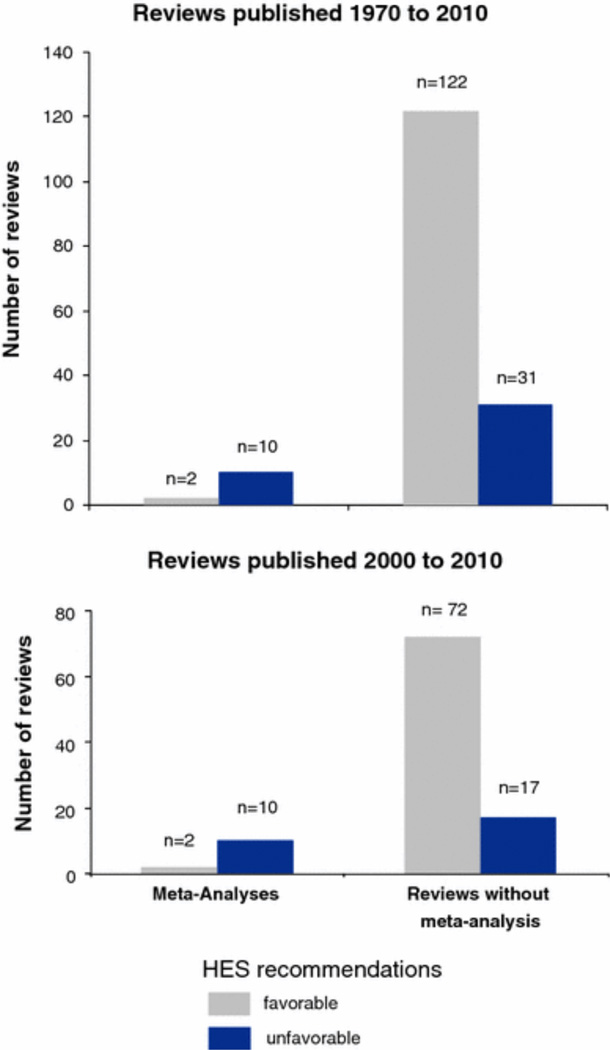
From 2000 to 2010 (HES meta-analyses were not published before this decade), a review with a meta-analysis was more likely to make an unfavorable recommendation on HES use (10/12, 83 %) while reviews without a meta-analysis were more likely to favor HES use (72/89, 81 %) (p < 0.0001; Fig. 3). The results remain unchanged if we consider all HES reviews that made a recommendation included in our analysis from 1970 to the present (Fig. 3). There was no significant difference in the clinical condition focused on by reviews with or without a meta-analysis to explain these results (p = 0.35; Table 1).
Fig. 3.
Hydroxyethyl starch recommendation in the meta-analyses and reviews without a meta-analysis. If a recommendation was made in a review with a meta-analysis, 83 % of the recommendations were unfavorable. In contrast, only 20 % of reviews without a meta-analysis made an unfavorable recommendation (83 vs. 20 %, respectively; p < 0.0001, Fisher’s exact test). The results are virtually identical if only studies from 2000 to 2010 are included (lower panel), the years in which HES meta-analyses began to be published
Table 1.
Clinical condition focused on by the HES reviews
| Clinical condition |
Meta-analyses | Reviews without a meta-analysis | ||||
|---|---|---|---|---|---|---|
| Unfavorable (n = 10) |
Favorable (n = 2) |
Total (n = 12) |
Unfavorable (n = 31) |
Favorable (n = 122) |
Total (n = 153) |
|
| Hypovolemia not specified |
3 | 0 | 3 | 12 | 51 | 63 |
| Shock, major bleeding, trauma, burns, pre- clinical fluid therapy |
1 | 0 | 1 | 11 | 19 | 30 |
| Critically ill and septic patients |
3 | 0 | 3 | 5 | 22 | 27 |
| Peri- operative volume therapy and ANH prior to surgery, fluid therapy to prevent hypotension following neural block |
2 | 2 | 4 | 2 | 25 | 27 |
| Fluid therapy for brain injury, including stroke, intracerebral hemorrhage or neurosurgery |
1 | 0 | 1 | 1 | 5 | 6 |
ANH Acute normovolemic hemodilution
Data are presented as the number of studies
HES reviews and sales over time and author’s potential conflict of interest (COI)
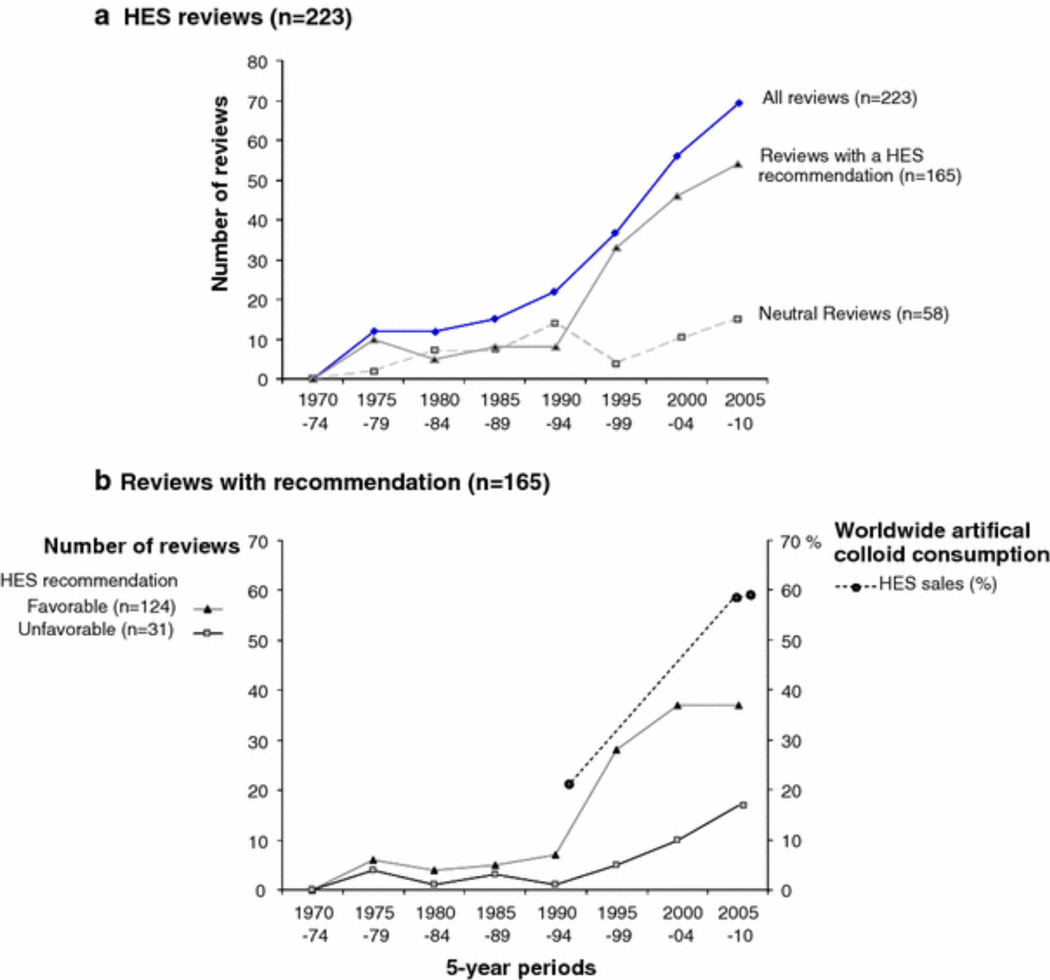
From 1970 to 2010 the number of HES reviews has steadily increased over time (p = 0.0008). If we divide this time period in half at 1990 and compare the earlier time period to the more recent one the number of positive reviews has increased (p = 0.05) and the percentage of positive reviews shows a trend to increase (p = 0.09). Notably, the number of favorable HES reviews has increased more dramatically after 1990 (2/year to 6–8/year), as has the world-wide artificial colloid market share of HES (from approximately 20 % in 1994 to approximately 60 % in 2008 [43, 44]; Fig. 4). A declaration of whether a pCOI was present or not with a source of funding was found in 18 % (27/153) reviews without a meta-analysis. Nine of these reviews reported that a pCOI was present, while 18 reported that they had no potential pCOI. All reviews (9/9; 100 %) which reported a pCOI were in favor of HES, while fewer of those reviews which reported no pCOI (12/18; 67 %) were favorable to HES (100 vs. 67 %, respectively; p = 0.07).
Fig. 4.
Hydroxyethyl starch reviews and HES consumption. The number of HES reviews increased after 1990, and most of these contained a recommendation (a). Favorable reviews in particular increased dramatically during this period in which the HES market share of worldwide artificial colloid consumption tripled from approx. 20 % [43] to approx. 60 % [44] (b)
