Abstract
The subcutaneous implantable cardioverter-defibrillator (S-ICD) has recently been approved for commercial use in Europe, New Zealand and the United States. It is comprised of a pulse generator, placed subcutaneously in a left lateral position, and a parasternal subcutaneous lead-electrode with two sensing electrodes separated by a shocking coil. Being an entirely subcutaneous system it avoids important periprocedural and long-term complications associated with transvenous implantable cardioverter-defibrillator (TV-ICD) systems as well as the need for fluoroscopy during implant surgery. Suitable candidates include pediatric patients with congenital heart disease that limits intracavitary lead placements, those with obstructed venous access, chronic indwelling catheters or high infection risk, as well as young patients with electrical heart disease (e.g., Brugada Syndrome, long QT syndrome, and hypertrophic cardiomyopathy). Nevertheless, given the absence of intracavitary leads, the S-ICD is unable to offer pacing (apart from short-term post-shock pacing). It is therefore not suitable in patients with an indication for antibradycardia pacing or cardiac resynchronization therapy, or with a history of repetitive monomorphic ventricular tachycardia that would benefit from antitachycardia pacing. Current data from initial clinical studies and post-commercialization “real-life” case series, including over 700 patients, have so far been promising and shown that the S-ICD successfully converts induced and spontaneous ventricular tachycardia/ventricular fibrillation episodes with associated complication and inappropriate shock rates similar to that of TV-ICDs. Furthermore, by using far-field electrograms better tachyarrhythmia discrimination when compared to TV-ICDs has been reported. Future results from ongoing clinical studies will determine the S-ICD system’s long-term performance, and better define suitable patient profiles.
Keywords: Implantable cardioverter-defibrillator, Subcutaneous, Sudden death, Ventricular tachycardia, Ventricular fibrillation
Core tip: The subcutaneous implantable cardioverter-defibrillator (S-ICD) has recently been commercialized in Europe, New Zealand and the United States and implanted in over 2000 patients so far worldwide. It represents an important innovation in the field of device therapy since it avoids the potential periprocedural and long-term complications associated with endovascular leads used with conventional transvenous ICDs. Future studies will better define patient target groups and thereby establish the therapeutic potential of this new device technology.
INTRODUCTION
The implantable cardioverter-defibrillator (ICD) effectively prevents sudden cardiac death, when used both in primary[1,2] and secondary prevention[3]. To date the vast majority of implanted systems utilize a conventional design, consisting of a transvenous lead for arrhythmia detection and treatment (antitachycardia pacing or defibrillation) positioned in the right ventricle. Nevertheless, transvenous ICD (TV-ICD) is associated with significant periprocedrual and long-term complications. A recent observational large-scale study reported 1.5% major complications (in-hospital death, cardiac arrest, cardiac perforation, cardiac valve injury, coronary venous dissection, hemothorax, pneumothorax, deep phlebitis, transient ischemic attack, stroke, myocardial infarction, cardiac tamponade, and arterial-venous fistula)[4]. Over time, the incidence of intrinsic lead defects, mainly due to insulation defects, invariably increases with a reported annual failure rate at 10-year-old leads of up to 20%[5]. Furthermore, the problem of defibrillation lead recalls is frequent and relevant[6] and revision or extraction of a chronic indwelling lead is frequently a difficult procedure with significant associated morbidity and mortality[7]. Therefore, although the TV-ICD is highly effective in treating ventricular arrhythmias its associated adverse effects are of relevance. A non-TV-ICD system is therefore an attractive option that would overcome many of these problems. Recently, a dedicated entirely subcutaneous ICD (S-ICD, Cameron Health, Inc, San Clemente, California, United States) system has been developed and recently approved for commercial use in Europe, New Zealand, and the United States with more than 2000 successful device implants so far worldwide.