We further researched declarations of pCOI for authors who wrote three or more reviews. No one author wrote more than two unfavorable (n = 41) or neutral reviews (n = 58). In comparison, 14 authors wrote three or more favorable reviews, representing 56 % of all positive reviews (70/124). Of these 14 authors, three alone wrote 25 % (31/124) of the positive reviews, and all three had or subsequently developed pCOI relationships with various manufacturers of HES after publishing the positive HES reviews. The other 11 authors writing three or more favorable reviews authored or co-authored another 31 % of the positive reviews (39/124); seven of these authors had or eventually developed a pCOI relationship with manufacturers of HES (see Table 2). Three authors simultaneously or subsequently served as salaried Medical Officers for a fluid manufacturing company. Most of these authors’ reviews were of low quality, and one was a favorable low-quality HES meta-analysis. Only six of 70 positive reviews (9 %) by these 14 authors gave any declaration of a pCOI with a HES manufacturer (Table 2).
Table 2.
The 14 most prolific authors of 124 favorable HES reviews and their potential conflict of interest with fluid manufacturers
| Author | pCOI declared/HES reviews by this author (n) |
Years in which HES reviews were published |
Years in which a pCOI related to a fluid manufacturer was declared by the author |
|---|---|---|---|
| 1 | 1/21 | 1998–2009 | 2009 (“past research activities were funded by…”) [19] |
| 2 | 1/5 | 2005, 2007–2009 |
2008 (lead author of a meta-analysis funded by and co-authored by a salaried employee of a fluid manufacturer) [86]; 2010 (“has received honoraria as a speaker and research support from…”) [87] |
| 3 | 0/5 | 1997–2000 | 2003 (“unrestricted grant by fluid manufacturer”) [87] |
| 4 | 0/4 | 1998, 2001, 2003 |
2006 (“received honoraria from …”) [88] |
| 5 | 1/4 | 2007–2009 | 2008 (“recipient of travel grants” and an “unrestricted educational grant”) [89] |
| 6 | 0/4 | 1993, 2003–2005 |
2008 (“honoraria and unrestricted grants from… “) [54] |
| 7 | 0/4 | 1991, 2000, 2004 |
2006 (“has received unrestricted grants”) [90]; see correction published [Br Med J 2006; 333 doi:10.1136/bmj.39041.739479.68] |
| 8 | 0/3 | 1998, 2000, 2002 |
2002 (recipient of salary from fluid manufacturer) [91] |
| 9 | 0/3 | 2008, 2009 | 2011 (recipient of salary from fluid manufacturer) [92] |
| 10 | 3/3 | 2005, 2007–2008 |
2002–2008 (recipient of salary from fluid manufacturer) [70,92] |
| 11 | 0/4 | 1993, 1998, 2007, 2009 |
No pCOI identified |
| 12 | 0/4 | 1982, 1986, 1996, 2002 |
No pCOI identified |
| 13 | 0/3 | 1986, 1996, 2007 |
No pCOI identified |
| 14 | 0/3 | 2004–2006 | No pCOI identified |
A potential conflict of interest (pCOI) was declared by four authors in six of these reviews. A pCOI with a fluid manufacturer was declared by additional six authors in other publications at the time or up to 3 years after their last HES review was published. Three authors (9/124 reviews) served as salaried Medical Officers for a fluid manufacturing company at the time of writing or soon thereafter
Fourteen authors wrote 56 % (70/124) of all favorable reviews. The three most prolific authors (authors 1, 2 and 3) wrote 25 % (31/124) of these reviews; the remaining 11 authors wrote 31 % (39/124)
Hypothetical statements
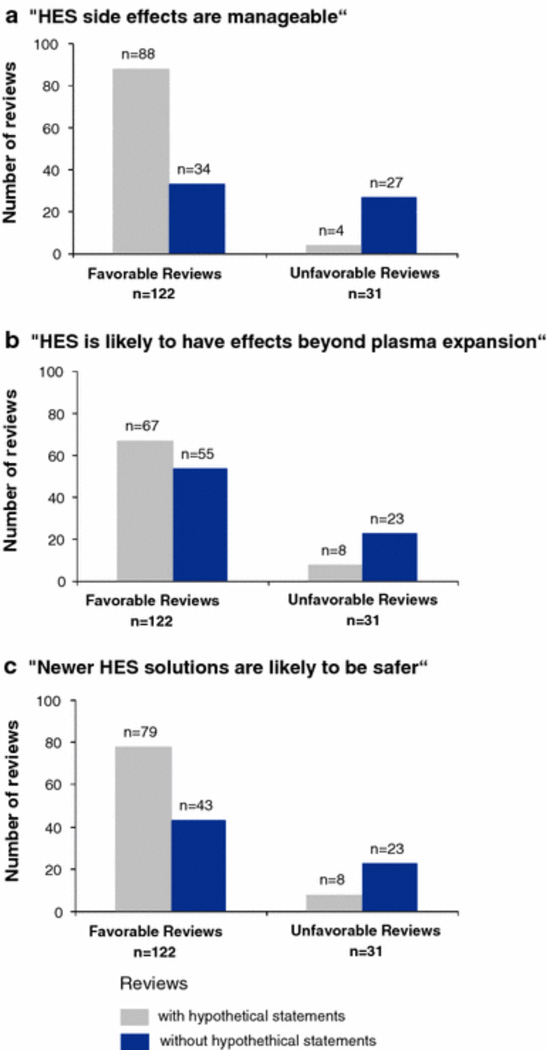
Among the 153 reviews which contained no meta-analysis, three statements were examined: (1) “HES side effects are manageable,” (2) “HES may have potential beneficial effects beyond plasma expansion,” and (3) “Newer HES solutions are likely to be safer.” These statements were significantly more frequently associated with favorable than non-favorable reviews (p = 0.005 to p = 0.0001; Fig. 5).
Fig. 5.
Hypothetical statements made in HES reviews without meta-analysis (n = 153). In reviews without a meta-analysis that recommended HES use, 72 % (88/122) stated that side effects were manageable (a), 55 % (67/122) stated that HES probably had additional beneficial effects beyond plasma expansion (b), and 65 % (79/122) stated that newer preparations of HES were likely to be safer (c). In contrast, in reviews without a meta-analysis that expressed an unfavorable recommendation with respect to HES use, 13 % (4/31) claimed that side effects were manageable (a), 26 % (8/31) claimed HES probably had additional beneficial effects (b), and 26 % (8/31) claimed that newer HES solutions were likely to be safer (c). a 72 versus 13 % (p “ 0.0001), b 55 versus 26 % (n = 0.005), c 65 versus 26 % (n = 0.0002), respectively, by Fisher’s exact test
Factors which were not significantly associated with HES recommendation
Among the 153 reviews that contained no meta-analysis, the mention of HES safety issues or cost aspects was not significantly different in the favorable compared to unfavorable reviews. Specifically, in reviews without a meta-analysis that recommended HES use, 91 % (111/122) discussed one or more aspects of HES safety and 51 % (62/122) discussed cost aspects. Similarly, in reviews without a meta-analysis that did not recommend HES use, 84 % (26/31) discussed one or more aspects of HES safety and 55 % (17/31) discussed cost aspects of HES (data not shown).
Consensus Guidelines
Our search identified by chance 12 Consensus Guidelines that mentioned HES: six were unfavorable to HES use by either favoring crystalloids [53, 59, 62] or cautioning specifically against the use of HES [56–58] and four were neutral, recommending the use of either crystalloids or artificial/synthetic colloids [55, 60, 63, 64]. Only two of the 12 guidelines were favorable to HES by either directly recommending HES [61] or indirectly recommending HES by cautioning against higher molecular weight formulations but not newer lower molecular weight formulations [54]. The second favorable HES guideline was co-authored by some of the 14 top-publishers of HES-positive reviews. The four guidelines that both referenced and based their conclusions in part on high-quality meta-analyses of HES trials [9–11, 13, 65, 66] resulted in unfavorable HES recommendations [56–58] or a recommendation that favored crystalloids [59]. Overall, most guidelines did not specifically recommend HES use, but those that did were written by authors who had or eventually developed ties to HES manufacturers [54, 61].
Discussion
Our analyses of 165 reviews with a recommendation for HES use shows that there is a strong association between methodological quality, the presence or absence of a meta-analysis, and the recommendation made. Meta-analyses with the highest scores (≥5) on the 7-point OQAQ rating system [27] were uniformly unfavorable to HES use (7/7). Among these very high-quality meta-analyses were six Cochrane reviews and one Health Technology Assessment report [10, 12, 13, 65, 67–69]. In contrast, the only two meta-analyses with low-quality scores both recommended HES use [66, 70]. Reviews without a meta-analysis also had a lower methodological quality score and favored HES, whereas overall, HES meta-analyses had high-quality scores and were unfavorable to HES use. Although the clinical conditions discussed in the reviews were similar, the differences in recommendations made with and without a meta-analysis were highly statistically significant.
We also found an association between the type of recommendation, HES sales, and declared and undeclared relationships with HES manufacturers. Over the last 35 years, the number of low-quality reviews without a meta-analysis in favor of HES use (n = 122) have outnumbered the number of low-quality reviews not in favor of HES use by four-to-one (n = 31). The increase in low-quality positive HES reviews without a meta-analysis in the last 20 years occurred over a time when HES sales increased. Very few of these reviews disclosed a pCOI. All reviews that did disclose a pCOI favored HES. Low disclosure rates are common for reviews [71], as are strong links between an author’s orientation and financial ties to pharmaceutical companies [71, 72]. These types of associations between an author’s affiliation(s) to industry and the favorable recommendation of a product have been described previously [71, 73–75].
Our research also showed that a relatively small number of physicians (n = 14) with ties to industry wrote the majority of the reviews recommending HES use. A pCOI with a HES manufacturer was declared in only 9 % (6/70) of these authors’ reviews. However, literature searches found that ten of these 14 authors had concurrently or within 3 years after the publication of their last review received funding from a HES manufacturer, and three eventually served as salaried medical officers for a HES fluid manufacturer (Table 2). One of the top 14 authors of favorable HES reviews published 17 % (21/124) of all positive reviews, the most by a single author. Only one of the most recent HES reviews authored by this individual declared a pCOI [19]. Importantly, not all journals required pCOI declarations at the time these HES reviews were published. This top author of 22 reviews—who has multiple commercial ties—is presently under investigation for scientific misconduct. A randomized controlled trial showing HES reduced cytokine levels and attenuated tissue damage was retracted [76]. At the time of writing, nearly 90 articles are being reviewed [77]. Because drug companies seek out researchers who happen to be getting positive results [78], one might speculate that particularly if such relationships are financially or academically rewarding, researchers with strong commercial ties may feel under pressure to produce favorable results.