IMPLANTATION, OPERATING AND PROGRAMMING FEATURES
The S-ICD system is comprised of a pulse generator, subcutaneous electrode, electrode insertion tool, and device programmer. The pulse generator has an estimated longevity of 5 years, is slightly larger and weights approximately the double (145 g) of a modern TV-ICD generator. It provides high-energy defibrillation shocks (80 J) therapy through the use of a constant tilt biphasic waveform, and is capable of delivering post-shock bradycardia pacing at 50 impulses per minute, using a 200 mA biphasic transthoracic pulse for a period of up to 30 s if > 3.5 s of post-shock asystole is detected. Since implantation is guided by anatomic landmarks, fluoroscopy is unnecessary and the operator and patient radiation exposure is subsequently avoided. The generator is placed subcutaneously in a left lateral position over the 6th rib between the midaxillary and anterior axillary lines. Via two parasternal incisions, a 3 mm tripolar parasternal electrode (polycarbonate urethane) is positioned parallel to and 1 to 2 cm to the left of the sternal midline with the distal sensing electrode localized adjacent to the manubriosternal junction and the proximal sensing electrode positioned adjacent to the xiphoid process. The 8 cm shocking coil is found between the two sensing electrodes (Figure 1). The cardiac rhythm is detected by the use of 1 of the 3 vectors, which are formed between the sensing electrodes and the pulse generator (proximal-to-can, distal-to-can, and distal to proximal) (Figure 2). The S-ICD automatically selects the most suitable vector for rhythm detection with a satisfactory R-wave/T-wave ratio, in order to minimize the risk for oversensing. In addition, the manufacture recommends carrying out a screening ECG template to confirm a satisfactory R-wave/T-wave ratio in at least 1 of the 3 available sensing configurations pre-implantation. During device insertion effective conversion of induced similar to ventricular fibrillation (VF) using 65 J is tested, nevertheless once implanted, the S-ICD only delivers a non-programmable 80 J shock to ensure a 15 J safety margin[8]. Noteworthy, since the device safety and effectiveness data comes from studies that utilized defibrillation testing this constitutes an obligatory step during implantation of the S-ICD, as opposed to the TV-ICD system where this is no longer considered necessary[8,9].
Figure 1.
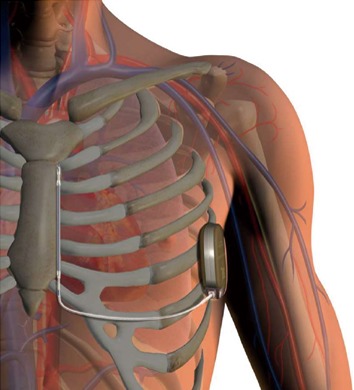
The subcutaneous implantable cardioverter-defibrillator system with the pulse generator implanted subcutaneously in a left lateral position, and the parasternal lead-electrode positioned parallel to and 1 to 2 cm to the left of the sternal midline. The lead-electrode contains two sensing electrodes separated by an 8 cm shocking coil.
Figure 2.
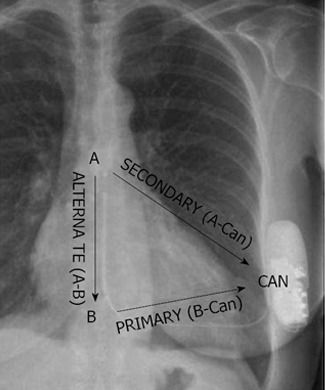
Chest X-ray of a patient with a subcutaneous implantable cardioverter-defibrillator system. The cardiac rhythm is detected by 1 of the 3 available vectors, formed between the 2 sensing electrodes and the pulse generator: B-Can, A-Can, and A-B. B-Can: Proximal-to-can; A-Can: Distal-to-can; A-B: Distal to proximal.
The S-ICD system calculates the heart rate as the average of the last 4 intervals, and performs tachycardia analysis using an 18/24 duration criteria. Tachycardia is reconfirmed after capacitor charging (average time of 14 ± 2 s) but before shock delivery to exclude the presence of non-sustained tachyarrhythmias[8]. Apart from a shock zone [VF zone in TV-ICDs], the device offers an optional conditional discrimination zone that involves 3 distinct rhythm analyses to distinguish atrial from ventricular tachyarrhythmia and avoid inappropriate shocks of the former: (1) Correlation waveform analysis of up to 41 points of each ventricular complex comparing the current tachycardia beat with the stored template acquired at rest. More than 50% of correlation is considered normal activity and suggests an atrial tachyarrhythmia; (2) Beat-to-beat analysis that evaluates monomorphic or polymorphic beat relationships. In the case of a polymorphic relationship, ventricular tachyarrhythmia is suspected and in the case of monomorphic relationship the algorithm continues; (3) QRS width analysis, using the baseline template, that indicate ventricular tachycardia (VT) if the QRS complex is wide and if the beat-to-beat analysis registered a monomorphic relationship. If the QRS complex is narrow, atrial tachyarrhythmia is assumed[8]. If ventricular tachyarrhythmia is confirmed the device is able to deliver up to 5 shocks of 80 J with shock polarity reversed if the first shock is unsuccessful (Figure 3). A total of 24 episodes can be stored with a maximum of 120 s of recorded electrograms per event. A software update, aimed at reducing the incidence of inappropriate shocks due to oversensing, was introduced in October 2009[8].