Synthetic colloids such as HES have been closely associated with serious side effects, including increased bleeding, impaired platelet function, and renal failure [79]. The long-term effects of large colloid molecules like HES, which can remain deposited in tissue for years, remain unknown. Moreover, HES in larger doses and in sicker patients has been associated with decreased survival rates [8, 9]. Of these side effects, coagulopathy and tissue uptake have been reported over longer periods of time (>35 years), while increased renal failure with HES solutions has only been recognized over the last 10 years. Most low-quality reviews addressed HES side effects but did not include data from adequately powered, randomized, controlled trials to substantiate the discussions [80]. Notably, safety issues were similarly mentioned in favorable and unfavorable reviews—potentially to protect patients from harm and liability concerns —while hypothetical statements were significantly more frequent in favorable reviews.
Specifically, the 122 favorable HES reviews lacking a meta-analysis were more likely to use hypothetical statements to support their recommendation, stating that HES side effects are “manageable,” that HES has “beneficial effects beyond plasma expansion,” and that “newer formulations of HES are safer.” None of the assertions in these statements has yet been shown to improve meaningful patient outcomes in adequately designed clinical trials. Hypothetical statements, such as these recurring in the medical literature over time, have been shown to create an “echo chamber effect” [81] which potentially mitigates concerns about drugs and exaggerates their effectiveness [82]. While misleading readers may not be the sole intent of such statements, it can be integral to a marketing strategy which may include medical ghost writing or management of medical investigators writing reviews [83]. Most importantly, physicians need to be made more aware of marketing efforts disguised as scientific literature.
Limitations
The underreporting of unfavorable trials may have influenced the findings of the meta-analysis reported here [84]. However, this cannot easily explain the difference in overall conclusions on HES use drawn by independent authors of high-quality Cochrane reviews and authors of low-quality reviews with ties to industry. Our search method focused on reviews and not on consensus guidelines. To be complete, those guidelines that were found by chance were reported separately, but there may have been some unknown sampling bias. We did not include guidelines in the analysis of reviews because this inclusion may be redundant since non-objective reviews with potential COI may have an effect on the objectivity of guidelines, as suggested by an example where recommendations [54] differ from evidence-based summaries [85]. The sponsorship of review by HES manufacturers may not have been the only influence on prescribing habits: the temporary discrediting of albumin, a competitor product for the same market as HES at the end of the 1990s, the amount and type of advertising in scientific journals and trade journals by the manufacturer, and industry handouts, as well as sponsorship of conferences, speakers or educational events may all have played a role.
Conclusions
More than one-half of the lower quality reviews that recommended HES use were written by a small group of authors with ties to industry; these authors came to different conclusions than those of high-quality meta-analyses by independent entities, such as Cochrane Reviews. The proliferation of reviews with a positive recommendation for HES use has been associated with increased utilization of an expensive therapy despite the lack of evidence for meaningful clinical benefit and increased risks to patients. Journals, medical societies, medical boards, and continuing medical education accrediting agencies need to work together to establish methodology to minimize the ability of a select group of clinicians with undisclosed industry ties to flood the scientific literature with low-quality positive reviews and possibly affect sales of products that may potentially increase patient risks.
Supplementary Material
Acknowledgments
The authors thank B. Kabisch, PhD, M. Muecke, and D. Schwarzkopf for their support in data analysis and J. Maltagliati for editing assistance. No compensation was received for these contributions. Funds for this project were provided by the Intramural Research Program of the U.S. National Institutes of Health. C. Natanson and J. Sun are U.S. government employees, and both did the work on this paper as part of their official U.S. government-funded research duties. However, the opinions expressed do not necessarily represent those of the U.S. National Institutes of Health.
Appendix 1
Electronic search strategy
Keywords: hetastarch OR hydroxyethyl starch OR hydroxyethylstarch OR pentastarch OR haes-steril OR Hextend OR Elohes OR Elohaes OR Expafusin OR Voluven OR hemohes OR hespan OR pentafraction OR pentaspan OR plasmasteril OR plasma expander OR hydroxyethylstarke OR hydroxyathylstarke OR hydroxyethyl starke OR HAES OR hydroxyethylamidon OR (colloid and crystalloid) AND fluid therapy OR fluid OR intensive care OR emergency OR burn OR organ transplantation OR donor resuscitation OR fluid resuscitation OR volume or hemodilution OR head injury OR stroke OR brain injury OR cerebral injury OR intracranial bleeding OR intravascular therapy OR plasma substitutes OR plasma expanders OR remplissage OR volumentherapy OR volumenersatz or plasmaersatz) AND review OR meta-analysis OR systematic review OR narrative review OR overview OR metaanalysis OR pooled analysis.
Appendix 2
The OQAQ is a validated instrument which has been used before in the setting of critical care [40] and anesthesia [41]. The OQAQ quality features according to Oxman et al. [27] and Delaney et al. [40] are as follows:
Were the search methods used to find evidence on the primary question(s) stated? (2) Was the search for evidence reasonably comprehensive?
Was the search for evidence reasonably comprehensive?
Were the criteria used for deciding which studies to include in the overview reported?
Was bias in the selection of studies avoided?
Were the criteria used for assessing the validity of the included studies reported?
Was the validity of all the studies referred to in the text assessed using appropriate criteria?
Were the methods used to combine the findings of the relevant studies (to reach a conclusion) reported?
Were the findings of the relevant studies combined appropriately relative to the primary question of the overview?
Were the conclusions made by the author(s) supported by the data and/or analysis reported in the overview?
How would you rate the overall quality of this overview?
Possible answers to questions 1–9 are: 1 = no; 2 = partially or cannot tell; 3 = yes. Answer to question 10 is: if the methods that were used are reported incompletely relative to a specific item, that item should be scored as “partially.” Similarly, if there is no information provided regarding what was done relative to a particular question, this question should be scored as “cannot tell,” unless there is information in the overview to suggest either that the criterion was or was not met.
For question 2, for a search to be considered comprehensive the methods used to perform the search should include searching for unpublished material as well as multiple medical databases (EMBASE as well as MEDLINE). If only published material was searched for, the search should be assessed as “partially” For question 4, for bias to have been avoided in the selection of studies, the report should indicate that explicit criteria were used to define studies eligible for inclusion. For question 6, to determine whether the validity was assessed using appropriate criteria, all of the studies in the text must have had their validity assessed and explicit criteria which were appropriate for the type of research question that was being addressed must have been used. For question 8, if no attempt has been made to combine findings, and no statement is made regarding the inappropriateness of combining findings, check “no.” If a summary (general) estimate is given anywhere in the abstract, the discussion, or the summary section of the paper, and it is not reported how that estimate was derived, check off “no,” even if there is a statement regarding the limitations of combining the findings of the studies reviewed. If in doubt, check off “can’t tell.” For an overview to be scored as “yes” on question 9, data (not just citations) must be reported that support the main conclusions regarding the primary question(s) that the overview addresses. The score for question 10, the overall scientific quality, should be based on your answers to the first nine questions. The following guidelines can be used to assist with deriving a summary score: if the “cannot tell” option is used one or more times on preceding questions, a review is likely to have minor flaws at best, and it is difficult to rule out major flows (i.e., a score ≤4). If the “no” option is used on questions 2, 4, 6, or 8, the review is likely to have major flaws (i.e., a score of ≤3, depending on the number and degree of the flaws).
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s00134-012-2614-0) contains supplementary material, which is available to authorized users.
Conflicts of interest
C. Hartog, H. Skupin, J. Sun, and C. Natanson declare that they have no conflict of interest. K. Reinhart has in the past received an unrestricted grant for the conduct of the VISEP study and speaker’s and consultancy fees from B. Braun, Melsungen, Germany. B.Braun, Melsungen also contributed to the German Sepsis Society to fund an endowed professorship for clinical sepsis research at the University Hospital of Jena.
References
- 1.Finfer S, Liu B, Taylor C, Bellomo R, Billot L, Cook D, Du B, McArthur C, Myburgh J, Investigators TS. Resuscitation fluid use in critically ill adults: an international cross sectional study in 391 intensive care units. Critical Care (Lond) 2010;14:R185. doi: 10.1186/cc9293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schortgen F, Deye N, Brochard L. Preferred plasma volume expanders for critically ill patients: results of an international survey. Intensive Care Med. 2004;30:2222–2229. doi: 10.1007/s00134-004-2415-1. [DOI] [PubMed] [Google Scholar]
- 3.The FLUIDS study investigators for the Scandinavian Critical Care Trials Group. Preferences for colloid use in Scandinavian intensive care units. Acta Anaesthesiol Scand. 2008;52:750–758. doi: 10.1111/j.1399-6576.2008.01690.x. [DOI] [PubMed] [Google Scholar]
- 4.Basora M, Moral V, Llau JV, Silva S. Perioperative colloid administration: a survey of Spanish anesthesiologists’ attitudes. Rev Esp Anestesiol Reanim. 2007;54:162–168. [PubMed] [Google Scholar]
- 5.Liu FC, Liao CH, Chang YW, Liou JT, Day YJ. Hydroxyethyl starch interferes with human blood ex vivo coagulation, platelet function and sedimentation. Acta Anaesthesiol Taiwan. 2009;47:71–78. doi: 10.1016/S1875-4597(09)60027-8. [DOI] [PubMed] [Google Scholar]
- 6.Hartog CS, Brunkhorst FM, Bloos F, Bogatsch H, Engel C, Sengebusch K, Reinhart K, Ragaller M. Practice of volume therapy in patients with severe sepsis: results from a nationwide sepsis prevalence study. Intensive Care Med. 2010;36:553–554. doi: 10.1007/s00134-009-1736-5. [DOI] [PubMed] [Google Scholar]
- 7.Westphal M, James MF, Kozek-Langenecker S, Stocker R, Guidet B, Van Aken H. Hydroxyethyl starches: different products—different effects. Anesthesiology. 2009;111:187–202. doi: 10.1097/ALN.0b013e3181a7ec82. [DOI] [PubMed] [Google Scholar]
- 8.Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–139. doi: 10.1056/NEJMoa070716. [DOI] [PubMed] [Google Scholar]
- 9.Zarychanski R, Turgeon AF, Fergusson DA, Cook DJ, Hebert P, Bagshaw SM, Monsour D, McIntyre LA. Renal outcomes and mortality following hydroxyethyl starch resuscitation of critically ill patients: systematic review and meta-analysis of randomized trials. Open Med. 2009;3:E196–E209. [PMC free article] [PubMed] [Google Scholar]
- 10.Dart AB, Mutter TC, Ruth CA, Taback SP. Hydroxyethyl starch (HES) versus other fluid therapies: effects on kidney function. Cochrane Database of Systematic Reviews. 2010 doi: 10.1002/14651858.CD007594.pub2. (Online):CD007594. [DOI] [PubMed] [Google Scholar]
- 11.Wilkes MM, Navickis RJ, Sibbald WJ. Albumin versus hydroxyethyl starch in cardiopulmonary bypass surgery: a meta-analysis of postoperative bleeding. Ann Thorac Surg. 2001;72:527–533. doi: 10.1016/s0003-4975(01)02745-x. [DOI] [PubMed] [Google Scholar]
- 12.Perel P, Roberts I. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database of Systematic Reviews. 2009 doi: 10.1002/14651858.CD000567.pub3. (Online):CD000567. [DOI] [PubMed] [Google Scholar]
- 13.Bunn F, Trivedi D, Ashraf S. Colloid solutions for fluid resuscitation. Cochrane Database of Systematic Reviews. 2008 doi: 10.1002/14651858.CD001319.pub2. (Online):CD001319. [DOI] [PubMed] [Google Scholar]