Figure 3.
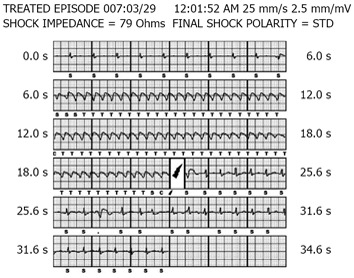
Subcutaneous implantable cardioverter-defibrillator electrogram showing a sustained monomorphic ventricular tachycardia that is terminated by a shock (lightning symbol). The subcutaneous implantable cardioverter-defibrillator (S-ICD) system uses an 18/24 interval criterion for tachycardia detection (T) which is reconfirmed after capacitor charging (C), but before shock delivery, to exclude the presence of non-sustained tachyarrhythmias. S: Sensed event not classified as tachycardia.
The programming of the S-ICD is simple since almost all device settings are automated apart from shock therapy (on/off), pacing after shock (on/off), and conditional discrimination zone (on/off) with a programmable rate cutoff between 170 to 250 bpm[8] (Table 1). The device is not adequate for patients with symptomatic bradycardia and/or frequent ventricular tachycardia episodes likely to benefit from antitachycardia pacing (ATP), or concurrent use of unipolar pacemakers (that would interfere with the S-ICD arrhythmia detection).
Table 1.
Subcutaneous implantable cardioverter-defibrillator programming
| Device options | Nominal settings |
| Shock therapy (“ON/OFF”) | On |
| Post shock pacing (“ON/OFF”) | On |
| Conditional discrimination zone (“ON/OFF”; rate cutoff: 170 to 250 bpm) | On (200 to 220 bpm) |
EARLY CLINICAL STUDIES: VALIDATING DEVICE SAFETY AND EFFICACY
The results of 4 small non-randomized initial studies using the S-ICD system in patients with standard indication for ICD implantation were published in 2010 by Bardy et al[8]. The first short-term study determined the best electrode configuration in a total of 78 patients, and led to the selection of the shock configuration currently available for clinical use. Subsequently, using the best shock configuration previously determined, a second short-term study compared defibrillation thresholds between S-ICD and TV-ICD systems that were simultaneously implanted in 49 patients. The mean defibrillation threshold was 11.1 ± 8.5 J with the TV-ICD and 36.6 ± 19.8 J with the S-ICD (P < 0.001). In one patient the S-ICD failed to defibrillate the induced VF, however this was due to incorrect electrode positioning, approximately 6 cm to the left of the sternum. Following this, two clinical studies evaluated the performance of permanently implanted S-ICD, in 6 patients from New Zealand and 55 from Europe, respectively. Those with a history of VT < 170 bpm, and documented VT known to be reliable terminated with ATP were excluded. The primary endpoint was successful conversion of 2 subsequent episodes of induced VF at 65 J out of 4 attempts. In the pilot trial, consisting of 6 patients, all 18 episodes of induced VF were appropriately detected and defibrillated, and after 16 mo follow-up there were no occurrence of VT/VF episodes, device-related complications or inappropriate shocks. In the European cohort, there were a total of 137 induced VF episodes, all appropriately detected by the S-ICD, and in 98% of the tested patients, the 2 consecutive VF episodes were successfully converted at 65 J. Mean time to shock delivery was 14.0 ± 2.5 s. In one patient (2%) defibrillation was achieved during the first induction but not during the second induction, and received as per protocol a TV-ICD. After a 10 mo follow-up 12 episodes of spontaneous VT were detected and successfully treated in 3 patients. Five patients presented minor complications (pocket infections, parasternal subcutaneous lead dislodgement). Oversensing occurred in 5 patients [muscle noise (n = 3), inadequate electrode placement (n = 1), and rate-dependent right bundle branch block (n = 1)], in all instances resolved by device reprogramming. There were no inappropriate shocks due to atrial tachyarrhythmias when such episodes occurred above > 170 bpm. Following these positive results the S-ICD was approved for commercial use in the European Union and New Zealand (June 2009).