- 14.Mishler JM. Synthetic plasma volume expanders—their pharmacology, safety and clinical efficacy. Clin Haematol. 1984;13:75–92. [PubMed] [Google Scholar]
- 15.Vincent JL. Fluids for resuscitation. Br J Anaesth. 1991;67:185–193. doi: 10.1093/bja/67.2.185. [DOI] [PubMed] [Google Scholar]
- 16.Treib J, Baron JF, Grauer MT, Strauss RG. An international view of hydroxyethyl starches. Intensive Care Med. 1999;25:258–268. doi: 10.1007/s001340050833. [DOI] [PubMed] [Google Scholar]
- 17.de Jonge E, Levi M. Effects of different plasma substitutes on blood coagulation: a comparative review. Crit Care Med. 2001;29:1261–1267. doi: 10.1097/00003246-200106000-00038. [DOI] [PubMed] [Google Scholar]
- 18.Kozek-Langenecker SA. Effects of hydroxyethyl starch solutions on hemostasis. Anesthesiology. 2005;103:654–660. doi: 10.1097/00000542-200509000-00031. [DOI] [PubMed] [Google Scholar]
- 19.Boldt J. Modern rapidly degradable hydroxyethyl starches: current concepts. Anesth Analg. 2009;108:1574–1582. doi: 10.1213/ane.0b013e31819e9e6c. [DOI] [PubMed] [Google Scholar]
- 20.McAlister FA, Graham I, Karr GW, Laupacis A. Evidence-based medicine and the practicing clinician. J Gen Intern Med. 1999;14:236–242. doi: 10.1046/j.1525-1497.1999.00323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J (Clinical Research edn) 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guyatt GH, Haynes RB, Jaeschke RZ, Cook DJ, Green L, Naylor CD, Wilson MC, Richardson WS. Users’ Guides to the Medical Literature: XXV. Evidence-based medicine: principles for applying the Users’ Guides to patient care. Evidence-based medicine working group. JAMA. 2000;284:1290–1296. doi: 10.1001/jama.284.10.1290. [DOI] [PubMed] [Google Scholar]
- 24.Loke YK, Derry S. Does anybody read “evidence-based” articles? BMC Med Res Methodol. 2003;3:14. doi: 10.1186/1471-2288-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med. 1997;126:376–380. doi: 10.7326/0003-4819-126-5-199703010-00006. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt LM, Gotzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334–338. [PubMed] [Google Scholar]
- 27.Oxman AD, Guyatt GH, Singer J, Goldsmith CH, Hutchison BG, Milner RA, Streiner DL. Agreement among reviewers of review articles. J Clin Epidemiol. 1991;44:91–98. doi: 10.1016/0895-4356(91)90205-n. [DOI] [PubMed] [Google Scholar]
- 28.Shikowitz MJ. Sudden sensorineural hearing loss. Med Clin N Am. 1991;75:1239–1250. doi: 10.1016/s0025-7125(16)30384-4. [DOI] [PubMed] [Google Scholar]
- 29.Heilmann L, Siekmann U, Schmid-Schonbein H. The rheologic properties of the blood during pregnancy. Dtsch Med Wochenschr. 1985;110:1705–1708. doi: 10.1055/s-2008-1069075. [DOI] [PubMed] [Google Scholar]
- 30.Laatikainen LT. Management of retinal vein occlusion. Curr Opin Ophthalmol. 1992;3:372–378. doi: 10.1097/00055735-199206000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Aboulghar MA, Mansour RT, Aboulghar MA, Mansour RT. Ovarian hyperstimulation syndrome: classifications and critical analysis of preventive measures. Hum Reprod Update. 2003;9:275–289. doi: 10.1093/humupd/dmg018. [DOI] [PubMed] [Google Scholar]
- 32.Forouzandeh B, Konicek F, Sheagren JN. Large-volume paracentesis in the treatment of cirrhotic patients with refractory ascites. The role of postparacentesis plasma volume expansion. J Clin Gastroenterol. 1996;22:207–210. doi: 10.1097/00004836-199604000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Berger W, Keller U, Berger W, Keller U. Treatment of diabetic ketoacidosis and non-ketotic hyperosmolar diabetic coma. Baillieres Clin Endocrinol Metab. 1992;6:1–22. doi: 10.1016/s0950-351x(05)80328-3. [DOI] [PubMed] [Google Scholar]
- 34.Leschke M, Klimek W, Jung F. Rheological determinants of end-organ damage. Der Internist. 2003;44:853–863. doi: 10.1007/s00108-003-0949-x. [DOI] [PubMed] [Google Scholar]
- 35.Linde I. Indications and contraindications of plasmapheresis and autologous blood donation. Beitr Infusionstherap (Contributions to infusion therapy) 1993;29:158–162. [PubMed] [Google Scholar]
- 36.Nusbacher J, McCullough J, Huestis DW. Granulocyte collection and processing. Prog Clin Biol Res. 1977;13:175–183. [PubMed] [Google Scholar]
- 37.Southard JH, Belzer FO. Organ preservation. Annu Rev Med. 1995;46:235–247. doi: 10.1146/annurev.med.46.1.235. [DOI] [PubMed] [Google Scholar]
- 38.Raju GM, Kochupillai V, Kumar L. Storage of haemopoietic stem cells for autologous bone marrow transplantation. Natl Med J India. 1995;8:216–221. [PubMed] [Google Scholar]
- 39.Kreimeier U, Christ F, Frey L, Habler O, Thiel M, Welte M, Zwissler B, Peter K. Small-volume resuscitation for hypovolemic shock. Concept, experimental and clinical results. Der Anaesthesist. 1997;46:309–328. doi: 10.1007/s001010050406. [DOI] [PubMed] [Google Scholar]
- 40.Delaney A, Bagshaw SM, Ferland A, Manns B, Laupland KB, Doig CJ. Critical Care. Vol. 9. London, England: 2005. A systematic evaluation of the quality of meta-analyses in the critical care literature; pp. R575–R582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi PT, Halpern SH, Malik N, Jadad AR, Tramer MR, Walder B. Examining the evidence in anesthesia literature: a critical appraisal of systematic reviews. Anesth Analg. 2001;92:700–709. doi: 10.1097/00000539-200103000-00029. [DOI] [PubMed] [Google Scholar]
- 42.Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, Henry DA, Boers M. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62:1013–1020. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 43.Nolan J. Fluid replacement. Br Med Bull. 1999;55:821–843. doi: 10.1258/0007142991902808. [DOI] [PubMed] [Google Scholar]
- 44.Artificial colloids. Market analysis. IMS Health. 2009 [Google Scholar]
- 45.Barron ME, Wilkes MM, Navickis RJ. A systematic review of the comparative safety of colloids. Arch Surg. 2004;139:552–563. doi: 10.1001/archsurg.139.5.552. [DOI] [PubMed] [Google Scholar]
- 46.Thompson WL. Rational use of albumin and plasma substitutes. Johns Hopkins Med J. 1975;136:220–225. [PubMed] [Google Scholar]
- 47.Boldt J. Volume therapy in cardiac surgery: are Americans different from Europeans? J Cardiothorac Vasc Anesth. 2006;20:98–105. doi: 10.1053/j.jvca.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 48.Gosling P, Rittoo D, Manji M, Mahmood A, Vohra R. Hydroxyethylstarch as a risk factor for acute renal failure in severe sepsis. Lancet. 2001;358:581. doi: 10.1016/S0140-6736(01)05718-X. author reply 582. [DOI] [PubMed] [Google Scholar]
- 49.Boldt J. Do plasma substitutes have additional properties beyond correcting volume deficits? Shock (Augusta Ga) 2006;25:103–116. doi: 10.1097/01.shk.0000189595.35661.40. [DOI] [PubMed] [Google Scholar]
- 50.Zikria BA, King TC, Stanford J, Freeman HP. A biophysical approach to capillary permeability. Surgery. 1989;105:625–631. [PubMed] [Google Scholar]
- 51.Boldt J. Saline versus balanced hydroxyethyl starch: does it matter? Curr Opin Anaesthesiol. 2008;21:679–683. doi: 10.1097/ACO.0b013e32830dd05b. [DOI] [PubMed] [Google Scholar]
- 52.Boldt J, Ince C. The impact of fluid therapy on microcirculation and tissue oxygenation in hypovolemic patients: a review. Intensive Care Med. 2010;36:1299–1308. doi: 10.1007/s00134-010-1912-7. [DOI] [PubMed] [Google Scholar]
- 53.Adams HA, Vogt PM. Circulation therapy for severe burn injuries. Der Unfallchirurg. 2009;112:462–471. doi: 10.1007/s00113-009-1653-7. [DOI] [PubMed] [Google Scholar]
- 54.Powell-Tuck J, Gosling P, Lobo DN, Allison S, Carlson GL, Gore M, Lewington AJ, Pearse RM, Mythen MG. British consensus guidelines on intravenous fluid therapy for adult surgical patients (GIFTASUP). 2008. London: NHS National Library of Health; 2008. Available at: http://www.ics.ac.uk/downloads/2008112340_GIFTASUP%20FINAL_31-10-08.pdf doi. [Google Scholar]
- 55.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 56.The American Thoracic Society Colloid Working Group. Evidence-based colloid use in the critically ill: American Thoracic Society Consensus Statement. Am J Respir Crit Care Med. 2004;170:1247–1259. doi: 10.1164/rccm.200208-909ST. [DOI] [PubMed] [Google Scholar]
- 57.Reinhart K, Brunkhorst FM, Bone HG, Bardutzky J, Dempfle CE, Forst H, Gastmeier P, Gerlach H, Grundling M, John S, Kern W, Kreymann G, Kruger W, Kujath P, Marggraf G, Martin J, Mayer K, Meier-Hellmann A, Oppert M, Putensen C, Quintel M, Ragaller M, Rossaint R, Seifert H, Spies C, Stuber F, Weiler N, Weimann A, Werdan K, Welte T. Prevention, diagnosis, treatment, and follow-up care of sepsis. First revision of the S2k Guidelines of the German Sepsis Society (DSG) and the German Interdisciplinary Association for Intensive and Emergency Care Medicine (DIVI) Der Anaesthesist. 2010;59:347–370. doi: 10.1007/s00101-010-1719-5. [DOI] [PubMed] [Google Scholar]
- 58.Joannidis M, Druml W, Forni LG, Groeneveld AB, Honore P, Oudemans-van Straaten HM, Ronco C, Schetz MR, Woittiez AJ. Prevention of acute kidney injury and protection of renal function in the intensive care unit. Expert opinion of the Working Group for Nephrology, ESICM. Intensive Care Med. 2009;36:392–411. doi: 10.1007/s00134-009-1678-y. [DOI] [PubMed] [Google Scholar]
- 59.Greaves I, Porter KM, Revell MP. Fluid resuscitation in pre-hospital trauma care: a consensus view. J R Coll Surg Edinb. 2002;47:451–457. [PubMed] [Google Scholar]
- 60.Hardy JF, de Moerloose P, Samama CM. Massive transfusion and coagulopathy: pathophysiology and implications for clinical management. Can J Anaesth (J Canadien d’anesthesie) 2006;53:S40–S58. doi: 10.1007/BF03022251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Human albumin expert group. Indications for the use of human albumin solutions: an expert report. Schweiz Med Wochenschr. 2000;130:516–522. [PubMed] [Google Scholar]
- 62.Kruskall MS, Mintz PD, Bergin JJ, Johnston MF, Klein HG, Miller JD, Rutman R, Silberstein L. Transfusion therapy in emergency medicine. Ann Emerg Med. 1988;17:327–335. doi: 10.1016/s0196-0644(88)80774-1. [DOI] [PubMed] [Google Scholar]
- 63.Martel MJ, MacKinnon KJ, Arsenault MY, Bartellas E, Klein MC, Lane CA, Sprague AE, Wilson AK. Hemorrhagic shock. J Obstet Gynaecol Can. 2002;24:504–520. quiz 521-504. [PubMed] [Google Scholar]
- 64.Vermeulen LC, Jr, Ratko TA, Erstad BL, Brecher ME, Matuszewski KA. A paradigm for consensus. The University Hospital Consortium guidelines for the use of albumin, nonprotein colloid, and crystalloid solutions. Arch Intern Med. 1995;155:373–379. doi: 10.1001/archinte.155.4.373. [DOI] [PubMed] [Google Scholar]
- 65.Asplund K. Haemodilution for acute ischaemic stroke. Cochrane database of systematic reviews. 2009 doi: 10.1002/14651858.CD000103. (Online):CD000103. [DOI] [PubMed] [Google Scholar]
- 66.Himpe D. Colloids versus crystalloids as priming solutions for cardiopulmonary bypass: a meta-analysis of prospective, randomised clinical trials. Acta Anaesthesiol Belg. 2003;54:207–215. [PubMed] [Google Scholar]
- 67.Cyna AM, Andrew M, Emmett RS, Middleton P, Simmons SW. Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane database of systematic reviews. 2009 doi: 10.1002/14651858.CD002251.pub2. (Online):CD002251. [DOI] [PubMed] [Google Scholar]
- 68.Toomtong P, Suksompong S. Intravenous fluids for abdominal aortic surgery. Cochrane database of systematic reviews. 2010 doi: 10.1002/14651858.CD000991.pub2. (Online):CD000991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dretzke J, Sandercock J, Bayliss S, Burls A. Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients. Health technology assessment (Winchester, England) 2004;8(23):1–103. doi: 10.3310/hta8230. [DOI] [PubMed] [Google Scholar]