The Subcutaneous versus Transvenous Arrhythmia Recognition Testing (START) study[10] further evaluated the accuracy of rhythm confirmation and discrimination algorithms of the S-ICD system in a prospective, multicenter, head-to-head comparison with conventional TV-ICDs from three device manufactures. Atrial and ventricular arrhythmias were induced and simultaneously recorded by transvenous and cutaneous electrodes, in 64 patients with standard indication for dual-chamber ICD or cardiac resynchronization therapy defibrillator implantation. Cutaneous electrodes were placed on the patient’s skin at locations that represented the subcutaneous position of the S-ICD system’s implanted electrode and hence simulated the 3 previously mentioned sensing vectors. A test library was developed based on data from induced atrial arrhythmias with duration ≥ 30 s and ventricular response > 170 bpm (n = 50), and ventricular arrhythmias with duration ≥ 10 s and rates > 170 bpm (n = 46). Sensitivity performance for appropriate detection of ventricular tachyarrhythmias was first assessed by comparing single-chamber TV-ICDs with S-ICD using a single-zone (VF ≥ 170 bpm) configuration, and subsequently repeated using a dual-zone (VF ≥ 240 bpm; VT ≥ 170 bpm) in order to test the impact of discrimination algorithms on the detection of ventricular arrhythmias. The dual-zone S-ICD was subsequently compared to dual-chamber TV-ICDs, in order to assess whether the addition of atrial lead information would impact on arrhythmia detection sensitivity. Finally, specificity performance for discrimination of supraventricular tachycardias of the S-ICD and single- and dual-chamber TV-ICDs was undertaken. All ventricular tachyarrhythmia were detected in all systems using a single-zone configuration, and with the dual zone configuration all but one episode were detected (a single-chamber TV-ICD failed to detect one of the ventricular episodes). There was no significant difference in the sensitivity performance to detect ventricular tachyarrhythmias between the S-ICD and the single- and dual-chamber TV-ICDs. However, specificity for supraventricular arrhythmias was significantly superior for the S-ICD when compared to 2 of the 3 TV-ICDs, and when compared to the composite of the 3 TV-ICDs [98.0% (S-ICD) vs 76.7% (single-chamber TV-ICDs) vs 68.0% (dual-chamber TV-ICDs); P < 0.001). No clear benefit of dual-chamber over single-chamber TV-ICDs was observed. Therefore, the results of the START study not only confirm the accuracy of ventricular tachyarrhythmia detection but also suggest a potential reduction in inappropriate therapies when compared to TV-ICDs. It should be noted however, that the START study included a limited number of patients, only evaluated induced arrhythmias and that most of the atrial tachyarrhythmias were atrial fibrillation. Furthermore, given that 3 different TV-ICD systems were included, comparison of the composite performance of these systems vs S-ICD should be interpreted with caution since their arrhythmia detection algorithms are not identical.
Following the initial clinical study by Bardy et al[8] and the European commercialization, the prospective, multicenter, international S-ICD System Clinical Investigation study [the investigational device exemption (IDE) study][9] was commenced in order to gain approval of the Food and Drug Administration in the United States. The primary endpoints of the study were complication-free rate at 180 d post-implant of ≥ 79% and induced VF conversion rate of ≥ 88%. Chronic performance of the S-ICD was also evaluated. The (unpublished) study results were presented at the Heart Rhythm Society conference in May 2012[9]. A total of 321 patients were included in the safety cohort and of those 92% had met the procedure-related complication-free rate at 180 d. Complications included (number of patients) system infections (4), suboptimal pulse generator and and/or electrode position (4), lead dislodgement (2), oversensing (3), inappropriate shock (3) and premature battery depletion (2). In 10 patients the device was explanted due to system infection (4), oversensing (2), pre-mature battery depletion (1), CRT indication (1), need for ATP (1), and elective due to patient request (1). The device successfully converted 100% of the induced VF episodes. During the total follow-up of a mean 321 d, 16 patients presented a total of 109 spontaneous VT/VF episodes, all of which were successfully converted with 80 J or spontaneously converted. Thirty-eight patients received inappropriate shocks (15 = atrial tachyarrhytmias with rates > discrimination zone; 24 = oversensing). On the basis of the results from the IDE study the FDA subsequently approved the S-ICD for commercial use in September 2012.
POST COMMERCIALIZATION CASE SERIES: THE INITIAL EUROPEAN EXPERIENCE
Since the European approval 6 early “real-life experience” case series have been reported from Germany[11,12], the Netherlands[13,14], and the United Kingdom[15,16] (Table 2). These studies include a total of 354 patients (32 and 41 patients with appropriate and inappropriate episodes respectively), the majority diagnosed with ischemic cardiomyopathy or idiopathic dilated cardiomyopathy and a primary prevention ICD indication[17]. Overall, the results confirm that the S-ICD effectively converts both induced and spontaneous VT/VF episodes, and indicate that complication rates and inappropriate shock (mainly due to T-wave oversensing) rates are similar to that of previous TV-ICD studies[1,18]. An interesting observation in some of the studies was that more complications occurred with the first implants, suggesting a physician-related learning curve[14,16]. The 2 United Kingdom registries by Jarman et al[15,16] from 2012 and 2013 that included 16 and 111 patients respectively, are of particular interest since they report on a different patient profile - younger individuals (23 and 33 years) with a higher prevalence of electrical inherited heart diseases (43 and 75%) and congenital structural heart diseases (12 and 25%). Both registries informed a higher rate of re-operations (17 and 19%) and inappropriate shocks (15 and 25%) than the other 4 case series. These findings were in part related to the greater incidence of T-wave oversensing (10% and 25%), since this not only caused inappropriate shocks but also led to device-explantation (0 and 5%) when present in multiple vectors. Therefore and with the study limitations (retrospective case series) in mind, it seems like T-wave oversensing may be a greater problem in young patients. As suggested by the authors, this could be ameliorated by increasing the pre-implantation requisite of satisfactory R-wave/T-wave ratio templates to > 1 in the three available sensing configurations (the manufacture currently recommends 1 satisfactory template). Furthermore, screening during exercise may be useful to assess for R-wave/T-wave ratio template changes during exertion[15,16].
Table 2.
Clinical subcutaneous implantable cardioverter-defibrillator case series n (%)
| Bardy et al[8] (2010) | Jarman et al[15] (2012) | Aydin et al[11] (2012) | Olde Nordkamp et al[14] (2012) | Köbe et al[12] (2013) | Jarman et al[16] (2013) | Burke et al[9] (ongoing, initial results) | |
| Number of patients | 55 | 16 | 40 | 118 | 69 | 111 | 304 |
| Male | 80% | 56% | 70% | 75% | 73% | N/A | 74% |
| Age [median (range)/ mean ± SD] | 56 ± 13 | 23 (10-48) | 42 ± 15 | 50 ± 15 | 46 ± 16 | 33 (10-87) | 52 ± 16 |
| Primary prevention | 78% | N/A | 44% | 60% | 59% | 50% | 79% |
| Secondary prevention | 22% | N/A | 56% | 40% | 41% | 50% | 21% |
| Underlying pathology | |||||||
| Ischemic cardiomyopathy or idiopathic dilated cardiomyopathy | 85% | 0% | 45% | 57% | 52% | 19% | 52% |
| Hypertrophic cardiomyopathy | N/A | 0% | 13% | N/A | 15% | 20% | 9% |
| Congenital heart disease | 4% | 25% | 3% | 1% | 4% | 12% | N/A |
| Electrical heart disease1 | N/A | 75% | 33% | 26% | 20% | 43% | 12% |
| Others | 11% | 0% | 6% | 16% | 10% | 7% | 27% |
| Follow-up | |||||||
| Mean/median follow-up (mo) | 10 | 9 | 8 | 18 | 7 | 13 | N/A |
| Patients with re-interventions | 6 (11) | 3 (19) | 5 (13) | 16 (14) | 3 (4) | 19 (17) | 92% procedure-related complication-free rate at 180 d |
| Patients with inappropriate shocks | 5 (9) | 4 (25) | 2 (5) | 15 (13) | 3 (4) | 17 (15) | 38 (13) |
| Patients with appropriate shocks | 3 (5) | 4 (25) | 4 (10) | 8 (7) | 3 (4) | 13 (12) | 16 (5) |
| Spontaneous VT/VF episode successfully converted by S-ICD or spontaneously converted | 100% | 100% [2 VF episodes with prolonged time (24 and 27 s) to therapy] | 96% (1 episode of electrical storm was terminated by external shocks) | 100% | 100% | 96% (1 death, see text for details) | 100% |
Brugada syndrome; long QT syndrome; catecholamine polymorphic ventricular tachycardia; idiopathic ventricular fibrillation. N/A: Data not available; S-ICD: Subcutaneous implantable cardioverter-defibrillator; VT: Ventricular tachycardia; VF: Ventricular fibrillation.
Finally, one arrhythmic death has so far been reported, however without evidence of device malfunction since the lowest detection rate was programmed to 180 bpm, and a monomorphic VT was appropriately detected at first but later fell below 180 bpm and therapy was subsequently aborted with the VT continued for a significant amount of time below the programmed rate limit. The VT later degenerated into VF, which was appropriately detected and shocked into a slow ventricular escape rhythm that did not respond to post-shock pacing[16].