- 70.Kozek-Langenecker SA, Jungheinrich C, Sauermann W, Van der Linden P. The effects of hydroxyethyl starch 130/0.4 (6 %) on blood loss and use of blood products in major surgery: a pooled analysis of randomized clinical trials. Anesth Analg. 2008;107:382–390. doi: 10.1213/ane.0b013e31817e6eac. [DOI] [PubMed] [Google Scholar]
- 71.Wang AT, McCoy CP, Murad MH, Montori VM. Association between industry affiliation and position on cardiovascular risk with rosiglitazone: cross sectional systematic review. Br Med J (Clinical Research edn) 2010;340:c1344. doi: 10.1136/bmj.c1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jorgensen AW, Hilden J, Gotzsche PC. Cochrane reviews compared with industry supported meta-analyses and other meta-analyses of the same drugs: systematic review. Br Med J (Clinical Research edn) 2006;333:782. doi: 10.1136/bmj.38973.444699.0B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barnes DE, Bero LA. Why review articles on the health effects of passive smoking reach different conclusions. JAMA. 1998;279:1566–1570. doi: 10.1001/jama.279.19.1566. [DOI] [PubMed] [Google Scholar]
- 74.Stelfox HT, Chua G, O’Rourke K, Detsky AS. Conflict of interest in the debate over calcium-channel antagonists. N Engl J Med. 1998;338:101–106. doi: 10.1056/NEJM199801083380206. [DOI] [PubMed] [Google Scholar]
- 75.Fugh-Berman A, McDonald CP, Bell AM, Bethards EC, Scialli AR. Promotional tone in reviews of menopausal hormone therapy after the women’s health initiative: an analysis of published articles. PLoS Med. 2011;8:e1000425. doi: 10.1371/journal.pmed.1000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shafer SL. Notice of retraction. Anesth Analg. 2010;111:1567. doi: 10.1213/ANE.0b013e3182040b99. [DOI] [PubMed] [Google Scholar]
- 77.Editors in-Chief. [Accessed 12 Mar 2011];Editor-in Chief statement regarding published clinical trials conducted without IRB approval by Joachim Boldt. 2011 Available at: http://journals.lww.com/ejanaesthesiology/Documents/EIC%20Joint%20Statement%20on%20Retractions%2012Mar2011.pdf. [PubMed]
- 78.Angell M. Is academic medicine for sale? N Engl J Med. 2000;342:1516–1518. doi: 10.1056/NEJM200005183422009. [DOI] [PubMed] [Google Scholar]
- 79.Groeneveld AB, Navickis RJ, Wilkes MM. Update on the comparative safety of colloids: a systematic review of clinical studies. Ann Surg. 2011;253:470–483. doi: 10.1097/SLA.0b013e318202ff00. [DOI] [PubMed] [Google Scholar]
- 80.Hartog CS, Kohl M, Reinhart K. A systematic review of third-generation hydroxyethyl starch (HES 130/0.4) in resuscitation: safety not adequately addressed. Anesth Analg. 2011;112:635–645. doi: 10.1213/ANE.0b013e31820ad607. [DOI] [PubMed] [Google Scholar]
- 81.Carey TS, Williams JW, Jr, Oldham JM, Goodman F, Ranney LM, Whitener L, Morgan LC, Melvin CL. Gabapentin in the treatment of mental illness: the echo chamber of the case series. J Psychiatr Pract. 2008;14(Suppl 1):15–27. doi: 10.1097/01.pra.0000333584.75741.45. [DOI] [PubMed] [Google Scholar]
- 82.Murphy GS, Greenberg SB. The new-generation hydroxyethyl starch solutions: the Holy Grail of fluid therapy or just another starch? J Cardiothorac Vasc Anesth. 2010;24:389–393. doi: 10.1053/j.jvca.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 83.Landefeld CS, Steinman MA. The Neurontin legacy-marketing through misinformation and manipulation. N Engl J Med. 2009;360:103–106. doi: 10.1056/NEJMp0808659. [DOI] [PubMed] [Google Scholar]
- 84.Prayle AP, Hurley MN, Smyth AR. Compliance with mandatory reporting of clinical trial results on ClinicalTrials.gov: cross sectional study. Br Med J (Clinical Research edn) 2012;344:d7373. doi: 10.1136/bmj.d7373. [DOI] [PubMed] [Google Scholar]
- 85.National Health Service. Colloids versus crystalloids for fluid resuscitation in critically ill patients. NHS evidence: quality, innovation, productivity and prevention (QIPP) 2008 Available online at: https://www.evidence.nhs.uk/qipp.
- 86.Schochl H, Nienaber U, Hofer G, Voelckel W, Jambor C, Scharbert G, Kozek-Langenecker S, Solomon C. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM)-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Crit Care (Lond) 2010;14:R55. doi: 10.1186/cc8948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Woessner R, Grauer MT, Dieterich HJ, Bepperling F, Baus D, Kahles T, Georgi S, Bianchi O, Morgenthaler M, Treib J. Influence of a long-term, high-dose volume therapy with 6 % hydroxyethyl starch 130/0.4 or crystalloid solution on hemodynamics, rheology and hemostasis in patients with acute ischemic stroke. Results of a randomized, placebo-controlled, double-blind study. Pathophysiol Haemost Thromb. 2003;33:121–126. doi: 10.1159/000077819. [DOI] [PubMed] [Google Scholar]
- 88.Dieterich HJ, Weissmuller T, Rosenberger P, Eltzschig HK. Effect of hydroxyethyl starch on vascular leak syndrome and neutrophil accumulation during hypoxia. Crit Care Med. 2006;34:1775–1782. doi: 10.1097/01.CCM.0000218814.77568.BC. [DOI] [PubMed] [Google Scholar]
- 89.James MF. The role of tetrastarches for volume replacement in the perioperative setting. Curr Opin Anaesthesiol. 2008;21:674–678. doi: 10.1097/ACO.0b013e32830dd073. [DOI] [PubMed] [Google Scholar]
- 90.Vincent JL. Resuscitation using albumin in critically ill patients: research in patients at high risk of complications is now needed. Br Med J (Clinical Research edn) 2006;333:1029–1030. doi: 10.1136/bmj.39029.490081.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jungheinrich C, Scharpf R, Wargenau M, Bepperling F, Baron JF. The pharmacokinetics and tolerability of an intravenous infusion of the new hydroxyethyl starch 130/0.4 (6 %, 500 mL) in mild-to-severe renal impairment. Anesth Analg. 2002;95:544–551. doi: 10.1097/00000539-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 92.Ertmer C, Kampmeier TG, Rehberg S, Morelli A, Kohler G, Lange M, Bollen Pinto B, Hohn C, Hahnenkamp K, Van doi: 10.1097/CCM.0b013e318206d403. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.