ONGOING CLINICAL STUDIES
There are currently several ongoing clinical studies that shall help to provide more information on the safety and effectiveness of S-ICD, and importantly, compare its performance to the conventional TV-ICD system. Two important studies are the Evaluation of factors impacting clinical outcome and cost effectiveness of the S-ICD (EFFORTLESS S-ICD) Registry (NCT01085435)[19], and the Prospective randomized comparison of subcutaneous and transvenous implantable cardioverter-defibrillator therapy (PRAETORIAN) trial (NCT01296022)[20].
The EFFORTLESS S-ICD Registry[19] is an observational, nonrandomized study assessing the standard of care in approximately 50 investigational centers in Europe and New Zealand where the device had been approved for commercial use at the start of the study. The endpoints of the main registry, with an estimated target sample size of 1000 patients and at least 60 mo’ follow-up, are perioperative (30 d post-implant) complication-free rate, 360-d complication free-rate, and proportion of inappropriate shocks for atrial tachyarrhythmias. The study will also enroll 250 patients from the main registry to the PRO substudy (12 mo follow-up) that will evaluate the patient perspective (e.g., quality of life) and hospital personnel implant and follow-up experience with the S-ICD. Initial results from the EFFORTLESS S-ICD Registry were presented in June 2012 by which time 219 patients had been enrolled[21]. Fourteen patients had experienced 19 VT/VF episodes with successful conversion in all instances. In addition, the proportion of device-related complications and inappropriate shocks were lower than previously reported in the IDE trial[10].
For the first time, in the randomized prospective PRAETORIAN trial[20] which aims to recruit 700 patients from various centers from the Netherlands with class I or IIa ICD indication[17] and without indication for pacing therapy, the S-ICD is being compared against conventional TV-ICD systems. The primary study objective is to demonstrate non-inferiority of the S-ICD to the TV-ICD in terms of the composite of inappropriate shocks and ICD-related complications. The follow-up is estimated to a median of 30 mo. The S-ICD will be programmed with the conditional zone activated with the discriminator rate cutoff between 180 and 250 bpm. The TV-ICDs will be programmed with a monitor zone (> 167 bpm), fast VT zone (> 182 bpm) with 1 sequence of ATP followed by shocks, and a VF zone with high-energy shocks only (> 250 bpm).
WHAT PATIENTS SHOULD RECEIVE A SUBCUTANEOUS CARDIAC DEFIBRILLATOR?
Given the lack of long-term data on the S-ICD safety and performance in comparison with the conventional TV-ICDs, one can only speculate on different patient group’s suitability for the subcutaneous system (Table 3). Nevertheless, patients with pacing indication (bradycardia pacing, CRT, and ATP for recurrent monomorphic VTs) should not receive an S-ICD since this feature is not offered. Furthermore patients with documented slow VTs (< 170 bpm) represent another patient group unsuitable for the S-ICD since the VT rate would fall below the programmable VT zone (minimum of 170 bpm) and subsequently not be treated. On the contrary, in certain patient groups (congenital heart disease, indwelling catheters, or immunocompromised), where implantation of the TV-ICD system is either technically difficult (or even impossible) and/or is associated with increased procedural risk, the S-ICD represents an attractive and suitable therapeutic option. Moreover, in young and active patients with a long life expectancy, a TV-ICD is associated with significant risk of lead failure and need for reinterventions. Thus, young patients with electrical heart diseases (e.g., Brugada syndrome, long QT syndrome, and hypertrophic cardiomyopathy) with low risk of bradycardia and monormophic VT, theoretically constitute another group where the S-ICD may be the preferred device. However, caution in this patient group is at present warranted since the S-ICD system longevity (including the subcutaneous leads) is currently unknown, and initial data indicate a higher rate of inappropriate shocks due to T-wave oversensing in younger individuals[15,16].
Table 3.
Subcutaneous implantable cardioverter-defibrillator patient suitability
| Suitable | Unsuitable |
| Young and active | Present (or high risk of) AV conduction loss requiring pacing |
| No venous access | Recurrent monomorphic VT |
| Permanent indwelling catheters | CRT indication |
| High infection risk | |
| Electrical heart disease | |
| Congenital structural heart disease |
AV: Atrioventricular; CRT: Cardiac resynchronization therapy; VT: Ventricular tachycardia.
Nonetheless, in real life clinical practice the majority of patients with ICD indication have ischemic cardiomyopathy or idiopathic dilated cardiomyopathy and they do not belong to any of the previously discussed groups. The initial clinical studies showed that the S-ICD was safe and effective in this patient profile, however long-term prospective data evaluating important aspects like the development of a pacing indication is missing. Nevertheless, this issue has been addressed by a recently published single-center retrospective analysis of 2712 patients that received an ICD during 2002 and 2011[22]. Half of the patients had a pacing indication and were excluded from the analysis, and of the remaining 1345 patients, the majority with ischemic cardiomyopathy, the combined endpoint (necessity for cardiac pacing, appropriate ATP without subsequent shock or device upgrade) was reached in 34% after a median follow-up of 3.4 years. Secondary prevention, NYHA class III/IV, QRS duration were independent determinants of future unsuitability for the S-ICD. Despite its obvious limitations, the study provides data from a real-life cohort, which shows that a large proportion of patients could represent potential suitable S-ICD candidates.
CONCLUSION
The S-ICD represents an important innovation that has recently gained approval for commercial use in Europe, New Zealand and the United States. Compared to the conventional TV-ICD it avoids the potential risks associated with the periprocedural and long-term complications associated with endovascular leads. Currently ongoing clinical studies shall help to establish the S-ICD system’s long-term performance, including subcutaneous lead longevity, better define optimal patient groups that would benefit more, and offer prospective comparisons against the conventional TV-ICD system, thereby determine the therapeutic potential of this new device technology.
Footnotes
P- Reviewers De Ponti R, Kettering K, Steinberg JS S- Editor Song XX L- Editor A E- Editor Wang CH
References
- 1.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 2.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 3.Connolly SJ, Hallstrom AP, Cappato R, Schron EB, Kuck KH, Zipes DP, Greene HL, Boczor S, Domanski M, Follmann D, et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study. Cardiac Arrest Study Hamburg . Canadian Implantable Defibrillator Study. Eur Heart J. 2000;21:2071–2078. doi: 10.1053/euhj.2000.2476. [DOI] [PubMed] [Google Scholar]
- 4.Curtis JP, Luebbert JJ, Wang Y, Rathore SS, Chen J, Heidenreich PA, Hammill SC, Lampert RI, Krumholz HM. Association of physician certification and outcomes among patients receiving an implantable cardioverter-defibrillator. JAMA. 2009;301:1661–1670. doi: 10.1001/jama.2009.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kleemann T, Becker T, Doenges K, Vater M, Senges J, Schneider S, Saggau W, Weisse U, Seidl K. Annual rate of transvenous defibrillation lead defects in implantable cardioverter-defibrillators over a period of & gt; 10 years. Circulation. 2007;115:2474–2480. doi: 10.1161/CIRCULATIONAHA.106.663807. [DOI] [PubMed] [Google Scholar]
- 6.Arias MA, Domínguez-Pérez L, Toquero J, Jiménez-Candil J, Olagüe J, Díaz-Infante E, Tercedor L, Valverde I, Castro J, García-Fernández FJ, et al. Sprint fidelis defibrillation lead: a nine-center experience in Spain. Rev Esp Cardiol. 2011;64:312–318. doi: 10.1016/j.recesp.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 7.Eckstein J, Koller MT, Zabel M, Kalusche D, Schaer BA, Osswald S, Sticherling C. Necessity for surgical revision of defibrillator leads implanted long-term: causes and management. Circulation. 2008;117:2727–2733. doi: 10.1161/CIRCULATIONAHA.107.740670. [DOI] [PubMed] [Google Scholar]
- 8.Bardy GH, Smith WM, Hood MA, Crozier IG, Melton IC, Jordaens L, Theuns D, Park RE, Wright DJ, Connelly DT, et al. An entirely subcutaneous implantable cardioverter-defibrillator. N Engl J Med. 2010;363:36–44. doi: 10.1056/NEJMoa0909545. [DOI] [PubMed] [Google Scholar]
- 9.Burke MC. Safety and efficacy of a subcutaneous implantable defibrillator (S-ICD). Heart rhythm society 33rd annual scientific sessions; 2012. pp. May 9–12; Boston, USA; 2012. [Google Scholar]
- 10.Gold MR, Theuns DA, Knight BP, Sturdivant JL, Sanghera R, Ellenbogen KA, Wood MA, Burke MC. Head-to-head comparison of arrhythmia discrimination performance of subcutaneous and transvenous ICD arrhythmia detection algorithms: the START study. J Cardiovasc Electrophysiol. 2012;23:359–366. doi: 10.1111/j.1540-8167.2011.02199.x. [DOI] [PubMed] [Google Scholar]
- 11.Aydin A, Hartel F, Schlüter M, Butter C, Köbe J, Seifert M, Gosau N, Hoffmann B, Hoffmann M, Vettorazzi E, et al. Shock efficacy of subcutaneous implantable cardioverter-defibrillator for prevention of sudden cardiac death: initial multicenter experience. Circ Arrhythm Electrophysiol. 2012;5:913–919. doi: 10.1161/CIRCEP.112.973339. [DOI] [PubMed] [Google Scholar]
- 12.Köbe J, Reinke F, Meyer C, Shin DI, Martens E, Kääb S, Löher A, Amler S, Lichtenberg A, Winter J, et al. Implantation and follow-up of totally subcutaneous versus conventional implantable cardioverter-defibrillators: a multicenter case-control study. Heart Rhythm. 2013;10:29–36. doi: 10.1016/j.hrthm.2012.09.126. [DOI] [PubMed] [Google Scholar]
- 13.Dabiri Abkenari L, Theuns DA, Valk SD, Van Belle Y, de Groot NM, Haitsma D, Muskens-Heemskerk A, Szili-Torok T, Jordaens L. Clinical experience with a novel subcutaneous implantable defibrillator system in a single center. Clin Res Cardiol. 2011;100:737–744. doi: 10.1007/s00392-011-0303-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olde Nordkamp LR, Dabiri Abkenari L, Boersma LV, Maass AH, de Groot JR, van Oostrom AJ, Theuns DA, Jordaens LJ, Wilde AA, Knops RE. The entirely subcutaneous implantable cardioverter-defibrillator: initial clinical experience in a large Dutch cohort. J Am Coll Cardiol. 2012;60:1933–1939. doi: 10.1016/j.jacc.2012.06.053. [DOI] [PubMed] [Google Scholar]
- 15.Jarman JW, Lascelles K, Wong T, Markides V, Clague JR, Till J. Clinical experience of entirely subcutaneous implantable cardioverter-defibrillators in children and adults: cause for caution. Eur Heart J. 2012;33:1351–1359. doi: 10.1093/eurheartj/ehs017. [DOI] [PubMed] [Google Scholar]
- 16.Jarman JW, Todd DM. United Kingdom national experience of entirely subcutaneous implantable cardioverter-defibrillator technology: important lessons to learn. Europace. 2013;15:1158–1165. doi: 10.1093/europace/eut016. [DOI] [PubMed] [Google Scholar]
- 17.Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117:e350–e408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 18.van Rees JB, Borleffs CJ, de Bie MK, Stijnen T, van Erven L, Bax JJ, Schalij MJ. Inappropriate implantable cardioverter-defibrillator shocks: incidence, predictors, and impact on mortality. J Am Coll Cardiol. 2011;57:556–562. doi: 10.1016/j.jacc.2010.06.059. [DOI] [PubMed] [Google Scholar]
- 19.Pedersen SS, Lambiase P, Boersma LV, Murgatroyd F, Johansen JB, Reeve H, Stuart AG, Adragao P, Theuns DA. Evaluation oF FactORs ImpacTing CLinical Outcome and Cost EffectiveneSS of the S-ICD: design and rationale of the EFFORTLESS S-ICD Registry. Pacing Clin Electrophysiol. 2012;35:574–579. doi: 10.1111/j.1540-8159.2012.03337.x. [DOI] [PubMed] [Google Scholar]
- 20.Olde Nordkamp LR, Knops RE, Bardy GH, Blaauw Y, Boersma LV, Bos JS, Delnoy PP, van Dessel PF, Driessen AH, de Groot JR, et al. Rationale and design of the PRAETORIAN trial: a Prospective, RAndomizEd comparison of subcuTaneOus and tRansvenous ImplANtable cardioverter-defibrillator therapy. Am Heart J. 2012;163:753–760.e2. doi: 10.1016/j.ahj.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 21.Lambiase P, Barr CS, Knops RE, Murgatroyd F, Johansen JB, Boersma L. International Experience with a Subcutaneous ICD; Preliminary Results of the EFFORTLESS S-ICD Registry. Cardiostim; 2012. pp. June 13–16; Nice, France; 2012. [Google Scholar]
- 22.de Bie MK, Thijssen J, van Rees JB, Putter H, van der Velde ET, Schalij MJ, van Erven L. Suitability for subcutaneous defibrillator implantation: results based on data from routine clinical practice. Heart. 2013;99:1018–1023. doi: 10.1136/heartjnl-2012-303349. [DOI] [PubMed] [Google Scholar]


